The Potential Impact of Selected Bacterial Strains on the Stress Response
Abstract
1. Introduction
2. Theoretical Background
2.1. Stress Response
2.2. Intestinal Microbiome and Microbiota
2.3. Pro- Pre- and Psychobiotics
2.4. Microbiome–Gut–Brain Axis
3. State of Research
4. Method
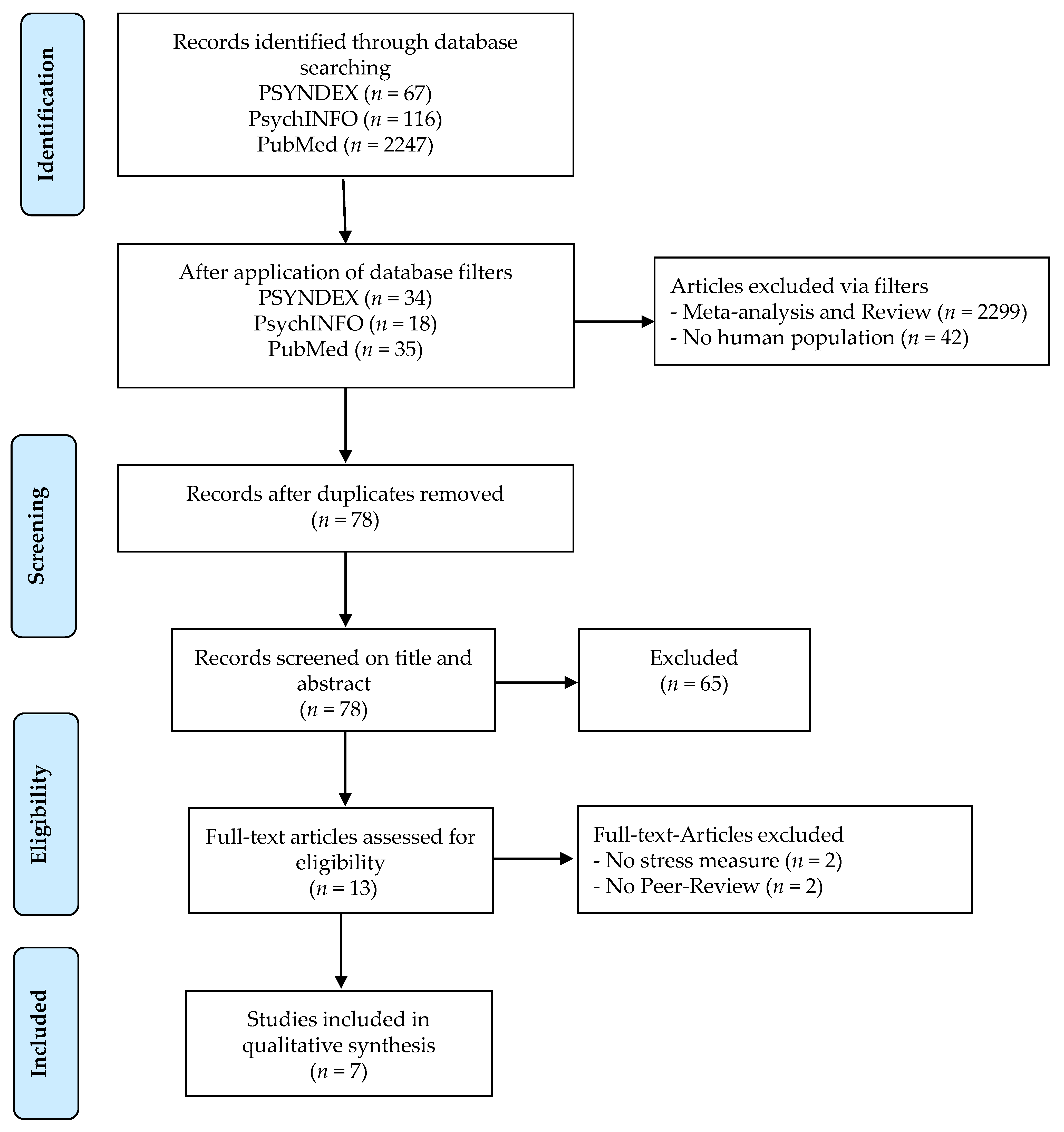
4.1. Identifiying Relevant Studies
4.1.1. Systematic Literature Search
4.1.2. Eligibility Criteria
4.2. Study Selection
Data Extraction
5. Results
5.1. Interventions and Impact on the Stress Response
5.2. Stressors and Survey of the Variable Stress
5.3. Sample Characteristics
“However, in the judgment of the author, for most behavioral science research (although admitting of many exceptions), power values as large as 0.90–0.99 would demand sample sizes so large as to exceed an investigator’s resources. […] The view offered here is that often, the behavioral scientist will decide that Type I errors, which result in false positive claims, are more serious and therefore to be more stringently guarded against than Type II errors, which result in false negative claims. The notion that failure to find is less serious than finding something that is not there accords with the conventional scientific view. It is proposed here as a convention that, when the investigator has no other basis for setting the desired power value, the value 0.80 be used. […] This 0.80 desired power convention is offered with the hope that it will be ignored whenever an investigator can find a basis in his substantive concerns in his specific research investigation to choose a value ad hoc.”[66], pp. 55–56.
5.4. Further Results
6. Discussion
6.1. Interventions and Effects on the Stress Response
6.2. Stressors and the Survey of the Variable Stress
6.3. Sample Characteristics
7. Limitations
8. Conclusion and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Hamer, M.; Endrighi, R.; Venuraju, S.M.; Lahiri, A.; Steptoe, A. Cortisol Responses to Mental Stress and the Progression of Coronary Artery Calcification in Healthy Men and Women. PLoS ONE 2012, 7, e31356. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Smith, M.; Lutgendorf, S.K.; Sood, A.K. Impact of Stress on Cancer Metastasis. Future Oncol. 2010, 6, 1863–1881. [Google Scholar] [CrossRef] [PubMed]
- Steptoe, A.; Kivimäki, M. Stress and Cardiovascular Disease: An Update on Current Knowledge. Annu. Rev. Public Health 2013, 34, 337–354. [Google Scholar] [CrossRef] [PubMed]
- Hyman, S.E. Revolution Stalled. Sci. Transl. Med. 2012, 4, 155cm11. [Google Scholar] [CrossRef]
- Insel, T.R. The NIMH Experimental Medicine Initiative. World Psychiatry 2015, 14, 151–153. [Google Scholar] [CrossRef]
- Dinan, T.G.; Cryan, J.F. Regulation of the Stress Response by the Gut Microbiota: Implications for Psychoneuroendocrinology. Psychoneuroendocrinology 2012, 37, 1369–1378. [Google Scholar] [CrossRef]
- Liang, S.; Wang, T.; Hu, X.; Luo, J.; Li, W.; Wu, X.; Duan, Y.; Jin, F. Administration of Lactobacillus Helveticus NS8 Improves Behavioral, Cognitive, and Biochemical Aberrations Caused by Chronic Restraint Stress. Neuroscience 2015, 310, 561–577. [Google Scholar] [CrossRef]
- Sudo, N. Microbiome, HPA Axis and Production of Endocrine Hormones in the Gut. In Microbial Endocrinology: The Microbiota-Gut-Brain Axis in Health and Disease; Lyte, M., Cryan, J.F., Eds.; Springer: New York, NY, USA, 2014; Volume 817, pp. 177–194. ISBN 978-1-4939-0896-7. [Google Scholar]
- Turnbaugh, P.J.; Ley, R.E.; Hamady, M.; Fraser-Liggett, C.M.; Knight, R.; Gordon, J.I. The Human Microbiome Project. Nature 2007, 449, 804–810. [Google Scholar] [CrossRef]
- Montiel-Castro, A.J.; González-Cervantes, R.M.; Bravo-Ruiseco, G.; Pacheco-López, G. The Microbiota-Gut-Brain Axis: Neurobehavioral Correlates, Health and Sociality. Front. Integr. Neurosci. 2013, 7. [Google Scholar] [CrossRef]
- Liang, S.; Wang, T.; Hu, X.; Li, W.; Jin, F.; Wang, L. Microorganism and Behavior and Psychiatric Disorders: Microorganism and Behavior and Psychiatric Disorders. Adv. Psychol. Sci. 2013, 20, 75–97. [Google Scholar] [CrossRef]
- Rhee, S.H.; Pothoulakis, C.; Mayer, E.A. Principles and Clinical Implications of the Brain–Gut–Enteric Microbiota Axis. Nat. Rev. Gastroenterol. Hepatol. 2009, 6, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Bharwani, A.; Mian, M.F.; Foster, J.A.; Surette, M.G.; Bienenstock, J.; Forsythe, P. Structural & Functional Consequences of Chronic Psychosocial Stress on the Microbiome & Host. Psychoneuroendocrinology 2016, 63, 217–227. [Google Scholar] [CrossRef] [PubMed]
- Dinan, T.G.; Stanton, C.; Cryan, J.F. Psychobiotics: A Novel Class of Psychotropic. Biol. Psychiatry 2013, 74, 720–726. [Google Scholar] [CrossRef] [PubMed]
- De Vrese, M.; Schrezenmeir, J. Probiotics, Prebiotics, and Synbiotics. In Food Biotechnology; Stahl, U., Donalies, U.E.B., Nevoigt, E., Eds.; Advances in Biochemical Engineering/Biotechnology; Springer: Berlin/Heidelberg, Germany, 2008; Volume 111, pp. 1–66. ISBN 978-3-540-70535-2. [Google Scholar]
- Reber, S.O. Stress and Animal Models of Inflammatory Bowel Disease—An Update on the Role of the Hypothalamo–Pituitary–Adrenal Axis. Psychoneuroendocrinology 2012, 37, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Tlaskalová-Hogenová, H.; Tucková, L.; Stepánková, R.; Hudcovic, T.; Palová-Jelínková, L.; Kozáková, H.; Rossmann, P.; Sanchez, D.; Cinová, J.; Hrnčíř, T.; et al. Involvement of Innate Immunity in the Development of Inflammatory and Autoimmune Diseases. Ann. N. Y. Acad. Sci. 2005, 1051, 787–798. [Google Scholar] [CrossRef]
- Ulrich-Lai, Y.M.; Herman, J.P. Neural Regulation of Endocrine and Autonomic Stress Responses. Nat. Rev. Neurosci. 2009, 10, 397–409. [Google Scholar] [CrossRef]
- Sapolsky, R.M. Stress Hormones: Good and Bad. Neurobiol. Dis. 2000, 7, 540–542. [Google Scholar] [CrossRef]
- Chrousos, G.P.; Gold, P.W. The Concepts of Stress and Stress System Disorders. Overview of Physical and Behavioral Homeostasis. JAMA 1992, 267, 1244–1252. [Google Scholar] [CrossRef]
- Chrousos, G. The Role of Stress and the Hypothalamic–Pituitary–Adrenal Axis in the Pathogenesis of the Metabolic Syndrome: Neuro-Endocrine and Target Tissue-Related Causes. Int. J. Obes. 2000, 24, S50–S55. [Google Scholar] [CrossRef]
- Chrousos, G.P.; Kino, T. Glucocorticoid Action Networks and Complex Psychiatric and/or Somatic Disorders. Stress 2007, 10, 213–219. [Google Scholar] [CrossRef]
- Gold, P.W.; Calabkese, J.R.; Kling, M.A.; Avgerinos, P.; Khan, I.; Gallucci, W.T.; Tomai, T.P.; Chrousos, G.P. Abnormal Acth and Cortisol Responses to Ovine Corticotropin Releasing Factor in Patients with Primary Affective Disorder. Prog. Neuropsychopharmacol. Biol. Psychiatry 1986, 10, 57–65. [Google Scholar] [CrossRef]
- Cryan, J.F.; O’Mahony, S.M. The Microbiome-Gut-Brain Axis: From Bowel to Behavior: From Bowel to Behavior. Neurogastroenterol. Motil. 2011, 23, 187–192. [Google Scholar] [CrossRef]
- Jacobson, L.; Sapolsky, R. The Role of the Hippocampus in Feedback Regulation of the Hypothalamic-Pituitary-Adrenocortical Axis*. Endocr. Rev. 1991, 12, 118–134. [Google Scholar] [CrossRef]
- Valdes, A.M.; Walter, J.; Segal, E.; Spector, T.D. Role of the Gut Microbiota in Nutrition and Health. BMJ 2018, k2179. [Google Scholar] [CrossRef]
- Qin, J.; Raes, J.; Arumugam, M.; Burgdorf, K.S.; Manichanh, C.; Nielsen, T.; Pons, N.; Levenez, F.; Yamada, T.; Mende, D.R.; et al. A Human Gut Microbial Gene Catalogue Established by Metagenomic Sequencing. Nature 2010, 464, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Ley, R.E.; Turnbaugh, P.J.; Klein, S.; Gordon, J.I. Microbial Ecology: Human Gut Microbes Associated with Obesity. Nature 2006, 444, 1022–1023. [Google Scholar] [CrossRef] [PubMed]
- Rupnik, M. Toward a True Bacteriotherapy for Clostridium Difficile Infection. N. Engl. J. Med. 2015, 372, 1566–1568. [Google Scholar] [CrossRef] [PubMed]
- The Human Microbiome Project Consortium Structure, Function and Diversity of the Healthy Human Microbiome. Nature 2012, 486, 207–214. [CrossRef] [PubMed]
- Braune, A. Für gesundes Gedeihen! Aktuelle Ernährungsmedizin 2012, 37, S7–S10. [Google Scholar] [CrossRef]
- Turroni, F.; Ribbera, A.; Foroni, E.; van Sinderen, D.; Ventura, M. Human Gut Microbiota and Bifidobacteria: From Composition to Functionality. Antonie Van Leeuwenhoek 2008, 94, 35–50. [Google Scholar] [CrossRef]
- Ngo, N.; Choucair, K.; Creeden, J.F.; Qaqish, H.; Bhavsar, K.; Murphy, C.; Lian, K.; Albrethsen, M.T.; Stanbery, L.; Phinney, R.C.; et al. Bifidobacterium Spp: The Promising Trojan Horse in the Era of Precision Oncology. Future Oncol. 2019, 15, 3861–3876. [Google Scholar] [CrossRef] [PubMed]
- Zacharof, M.-P.; Lovitt, R.B.; Ratanapongleka, K. The Importance of Lactobacilli in Contemporary Food and Pharmaceutical Industry A Review Article. In Proceedings of the 2010 International Conference on Chemical Engineering and Applications (CCEA 2010), Singapore, 26–28 February 2010. [Google Scholar]
- Sarkar, A.; Lehto, S.M.; Harty, S.; Dinan, T.G.; Cryan, J.F.; Burnet, P.W.J. Psychobiotics and the Manipulation of Bacteria–Gut–Brain Signals. Trends Neurosci. 2016, 39, 763–781. [Google Scholar] [CrossRef] [PubMed]
- O’Mahony, S.M.; Hyland, N.P.; Dinan, T.G.; Cryan, J.F. Maternal Separation as a Model of Brain–Gut Axis Dysfunction. Psychopharmacology 2011, 214, 71–88. [Google Scholar] [CrossRef] [PubMed]
- Tanida, M.; Imanishi, K.; Akashi, H.; Kurata, Y.; Chonan, O.; Naito, E.; Kunihiro, S.; Kawai, M.; Kato-kataoka, A.; Shibamoto, T. Injection of Lactobacillus Casei Strain Shirota Affects Autonomic Nerve Activities in a Tissue-Specific Manner, and Regulates Glucose and Lipid Metabolism in Rats. J. Diabetes Investig. 2014, 5, 153–161. [Google Scholar] [CrossRef]
- Takada, M.; Nishida, K.; Kataoka-Kato, A.; Gondo, Y.; Ishikawa, H.; Suda, K.; Kawai, M.; Hoshi, R.; Watanabe, O.; Igarashi, T.; et al. Probiotic Lactobacillus Casei Strain Shirota Relieves Stress-Associated Symptoms by Modulating the Gut-Brain Interaction in Human and Animal Models. Neurogastroenterol. Motil. 2016, 28, 1027–1036. [Google Scholar] [CrossRef]
- Bravo, J.A.; Forsythe, P.; Chew, M.V.; Escaravage, E.; Savignac, H.M.; Dinan, T.G.; Bienenstock, J.; Cryan, J.F. Ingestion of Lactobacillus Strain Regulates Emotional Behavior and Central GABA Receptor Expression in a Mouse via the Vagus Nerve. Proc. Natl. Acad. Sci. USA 2011, 108, 16050–16055. [Google Scholar] [CrossRef]
- Clarke, G.; Grenham, S.; Scully, P.; Fitzgerald, P.; Moloney, R.D.; Shanahan, F.; Dinan, T.G.; Cryan, J.F. The Microbiome-Gut-Brain Axis during Early Life Regulates the Hippocampal Serotonergic System in a Sex-Dependent Manner. Mol. Psychiatry 2013, 18, 666–673. [Google Scholar] [CrossRef]
- Desbonnet, L.; Garrett, L.; Clarke, G.; Bienenstock, J.; Dinan, T.G. The Probiotic Bifidobacteria Infantis: An Assessment of Potential Antidepressant Properties in the Rat. J. Psychiatr. Res. 2008, 43, 164–174. [Google Scholar] [CrossRef]
- O’Mahony, S.M.; Marchesi, J.R.; Scully, P.; Codling, C.; Ceolho, A.-M.; Quigley, E.M.M.; Cryan, J.F.; Dinan, T.G. Early Life Stress Alters Behavior, Immunity, and Microbiota in Rats: Implications for Irritable Bowel Syndrome and Psychiatric Illnesses. Biol. Psychiatry 2009, 65, 263–267. [Google Scholar] [CrossRef]
- Bailey, M.T.; Dowd, S.E.; Galley, J.D.; Hufnagle, A.R.; Allen, R.G.; Lyte, M. Exposure to a Social Stressor Alters the Structure of the Intestinal Microbiota: Implications for Stressor-Induced Immunomodulation. Brain. Behav. Immun. 2011, 25, 397–407. [Google Scholar] [CrossRef]
- Barouei, J.; Moussavi, M.; Hodgson, D.M. Effect of Maternal Probiotic Intervention on HPA Axis, Immunity and Gut Microbiota in a Rat Model of Irritable Bowel Syndrome. PLoS ONE 2012, 7, e46051. [Google Scholar] [CrossRef]
- Bailey, M.T.; Coe, C.L. Maternal Separation Disrupts the Integrity of the Intestinal Microflora in Infant Rhesus Monkeys. Dev. Psychobiol. 1999, 35, 146–155. [Google Scholar] [CrossRef]
- Desbonnet, L.; Clarke, G.; Shanahan, F.; Dinan, T.G.; Cryan, J.F. Microbiota Is Essential for Social Development in the Mouse. Mol. Psychiatry 2014, 19, 146–148. [Google Scholar] [CrossRef] [PubMed]
- Hoban, A.E.; Stilling, R.M.; Ryan, F.J.; Shanahan, F.; Dinan, T.G.; Claesson, M.J.; Clarke, G.; Cryan, J.F. Regulation of Prefrontal Cortex Myelination by the Microbiota. Transl. Psychiatry 2016, 6, e774. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.L.A.; Vieira-Silva, S.; Liston, A.; Raes, J. How Informative Is the Mouse for Human Gut Microbiota Research? Dis. Model. Mech. 2015, 8, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Ogbonnaya, E.S.; Clarke, G.; Shanahan, F.; Dinan, T.G.; Cryan, J.F.; O’Leary, O.F. Adult Hippocampal Neurogenesis Is Regulated by the Microbiome. Biol. Psychiatry 2015, 78, e7–e9. [Google Scholar] [CrossRef] [PubMed]
- Gareau, M.G.; Jury, J.; MacQueen, G.; Sherman, P.M.; Perdue, M.H. Probiotic Treatment of Rat Pups Normalises Corticosterone Release and Ameliorates Colonic Dysfunction Induced by Maternal Separation. Gut 2007, 56, 1522–1528. [Google Scholar] [CrossRef] [PubMed]
- Sudo, N.; Chida, Y.; Aiba, Y.; Sonoda, J.; Oyama, N.; Yu, X.-N.; Kubo, C.; Koga, Y. Postnatal Microbial Colonization Programs the Hypothalamic-Pituitary-Adrenal System for Stress Response in Mice: Commensal Microbiota and Stress Response. J. Physiol. 2004, 558, 263–275. [Google Scholar] [CrossRef] [PubMed]
- Golubeva, A.V.; Crampton, S.; Desbonnet, L.; Edge, D.; O’Sullivan, O.; Lomasney, K.W.; Zhdanov, A.V.; Crispie, F.; Moloney, R.D.; Borre, Y.E.; et al. Prenatal Stress-Induced Alterations in Major Physiological Systems Correlate with Gut Microbiota Composition in Adulthood. Psychoneuroendocrinology 2015, 60, 58–74. [Google Scholar] [CrossRef]
- Savignac, H.M.; Kiely, B.; Dinan, T.G.; Cryan, J.F. Bifidobacteria Exert Strain-Specific Effects on Stress-Related Behavior and Physiology in BALB/c Mice. Neurogastroenterol. Motil. 2014, 26, 1615–1627. [Google Scholar] [CrossRef]
- Zareie, M.; Johnson-Henry, K.; Jury, J.; Yang, P.-C.; Ngan, B.-Y.; McKay, D.M.; Soderholm, J.D.; Perdue, M.H.; Sherman, P.M. Probiotics Prevent Bacterial Translocation and Improve Intestinal Barrier Function in Rats Following Chronic Psychological Stress. Gut 2006, 55, 1553–1560. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping Studies: Towards a Methodological Framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983, 24, 385. [Google Scholar] [CrossRef] [PubMed]
- Daudt, H.M.; van Mossel, C.; Scott, S.J. Enhancing the Scoping Study Methodology: A Large, Inter-Professional Team’s Experience with Arksey and O’Malley’s Framework. BMC Med. Res. Methodol. 2013, 13, 48. [Google Scholar] [CrossRef] [PubMed]
- Allen, A.P.; Hutch, W.; Borre, Y.E.; Kennedy, P.J.; Temko, A.; Boylan, G.; Murphy, E.; Cryan, J.F.; Dinan, T.G.; Clarke, G. Bifidobacterium Longum 1714 as a Translational Psychobiotic: Modulation of Stress, Electrophysiology and Neurocognition in Healthy Volunteers. Transl. Psychiatry 2016, 6, e939. [Google Scholar] [CrossRef] [PubMed]
- Kato-Kataoka, A.; Nishida, K.; Takada, M.; Kawai, M.; Kikuchi-Hayakawa, H.; Suda, K.; Ishikawa, H.; Gondo, Y.; Shimizu, K.; Matsuki, T.; et al. Fermented Milk Containing Lactobacillus Casei Strain Shirota Preserves the Diversity of the Gut Microbiota and Relieves Abdominal Dysfunction in Healthy Medical Students Exposed to Academic Stress. Appl. Environ. Microbiol. 2016, 82, 3649–3658. [Google Scholar] [CrossRef]
- Kelly, J.R.; Allen, A.P.; Temko, A.; Hutch, W.; Kennedy, P.J.; Farid, N.; Murphy, E.; Boylan, G.; Bienenstock, J.; Cryan, J.F.; et al. Lost in Translation? The Potential Psychobiotic Lactobacillus Rhamnosus (JB-1) Fails to Modulate Stress or Cognitive Performance in Healthy Male Subjects. Brain. Behav. Immun. 2017, 61, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Messaoudi, M.; Lalonde, R.; Violle, N.; Javelot, H.; Desor, D.; Nejdi, A.; Bisson, J.-F.; Rougeot, C.; Pichelin, M.; Cazaubiel, M.; et al. Assessment of Psychotropic-like Properties of a Probiotic Formulation ( Lactobacillus Helveticus R0052 and Bifidobacterium Longum R0175) in Rats and Human Subjects. Br. J. Nutr. 2011, 105, 755–764. [Google Scholar] [CrossRef]
- Möller, C.M.; Olsa, E.J.A.; Ginty, A.T.; Rapelje, A.L.; Tindall, C.L.; Holesh, L.A.; Petersen, K.L.; Conklin, S.M. Influence of Acute Multispecies and Multistrain Probiotic Supplementation on Cardiovascular Function and Reactivity to Psychological Stress in Young Adults: A Double-Blind, Randomized, Placebo-Controlled Trial. Psychosom. Med. 2017, 79, 914–919. [Google Scholar] [CrossRef]
- Schmidt, K.; Cowen, P.J.; Harmer, C.J.; Tzortzis, G.; Errington, S.; Burnet, P.W.J. Prebiotic Intake Reduces the Waking Cortisol Response and Alters Emotional Bias in Healthy Volunteers. Psychopharmacology 2015, 232, 1793–1801. [Google Scholar] [CrossRef]
- Montero-López, E.; Santos-Ruiz, A.; García-Ríos, M.C.; Rodríguez-Blázquez, M.; Rogers, H.L.; Peralta-Ramírez, M.I. The Relationship between the Menstrual Cycle and Cortisol Secretion: Daily and Stress-Invoked Cortisol Patterns. Int. J. Psychophysiol. 2018, 131, 67–72. [Google Scholar] [CrossRef]
- Di Stefano, J. How Much Power Is Enough? Against the Development of an Arbitrary Convention for Statistical Power Calculations. Forum. Funct. Ecol. 2003, 17, 707–709. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; L. Erlbaum Associates: Hillsdale, NJ, USA, 1988; ISBN 978-0-8058-0283-2. [Google Scholar]
- Tillisch, K.; Labus, J.; Kilpatrick, L.; Jiang, Z.; Stains, J.; Ebrat, B.; Guyonnet, D.; Legrain–Raspaud, S.; Trotin, B.; Naliboff, B.; et al. Consumption of Fermented Milk Product With Probiotic Modulates Brain Activity. Gastroenterology 2013, 144, 1394–1401. [Google Scholar] [CrossRef]
- Steenbergen, L.; Sellaro, R.; van Hemert, S.; Bosch, J.A.; Colzato, L.S. A Randomized Controlled Trial to Test the Effect of Multispecies Probiotics on Cognitive Reactivity to Sad Mood. Brain. Behav. Immun. 2015, 48, 258–264. [Google Scholar] [CrossRef]
- Romijn, A.R.; Rucklidge, J.J. Systematic Review of Evidence to Support the Theory of Psychobiotics. Nutr. Rev. 2015, 73, 675–693. [Google Scholar] [CrossRef]
- McFarland, L.V. Use of Probiotics to Correct Dysbiosis of Normal Microbiota Following Disease or Disruptive Events: A Systematic Review. BMJ Open 2014, 4, e005047. [Google Scholar] [CrossRef]
- Bauer, S.A.W.; Schneider, S.; Behr, J.; Kulozik, U.; Foerst, P. Combined Influence of Fermentation and Drying Conditions on Survival and Metabolic Activity of Starter and Probiotic Cultures after Low-Temperature Vacuum Drying. J. Biotechnol. 2012, 159, 351–357. [Google Scholar] [CrossRef]
- Foerst, P.; Kulozik, U.; Schmitt, M.; Bauer, S.; Santivarangkna, C. Storage Stability of Vacuum-Dried Probiotic Bacterium Lactobacillus Paracasei F19. Food Bioprod. Process. 2012, 90, 295–300. [Google Scholar] [CrossRef]
- Probiotische Mikroorganismenkulturen. In Lebensmitteln Abschlussbericht der Arbeitsgruppe “Probiotische Mikroorganismen in Lebensmitteln” am BgVV; Ernährungs-Umschau 47; Bundesinstitut für gesundheitlichen Verbraucherschutz und Veterinärmedizin: Berlin, Germany, 2000; pp. 191–195.
- Kleiman, S.C.; Bulik-Sullivan, E.C.; Glenny, E.M.; Zerwas, S.C.; Huh, E.Y.; Tsilimigras, M.C.B.; Fodor, A.A.; Bulik, C.M.; Carroll, I.M. The Gut-Brain Axis in Healthy Females: Lack of Significant Association between Microbial Composition and Diversity with Psychiatric Measures. PLoS ONE 2017, 12, e0170208. [Google Scholar] [CrossRef]
- Errisuriz, V.L.; Pasch, K.E.; Perry, C.L. Perceived Stress and Dietary Choices: The Moderating Role of Stress Management. Eat. Behav. 2016, 22, 211–216. [Google Scholar] [CrossRef]
- Kandiah, J.; Yake, M.; Jones, J.; Meyer, M. Stress Influences Appetite and Comfort Food Preferences in College Women. Nutr. Res. 2006, 26, 118–123. [Google Scholar] [CrossRef]
- Studitemps GmbH; Maastricht University. Fachkraft 2030: 9. Und 10. Erhebung Zur Wirtschaftlichen Und Allgemeinen Lebenssituation Der Studierenden in Deutschland; Constata UG: Bonn, Germany, 2019. [Google Scholar]
- Browning, M.; Reid, C.; Cowen, P.J.; Goodwin, G.M.; Harmer, C.J. A Single Dose of Citalopram Increases Fear Recognition in Healthy Subjects. J. Psychopharmacol. 2007, 21, 684–690. [Google Scholar] [CrossRef]
- Murphy, S.E.; Norbury, R.; O’Sullivan, U.; Cowen, P.J.; Harmer, C.J. Effect of a Single Dose of Citalopram on Amygdala Response to Emotional Faces. Br. J. Psychiatry 2009, 194, 535–540. [Google Scholar] [CrossRef]
- Naseribafrouei, A.; Hestad, K.; Avershina, E.; Sekelja, M.; Linløkken, A.; Wilson, R.; Rudi, K. Correlation between the Human Fecal Microbiota and Depression. Neurogastroenterol. Motil. 2014, 26, 1155–1162. [Google Scholar] [CrossRef]
- Rao, S.S.C.; Rehman, A.; Yu, S.; de Andino, N.M. Brain Fogginess, Gas and Bloating: A Link between SIBO, Probiotics and Metabolic Acidosis. Clin. Transl. Gastroenterol. 2018, 9, e162. [Google Scholar] [CrossRef]
- IMD Institut für Medizinische Diagnostik Berlin-Potsdam Gbr. Labor Parameterverzeichnis 2020. Available online: https://www.imd-berlin.de/de/leistungsverzeichnis/parameter.html?tx_ajdiagnostics_analyse%5Baction%5D=showmod&tx_ajdiagnostics_analyse%5Banalyse%5D=151114&tx_ajdiagnostics_analyse%5Bcontroller%5D=Analyse&tx_ajdiagnostics_analyse%5Bsynonym%5D=&tx_ajdiagnostics_analyse%5Btitle%5D=Echovirus%20-30%20-%20AK&cHash=1eae299d4e6e66a33ea60ed52bb96269 (accessed on 3 July 2020).
- Smyth, N.; Clow, A.; Thorn, L.; Hucklebridge, F.; Evans, P. Delays of 5–15min between Awakening and the Start of Saliva Sampling Matter in Assessment of the Cortisol Awakening Response. Psychoneuroendocrinology 2013, 38, 1476–1483. [Google Scholar] [CrossRef]
- Stalder, T.; Kirschbaum, C.; Kudielka, B.M.; Adam, E.K.; Pruessner, J.C.; Wüst, S.; Dockray, S.; Smyth, N.; Evans, P.; Hellhammer, D.H.; et al. Assessment of the Cortisol Awakening Response: Expert Consensus Guidelines. Psychoneuroendocrinology 2016, 63, 414–432. [Google Scholar] [CrossRef]
- Carroll, D.; Ginty, A.T.; Der, G.; Hunt, K.; Benzeval, M.; Phillips, A.C. Increased Blood Pressure Reactions to Acute Mental Stress Are Associated with 16-Year Cardiovascular Disease Mortality: Stress Reactivity and Cardiovascular Disease Mortality. Psychophysiology 2012, 49, 1444–1448. [Google Scholar] [CrossRef]
- Messaoudi, M.; Violle, N.; Bisson, J.-F.; Desor, D.; Javelot, H.; Rougeot, C. Beneficial Psychological Effects of a Probiotic Formulation (Lactobacillus Helveticus R0052 and Bifidobacterium Longum R0175) in Healthy Human Volunteers. Gut Microbes 2011, 2, 256–261. [Google Scholar] [CrossRef]
- Köhler, A. Japan: Schulstress Bis in Die Tiefe Nacht. Available online: https://www.diepresse.com/5080604/japan-schulstress-bis-in-die-tiefe-nacht (accessed on 22 April 2021).
- Biggs, A.; Brough, P.; Drummond, S. Lazarus and Folkman’s Psychological Stress and Coping Theory. In The Handbook of Stress and Health; Cooper, C.L., Quick, J.C., Eds.; John Wiley & Sons, Ltd.: Chichester, UK, 2017; pp. 349–364. ISBN 978-1-118-99381-1. [Google Scholar]
- Woodmansey, E.J. Intestinal Bacteria and Ageing. J. Appl. Microbiol. 2007, 102, 1178–1186. [Google Scholar] [CrossRef] [PubMed]
| Database and Date of Search | Hits | Exclusion of Meta-Analysis and Reviews | Additional Filters |
|---|---|---|---|
| PsychINFO 3 December 2020 | n = 116 | n = 56 | Dates of coverage 2010–2020: Species human: n = 18 |
| PSYNDEX 3 December 2020 | n = 67 | n = 35 | Dates of coverage 2010–2020: n = 34 Species human: n = 34 |
| PubMed 3 December 2020 | n = 2.247 | n = 40 | Dates of coverage 2010–2020: n = 39 Species human: n = 35 |
| First Author and Year | Sample Characteristics | Outcome Measures and Stressor | Intervention | Main Findings and Statistical Limitations |
|---|---|---|---|---|
| Allen et al. [58] | Planned sample size of one-way ANOVA: 20 (alpha/beta/eta: 0.05/0.20/0.3) Actual sample size: 22 Age, mean (SD) years: 25.5 (1.2) Gender, n (%) male: 22 (100) Exclusion criteria: women, chronic diseases, psychiatric diagnosis, following a diet, regular intake of medication Country: Ireland | Primary: Salivary cortisol Secondary: State-Trait Anxiety Inventory (STAI), PSS Stressor: Socially Evaluated Cold Pressure Test (SECPT) | Daily Intake of: one probiotics stick containing Bifidobacterium longum 1714 or placebo Duration: four weeks and a two-week follow-up period without intake of probiotics or placebo | Daily perceived stress of the experimental group after four weeks was significantly lower by 15% compared to control group (p < 0.05). Daily perceived stress increased again in the follow-up period. SECPT triggered an equal stress reaction at an overall lower stress hormone level and without leading to an increased subjective anxiety on the STAI score (p < 0.05). Limitations: Unreasonable beta and eta. No extra power analysis for non-parametric tests => Probably all tests underpowered. |
| Kato-Kataoka et al. [59] | Planned sample Size: unknown Actual sample size: 47 Age, mean (SD) years: 22.8 (0.4) Gender, n (%) female: 21 (45); male: 26 (55) Exclusion criteria: age > 30 years, taking medication three months prior to enrollment Country: Japan | Primary: Salivary Cortisol Secondary: STAI, stool samples, Visual Analogue Scale (VAS), Gastrointestinal Symptom rating scale (Japanese version); GSRS) Stressor: School examination | Daily intake of: 100 mL of milk fermented with L. casei strain Shirota or placebo Duration: 56 days | Subjects in the experimental group had significantly lower salivary cortisol levels than the control group one day before their examination (p < 0.05). No effect on STAI scores but significantly lower expression of the subjective feeling of stress on the VAS. Reduction in stress-induced physical pain and cold symptoms (p < 0.05). Limitations: Kato-Kataoka et al. [59]: “The major limitation of this study was its lack of statistical power because of its small sample of participants.” |
| Kelly et al. [60] | Planned sample size of one-way ANOVA: 20 (alpha/beta/eta: 0.05/0.20/0.3) Actual sample size: 29 Age, mean (SD) years: 24.69 (0.75) Gender, n (%) male: 29 (100) Exclusion criteria: chronic diseases, regular intake of medicine or antibiotics, following a diet Country: Ireland | Primary: Salivary Cortisol Secondary: Blood sample for cytokine measurements, PSS, STAI Stressor: SECPT | Daily intake of: one capsule containing probiotics (Lactobacillus rhamnosus) or placebo Duration: four weeks, then conditions for experimental and control group were switched | No effect of probiotics on subjective stress levels (before and after SECPT), salivary cortisol levels in response to the SECPT, PSS and STAI scores, compared with control group. Increase in cytokine levels in the placebo phase which was not significant. Limitations: same as Allen et al. [58] |
| Messaoudi et al. [61] | Planned sample size of U-Test: 56 (alpha/beta/effect size: 0.05/0.20/unknown) Actual s Sample size: 55 Age, mean (SD) years: 42.8 (8) Gender, n (%) female: 41 (75); male: 14 (25) Exclusion criteria: psychiatric, neurological or cardiovascular disease, allergies, regular intake of vitamins Country: France | Primary: urinary cortisol over a 24-h period Secondary: Hospital and Depression Anxiety Scale (HADS), Coping Checklist, PSS Stressor: no acute stressor, normal everyday life of subjects | Daily intake of: one probiotic stick containing 1.5 g of two species (L. helveticus R0052, B. longum R0175) Duration: 30 days | Lower urinary cortisol levels and subjectively lower stress level in the experimental group (p < 0.05). Lower depression scale subscore on the HADS (p < 0.01) and higher positive re-evaluation (p < 0.05), lower self-blame (p < 0.05), higher problem-solving competence in the Coping Checklist (p < 0.05). No Effects were found for both groups on the results of the PSS. Limitations: Unreasonable beta and no clear statement on the assumed effect size. G*Power gives a planned sample size of 60 if we assume a large effect for a two-tailed U-Test => Tests probably underpowered since found effects are smaller. |
| Möller et al. [62] | Planned sample size: none Actual sample size: 105 Age, mean (SD) years: 20.17 (1.26) Gender, n (%) female: 69 (66); male: 36 (34) Exclusion criteria: bowel disease, taking antibiotics three months prior to enrollment, regular intake of pro- or prebiotics | Primary: Blood pressure, pulse Secondary: stress procedure evaluation Stressor: Paced Auditory Serial Addition Test (PASAT) | Daily intake of: one probiotic capsule containing three Bifidobacterium and five Lactobacillus species Duration: 14 days | No significant effect of probiotics intake on blood pressure or pulse rate (p < 0.05). Limitations: Explorative study with no post hoc power analysis. However, a power of 0.79 is given if we use n/alpha/eta as 105/0.05/0.1 for an ANOVA with repeated measures, within-between interaction and otherwise G*Power default values. |
| Schmidt et al. [63] | Planned sample size: none Actual sample size: 45 Age, mean (SD) years: 23.27 (3.89) Gender, n (%) female: 23 (51); male: 22 (49) Exclusion criteria: DSM-IV diagnosis, gastroenteric, neurological or immune disease, taking antibiotics three months prior to enrollment, regular intake of pre- or probiotics | Primary: Salivary Cortisol Awakening Response (CAR) Secondary: STAI, PSS, Dot probe-task Stressor: no acute stressor, anticipation of a stressful event of the upcoming day | Daily intake of: one of two probiotic sticks (fructooligsaccharides (FOS) or Bimuno™-galacto-oligosaccharides (B-GOS)) or placebo Duration three weeks | CAR in saliva was significantly lower in the B-GOS experimental group compared to the control group (p < 0.05). The experimental group also showed significantly lower alertness to emotional stimuli (p > 0.01) in the dot probe task. No effects could be found for the FOS group and no changes in STAI or PSS scores were shown in both experimental groups. Limitations: No sample size planning. The study claims that underpowered results were not interpreted, but does not provide any information on how large the minimum power was set or calculated => Power unknown. |
| Takada et al. [38] | Planned sample size: none Actual sample size: 140 Age, mean (SD) years: 22.9 (0.2) Gender, n (%) female: 64 (46); male 76 (54) Exclusion criteria: subjects > 30 years, diagnosis of mental disorder and a score of ≤60 on the Self-rating Depression scale, regular intake of pre- or probiotics | Primary: Salivary cortisol levels Secondary: STAI Stressor: School examination | Daily intake of: 100 mL milk fermented with L. casei strain Shirota YIT 9029 or placebo Duration: eight weeks | Significant reduction in cold symptoms (sore throat, headache, fever) at week 5–6 (p < 0.05) and abdominal region pain at week 7–8 (p < 0.05) in the experimental group. The group as well had significantly lower cortisol level (p < 0.05) one day before the exam. Significant changes were found for STAI scores in comparison to the control group (p < 0.01). Limitations: No sample size planning. Power unknown. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anker-Ladefoged, C.; Langkamp, T.; Mueller-Alcazar, A. The Potential Impact of Selected Bacterial Strains on the Stress Response. Healthcare 2021, 9, 494. https://doi.org/10.3390/healthcare9050494
Anker-Ladefoged C, Langkamp T, Mueller-Alcazar A. The Potential Impact of Selected Bacterial Strains on the Stress Response. Healthcare. 2021; 9(5):494. https://doi.org/10.3390/healthcare9050494
Chicago/Turabian StyleAnker-Ladefoged, Clara, Thomas Langkamp, and Anett Mueller-Alcazar. 2021. "The Potential Impact of Selected Bacterial Strains on the Stress Response" Healthcare 9, no. 5: 494. https://doi.org/10.3390/healthcare9050494
APA StyleAnker-Ladefoged, C., Langkamp, T., & Mueller-Alcazar, A. (2021). The Potential Impact of Selected Bacterial Strains on the Stress Response. Healthcare, 9(5), 494. https://doi.org/10.3390/healthcare9050494







