The Effects of Conflicts and Self-Reported Insecurity on Maternal Healthcare Utilisation and Children Health Outcomes in the Democratic Republic of Congo (DRC)
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. Measures and Variables
2.2.1. Self-Reported Insecurity
2.2.2. The Severity of Conflicts
2.2.3. Maternal Health-Seeking Behaviours
2.2.4. Diseases of Children under Five
2.2.5. Other Covariates
2.3. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.1.1. The Severity of Conflicts
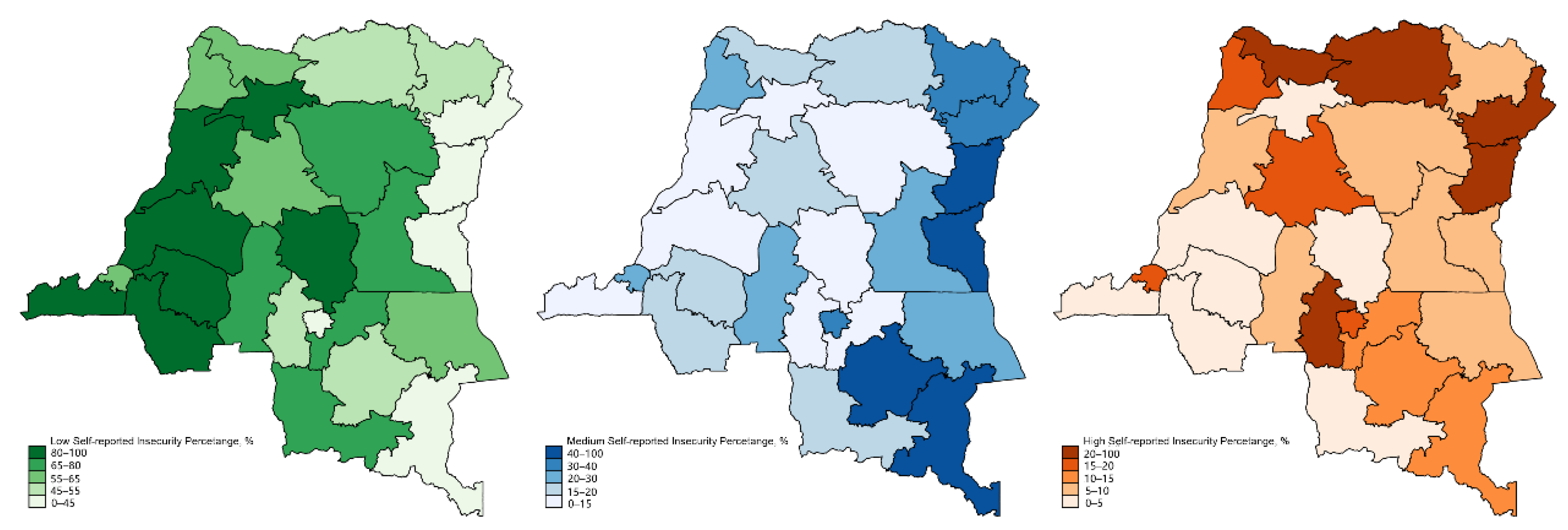
3.1.2. The Self-Reported Insecurity of Females in the DRC
3.1.3. Maternal Health-Seeking Behaviours and Diseases in Children
3.2. Maternal Health-Seeking Behaviours
3.3. Diseases in Children under Five
3.4. Stratification by the Severity of Conflicts
4. Discussions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| DRC | Democratic Republic of Congo |
| MICS | Multiple Indicators Cluster Survey |
| UCDP | Uppsala Conflict Data Program |
| UNICEF | United Nations Children’s Fund |
| MCH | Maternal and child health |
| SDGs | Sustainable Development Goals |
| UN | The United Nations |
| LMICs | Low- and middle-income countries |
| MMR | Maternal mortality ratio |
| ANC | Antenatal care |
| PNC | Post-natal care |
| BBC | British Broadcasting Corporation |
| USAID | United States Agency for International Development |
| GED | Georeferenced Event Dataset |
| BRDs | Battled related deaths |
| EIB | Early initiation breastfeeding |
| WHO | World Health Organisation |
| ORs | Odds ratios |
| CI | Confidence intervals |
| SD | Standard deviation |
References
- Global Humanitarian Overview 2019 [EN/AR/ES/FR/ZH]. 2018. Available online: https://reliefweb.int/report/world/global-humanitarian-overview-2019-enaresfrzh (accessed on 28 November 2020).
- Nordenstedt, H.; Rosling, H. Chasing 60% of maternal deaths in the post-fact era. Lancet 2016, 388, 1864–1865. [Google Scholar] [CrossRef]
- Hasan, M.M.; Magalhaes, R.J.S.; Ahmed, S.; Ahmed, S.; Biswas, T.; Fatima, Y.; Islam, M.S.; Hossain, M.S.; Mamun, A.A. Meeting the Global Target in Reproductive, Maternal, Newborn, and Child Health Care Services in Low-and Middle-Income Countries. Glob. Health Sci. Pract. 2020, 8, 654–665. [Google Scholar] [CrossRef]
- Gopalan, S.S.; Silverwood, R.J.; Salman, O.; Howard, N. Associations between acute conflict and maternal care usage in Egypt: An uncontrolled before-and-after study using demographic and health survey data. Int. J. Health Policy Manag. 2019, 8, 158. [Google Scholar] [CrossRef]
- WHO. Health in 2015: From MDGs, Millennium Development Goals to SDGs, Sustainable Development Goals; WHO: Geneva, Switzerland, 2015; 212p. [Google Scholar]
- Asi, Y.M.; Williams, C. The role of digital health in making progress toward Sustainable Development Goal (SDG) 3 in conflict-affected populations. Int. J. Med. Inform. 2018, 114, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Sustainable Development and the Sustainable Development and the Progress in Conflict Progress in Conflict-Affected Countries Affected Countries. Available online: https://sustainabledevelopment.un.org/content/documents/1503nsds-conflict-web.pdf (accessed on 28 November 2020).
- Bamberger, L. International Institute for Strategic Studies (IISS): Armed Conflict Survey. The Worldwide review of Political, Military and Humanitarian Trends in Current Conflicts. SIRIUS–Z. für Strateg. Anal. 2017, 1, 311–312. [Google Scholar] [CrossRef] [Green Version]
- DRC Conflict: Facts, FAQs, and How to Help. 2020. Available online: https://www.worldvision.org/disaster-relief-news-stories/drc-conflict-facts (accessed on 28 November 2020).
- Vlassenroot, K.; Huggins, C. Land, Migration and Conflict in Eastern DRC. From the Ground up: Land Rights, Conflict and Peace in sub-Saharan Africa; Clover, J., Ed.; Institute for Security Studies: Pretoria, South Africa, 2005; pp. 115–194. [Google Scholar]
- Democratic Republic of Congo: The Conflict in Focus. 2020. Available online: https://www.c-r.org/programme/east-and-central-africa/democratic-republic-congo-conflict-focus?gclid=Cj0KCQiAh4j-BRCsARIsAGeV12Buy5_iIJBiIBmztCe0eIcmNBAxqkyT1yRAVMULfjpPUiBiuw3DXkMaApczEALw_wcB (accessed on 28 November 2020).
- Top 5 Things to Know about the Violence in the Kasai Region. 2020. Available online: https://reliefweb.int/report/democratic-republic-congo/top-5-things-know-about-violence-kasai-region (accessed on 28 November 2020).
- Global Report on Internal Displacement 2020. 2020. Available online: https://www.internal-displacement.org/global-report/grid2020/ (accessed on 28 November 2020).
- Maternal Mortality. Available online: https://www.who.int/en/news-room/fact-sheets/detail/maternal-mortality (accessed on 28 November 2020).
- Democratic Republic of Congo Systematic Country Diagnostic. Available online: http://documents1.worldbank.org/curated/en/171101529346675751/pdf/DRC-SCD-FINAL-ENGLISH-06132018.pdf (accessed on 28 November 2020).
- The World Bank in DRC. Available online: https://www.worldbank.org/en/country/drc/overview (accessed on 6 April 2020).
- Malnutrition: Quantifying the Health Impact at National and Local Levels. Available online: https://www.who.int/quantifying_ehimpacts/publications/MalnutritionEBD12.pdf (accessed on 6 April 2020).
- Impact of Armed Conflict on the Nutritional Situation of Children. Available online: http://www.fao.org/3/w2357e/W2357E02.htm (accessed on 6 April 2020).
- Jones, G.A.; Rodgers, D. The World Bank’s World Development Report 2011 on conflict, security and development: A critique through five vignettes. J. Int. Dev. 2011, 23, 980–995. [Google Scholar] [CrossRef]
- Congo, Democratic Republic of the, 2017–2018 MICS Survey Findings_French. Available online: https://mics-surveys-prod.s3.amazonaws.com/MICS6/West%20and%20Central%20Africa/Congo%2C%20Democratic%20Republic%20of%20the/2017-2018/Snapshots/Congo%2C%20Democratic%20Republic%20of%20the%2C%202017-18%20MICS%20Snapshots_French.pdf (accessed on 28 November 2020).
- UNICEF. MICS6 TOOLS-Data Collection. Available online: https://mics.unicef.org/tools#data-collection (accessed on 15 June 2020).
- Pettersson, T.; Öberg, M. Organized violence, 1989–2019. J. Peace Res. 2020, 57, 597–613. [Google Scholar] [CrossRef]
- Sundberg, R.; Melander, E. Introducing the UCDP georeferenced event dataset. J. Peace Res. 2013, 50, 523–532. [Google Scholar] [CrossRef]
- WHO. Indicators for Assessing Infant and Young Child Feeding Practices: Part 2: Measurement; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- Chi, P.C.; Bulage, P.; Urdal, H.; Sundby, J. A qualitative study exploring the determinants of maternal health service uptake in post-conflict Burundi and Northern Uganda. BMC Pregnancy Childbirth 2015, 15, 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsuoka, S.; Aiga, H.; Rasmey, L.C.; Rathavy, T.; Okitsu, A. Perceived barriers to utilization of maternal health services in rural Cambodia. Health Policy 2010, 95, 255–263. [Google Scholar] [CrossRef] [PubMed]
- USAID. Global Health of Democratic Republic of the Congo 2021. 2021. Available online: https://www.usaid.gov/democratic-republic-congo/global-health (accessed on 28 November 2020).
- UNICEF. Conflict in the Kasai, Democratic Republic of the Congo. Available online: https://www.unicef.org/child-alert/democratic-republic-of-congo (accessed on 28 November 2020).
- Kadir, A.; Shenoda, S.; Goldhagen, J.; Pitterman, S. The effects of armed conflict on children. Pediatrics 2018, 142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wagner, Z.; Heft-Neal, S.; Bhutta, Z.A.; Black, R.E.; Burke, M.; Bendavid, E. Armed conflict and child mortality in Africa: A geospatial analysis. Lancet 2018, 392, 857–865. [Google Scholar] [CrossRef]
- Tickell, K.D.; Pavlinac, P.B.; John-Stewart, G.C.; Denno, D.M.; Richardson, B.A.; Naulikha, J.M.; Kirera, R.K.; Swierczewski, B.E.; Singa, B.O.; Walson, J.L. Impact of childhood nutritional status on pathogen prevalence and severity of acute diarrhea. Am. J. Trop. Med. Hyg. 2017, 97, 1337–1344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
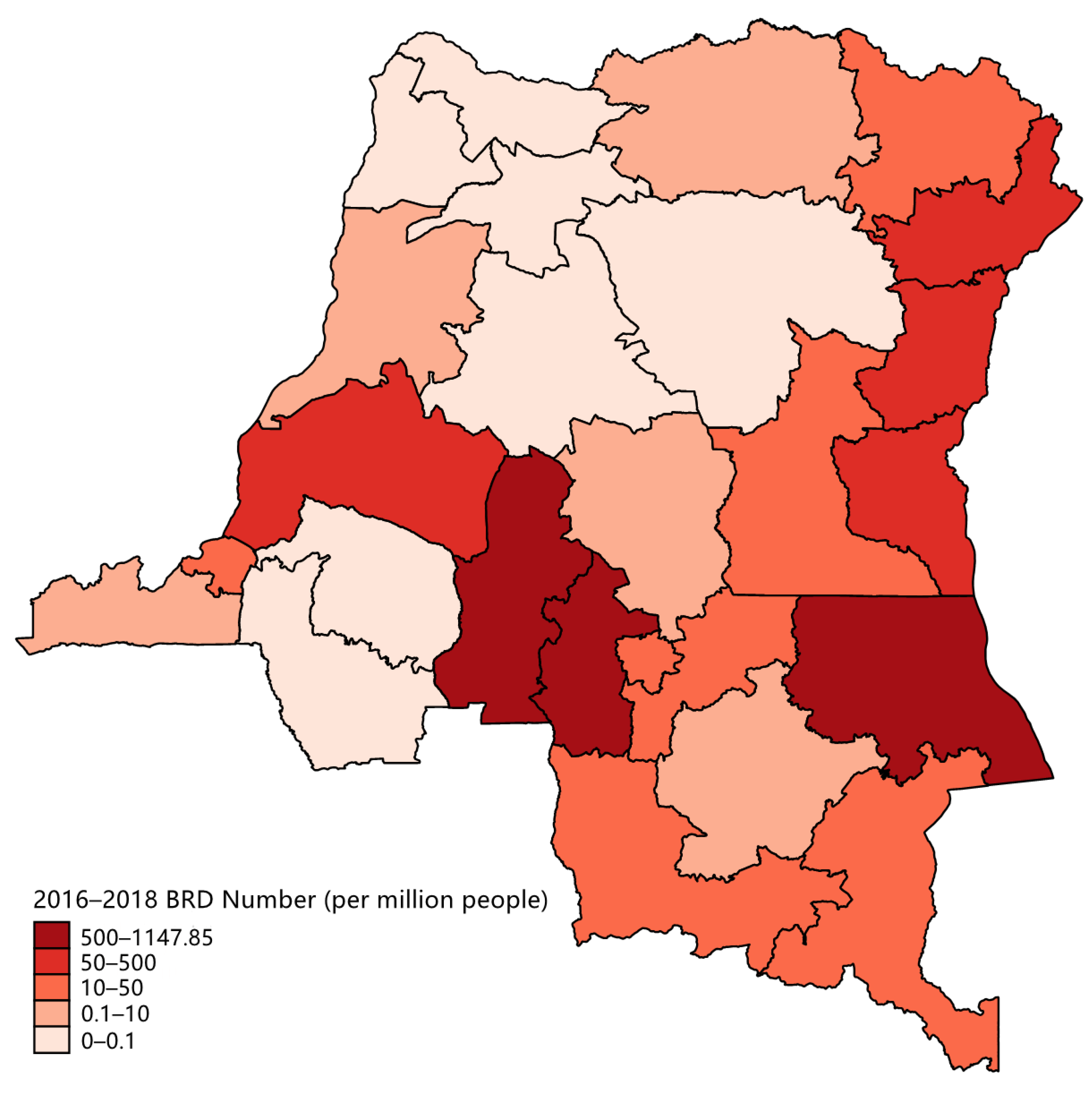
| Province | Population a | Cumulative BRD Number | BRD Incidence (per Million People) |
|---|---|---|---|
| Kasai | 2,313,020 | 2655 | 1147.85 |
| Kasai Central | 2,870,553 | 2237 | 779.29 |
| Tanganyika | 1,639,923 | 920 | 561 |
| Maindombe | 1,899,673 | 875 | 460.61 |
| Nord Kivu | 5,555,285 | 2516 | 452.9 |
| Ituri | 4,275,675 | 806 | 188.51 |
| Sud Kivu | 4,817,219 | 526 | 109.19 |
| Maniema | 1,946,690 | 87 | 44.69 |
| Kasai Oriental | 3,000,730 | 112 | 37.32 |
| Lomami | 2,146,227 | 42 | 19.57 |
| Lualaba | 2,140,924 | 38 | 17.75 |
| Haut Uele | 1,443,995 | 25 | 17.31 |
| Haut-Katanga | 4,382,428 | 62 | 14.15 |
| Kinshasa | 8,808,080 | 108 | 12.26 |
| Kongo Central | 4,624,229 | 39 | 8.43 |
| Bas Uele | 883,848 | 7 | 7.92 |
| Sankuru | 1,285,635 | 1 | 0.78 |
| Equateur | 1,806,970 | 1 | 0.55 |
| Haut Lomami | 2,526,306 | 1 | 0.4 |
| Tshuapa | 1,113,011 | 0 | 0 |
| Mongala | 1,227,929 | 0 | 0 |
| Nord Ubangi | 1,178,158 | 0 | 0 |
| Sud Ubangi | 2,016,644 | 0 | 0 |
| Kwango | 2,063,644 | 0 | 0 |
| Kwilu | 4,128,694 | 0 | 0 |
| Tshopo | 1,446,446 | 0 | 0 |
| Total | Low Insecurity | Medium Insecurity | High Insecurity | p-Value | |
|---|---|---|---|---|---|
| Number of observations (N) | 8144 | 5224 | 1933 | 987 | |
| Percentage (%) | 100 | 59.12 | 28.62 | 12.26 | |
| Maternal age, year (SD) | 1.66 (0.47) | 1.69 (0.46) | 1.59 (0.49) | 1.63 (0.48) | 0.0463 |
| Region | <0.001 | ||||
| Urban | 34.28 | 30.77 | 40.55 | 36.60 | |
| Rural | 65.72 | 69.23 | 59.45 | 63.40 | |
| Household wealth | 0.0658 | ||||
| Highest | 11.30 | 10.68 | 11.86 | 12.92 | |
| Upper middle | 18.89 | 16.97 | 22.97 | 18.59 | |
| Middle | 20.71 | 21.85 | 19.26 | 18.67 | |
| Lower middle | 23.12 | 23.25 | 22.63 | 23.60 | |
| Lowest | 25.98 | 27.25 | 23.28 | 26.22 | |
| Maternal education | 0.0595 | ||||
| Preschool | 18.74 | 18.48 | 17.72 | 22.40 | |
| Primary school | 35.98 | 35.22 | 38.53 | 33.73 | |
| Lower secondary school | 14.59 | 16.21 | 12.64 | 11.35 | |
| Higher secondary school | 27.68 | 27.69 | 27.03 | 29.19 | |
| Above | 3.00 | 2.41 | 4.08 | 3.33 | |
| The severity of conflicts | <0.001 | ||||
| Low | 37.25 | 46.51 | 22.66 | 26.65 | |
| High | 62.75 | 53.49 | 77.34 | 73.35 | |
| Maternal health-seeking behaviours | |||||
| Skilled Antenatal Care (ANC) ≥ 4 | 41.52 | 37.31 | 44.86 | 54.06 | <0.001 |
| Skilled attendants at delivery | 84.26 | 82.15 | 87.23 | 87.53 | <0.001 |
| Received Postnatal Care (PNC) | 6.56 | 6.35 | 8.13 | 3.94 | 0.0245 |
| Early initiation of breastfeeding (EIB) | 47.41 | 44.93 | 50.03 | 53.26 | 0.0083 |
| Total | Low Insecurity | Medium Insecurity | High Insecurity | p-Value | |
|---|---|---|---|---|---|
| Number of observations (N) | 14,403 | 9245 | 3418 | 1740 | |
| Percentage (%) | 100 | 59.04 | 28.84 | 12.12 | |
| Maternal age, year (SD) | 29.14 (6.68) | 29.30 (6.70) | 29.09 (6.70) | 28.51 (6.45) | <0.001 |
| Region | <0.001 | ||||
| Urban | 34.07 | 30.93 | 39.82 | 35.67 | |
| Rural | 65.93 | 69.07 | 60.18 | 64.33 | |
| Household wealth | 0.0018 | ||||
| Highest | 11.11 | 10.32 | 11.96 | 12.98 | |
| Upper middle | 19.22 | 17.63 | 22.72 | 18.68 | |
| Middle | 20.84 | 21.93 | 19.7 | 18.21 | |
| Lower middle | 23.08 | 23.06 | 22.83 | 23.71 | |
| Lowest | 25.75 | 27.06 | 22.79 | 26.42 | |
| Maternal education | <0.001 | ||||
| Preschool | 19.27 | 19.34 | 17.26 | 23.68 | |
| Primary school | 36.59 | 35.43 | 39.86 | 34.46 | |
| Lower secondary school | 14.91 | 16.74 | 12.63 | 11.43 | |
| Higher secondary school | 26.34 | 26.08 | 26.28 | 27.76 | |
| Above | 2.89 | 2.41 | 3.97 | 2.67 | |
| Child age, year (SD) | 1.61 (1.43) | 1.60 (1.43) | 1.60 (1.43) | 1.63 (1.47) | 0.8830 |
| Child sex | 0.6406 | ||||
| Male | 49.33 | 49.95 | 48.35 | 48.62 | |
| Female | 50.67 | 50.05 | 51.65 | 51.38 | |
| The severity of conflicts | <0.001 | ||||
| Low | 35.55 | 44.53 | 21.27 | 25.74 | |
| High | 64.45 | 55.47 | 78.73 | 74.26 | |
| Child diseases | |||||
| Diarrhoea | 15.75 | 13.35 | 19.32 | 18.97 | <0.001 |
| Fever | 28.01 | 27.06 | 28.69 | 30.98 | 0.1420 |
| Cough | 26.33 | 24.41 | 27.58 | 32.72 | <0.001 |
| Dyspnea | 9.36 | 7.07 | 12.15 | 13.92 | <0.001 |
| Low Insecurity | Medium Insecurity OR (95%CI) | High Insecurity OR (95%CI) | |
|---|---|---|---|
| Skilled antenatal care (ANC) ≥4 | [1] | 1.30 (1.07, 1.58) ** | 1.93 (1.50, 2.49) *** |
| Skilled attendants at delivery | 1.28 (1.02, 1.62)* | 1.42 (1.08, 1.87) * | |
| Received postnatal care (PNC) | 1.55 (1.12. 2.16) ** | 0.69 (0.38, 1.24) | |
| Early initiation of breastfeeding (EIB) | 1.15 (0.96, 1.38) | 1.32 (1.04, 1.68) * |
| Low Insecurity | Medium Insecurity OR (95%CI) | High Insecurity OR (95%CI) | |
|---|---|---|---|
| Diseases in children under five | |||
| Diarrhea | [1] | 1.45 (1.21, 1.74) *** | 1.47 (1.14, 1.88) ** |
| Fever | 1.08 (0.93, 1.25) | 1.23 (1.01, 1.50) * | |
| Cough | 1.11 (0.95, 1.28) | 1.45 (1.19, 1.77) *** | |
| Dyspnea | 1.68 (1.36, 2.08) *** | 2.04 (1.52, 2.73) *** | |
| Low Insecurity | Medium Insecurity | High Insecurity | ||||
|---|---|---|---|---|---|---|
| N | OR (95%CI) | N | OR (95%CI) | N | OR (95%CI) | |
| Low severity of conflicts | 2732 | 743 | 452 | |||
| Skilled antenatal care (ANC) ≥4 | 899 | [1] | 281 | 1.10 (0.81, 1.49) | 164 | 1.24 (0.81, 1.88) |
| Skilled attendants at delivery | 1853 | 470 | 0.67 (0.50, 0.89) ** | 268 | 0.83 (0.61, 1.14) | |
| Received postnatal care (PNC) | 239 | 101 | 2.30 (1.51, 3.50) *** | 41 | 1.16 (0.50, 2.69) | |
| Early initiation of breastfeeding (EIB) | 1205 | 256 | 0.84 (0.63, 1.12) | 170 | 0.82 (0.55, 1.22) | |
| High severity of conflicts | 2492 | 1190 | 535 | |||
| Skilled antenatal care (ANC) ≥4 | 905 | [1] | 493 | 1.40 (1.10, 1.77) ** | 248 | 2.23 (1.64, 3.03) *** |
| Skilled attendants at delivery | 1980 | 1006 | 1.77 (1.29, 2.43) *** | 448 | 1.91 (1.29, 2.82) ** | |
| Received postnatal care (PNC) | 118 | 72 | 1.06 (0.67, 1.68) | 19 | 0.39 (0.19, 0.77) ** | |
| Early initiation of breastfeeding (EIB) | 1164 | 625 | 1.32 (1.05, 1.65) * | 314 | 1.63 (1.21, 2.21) ** | |
| Low Insecurity | Medium Insecurity | High Insecurity | ||||
|---|---|---|---|---|---|---|
| N | OR (95%CI) | N | OR (95%CI) | N | OR (95%CI) | |
| Low severity of conflicts | 4727 | 1272 | 770 | |||
| Diarrhea | 644 | [1] | 223 | 1.56 (1.14, 2.14) ** | 135 | 1.40 (0.96, 2.02) |
| Fever | 1183 | 413 | 1.27 (1.01, 1.61) * | 235 | 1.18 (0.86, 1.64) | |
| Cough | 1030 | 364 | 1.40 (1,10, 1,77) ** | 211 | 1.29 (0.92, 1.81) | |
| Dyspnea | 334 | 138 | 1.64 (1.17, 2.29) ** | 88 | 1.91 (1.23, 2.95) ** | |
| High severity of conflicts | 4518 | 2146 | 970 | |||
| Diarrhea | 659 | [1] | 390 | 1.41 (1.13, 1.75) ** | 174 | 1.44 (1.06, 1.95) * |
| Fever | 1259 | 605 | 1.01 (0.84, 1.22) | 309 | 1.19 (0.93, 1.53) | |
| Cough | 1161 | 588 | 1.02 (0.85,1.23) | 336 | 1.47 (1.15, 1.87) ** | |
| Dyspnea | 354 | 243 | 1.70 (1.31, 2.21) *** | 126 | 2.05 (1.44, 2.93) *** | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, T.; Qi, X.; He, Q.; Hee, J.; Takesue, R.; Yan, Y.; Tang, K. The Effects of Conflicts and Self-Reported Insecurity on Maternal Healthcare Utilisation and Children Health Outcomes in the Democratic Republic of Congo (DRC). Healthcare 2021, 9, 842. https://doi.org/10.3390/healthcare9070842
Zhang T, Qi X, He Q, Hee J, Takesue R, Yan Y, Tang K. The Effects of Conflicts and Self-Reported Insecurity on Maternal Healthcare Utilisation and Children Health Outcomes in the Democratic Republic of Congo (DRC). Healthcare. 2021; 9(7):842. https://doi.org/10.3390/healthcare9070842
Chicago/Turabian StyleZhang, Tingkai, Xinran Qi, Qiwei He, Jiayi Hee, Rie Takesue, Yan Yan, and Kun Tang. 2021. "The Effects of Conflicts and Self-Reported Insecurity on Maternal Healthcare Utilisation and Children Health Outcomes in the Democratic Republic of Congo (DRC)" Healthcare 9, no. 7: 842. https://doi.org/10.3390/healthcare9070842
APA StyleZhang, T., Qi, X., He, Q., Hee, J., Takesue, R., Yan, Y., & Tang, K. (2021). The Effects of Conflicts and Self-Reported Insecurity on Maternal Healthcare Utilisation and Children Health Outcomes in the Democratic Republic of Congo (DRC). Healthcare, 9(7), 842. https://doi.org/10.3390/healthcare9070842








