Abstract
The specific aims of the present study were twofold: (i) to examine the psychometric properties of a Chinese version of the 17-item Benefit Finding Scale (BFS-C), and (ii) to explore the experienced benefits in colorectal cancer (CRC) survivors and their spousal caregivers (SCs). A total of 286 CRC survivors and SCs participated in the investigation, which assessed participant variables of demographic characteristics and benefit finding (BF). Statistical methods applied were confirmatory factor analysis (CFA), Cronbach’s α, Pearson’s correlation, Kappa coefficient, paired t-tests, and one-way ANOVAs. CFA analysis supported a three-factor model for structure validity. All Cronbach’s α for BFS-C was greater than 0.870 in both CRC survivors and SCs. The test–retest correlations at the scale level ranged from good to excellent for CRC survivors (r = 0.752–0.922), and from moderate to good for SCs (r = 0.469–0.654). There were moderate to high correlations between CRC survivors and SCs in all of the paired BFs (all Ps < 0.001, r = 0.332–0.575). This report provided the satisfactory psychometric properties of the BFS-C in such aspects as construct validity, internal, and test–retest reliability among couples coping with CRC in China. Healthcare professionals need to treat couples as a unit and develop dyadic interventions to improve dyadic BF when supporting CRC survivors.
1. Introduction
Evidence shows that colorectal cancer (CRC) is one of the most common cancer types in the world in terms of incidence and mortality [1]. That is the case in China too, where both CRC incidence and mortality rates have demonstrated a progressively growing tendency since 1990 [2]. It has long been recognized that in the context of an exceedingly stressful experience, e.g., the diagnosis of cancer and its management, the unavoidable negative life fluctuations that follow (e.g., depressive and traumatic indications, impaired physical activities, reduced quality of life) [3,4,5] may also be accompanied by positive features [6].
Indeed, research findings have discovered that either cancer survivors or their intimate others experience positive life changes, e.g., intensified self-awareness, adjusted life precedence, and improved family interactions [7,8,9,10,11,12]. Under the circumstance of cancer-related stressful incidents, the positive experiences have been designated using numerous terminologies, including benefit finding (BF), positive effects, and post-traumatic growth [8]. The terminology BF was selected in the current study to describe the positive life experience that follows a CRC identification in CRC survivor–spousal caregiver (SC) couples [13].
Given the growing attention on and increasing acknowledgement of the prominence of BF in the context of cancer investigation, various types of scales assessing BF have been used [14]. However, it has been reported that in a majority of BF instruments, there is a need for further validation of their psychometric properties [14]. Taking the 17-item Benefit Finding Scale (BFS) [15] as an example, despite having served as one of the most frequently used BF measures in a wide variety of cancers, the evidence for its construct validity remains inconsistent [11,13,15,16,17,18,19,20], with either unidimensional [15,16,17] or multidimensional [11,13,18,19,20] models reported. These discrepancies in the 17-item BFS indicate the need to further validate its psychometric properties. Considering the viewpoint that an illness-specific tendency on BF finding exists, that is, findings of BF may not be transferrable across various illnesses, e.g., among different cancer types in the present situation [21], it is essential to examine its psychometric properties under the circumstance of a particular cancer category, e.g., CRC.
Further, evidence corroborates the view that the challenges following a cancer identification and the succeeding related cancer management plan involves the cancer family, e.g., patient–family caregiver dyads, particularly cancer couples, in coping together and supporting one another throughout the entire cancer trajectory [22]. The fact that couples cope with cancer together is increasingly recognized [23,24,25], with diverse types of dyadic relationships, including role alteration, dyadic interaction, and relationship or marriage quality [26,27,28]. Therefore, it is reasonable to conclude that a need exists to explore the related aspects from a dyadic perspective in a cancer context.
To fill in the above illustrated study gaps, the current study was designed to measure and estimate BF from the dyadic perspective of couples coping with CRC together. Based on our previous study [13], which was mainly dedicated to discovering the factor analysis of the Chinese version 17-item BFS (BFS-C) using samples of 772 dyads of mixed cancer (any type of cancer) patients and their family caregivers, the present study is psychometrically a more in-depth data analysis and exploration of the benefits that were experienced using specific examples of CRC survivor–SC dyads. The specific aims were twofold: (i) to examine the psychometric properties of the BFS-C in terms of construct validity, internal, and test–retest reliability, and (ii) to explore the experienced benefits in terms of BF levels and their correlations with sociodemographic variables in CRC survivor–SC dyads.
2. Methods
2.1. Participants and Procedures
Present data are drawn from a study (with details of the participants and procedures) exploring “the dyadic relationship of BF and its impact on quality of life in colorectal cancer survivor and spousal caregiver couples” [29]. Briefly, participants included CRC survivors who suffered from CRC and had completed first-line active treatment, and their partner or spouse: who took care of their spouse with CRC. The targeted sample was confirmed by means of the prerequisite of conducting factor analysis, e.g., confirmatory factor analysis (CFA) in this case, with a recommendation of 200–400 cases in most models [30]. The present analysis only involves the psychometric properties of the BFS-C and the experienced benefits in terms of BF levels and their correlations with the sociodemographic variables in CRC survivor–SC dyads.
After receiving ethical approval from the associated research ethics board (no. HREC201804001), the head nurse of the oncology ward approached eligible couples and invited them to take part in the survey. Once written informed consent was received from the targeted couples, they were advised to finish the survey independently. The investigation was conducted between May 2018 and December 2018 at a hospital in China. To evaluate test–retest reliability, 40 couples were designated for a second assessment (with approximately two to three weeks between the two assessments).
2.2. Assessment Measurements
Assessment measurements included a self-developed demographic questionnaire and the 17-item BFS [15], with the former applied to solicit demographic and health-correlated information, and the latter the BF. The BFS, including 17 items, has been evaluated in populations of cancer patients [11,13,15,16,17,18,19] and family caregivers [11]. For the BFS-C, a previous study has established a three-factor construct validity in dyads of Chinese cancer patients and family caregivers [13].
2.3. Data Analysis
A CFA was conducted on the BFS-C to further approve its previous three-factor model using Amos version 22.0 (IBM, Armonk, New York, USA). Table 1 shows data analysis for psychometric properties, including method applied and related indices and values for adequate model in CFA for construct validity [31], values of Cronbach’s α for estimating internal reliability, correlation coefficient (r), and Kappa for test–retest reliability at the scale and item levels, respectively [32].

Table 1.
Data analysis for psychometric properties.
Paired t-tests were conducted for comparison of CRC survivor scores to SC scores using r as effect size measures for correlations. Cutoff standards relating to the prevalence of the BFS-C at an item level (scoring 4 or 5) were prearranged along with a previous description by Llewellyn et al. [19]. In addition, according to the responses of the scale labels, where “not at all” = 1, “a little” = 2, “moderately” = 3, “quite a bit” = 4, and “extremely” = 5, scoring “1 or 2”,“3”, and “4 or 5” were considered low, moderate, and high levels of BF, respectively. In this way, high levels of BF equal the above cutoff standards of relating to the prevalence of the BFS-C (scoring 4 or 5) [19].
Pearson correlations, t-tests, and one-way ANOVAs were performed to examine the correlations of overall BFS scale level with the sociodemographic variables, e.g., age, gender, education, and working status, in CRC survivors and SCs. The Statistical Package for the Social Sciences, version 22.0 (SPSS, Chicago, Illinois, USA) was employed to conduct data analysis with the exception of CFA, which was conducted using Amos version 22.0.
3. Results
As shown in Table 2, a total of 286 couples had an average age of approximately 60 (ranging from 28–83) years old, with nearly 24 months on average since diagnosis for CRC survivors. The majority of CRC survivors were male (62.6%). Only about 10% of couples (11.9 and 8.7% for CRC survivors and SCs, respectively) had an educational level of a university undergraduate degree or above. Most participants were not working. Thirty-four of the 40 couples completed a second evaluation, which assessed test–retest reliability.

Table 2.
Descriptive statistics of colorectal cancer survivors and spousal caregivers (n = 286).
3.1. Psychometric Properties of the BFS-C
Construct validity: CFA of the BFS-C presented that the three-factor structure fit the data reasonably well, while values of CMIN/DF, RMSEA, SRMR, and CFI equaled 2.742, 0.079, 0.0467, and 0.949, respectively, for CRC survivors, while values of CMIN/DF, RMSEA, SRMR, and CFI for SCs were 2.793, 0.080, 0.0462, and 0.953, respectively. Figure 1 illustrates CFA standardized path coefficients.
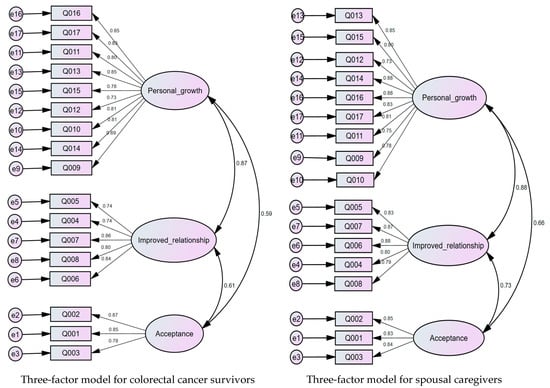
Figure 1.
BFS-C structure model with standardized path coefficients for colorectal cancer survivors and spousal caregivers.
Internal reliability: As shown in Table 3, good to excellent item–factor correlations were identified for both CRC survivors (r = 0.665–0.830, column 2) and SCs (r = 0.724–0.850, column 5). The Cronbach’s α of overall scale and each subscale ranged from 0.870 to 0.951 for CRC survivors (column 3), and from 0.876 to 0.959 for SCs (column 6).

Table 3.
Cronbach’s alphas for each factor and item–factor correlations, test–retest reliability (n = 286).
Test–retest reliability: At the scale level, the test–retest correlations ranged from good to excellent for CRC survivors (r = 0.752–0.922, Table 3: column 4), and from moderate to good for their SCs (r = 0.469–0.654, Table 3: column 7). At the item level, the average Kappa coefficient was 52 and 46% for CRC survivors and SCs, respectively, with most items (15 out of 17 for CRC survivors, and 11 out of 17 for SCs) having a Kappa coefficient greater than 40% (Table 3: columns 4 and 7).
3.2. Experienced Benefits under Cancer Care between CRC Survivors and SCs
As presented in Table 4, at the item level, the percentage of participants reporting a low level of BF ranged from 15.4 to 36.4% in CRC survivors (column 2), and from 13.3 to 35.9% in SCs (column 6). The percentage of participants reporting a moderate BF level ranged from 19.2 to 27.3% in CRC survivors (column 3), and from 17.3 to 24.9% in SCs (column 7). While the high BF level is the same as the endorsement of positive growth in the item level (scoring 4 or 5), the percentage of participants reporting a BFS-C positive growth experience ranged from 43.0 to 63.6% in CRC survivors (column 4), and from 43.5 to 65.3% in SCs (column 8). Overall, SCs experienced higher levels of the BFS-C than CRC survivors, with two exceptions, in items 14 and 15. However, only two statistically significant differences were identified, in items 5 (p < 0.05) and 10 (p < 0.01). Effect size (r) measures for correlations ranged from 0.332 to 0.575 at the item level, and r = 0.612 at the overall scale level.

Table 4.
Percentage of participants reporting growth experience in 17-item level, mean values, paired samples differences, and Pearson correlations between colorectal cancer survivors and spousal caregivers in 17-item Benefit Finding Scale (n = 286).
Further analysis of the correlations of overall BFS level with the sociodemographic variables in CRC survivors and SCs showed that (Table 5) ① BF of CRC survivors was negatively related to CRC survivors age (r = −0.14, p = 0.021, Table 5a), with CRC survivors who were older more likely to report lower levels of BF; ② significant differences in BF (p = 0.001) of CRC survivors in terms of education level, with a trend that CRC survivors with higher education reported higher levels of BF (Table 5a); ③ significant differences in SC BF in terms of the education levels of both CRC survivors (p = 0.035, Table 5a) and SCs (p = 0.005, Table 5b), with a trend that the higher the education level, the higher the BF scores; ④ significant differences in SC BF in terms of SC time spent in caring for the CRC survivors per day (p = 0.010, Table 5b), with a trend that the longer the time spent by the SC in caring for the CRC survivors per day, the higher the BF scores.

Table 5.
Correlations of overall Benefit Finding Scale level with sociodemographic variables in colorectal cancer survivors and spousal caregivers (n = 286).
4. Discussion
The overall objectives of this paper involved examining the psychometric property of the BFS-C and exploring the experienced benefits in CRC survivor–SC dyads. Our findings indicate that the three-factor construct fit the data reasonably well, the BFS-C has good internal consistency, with an overall moderate level of agreement for test–retest reliability. There is also evidence that effect size ® measures exist for correlations ranging from 0.332 to 0.575 at the item level, and r = 0.612 at the overall scale level. Grounded in the study aims and findings, the discussion mainly focuses on the following two aspects: the psychometric properties of the BFS-C and experienced benefits under cancer care between CRC survivors and SCs.
4.1. The Psychometric Properties of the BFS-C
The current CFA analysis further confirms the three-factor structure of the BFS-C [13]. As we had mentioned previously, evidence for the construct validity of the 17-item BFS remains inconsistent, with both unidimensional [15,16,17] and multidimensional [11,13,18,19,20] structures identified in related research. These discrepancies may partly be due to patients coming from different cultural backgrounds, as well as having different contexts for their cancer diagnosis, e.g., a one-factor structure for breast cancer patients in the United States [15], as well as for prostate cancer patients in Australia [16]; a four-factor model for mixed cancer patients in Germany [18]; a five-factor model for breast cancer populations in China [20], and a six-factor model for caregivers of American mixed cancer patients [11]. Accordingly, it is suggested that reporting at the item and/or overall scale levels be applied for the appraisal of patients across various cultural backgrounds and with diverse cancer diagnoses, whereas reporting on the different factor structure levels could be used in an in-depth national analysis.
Evidence from the present sample showed that the BFS-C had good internal consistency (with all Cronbach’s α ≥ 0.870). This good internal consistency of the BFS-C is in line with other reports, either in samples of patients with cancer, as well as in family caregivers (Cronbach’s α = 0.76–0.96) [11,13,15,16,17,18,19,20].
In terms of test–retest reliability, current findings showed a high and moderate level of agreement at the scale level (including the total and subscale scores) and at the item level, respectively, as suggested by Portney and Watkins [32]. The high level of agreement in the total scale level is in line with a report on samples of breast cancer patients [15]. No similar report on test–retest reliability for SCs was identified. Further investigation is required to establish its test–retest reliability in cancer practice.
4.2. Experienced Benefits under Cancer Care between CRC Survivors and SCs
Our findings on CRC survivors experiencing a percentage of positive growth (BF in this case) on 17 item levels (ranging from 43.0 to 63.6%) are somewhat in line with another study, in that cancer patients reported a percentage range of positive growth, from 33 to 85%. SCs in the present sample reported similar rates of positive growth (ranging from 43.5 to 65.3%) as CRC survivors. Although no similar report was identified for SCs of cancer survivors, the above findings of couples experiencing positive growth are in line with our previous findings on cancer patient–caregiver dyads [33].
Interestingly, both CRC survivors and their SCs reported their lowest and highest BF experience in the same items, i.e., item 12 and item 4, respectively, see Table 4). This may be a reminder that coping with the disease brought families closer together and improved their relationships. On the other hand, more attention also needs to be given to social support, e.g., support from friends, neighbors, and the surrounding community [10,11,12,27,28,29].
Further comparisons on the mean value of paired differences between CRC survivor and SC couples found that SCs experienced greater levels of BF in items 5 and 10 than CRC survivors did. This may be due to the demands of the caregiver role in caring for loved ones with cancer, e.g., physical (symptom management), mental (emotional), social (their family), as well as financial [34].
Findings that older CRC survivors were more likely to report lower levels of BF is a reminder that more attention should be given to elderly CRC survivors populations. Findings that CRC survivors with higher education reported higher levels of BF is consistent with the findings of another study, in that greater educational achievement was found to have a protective effect on BF [19]. It is assumed that CRC survivors who had received higher education can easily comprehend the disease and its treatment, which could facilitate their coping process and increase the benefits they experience. However, a different finding was reported by Jansen et al. [7], in that CRC survivors with higher education levels were associated with less BF. These inconsistent findings on the association between education levels and BF require future verification.
In addition, no similar report was identified regarding the associations of BF in SCs with other variables, e.g., education levels of both CRC survivors and SCs, time spent by SCs in caring for CRC survivors per day. This is a reminder that more attention should be paid to SCs with lower education levels, who spent a shorter time caring for a CRC survivor per day. It is suggested that special support be provided to couples with lower education levels.
In the Chinese culture, due to the Confucian ideal of filial piety, caregiving is considered an essential and integral element of family life [35]. SCs of cancer patients would sacrifice their own health to take care of their loved one with cancer [36]. In addition, the dual aspect of mutual “protection” in couples coping with cancer [36] further increases the caregiving burden. A previous qualitative study on Chinese couples coping with CRC also showed that while providing support to one another, couples must manage various challenges, e.g., insufficient communication, lack of knowledge, role conflict, and financial burden. The couples stated that receiving help or support from healthcare professionals would facilitate their journey of coping with CRC together and providing mutual support to one another [28]. Thus, it is of paramount importance for healthcare professionals to provide support to couples in their journey of coping with cancer together, and to encourage them to experience the benefits of the journey, while also confronting the challenges.
4.3. Limitations
As this study includes only Chinese couples dealing with CRC, which can be viewed as a very selective sample, its findings should be generalized only with the utmost caution to CRC patients from other cultural backgrounds and cancer diagnoses other than CRC. Further exploration, targeting populations coping with diverse cancer types in different cultures, should be conducted. Moreover, although the extracted sample size was confirmed by the prerequisite to conduct factor analysis, the second survey’s small sample size for assessing test–retest reliability may act as another study limitation. Further evaluation using an adequate sample size is required. In addition, the majority prevalence of males versus females in this study could have influenced the results. Future study on a balanced gender population is needed. Another limitation could be that it is necessary to study the concurrent validity with other tests assessing BF or personal growth.
5. Conclusions
The current findings not only confirm the three-factor construct validity of the BFS-C, but also offer the acceptable psychometric properties of the BFS-C in Chinese CRC survivor and SC couples. Considering the BF psychological properties, it is suggested that while adopting this instrument in clinical practice, it would be beneficial to apply other possible instruments and understand the possible correlations with other psychological wellbeing surveys. In addition, the findings also demonstrate that a dyadic BF relationship in couples coping with CRC may exist. Further intervention studies on improving dyadic BF in couples coping with CRC are highly recommended, particularly for those with low or moderate BF levels and lower education levels.
Author Contributions
M.C.: study conception/design, data collection/analysis, drafting of manuscript; J.G., J.L., X.L.: data collection/analysis, drafting of manuscript; Q.L.: data collection/analysis, drafting of manuscript, critical manuscript revisions. All authors have read and agreed to the published version of the manuscript.
Funding
Financial support for this study was provided by the National Natural Science Foundation of China (no. 81773297). The funders had no role in study design, data collection and analysis, decision to publish, or manuscript preparation.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of Jiangnan University (No. HREC20184001).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
We (the authors) have full control of all primary data and agree to allow the journal to review the data if requested.
Acknowledgments
The authors gratefully acknowledge the support of the related hospital and all participants for sharing their experience in this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A. Jemal A Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Zhang, L.; Cao, F.; Zhang, G.; Shi, L.; Chen, S.; Zhang, Z.; Zhi, W.; Ma, T. Trends in and Predictions of Colorectal Cancer Incidence and Mortality in China From 1990 to 2025. Front. Oncol. 2019, 9, 98. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Loke, A.Y. A spectrum of hidden morbidities among spousal caregivers for patients with cancer, and differences between the genders: A review of the literature. J. Eur. Oncol. Nurs. Soc. 2013, 17, 578–587. [Google Scholar] [CrossRef]
- Kim, Y.; Carver, C.S.; Shaffer, K.M.; Gansler, T.; Cannady, R.S. Cancer caregiving predicts physical impairments: Roles of earlier caregiving stress and being a spousal caregiver. Cancer 2015, 121, 302–310. [Google Scholar] [CrossRef] [PubMed]
- Graça Pereira, M.; Figueiredo, A.P.; Fincham, F.D. Anxiety, depression, traumatic stress and quality of life in colorectal cancer after different treatments: A study with Portuguese patients and their partners. Eur. J. Oncol. Nurs. 2012, 16, 227–232. [Google Scholar] [CrossRef]
- Folkman, S. Positive psychological states and coping with severe stress. Soc. Sci. Med. 1997, 45, 1207–1221. [Google Scholar] [CrossRef]
- Jansen, L.; Hoffmeister, M.; Chang-Claude, J.; Brenner, H.; Arndt, V. Benefit finding and post-traumatic growth in long-term colorectal cancer survivors: Prevalence, determinants, and associations with quality of life. Br. J. Cancer 2011, 105, 1158–1165. [Google Scholar] [CrossRef]
- Coyne, J.C.; Tennen, H.; Ranchor, A.V. Positive psychology in cancer care: A story line resistant to evidence. Ann. Behav. Med. 2010, 39, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Rinaldis, M.; Pakenham, K.I.; Lynch, B.M. Relationships between quality of life and finding benefits in a diagnosis of colorectal cancer. Br. J. Psychol. 1953, 101 Pt 2, 259–275. [Google Scholar] [CrossRef]
- Li, Q.; Loke, A.Y. The positive aspects of caregiving for cancer patients: A critical review of the literature and directions for future research. Psycho Oncol. 2013, 22, 2399–2407. [Google Scholar] [CrossRef]
- Kim, Y.; Schulz, R.; Carver, C.S. Benefit-finding in the cancer caregiving experience. Psychosom. Med. 2007, 69, 283–291. [Google Scholar] [CrossRef]
- Mosher, C.E.; Adams, R.N.; Helft, P.R.; O’Neil, B.H.; Shahda, S.; Rattray, N.A.; Champion, V.L. Positive changes among patients with advanced colorectal cancer and their family caregivers: A qualitative analysis. Psychol. Health 2017, 32, 94–109. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Lin, Y.; Xu, Y.; Zhou, H.; Yang, L.; Xu, Y. Construct validity of the 17-item Benefit Finding Scale in Chinese cancer patients and their family caregivers: A cross-sectional study. Supportive Care Cancer 2017, 25, 2387–2397. [Google Scholar] [CrossRef] [PubMed]
- Pascoe, L.; Edvardsson, D. Benefit finding in adult cancer populations: Psychometric properties and performance of existing instruments. Eur. J. Oncol. Nurs. 2014, 18, 484–491. [Google Scholar] [CrossRef] [PubMed]
- Antoni, M.H.; Lehman, J.M.; Kilbourn, K.M.; Boyers, A.E.; Culver, J.L.; Alferi, S.M.; Yount, S.E.; McGregor, B.A.; Arena, P.L.; Harris, S.D.; et al. Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychol. 2001, 20, 20–32. [Google Scholar] [CrossRef]
- Pascoe, L.; Edvardsson, D. Psychometric properties and performance of the 17-item Benefit Finding Scale (BFS) in an outpatient population of men with prostate cancer. Eur. J. Oncol. Nurs. 2015, 19, 169–173. [Google Scholar] [CrossRef]
- Urcuyo, K.R.; Boyers, A.E.; Carver, C.S.; Antoni, M.H. Finding benefit in breast cancer: Relations with personality, coping, and concurrent well-being. Psychol. Health 2005, 20, 175–192. [Google Scholar] [CrossRef]
- Luszczynska, A.; Mohamed, N.E.; Schwarzer, R. Self-efficacy and social support predict benefit finding 12 months after cancer surgery: The mediating role of coping strategies. Psychol. Health Med. 2005, 10, 365–375. [Google Scholar] [CrossRef]
- Llewellyn, C.D.; Horney, D.J.; McGurk, M.; Weinman, J.; Herold, J.; Altman, K.; Smith, H.E. Assessing the psychological predictors of benefit finding in patients with head and neck cancer. Psycho Oncol. 2013, 22, 97–105. [Google Scholar] [CrossRef]
- Wang, Y.; Li, L.Y.; Cai, L.; Chen, G.; Tang, L.; Zhu, X. Reliability and Validity of the Benefit Finding Scale in Women with Breast Cancer. Chin. J. Clin. Psychol. 2013, 21, 410–412. [Google Scholar]
- Barskova, T.; Oesterreich, R. Post-traumatic growth in people living with a serious medical condition and its relations to physical and mental health: A systematic review. Disabil. Rehabil. 2009, 31, 1709–1733. [Google Scholar] [CrossRef]
- Kayser, K.; Watson, L.E.; Andrade, J.T. Cancer as a “we-disease”: Examining the process of coping from a relational perspective. Fam. Syst. Health 2007, 25, 404–418. [Google Scholar] [CrossRef]
- Hagedoorn, M.; Sanderman, R.; Bolks, H.N.; Tuinstra, J.; Coyne, J.C. Distress in couples coping with cancer: A meta-analysis and critical review of role and gender effects. Psychol. Bull. 2008, 134, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Traa, M.J.; De Vries, J.; Bodenmann, G.; Den Oudsten, B.L. Dyadic coping and relationship functioning in couples coping with cancer: A systematic review. Br. J. Health Psychol. 2015, 20, 85–114. [Google Scholar] [CrossRef] [PubMed]
- Regan, T.W.; Lambert, S.D.; Girgis, A.; Kelly, B.; Kayser, K.; Turner, J. Do couple-based interventions make a difference for couples affected by cancer? A systematic review. BMC Cancer 2012, 12, 279. [Google Scholar] [CrossRef] [PubMed]
- Northouse, L.L.; Mood, D.; Templin, T.; Mellon, S.; George, T. Couples’ patterns of adjustment to colon cancer. Soc. Sci. Med. 2000, 50, 271–284. [Google Scholar] [CrossRef]
- Kayser, K.; Acquati, C.; Reese, J.B.; Mark, K.; Wittmann, D.; Karam, E. A systematic review of dyadic studies examining relationship quality in couples facing colorectal cancer together. Psycho Oncol. 2018, 27, 13–21. [Google Scholar] [CrossRef]
- Li, Q.; Lin, Y.; Chen, Y.; Loke, A.Y. Mutual Support and Challenges Among Chinese Couples Living With Colorectal Cancer: A Qualitative Study. Cancer Nurs. 2018, 41, E50–E60. [Google Scholar] [CrossRef]
- Lin, Y.; Luo, X.; Li, J.; Xu, Y.; Li, Q. The dyadic relationship of benefit finding and its impact on quality of life in colorectal cancer survivor and spousal caregiver couples. Supportive Care Cancer 2021, 29, 1477–1486. [Google Scholar] [CrossRef]
- Hoyle, R.H. Structural equation modeling for social and personality psychology. In Sage Library of Methods in Social & Personality Psychology, 1st ed.; SAGE Publications Ltd.: London, UK, 2011. [Google Scholar]
- Hooper, D.; Coughlan, J.; Mullen, M.R. Structural Equation Modeling: Guidelines for Determining Model Fit. Electron. J. Bus. Res. Methods 2008, 6, 53–60. [Google Scholar]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice, 3rd ed.; Pearson Hall: London, UK, 2009. [Google Scholar]
- Li, Q.; Lin, Y.; Zhou, H.; Xu, Y.; Yang, L.; Xu, Y. Factors moderating the mutual impact of benefit finding between Chinese patients with cancer and their family caregivers: A cross-sectional study. Psycho Oncol. 2018, 27, 2363–2373. [Google Scholar] [CrossRef] [PubMed]
- Given, B.A.; Given, C.W.; Kozachik, S. Family Support in Advanced Cancer. CA Cancer J. Clin. 2001, 51, 213–231. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.S.; Hung, L.C. The influence of eastern philosophy on elder care by Chinese Americans: Attitudes toward long-term care. J. Transcult. Nurs. 2012, 23, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Chiang, V.C.; Xu, X.; Xu, Y.; Loke, A.Y. The Experiences of Chinese Couples Living With Cancer: A Focus Group Study. Cancer Nurs. 2015, 38, 383–394. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).