Prevalence of Low Back Pain and Associated Factors in Older Adults: Amazonia Brazilian Community Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Sample Size
2.4. Evaluation
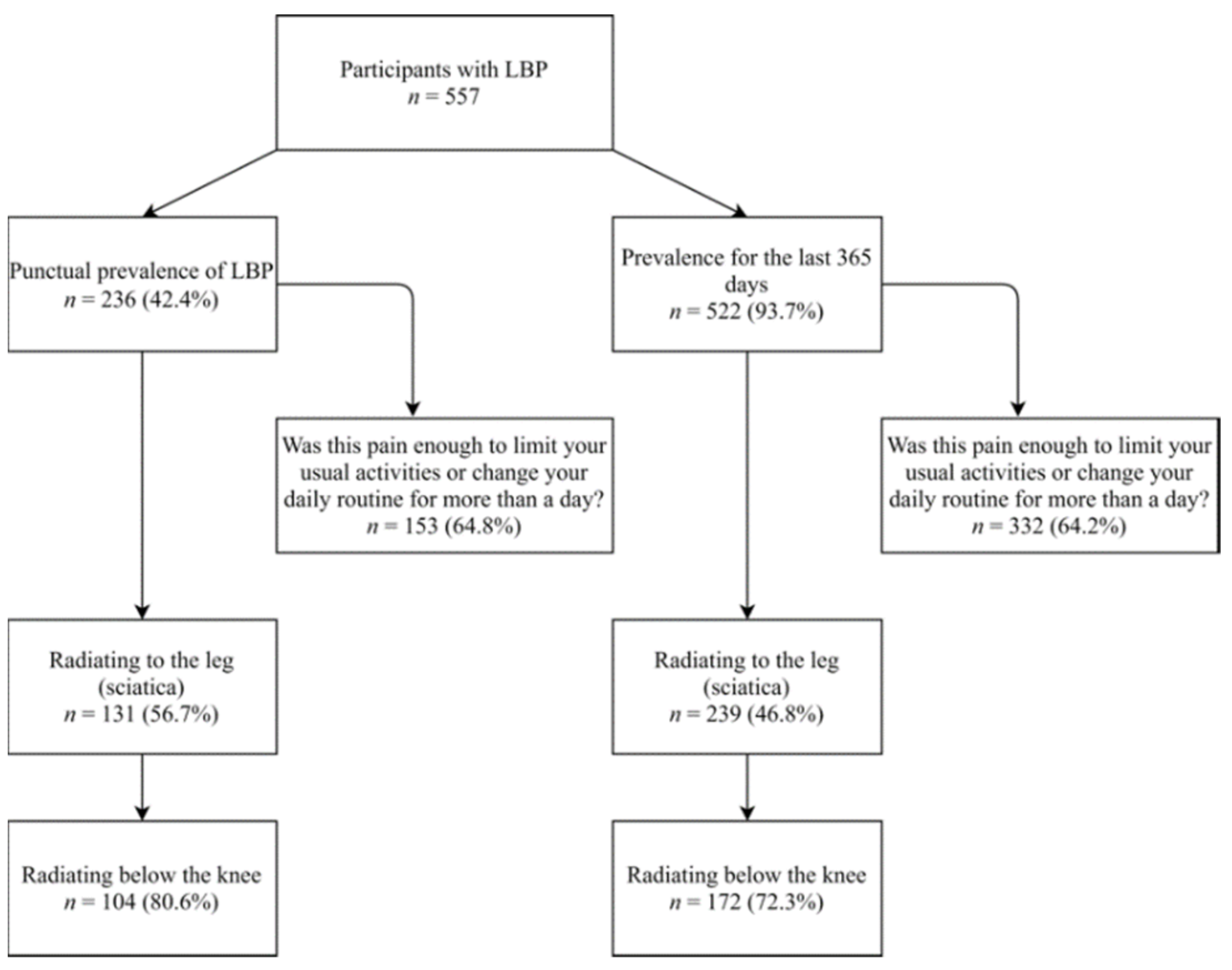
2.4.1. LBP Prevalence: Punctual and for the Last 365 Days
2.4.2. Sociodemographic and Clinical Variables
2.4.3. Pain Assessment
2.4.4. Functional Disability
2.4.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vos, T.; Allen, C.; Arora, M.; Barber, R.M.; Bhutta, Z.A.; Brown, A.; Carter, A.; Casey, D.C.; Charlson, F.J.; Chen, A.Z.; et al. Global, Regional, and National Incidence, Prevalence, and Years Lived with Disability for 310 Diseases and Injuries, 1990–2015: A Systematic Analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1545–1602. [Google Scholar] [CrossRef]
- Dionne, C.E.; Dunn, K.M.; Croft, P.R.; Nachemson, A.L.; Buchbinder, R.; Walker, B.F.; Wyatt, M.; Cassidy, J.D.; Rossignol, M.; Leboeuf-Yde, C.; et al. A Consensus Approach Toward the Standardization of Back Pain Definitions for Use in Prevalence Studies. Spine 2008, 33, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Hoy, D.; Bain, C.; Williams, G.; March, L.; Brooks, P.; Blyth, F.; Woolf, A.; Vos, T.; Buchbinder, R. A Systematic Review of the Global Prevalence of Low Back Pain. Arthritis Rheum. 2012, 64, 2028–2037. [Google Scholar] [CrossRef] [PubMed]
- Kamper, S.J.; Henschke, N.; Hestbaek, L.; Dunn, K.M.; Williams, C.M. Musculoskeletal Pain in Children and Adolescents. Braz. J. Phys. Ther. 2016, 20, 275–284. [Google Scholar] [CrossRef] [PubMed]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What Low Back Pain is and why we Need to Pay Attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef]
- Dellaroza, M.S.G.; Furuya, R.K.; Cabrera, M.A.S.; Matsuo, T.; Trelha, C.; Yamada, K.N.; Pacola, L. Caracterização Da Dor Crônica e Métodos Analgésicos Utilizados Por Idosos Da Comunidade. Rev. Assoc. Med. Bras. 2008, 54, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, G.D.; Silva, M.C.; Rombaldi, A.J.; Wrege, E.D.; Siqueira, F.V.; Hallal, P.C. Prevalência de Dor Nas Costas e Fatores Associados Em Adultos Do Sul Do Brasil: Estudo de Base Populacional. Rev. Bras. Fisioter. 2011, 15, 31–36. [Google Scholar] [CrossRef]
- Bressler, H.B.; Keyes, W.J.; Rochon, P.A.; Badley, E. The Prevalence of Low Back Pain in the Elderly: A Systematic Review of the Literature. Spine 1999, 24, 1813. [Google Scholar] [CrossRef]
- Weiner, D.K.; Sakamoto, S.; Perera, S.; Breuer, P. Chronic Low Back Pain in Older Adults: Prevalence, Reliability, and Validity of Physical Examination Findings: Physical Examination for Low Back Pain. J. Am. Geriatr. Soc. 2006, 54, 11–20. [Google Scholar] [CrossRef]
- De Souza, I.M.B.; Sakaguchi, T.F.; Yuan, S.L.K.; Matsutani, L.A.; do Espírito-Santo, A.D.S.; Pereira, C.A.D.B.; Marques, A.P. Prevalence of Low Back Pain in the Elderly Population: A Systematic Review. Clinics 2019, 74, e789. [Google Scholar] [CrossRef]
- Leopoldino, A.A.O.; Diz, J.B.M.; Martins, V.T.; Henschke, N.; Pereira, L.S.M.; Dias, R.C.; Oliveira, V.C. Prevalence of Low Back Pain in Older Brazilians: A Systematic Review with Meta-Analysis. Rev. Bras. Reumatol. 2016, 56, 258–269. [Google Scholar] [CrossRef]
- Alves, L.C.; Leimann, B.C.Q.; Vasconcelos, M.E.L.; Carvalho, M.S.; Vasconcelos, A.G.G.; Fonseca, T.C.O.D.; Lebrão, M.L.; Laurenti, R. A Influência Das Doenças Crônicas Na Capacidade Funcional Dos Idosos Do Município de São Paulo, Brasil. Cad. Saúde Pública 2007, 23, 1924–1930. [Google Scholar] [CrossRef]
- Quintino, N.M.; Conti, M.H.S.D.; Palma, R.; Gatti, M.A.N.; Simeão, S.F.A.P.; Vitta, A.D. Prevalence and Factors Associated with Low Back Pain in Elderly Registered in the Family Health Strategy. Fisioter. Mov. 2017, 30, 367–377. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. für die STROBE Initiative Das Strengthening the Reporting of Observational Studies in Epidemiology (STROBE-) Statement: Leitlinien für das Berichten von Beobachtungsstudien. Notfall Rettungsmed 2008, 11, 260–265. [Google Scholar] [CrossRef]
- Maher, C.; Underwood, M.; Buchbinder, R. Non-Specific Low Back Pain. Lancet 2017, 389, 736–747. [Google Scholar] [CrossRef]
- Hancock, M.J.; Maher, C.G.; Latimer, J.; Spindler, M.F.; McAuley, J.H.; Laslett, M.; Bogduk, N. Systematic Review of Tests to Identify the Disc, SIJ or Facet Joint as the Source of Low Back Pain. Eur. Spine J. 2007, 16, 1539–1550. [Google Scholar] [CrossRef]
- Brasil Instituto Brasileiro de Geografia e Estatística Censo Demográfico. 2010. Available online: https://cidades.ibge.gov.br/brasil/am/manaus/panorama (accessed on 8 June 2020).
- Berenson, M.; Levine, D.; Szabat, K.A.; Krehbiel, T.C. Estimation and Sample Size Determination for Finite Populations. In Basic Business Statistics: Concepts and Applications; Pearson Higher Education Australia: Melbourne, VIC, Australia, 2012; ISBN 0-13-216838-3. [Google Scholar]
- Lipschitz, D.A. Screening for Nutritional Status in the Elderly. Prim Care 1994, 21, 55–67. [Google Scholar]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Costa, L.O.P.; Maher, C.G.; Latimer, J.; Ferreira, P.H.; Ferreira, M.L.; Pozzi, G.C.; Freitas, L.M.A. Clinimetric Testing of Three Self-Report Outcome Measures for Low Back Pain Patients in Brazil: Which One is the Best? Spine 2008, 33, 2459–2463. [Google Scholar] [CrossRef]
- Nusbaum, L.; Natour, J.; Ferraz, M.B.; Goldenberg, J. Translation, Adaptation and Validation of the Roland-Morris Questionnaire—Brazil Roland-Morris. Braz. J. Med. Biol. Res. 2001, 34, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Pereira, J.C.R. Bioestatística Em Outras Palavras; EDUSP Fapesp: São Paulo, Brasil, 2010; ISBN 85-314-1226-9. [Google Scholar]
- Munzel, U.; Hothorn, L.A. A Unified Approach to Simultaneous Rank Test Procedures in the Unbalanced One-Way Layout. Biom. J. 2001, 43, 553–569. [Google Scholar] [CrossRef]
- Chen, W.; Qian, L.; Shi, J.; Franklin, M. Comparing Performance between Log-Binomial and Robust Poisson Regression Models for Estimating Risk Ratios under Model Misspecification. BMC Med. Res. Methodol. 2018, 18, 63. [Google Scholar] [CrossRef] [PubMed]
- Bastos, L.S.; de Oliveira, R.V.C.; de Velasque, L.S. Obtaining Adjusted Prevalence Ratios from Logistic Regression Models in Cross-Sectional Studies. Cad. Saúde Pública 2015, 31, 487–495. [Google Scholar] [CrossRef] [PubMed]
- Dellaroza, M.S.G.; Pimenta, C.A.d.M.; Duarte, Y.A.; Lebrão, M.L. Dor Crônica Em Idosos Residentes Em São Paulo, Brasil: Prevalência, Características e Associação Com Capacidade Funcional e Mobilidade (Estudo SABE). Cad. Saúde Pública 2013, 29, 325–334. [Google Scholar] [CrossRef]
- Sampaio, L.S.; Reis, L.A.d.; Lessa, R.S.; Torres, G.d.V. Prevalência de Patologias Ortopédicas Em Idosos Atendidos Em Hospital Público No Município de Lajedo Do Tabocal-BA. Enferm Atual 2007, 7, 30–32. [Google Scholar]
- Dellaroza, M.S.G.; Pimenta, C.A.d.M.; Matsuo, T. Prevalência e Caracterização Da Dor Crônica Em Idosos Não Institucionalizados. Cad. Saúde Pública 2007, 23, 1151–1160. [Google Scholar] [CrossRef]
- Barros, M.B.d.A.; Francisco, P.M.S.B.; Zanchetta, L.M.; César, C.L.G. Tendências Das Desigualdades Sociais e Demográficas Na Prevalência de Doenças Crônicas No Brasil, PNAD: 2003–2008. Ciênc. Saúde Coletiva 2011, 16, 3755–3768. [Google Scholar] [CrossRef]
- Hoy, D.; March, L.; Brooks, P.; Blyth, F.; Woolf, A.; Bain, C.; Williams, G.; Smith, E.; Vos, T.; Barendregt, J.; et al. The Global Burden of Low Back Pain: Estimates from the Global Burden of Disease 2010 Study. Ann. Rheum. Dis. 2014, 73, 968–974. [Google Scholar] [CrossRef]
- Dionne, C.E.; Dunn, K.M.; Croft, P.R. Does Back Pain Prevalence Really Decrease with Increasing Age? A Systematic Review. Age Ageing 2006, 35, 229–234. [Google Scholar] [CrossRef]
- Stewart Williams, J.; Ng, N.; Peltzer, K.; Yawson, A.; Biritwum, R.; Maximova, T.; Wu, F.; Arokiasamy, P.; Kowal, P.; Chatterji, S. Risk Factors and Disability Associated with Low Back Pain in Older Adults in Low- and Middle-Income Countries. Results from the WHO Study on Global AGEing and Adult Health (SAGE). PLoS ONE 2015, 10, e0127880. [Google Scholar] [CrossRef]
- Silva, M.C.d.; Fassa, A.G.; Valle, N.C.J. Dor Lombar Crônica Em Uma População Adulta Do Sul Do Brasil: Prevalência e Fatores Associados. Cad. Saúde Pública 2004, 20, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Loyola Filho, A.I.d.; Uchoa, E.; Lima-Costa, M.F. Estudo Epidemiológico de Base Populacional Sobre Uso de Medicamentos Entre Idosos Na Região Metropolitana de Belo Horizonte, Minas Gerais, Brasil. Cad. Saúde Pública 2006, 22, 2657–2667. [Google Scholar] [CrossRef] [PubMed]
- Murtagh, K.N.; Hubert, H.B. Gender Differences in Physical Disability Among an Elderly Cohort. Am. J. Public Health 2004, 94, 1406–1411. [Google Scholar] [CrossRef] [PubMed]
- Bartley, E.J.; Fillingim, R.B. Sex Differences in Pain: A Brief Review of Clinical and Experimental Findings. Br. J. Anaesth. 2013, 111, 52–58. [Google Scholar] [CrossRef]
- Docking, R.E.; Fleming, J.; Brayne, C.; Zhao, J.; Macfarlane, G.J.; Jones, G.T.; on behalf of the Cambridge City over-75s Cohort. Study collaboration Epidemiology of Back Pain in Older Adults: Prevalence and Risk Factors for Back Pain Onset. Rheumatology 2011, 50, 1645–1653. [Google Scholar] [CrossRef]
- Waddell, G. Biopsychosocial Analysis of Low Back Pain. Baillière’s Clin. Rheumatol. 1992, 6, 523–557. [Google Scholar] [CrossRef]
- Shiri, R.; Karppinen, J.; Leino-Arjas, P.; Solovieva, S.; Viikari-Juntura, E. The Association Between Obesity and Low Back Pain: A Meta-Analysis. Am. J. Epidemiol. 2010, 171, 135–154. [Google Scholar] [CrossRef]
- Weiner, D.K.; Rudy, T.E.; Kim, Y.-S.; Golla, S. Do Medical Factors Predict Disability in Older Adults with Persistent Low Back Pain? Pain 2004, 112, 214–220. [Google Scholar] [CrossRef]
- Corseuil, M.W.; Schneider, I.J.C.; Silva, D.A.S.; Costa, F.F.; Silva, K.S.; Borges, L.J.; d’Orsi, E. Perception of Environmental Obstacles to Commuting Physical Activity in Brazilian Elderly. Prev. Med. 2011, 53, 289–292. [Google Scholar] [CrossRef]
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W.; Ekelund, U. Global Physical Activity Levels: Surveillance Progress, Pitfalls, and Prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef]
- Gualano, B.; Tinucci, T. Sedentarismo, Exercício Físico e Doenças Crônicas. Rev. Bras. Educ. Fís. Esporte 2011, 25, 37–43. [Google Scholar] [CrossRef]
- Ledoux, É.; Dubois, J.-D.; Descarreaux, M. Physical and Psychosocial Predictors of Functional Trunk Capacity in Older Adults with and without Low Back Pain. J. Manip. Physiol. Ther. 2012, 35, 338–345. [Google Scholar] [CrossRef]
- Farias, R.G.; Santos, S.M.A. Dos Influência Dos Determinantes Do Envelhecimento Ativo Entre Idosos Mais Idosos. Texto Contexto Enferm. 2012, 21, 167–176. [Google Scholar] [CrossRef]
- Palma, R.; Conti, M.H.S.d.; Quintino, N.M.; Gatti, M.A.N.; Simeão, S.F.A.P.; Vitta, A.d. Functional Capacity and Its Associated Factors in the Elderly with Low Back Pain. Acta Ortop. Bras. 2014, 22, 295–299. [Google Scholar] [CrossRef]
- Scherer, M.; Hansen, H.; Gensichen, J.; Mergenthal, K.; Riedel-Heller, S.; Weyerer, S.; Maier, W.; Fuchs, A.; Bickel, H.; Schön, G.; et al. Association between Multimorbidity Patterns and Chronic Pain in Elderly Primary Care Patients: A Cross-Sectional Observational Study. BMC Fam. Pract. 2016, 17, 68. [Google Scholar] [CrossRef]
- Elfering, A.; Mannion, A.F.; Jacobshagen, N.; Tamcan, O.; Müller, U. Beliefs about Back Pain Predict the Recovery Rate over 52 Consecutive Weeks. Scand. J. Work Environ. Health 2009, 35, 437–445. [Google Scholar] [CrossRef]
- Smith, A.J.; O’Sullivan, P.B.; Beales, D.; Straker, L. Back Pain Beliefs are Related to the Impact of Low Back Pain in 17-Year-Olds. Phys. Ther. 2012, 92, 1258–1267. [Google Scholar] [CrossRef]
- Alves, L.C.; Rodrigues, R.N. Determinantes Da Autopercepção de Saúde Entre Idosos Do Município de São Paulo, Brasil. Rev. Panam. Salud Publica 2005, 17. [Google Scholar] [CrossRef] [PubMed]
- Linton, S.J.; Shaw, W.S. Impact of Psychological Factors in the Experience of Pain. Phys. Ther. 2011, 91, 700–711. [Google Scholar] [CrossRef] [PubMed]
| Variable | Participants n = 700 (%) | Pain Median (557) | First Quartile Interval | Third Quartile Interval | p-Value | Functional Disability Median (557) | First Quartile Interval | Third Quartile Interval | p-Value |
|---|---|---|---|---|---|---|---|---|---|
| Sex | |||||||||
| Female | 546 (78) | 6 | 5.00 | 8.00 | 0.039 1 | 12 | 7.00 | 17.00 | <0.001 1 |
| Male | 154 (22) | 6 | 5.00 | 7.00 | 9 | 4.50 | 12.00 | ||
| Age group | |||||||||
| 60 to 70 years old | 526 (75.1) | 6 | 5.00 | 8.00 | 0.651 2 | 11 | 6.00 | 16.00 | 0.220 2 |
| 71 to 80 years old | 146 (20.9) | 6 | 5.00 | 7.00 | 11 | 7.00 | 17.00 | ||
| >80 years old | 28 (4) | 6 | 5.00 | 7.00 | 15 | 7.00 | 19.00 | ||
| Skin color (self-reported) | |||||||||
| Yellow | 27 (3.9) | 7 | 5.50 | 8.00 | 0.866 2 | 11 | 6.00 | 16.00 | 0.790 2 |
| White | 196 (28) | 6 | 5.00 | 8.00 | 11 | 7.00 | 17.00 | ||
| Indigenous | 18 (2.6) | 6 | 5.00 | 7.00 | 12 | 5.00 | 15.00 | ||
| Brown | 387 (55.3) | 6 | 5.00 | 8.00 | 11.5 | 7.00 | 16.00 | ||
| Black | 72 (10.3) | 6 | 5.00 | 8.00 | 10.5 | 4.50 | 16.00 | ||
| Marital status | |||||||||
| Married | 338 (48.3) | 6 | 5.00 | 8.00 | 0.357 2 | 11 | 5.50 | 16.00 | 0.483 2 |
| Divorced | 65 (9.3) | 6 | 4.50 | 7.00 | 10 | 5.00 | 14.50 | ||
| Single | 118 (16.9) | 6 | 5.00 | 8.00 | 11 | 7.00 | 17.00 | ||
| Widower | 179 (25.6) | 6 | 5.00 | 7.00 | 11 | 8.00 | 16.00 | ||
| Individual income * | |||||||||
| Without income | 85 (12.1) | 6 | 5.00 | 8.00 | 12.5 | 5.50 | 18.00 | ||
| Class A | 2 (0.3) | 7.5 | 7.00 | 8.00 | 0.096 2 | 17.5 | 12.00 | 23.00 | 0.168 2 |
| Class B | 6 (0.9) | 6 | 6.00 | 7.00 | 9 | 0.00 | 19.00 | ||
| Class C | 46 (6.6) | 5 | 4.00 | 7.00 | 8 | 4.50 | 13.50 | ||
| Class D | 123 (17.6) | 6 | 5.0 | 7.00 | 10 | 7.00 | 15.00 | ||
| Class E | 438 (62.6) | 6 | 5.00 | 8.00 | 11 | 6.00 | 17.00 | ||
| Education (years) | |||||||||
| Did not study | 3 (0.4) | 8 | 7.00 | 8.50 | <0.001 2 | 17 | 10.50 | 18.50 | 0.064 2 |
| 1 to 4 years | 219 (31.3) | 6 | 5.00 | 8.00 | 12 | 7.00 | 17.00 | ||
| 5 to 8 years | 135 (19.3) | 7 | 5.00 | 9.00 | 13 | 7.00 | 18.00 | ||
| 9 to 11 years | 76 (10.9) | 5 | 4.00 | 7.00 | 10 | 5.00 | 15.00 | ||
| >11 years | 267 (38.1) | 6 | 5.00 | 7.50 | 10 | 5.00 | 15.00 | ||
| Previous occupation ** | 0.536 2 | 0.066 2 | |||||||
| Armed forces, police, and military Firefighters | 2 (0.3) | 4 | 2.00 | 6.00 | 6 | 3.00 | 9.00 | ||
| Science and arts professionals | 75 (10.7) | 6 | 5.00 | 7.00 | 8 | 4.00 | 14.00 | ||
| Agricultural, forestry, hunting, and fishing workers | 69 (9.9) | 6 | 6.00 | 7.50 | 13.5 | 7.00 | 17.50 | ||
| Industrial goods and service production workers 1 | 77 (11) | 6 | 5.00 | 7.50 | 10 | 7.50 | 18.00 | ||
| Industrial goods and service production workers 2 | 29 (4.1) | 6 | 5.00 | 8.00 | 11 | 4.50 | 16.00 | ||
| Administrative service workers | 65 (9.3) | 6 | 5.00 | 6.00 | 12 | 5.00 | 18.00 | ||
| Service workers and salespeople in shops and markets | 352 (50.3) | 6 | 5.00 | 7.00 | 11 | 7.50 | 15.00 | ||
| Secondary school technicians | 29 (4.1) | 6 | 5.00 | 8.00 | 12 | 7.00 | 16.00 | ||
| Current Occupation | |||||||||
| Do not work | 634 (90.6) | - | - | - | - | - | - | ||
| Work | 66 (9.4) | - | - | - | - | - | - |
| Variable | Participants n = 700 (%) | Pain Median (557) | First Quartile Interval | Third Quartile Interval | p-Value | Functional Disability Median (557) | First Quartile Interval | Third Quartile Interval | p-Value |
|---|---|---|---|---|---|---|---|---|---|
| BMI (kg/m2) * | |||||||||
| <22: underweight | 77 (11) | 6 | 5.00 | 8.00 | 0.048 2 | 13 | 7.00 | 18.00 | <0.001 2 |
| 22–27: normal weight | 310 (44.3) | 6 | 5.00 | 7.00 | 10 | 5.00 | 15.00 | ||
| >27: obesity | 313 (44.7) | 6 | 5.00 | 8.00 | 12 | 7.00 | 17.00 | ||
| Physical activity level (IPAQ) | |||||||||
| Active | 243 (34.7) | 7 | 5.00 | 8.00 | 0.085 2 | 10 | 5.00 | 14.50 | <0.001 2 |
| Very active | 55 (7.9) | 6 | 4.00 | 7.00 | 9 | 3.50 | 12.00 | ||
| Insufficiently active | 150 (21.4) | 6 | 5.00 | 7.00 | 10 | 7.00 | 16.00 | ||
| Sedentary | 252 (36) | 6 | 5.00 | 8.00 | 14 | 7.00 | 18.00 | ||
| Smoking | |||||||||
| Nonsmoker | 447 (63.9) | 6 | 5.00 | 8.00 | 0.245 2 | 12 | 7.00 | 17.00 | 0.658 2 |
| Ex-smoker | 235 (33.6) | 6 | 5.00 | 8.00 | 10 | 6.00 | 15.00 | ||
| Smoker | 18 (2.6) | 6 | 6.00 | 9.00 | 9 | 6.00 | 16.00 | ||
| Alcohol consumption | |||||||||
| Do not consume | 594 (84.9) | 6 | 5.00 | 8.00 | 0.464 2 | 11 | 7.00 | 17.00 | 0.139 2 |
| Once a month or less | 61 (8.7) | 6 | 5.00 | 7.00 | 12.5 | 5.50 | 15.00 | ||
| Twice to four times/month | 35 (5.0) | 6 | 4.00 | 7.50 | 9 | 4.00 | 12.5 | ||
| Twice to three times/week | 8 (1.1) | 5.5 | 5.00 | 6.00 | 7.5 | 3.00 | 9.00 | ||
| Four or more times/week | 2 (0.3) | 4.5 | 4.00 | 5.00 | 12.5 | 8.00 | 17.00 | ||
| Emotional Level ** | |||||||||
| No way | 338 (48.3) | 6 | 5.00 | 7.50 | 0.007 2 | 8.5 | 4.00 | 14.00 | <0.001 2 |
| Lightly | 172 (24.6) | 6 | 5.00 | 8.00 | 14 | 8.00 | 18.00 | ||
| Moderately | 123 (17.6) | 6 | 5.00 | 7.00 | 12 | 8.00 | 17.00 | ||
| Considerable | 42 (6) | 7 | 5.00 | 9.00 | 15 | 12.00 | 18.00 | ||
| Extremely | 25 (3.6) | 8 | 6.00 | 10.00 | 14 | 11.00 | 19.00 | ||
| Health perception | |||||||||
| Bad | 87 (12.4) | 8 | 5.50 | 10.00 | <0.001 2 | 16 | 11.00 | 20.00 | <0.001 2 |
| Regular | 327 (46.7) | 6 | 5.00 | 8.00 | 11 | 7.00 | 16.00 | ||
| Good | 233 (33.3) | 6 | 4.00 | 7.00 | 10 | 4.00 | 15.00 | ||
| Very good | 43 (6.1) | 6 | 5.00 | 6.00 | 8.5 | 4.00 | 11.00 | ||
| Excellent | 10 (1.4) | 4.5 | 3.00 | 10.00 | 4.5 | 1.00 | 10.00 | ||
| Disease (self-reported) *** | |||||||||
| Diabetes mellitus | 160 (28.8) | Absent 6 | 5.00 | 8.00 | 0.077 1 | Absent 11 | 6.00 | 16.00 | 0.032 1 |
| Present 7 | 5.00 | 8.00 | Present 12 | 7.00 | 17.00 | ||||
| Dyslipidemia | 17 (3.1) | Absent 6 | 5.00 | 8.00 | 0.255 1 | Absent 11 | 6.00 | 16.00 | <0.001 1 |
| Present 6 | 4.00 | 6.00 | Present 16 | 14.00 | 20.00 | ||||
| Arterial hypertension | 244 (43.9) | Absent 6 | 5.00 | 8.00 | 0.521 1 | Absent 10 | 5.00 | 16.00 | 0.051 1 |
| Present 6 | 5.00 | 8.00 | Present 12 | 7.00 | 17.00 | ||||
| Rheumatoid arthritis | 86 (9) | - | - | ||||||
| Osteoarthritis | 99 (11) | ||||||||
| Osteoporosis | 22 (2) | - | - | - | - | - | - | ||
| Other diseases | 62 (6) | ||||||||
| Did not report | 169 (17) | ||||||||
| Variable | Coefficient | SE | PR | 95% CI | p-Value | |
|---|---|---|---|---|---|---|
| Lower Limit | Higher Limit | |||||
| Intercept | −0.5739 | 0.6291 | ||||
| Age | −0.0088 | 0.0083 | 0.9912 | 0.9753 | 10.074 | 0.2889 |
| Sex (male) | −0.2628 | 0.1460 | 0.7689 | 0.5776 | 10.236 | 0.0718 |
| BMI | 0.0128 | 0.0076 | 10.129 | 0.9978 | 10.282 | 0.0943 |
| DLP | −0.5783 | 0.4443 | 0.5609 | 0.2348 | 13.398 | 0.193 |
| DM | 0.2163 | 0.0981 | 12.415 | 10.244 | 15.046 | 0.0274 |
| Education (5 to 8 years) | 0.1408 | 0.1216 | 11.512 | 0.907 | 1.461 | 0.247 |
| Education (9 or more years) | −0.1543 | 0.1141 | 0.857 | 0.6853 | 10.718 | 0.1761 |
| Variable | Coefficient | SE | PR | 95% CI | p-Value | |
|---|---|---|---|---|---|---|
| Lower Limit | Higher Limit | |||||
| Intercept | −19.871 | 0.6224 | 0.0014 | |||
| Age | 0.0054 | 0.0082 | 10.054 | 0.9895 | 10.216 | 0.5064 |
| Sex (male) | −0.4032 | 0.1607 | 0.6682 | 0.4877 | 0.9156 | 0.0121 |
| BMI | 0.0146 | 0.0080 | 10.147 | 0.9989 | 10.308 | 0.0684 |
| Arterial hypertension | 0.1067 | 0.1019 | 11.126 | 0.9111 | 13.585 | 0.2952 |
| DLP | 0.7629 | 0.1537 | 21.445 | 15.868 | 28.982 | <0.0001 |
| DM | 0.1357 | 0.1030 | 11.453 | 0.9359 | 14.014 | 0.1877 |
| Education (5 to 8 years) | 0.2146 | 0.1341 | 12.394 | 0.9529 | 16.119 | 0.1095 |
| Education (9 or more years) | −0.0093 | 0.1238 | 0.9907 | 0.7773 | 12.626 | 0.9399 |
| Physical activity level (sedentary) | 0.4471 | 0.1039 | 15.638 | 12.757 | 19.171 | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Souza, I.M.B.; Merini, L.R.; Ramos, L.A.V.; Pássaro, A.d.C.; França, J.I.D.; Marques, A.P. Prevalence of Low Back Pain and Associated Factors in Older Adults: Amazonia Brazilian Community Study. Healthcare 2021, 9, 539. https://doi.org/10.3390/healthcare9050539
de Souza IMB, Merini LR, Ramos LAV, Pássaro AdC, França JID, Marques AP. Prevalence of Low Back Pain and Associated Factors in Older Adults: Amazonia Brazilian Community Study. Healthcare. 2021; 9(5):539. https://doi.org/10.3390/healthcare9050539
Chicago/Turabian Stylede Souza, Ingred Merllin Batista, Lilian Regiani Merini, Luiz Armando Vidal Ramos, Anice de Campos Pássaro, João Italo Dias França, and Amélia Pasqual Marques. 2021. "Prevalence of Low Back Pain and Associated Factors in Older Adults: Amazonia Brazilian Community Study" Healthcare 9, no. 5: 539. https://doi.org/10.3390/healthcare9050539
APA Stylede Souza, I. M. B., Merini, L. R., Ramos, L. A. V., Pássaro, A. d. C., França, J. I. D., & Marques, A. P. (2021). Prevalence of Low Back Pain and Associated Factors in Older Adults: Amazonia Brazilian Community Study. Healthcare, 9(5), 539. https://doi.org/10.3390/healthcare9050539






