Adherence Level to Arterial Hypertension Treatment: A Cross-Sectional Patient Survey and Retrospective Analysis of the NHS Prescription Database
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Approval
2.2. Data Collection
2.2.1. Patient Survey
2.2.2. Questionnaire
- 1.
- The patient demographics included data on age, sex, living status, education, residence, employment status, monthly income after taxes in euros (EUR), body mass index (BMI), smoking status, and physical activity.
- 2.
- The following items were assessed to characterize the therapy used and to evaluate AH control:
- How much and how often the patient takes medication on daily basis;
- Whether the patient takes dietary supplements;
- Years since the initiation of AH medication use;
- Whether the patient has a blood pressure monitor at home;
- Whether the patient’s blood pressure is controlled;
- Whether there has been a hospitalization related to AH.
- 3.
- Closed-ended questions were selected to characterize pharmaceutical care and to determine whether the pharmacist:
- Is able to answer all the patient’s questions;
- Warns the patient about possible side effects and informs them on which medicines should not be taken concomitantly;
- Asks the patient about the effectiveness of therapy used;
- Recommends solutions to reduce medication costs;
- Asks about any disease or medicine used prior to offering any medication or dietary supplement.
- 4.
- The participants’ medication adherence level was assessed using Morisky Widget MMAS-8 software. MMAS-8 is a validated survey method with high reliability and validity used to evaluate the level of adherence to medication for chronic conditions such as AH. MMAS-8 consists of eight items, the first seven of which are yes/no questions, while the last one is a five-point Likert scale rating [17,18,19,20,21]:
- 1.
- Do you sometimes forget to take your hypertension medication?
- 2.
- People sometimes miss taking their medications for reasons other than forgetting. Thinking over the past two weeks, were there any days when you did not take your hypertension medication?
- 3.
- Have you ever cut back or stopped taking your hypertension medication without telling your doctor because you felt worse when you took it?
- 4.
- When you travel or leave home, do you sometimes forget to bring along your hypertension medication?
- 5.
- Did you take your hypertension medication yesterday?
- 6.
- When you feel like your symptoms are under control, do you sometimes stop taking your hypertension medication?
- 7.
- Taking medication every day is a real inconvenience for some people. Do you ever feel hassled about sticking to your hypertension treatment plan?
- 8.
- How often do you have difficulty remembering to take all your hypertension medications?
2.2.3. E-Health System
2.3. Data Analysis
3. Results
3.1. Patient Survey
3.2. E-Health System
4. Discussion
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Blood Pressure. Available online: https://www.who.int/gho/ncd/risk_factors/blood_pressure_prevalence/en/ (accessed on 5 June 2019).
- Cimmaruta, D.; Lombardi, N.; Borghi, C.; Rosano, G.; Rossi, F.; Mugelli, A. Polypill, hypertension and medication adherence: The solution strategy? Int. J. Cardiol. 2018, 252, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Rosei, E.A.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; De Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for themanagement of arterial hypertension. Pol. Heart J. 2019, 77, 71–159. [Google Scholar]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertensionThe Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Abegaz, T.M.; Shehab, A.; Gebreyohannes, E.A.; Bhagavathula, A.S.; Elnour, A.A. Nonadherence to antihypertensive drugs a systematic review and meta-analysis. Medicine 2017, 96, e5641. [Google Scholar] [CrossRef] [PubMed]
- Lapi, F.; Lucenteforte, E.; Moschini, M.; Bonaiuti, R.; Di Pirro, M.; Barchielli, A.; Benemei, S.; Belladonna, M.; Nesti, N.; Coppini, R.; et al. Representativeness of the “fiesole Misurata” study database for use in pharmaco-epidemiological investigations on adherence to antihypertensive medications. Aging Clin. Exp. Res. 2013, 25, 433–445. [Google Scholar] [CrossRef] [PubMed]
- Iihara, N.; Nishio, T.; Okura, M.; Anzai, H.; Kagawa, M.; Houchi, H.; Kirino, Y. Comparing patient dissatisfaction and rational judgment in intentional medication non-adherence versus unintentional non-adherence. J. Clin. Pharm. Ther. 2014, 39, 45–52. [Google Scholar] [CrossRef]
- Uchmanowicz, B.; Jankowska, E.A.; Uchmanowicz, I.; Morisky, D.E. Self-Reported Medication Adherence Measured With Morisky Medication Adherence Scales and Its Determinants in Hypertensive Patients Aged ≥60 Years: A Systematic Review and Meta-Analysis. Front. Pharmacol. 2019, 10, 168. [Google Scholar] [CrossRef] [Green Version]
- Nunes, V.; Neilson, J.; O’Flynn, N.; Calvert, N.; Kuntze, S.; Smithson, H.; Benson, J.; Blair, J.; Bowser, A.; Clyne, W.; et al. Medicines adherence: Involving patients in decisions about prescribed medicines and supporting adherence. In NICE Guidance; NICE: London, UK, 2009; pp. 1–31. [Google Scholar]
- Nieuwlaat, R.; Wilczynski, N.; Navarro, T.; Hobson, N.; Jeffery, R.; Keepanasseril, A.; Agoritsas, T.; Mistry, N.; Iorio, A.; Jack, S.; et al. Interventions for enhancing medication adherence. Cochrane Database Syst. Rev. 2014, 11, CD000011. [Google Scholar] [CrossRef]
- Fernandez-Lazaro, C.I.; García-González, J.M.; Adams, D.P.; Fernandez-Lazaro, D.; Mielgo-Ayuso, J.; Caballero-Garcia, A.; Moreno Racionero, F.; Córdova, A.; Miron-Canelo, J.A. Adherence to treatment and related factors among patients with chronic conditions in primary care: A cross-sectional study. BMC Fam. Pract. 2019, 20, 132. [Google Scholar] [CrossRef]
- Samadian, F.; Dalili, N.; Jamalian, A. Lifestyle modifications to prevent and control hypertension. Iran. J. Kidney Dis. 2016, 10, 237–263. [Google Scholar]
- Gourley, G.K.; Gourley, D.R.; Rigolosi, E.L.M.; Reed, P.; Solomon, D.K.; Washington, E. Development and validation of the pharmaceutical care satisfaction questionnaire. Am. J. Manag. Care 2001, 7, 461–466. [Google Scholar] [PubMed]
- Malewski, D.F.; Ream, A.; Gaither, C.A. Patient satisfaction with community pharmacy: Comparing urban and suburban chain-pharmacy populations. Res. Soc. Adm. Pharm. 2015, 11, 121–128. [Google Scholar] [CrossRef]
- Jankowska-Polańska, B.; Uchmanowicz, I.; Dudek, K.; Mazur, G. Relationship between patients’ knowledge and medication adherence among patients with hypertension. Patient Prefer. Adherence 2016, 10, 2437–2447. [Google Scholar] [CrossRef] [Green Version]
- Lee, G.K.Y.; Wang, H.H.X.; Liu, K.Q.L.; Cheung, Y.; Morisky, D.E.; Wong, M.C.S. Determinants of Medication Adherence to Antihypertensive Medications among a Chinese Population Using Morisky Medication Adherence Scale. PLoS ONE 2013, 8, e62775. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Voils, C.I.; Hoyle, R.H.; Thorpe, C.T.; Maciejewski, M.L.; Yancy, W.S., Jr. Improving the measurement of self-reported medication nonadherence. J. Clin. Epidemiol. 2011, 64, 250–254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morisky, D.E.; Ang, A.; Krousel-Wood, M. Predictive validity of a medication adherence measure for hypertension control. J. Clin. Hypertens. 2008, 10, 348–354. [Google Scholar] [CrossRef] [Green Version]
- Moon, S.J.; Lee, W.-Y.; Hwang, J.S.; Hong, Y.P.; Morisky, D.E. Accuracy of a screening tool for medication adherence: A systematic review and meta-analysis of the Morisky Medication Adherence Scale-8. PLoS ONE 2017, 12, e0187139. [Google Scholar] [CrossRef]
- Krousel-Wood, M.; Islam, T.; Webber, L.S.; Re, R.; Morisky, D.E.; Muntner, P. New medication adherence scale versus pharmacy fill rates in hypertensive seniors. Am. J. Manag. Care 2009, 15, 59. [Google Scholar]
- Morisky, D.E.; Dimatteo, M.R. Improving the measurement of self-reported medication nonadherence: Final response. J. Clin. Epidemiol. 2011, 64, 262–263. [Google Scholar] [CrossRef]
- Shi, S.; Shen, Z.; Duan, Y.; Ding, S.; Zhong, Z. Association Between Medication Literacy and Medication Adherence Among Patients With Hypertension. Front. Pharmacol. 2019, 10, 822. [Google Scholar] [CrossRef] [Green Version]
- Gagnon, M.D.; Waltermaurer, E.; Martin, A.; Friedenson, C.; Gayle, E.; Hauser, D.L. Patient beliefs have a greater impact than barriers on medication adherence in a community health center. J. Am. Board Fam. Med. 2017, 30, 331–336. [Google Scholar] [CrossRef] [Green Version]
- Milosavljevic, A.; Aspden, T.; Harrison, J. Community pharmacist-led interventions and their impact on patients’ medication adherence and other health outcomes: A systematic review. Int. J. Pharm. Pract. 2018, 26, 387–397. [Google Scholar] [CrossRef] [PubMed]
- Wald, D.S.; Morris, J.K.; Wald, N.J. Randomized polypill crossover trial in people aged 50 and over. PLoS ONE 2012, 7, e41297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shrank, W.H.; Patrick, A.R.; Brookhart, M.A. Healthy user and related biases in observational studies of preventive interventions: A primer for physicians. J. Gen. Intern. Med. 2011, 26, 546–550. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Variable | Category | Adherence Level | p-Value | ||
|---|---|---|---|---|---|
| Adherent * | Intentionally Non-Adherent * | Unintentionally Non-Adherent * | |||
| Years, Mean ± SD | |||||
| Age | 677 ± 123 | 586 ± 123 | 641 ± 131 | <0.001 | |
| Number (n) | |||||
| Sex | Female | 73 | 23 | 31 | 0.002 |
| Male | 18 | 19 | 5 | ||
| Odds | 4.06 | 1.21 | 6.20 | ||
| Health Event that Led to Hospitalization due to AH | Yes | 24 | 6 | 14 | 0.048 |
| No | 65 | 36 | 22 | ||
| Odds | 0.37 | 0.17 | 0.64 | ||
| Patients Considering the Co-Payment for their Medicines to be High | Yes | 45 | 10 | 20 | 0.007 |
| No | 47 | 32 | 16 | ||
| Odds | 0.96 | 0.31 | 1.25 | ||
| Monthly Income after Taxes in Euro | <600 | 67 | 24 | 29 | 0.032 |
| ≥600 | 23 | 18 | 6 | ||
| Odds | 2.91 | 1.33 | 4.83 | ||
| Informs Family Doctor about other Prescribed Drugs from Different Specialists | Yes | 57 | 16 | 23 | 0.004 |
| No | 9 | 12 | 4 | ||
| Odds | 6.33 | 1.33 | 5.75 | ||
| Informs Family Doctor about other Over-the-Counter Drug Use | Yes | 28 | 6 | 12 | 0.050 |
| No | 37 | 27 | 22 | ||
| Odds | 0.76 | 0.22 | 0.55 | ||
| Informs Family Doctor about other Food Supplement Use | Yes | 26 | 6 | 9 | 0.165 |
| No | 32 | 20 | 15 | ||
| Odds | 0.81 | 0.30 | 0.60 | ||
| Has Sufficient Knowledge about AH | Yes | 76 | 29 | 23 | 0.059 |
| No | 16 | 12 | 13 | ||
| Odds | 4.75 | 2.42 | 1.77 | ||
| Variable | Category | Duration of AH Medical Treatment (Years) | p-Value | |||
|---|---|---|---|---|---|---|
| <2 | 2–4.9 | 5–9.9 | >10 | |||
| Number (n) | ||||||
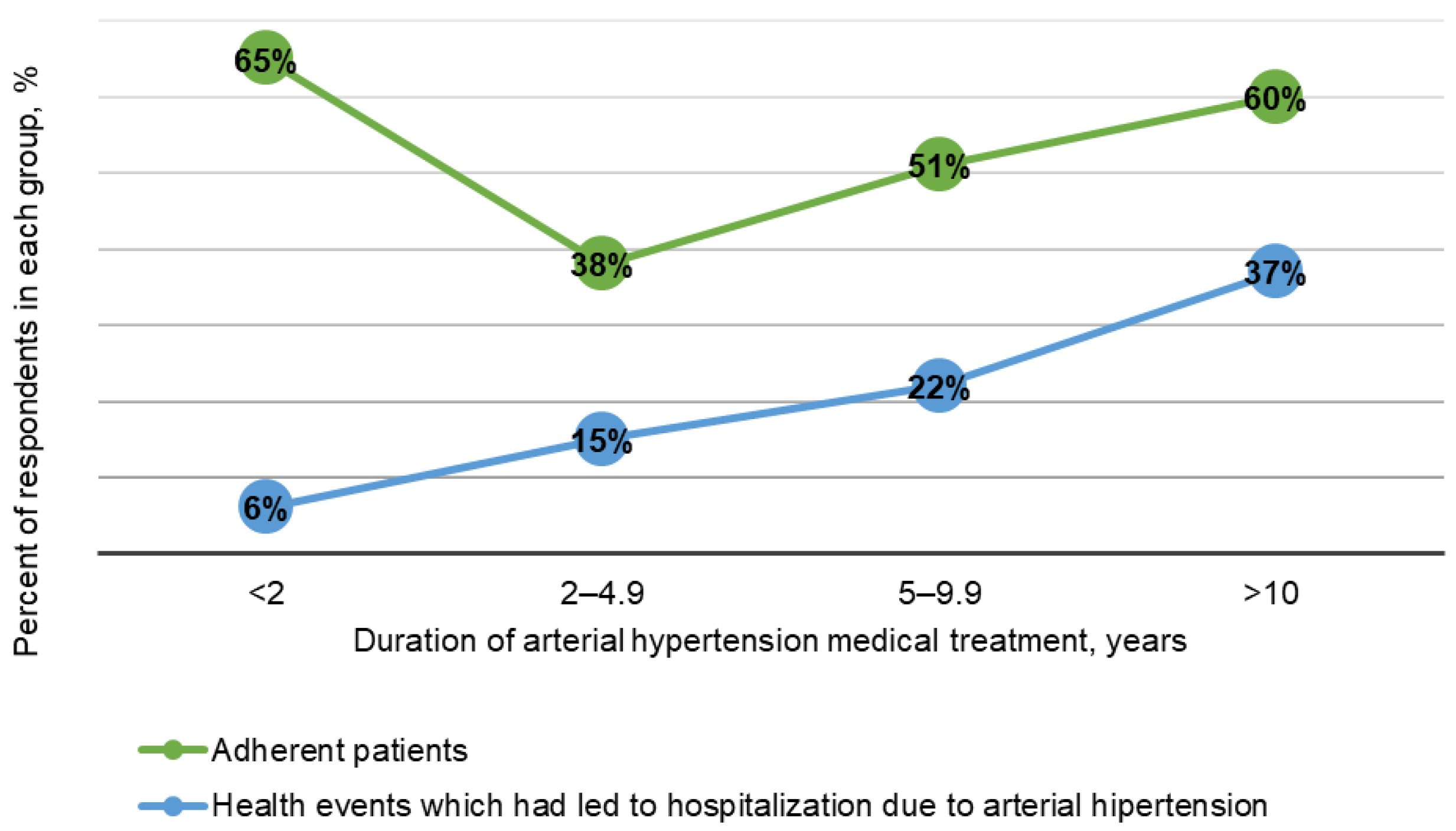
| Health Event that Led to Hospitalization due to AH | Yes | 1 | 5 | 9 | 29 | 0.011 |
| No | 16 | 28 | 31 | 48 | ||
| Odds | 0.06 | 0.18 | 0.29 | 0.60 | ||
| Adherence Level | Adherent | 11 | 13 | 21 | 47 | 0.136 |
| Non-Adherent | 6 | 21 | 20 | 31 | ||
| Odds | 1.83 | 0.62 | 1.05 | 1.51 | ||
| Variable | Category | Duration of AH Medical Treatment (Years) | p-Value | |||
|---|---|---|---|---|---|---|
| <2 | 2–4.9 | 5–9.9 | >10 | |||
| Number (n) | ||||||
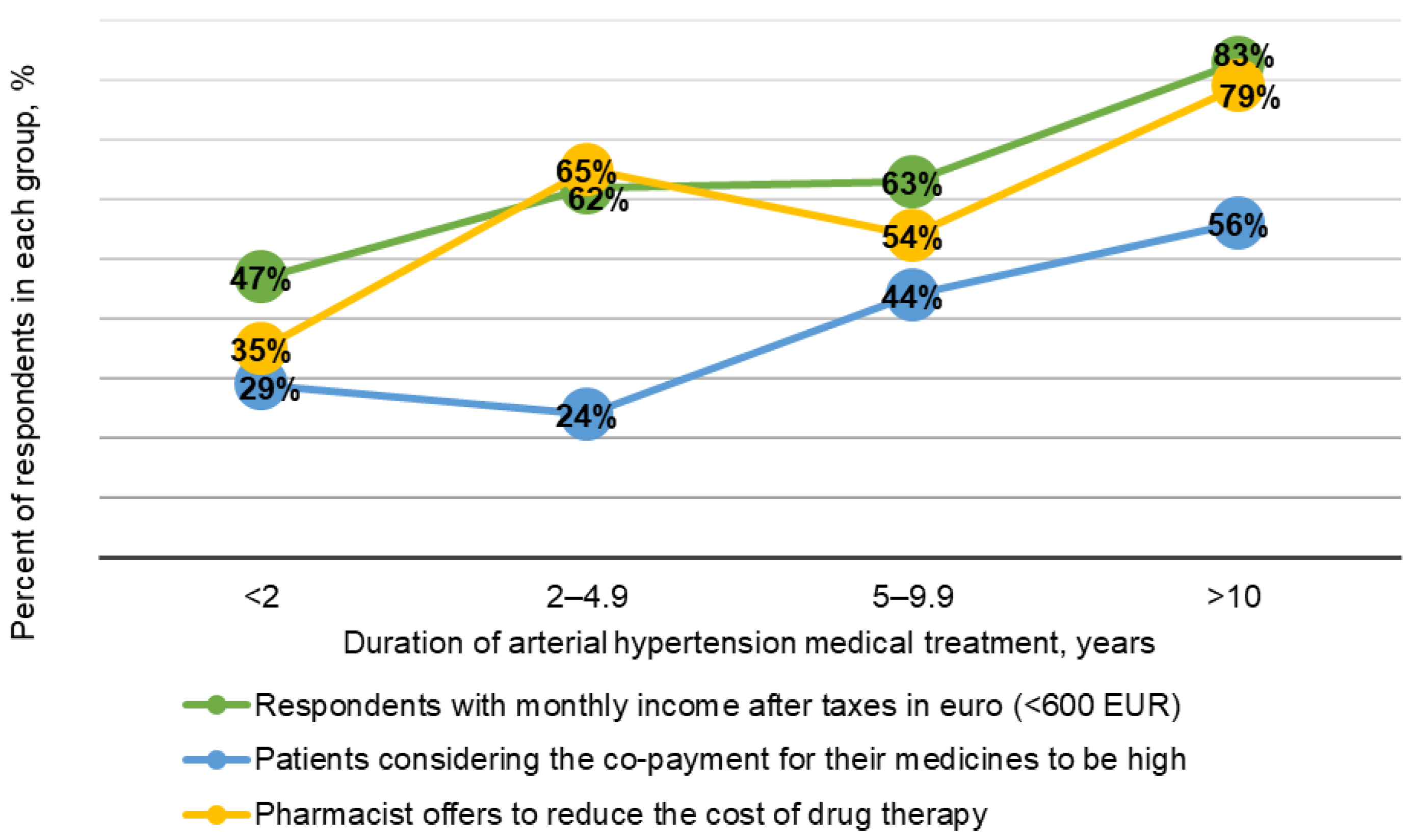
| Monthly Income after Taxes in Euro | <600 | 8 | 21 | 26 | 65 | 0.004 |
| ≥600 | 16 | 28 | 31 | 48 | ||
| Odds | 0.06 | 0.18 | 0.29 | 0.60 | ||
| Patients Considering the Co-Payment for their Medicines to be High | Yes | 5 | 8 | 18 | 44 | 0.007 |
| No | 12 | 26 | 23 | 34 | ||
| Odds | 0.41 | 0.31 | 0.78 | 1.29 | ||
| The Pharmacist Offers to Reduce the Cost of Medication Therapy | Yes | 6 | 22 | 22 | 62 | 0.002 |
| No | 11 | 10 | 17 | 16 | ||
| Odds | 0.55 | 2.20 | 1.29 | 3.88 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gavrilova, A.; Bandere, D.; Logviss, K.; Šmits, D.; Urtāne, I. Adherence Level to Arterial Hypertension Treatment: A Cross-Sectional Patient Survey and Retrospective Analysis of the NHS Prescription Database. Healthcare 2021, 9, 1085. https://doi.org/10.3390/healthcare9081085
Gavrilova A, Bandere D, Logviss K, Šmits D, Urtāne I. Adherence Level to Arterial Hypertension Treatment: A Cross-Sectional Patient Survey and Retrospective Analysis of the NHS Prescription Database. Healthcare. 2021; 9(8):1085. https://doi.org/10.3390/healthcare9081085
Chicago/Turabian StyleGavrilova, Anna, Dace Bandere, Konstantīns Logviss, Dins Šmits, and Inga Urtāne. 2021. "Adherence Level to Arterial Hypertension Treatment: A Cross-Sectional Patient Survey and Retrospective Analysis of the NHS Prescription Database" Healthcare 9, no. 8: 1085. https://doi.org/10.3390/healthcare9081085
APA StyleGavrilova, A., Bandere, D., Logviss, K., Šmits, D., & Urtāne, I. (2021). Adherence Level to Arterial Hypertension Treatment: A Cross-Sectional Patient Survey and Retrospective Analysis of the NHS Prescription Database. Healthcare, 9(8), 1085. https://doi.org/10.3390/healthcare9081085






