Successful Treatment of Pediatric Inflammatory Multisystem Syndrome Temporally Associated with COVID-19 (PIMS-TS) with Split Doses of Immunoglobulin G and Estimation of PIMS-TS Incidence in a County District in Southern Germany
Abstract
:1. Introduction
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Toubiana, J.; Poirault, C.; Corsia, A.; Bajolle, F.; Fourgeaud, J.; Angoulvant, F.; Debray, A.; Basmaci, R.; Salvador, E.; Biscardi, S.; et al. Kawasaki-like multisystem inflammatory syndrome in children during the covid-19 pandemic in Paris, France: Prospective observational study. BMJ 2020, 369, m2094. [Google Scholar] [CrossRef] [PubMed]
- Whittaker, E.; Bamford, A.; Kenny, J.; Kaforou, M.; Jones, C.E.; Shah, P.; Ramnarayan, P.; Fraisse, A.; Miller, O.; Davies, P.; et al. Clinical Characteristics of 58 Children with a Pediatric Inflammatory Multisystem Syndrome Temporally Associated with SARS-CoV-2. JAMA 2020, 324, 259–269. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.; Tang, K.; Levin, M.; Irfan, O.; Morris, S.K.; Wilson, K.; Klein, J.D.; Bhutta, Z.A. COVID-19 and multisystem inflammatory syndrome in children and adolescents. Lancet Infect. Dis. 2020, 20, e276–e288. [Google Scholar] [CrossRef]
- Riphagen, S.; Gomez, X.; Gonzalez-Martinez, C.; Wilkinson, N.; Theocharis, P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet 2020, 395, 1607–1608. [Google Scholar] [CrossRef]
- WHO. Multisystem Inflammatory Syndrome in Children and Adolscents Temporally Related to COVID-19 [Scientific Brief]; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Lutchman, D. PIMS-TS and Kawasaki Disease: The Mystery Deepens. Pediatr. Infect. Dis. J. 2020, 39, e215–e216. [Google Scholar] [CrossRef] [PubMed]
- Davies, P.; Evans, C.; Kanthimathinathan, H.K.; Lillie, J.; Brierley, J.; Waters, G.; Johnson, M.; Griffiths, B.; du Pré, P.; Mohammad, Z.; et al. Intensive care admissions of children with paediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS) in the UK: A multicentre observational study. Lancet Child Adolesc. Health 2020, 4, 669–677. [Google Scholar] [CrossRef]
- Nydegger, U.E.; Sturzenegger, M. Adverse Effects of Intravenous Immunoglobulin Therapy. Drug Saf. 1999, 21, 171–185. [Google Scholar] [CrossRef] [PubMed]
- Altman, D.G.; Machin, D.; Bryant, T.N.; Gardner, M.J. Statistics with Confidence; Confidence Intervals and Statistical Guidelines, 2 ed.; BMJ Books: Bristol, UK, 2000; pp. 46–48. [Google Scholar]
- Becker, T.; (Stadt Kaufbeuren, Kaufbeuren, Germany); Greif, C.; (Landratsamt Marktoberdorf, Marktoberdorf, Germany). Personal communication, 2021.
- Krikilion, J.; Nuyttens, L.; Daelemans, S.; François, K.; Mauel, R.; De Wolf, D.; Van Berlaer, G. Varying Presentations of Multisystem Inflammatory Syndrome Temporarily Associated with COVID-19. Case Rep. Pediatr. 2020, 2020, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Licciardi, F.; Pruccoli, G.; Denina, M.; Parodi, E.; Taglietto, M.; Rosati, S.; Montin, D. SARS-CoV-2–Induced Kawasaki-Like Hyperinflammatory Syndrome: A Novel COVID Phenotype in Children. Pediatrics 2020, 146, e20201711. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Michihata, N.; Yoshikawa, T.; Hata, T.; Matsui, H.; Fushimi, K.; Yasunaga, H. High-dose versus low-dose intravenous immunoglobulin for treatment of children with Kawasaki disease weighing 25 kg or more. Eur. J. Nucl. Med. Mol. Imaging 2020, 179, 1901–1907. [Google Scholar] [CrossRef] [PubMed]
- Toniati, P.; Piva, S.; Cattalini, M.; Garrafa, E.; Regola, F.; Castelli, F.; Franceschini, F.; Airò, P.; Bazzani, C.; Beindorf, E.-A.; et al. Tocilizumab for the treatment of severe COVID-19 pneumonia with hyperinflammatory syndrome and acute respiratory failure: A single center study of 100 patients in Brescia, Italy. Autoimmun. Rev. 2020, 19, 102568. [Google Scholar] [CrossRef] [PubMed]
- DGPI. PIMS Falldefinition. Available online: www.dgpi.de/pims-survey-anleitung (accessed on 9 March 2021).
- Felsenstein, S.; Willis, E.; Lythgoe, H.; McCann, L.; Cleary, A.; Mahmood, K.; Porter, D.; Jones, J.; McDonagh, J.; Chieng, A.; et al. Presentation, Treatment Response and Short-Term Outcomes in Paediatric Multisystem Inflammatory Syndrome Temporally Associated with SARS-CoV-2 (PIMS-TS). J. Clin. Med. 2020, 9, 3293. [Google Scholar] [CrossRef] [PubMed]
- Radia, T.; Williams, N.; Agrawal, P.; Harman, K.; Weale, J.; Cook, J.; Gupta, A. Multi-system inflammatory syndrome in children & adolescents (MIS-C): A systematic review of clinical features and presentation. Paediatr. Respir. Rev. 2020. [Google Scholar] [CrossRef]
- McMurray, J.C.; May, J.W.; Cunningham, M.W.; Jones, O.Y. Multisystem Inflammatory Syndrome in Children (MIS-C), a Post-viral Myocarditis and Systemic Vasculitis—A Critical Review of Its Pathogenesis and Treatment. Front. Pediatr. 2020, 8, 626182. [Google Scholar] [CrossRef] [PubMed]
- Evans, C.; Davies, P. SARS-CoV-2 paediatric inflammatory syndrome. Paediatr. Child Health 2021, 31, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Balasubramanian, S.; Nagendran, T.M.; Ramachandran, B.; Ramanan, A.V. Hyper-inflammatory Syndrome in a Child with COVID-19 Treated Successfully with Intravenous Immunoglobulin and Tocilizumab. Indian Pediatr. 2020, 57, 681–683. [Google Scholar] [CrossRef] [PubMed]
- Diorio, C.; Henrickson, S.E.; Vella, L.A.; McNerney, K.O.; Chase, J.M.; Burudpakdee, C.; Lee, J.H.; Jasen, C.; Balamuth, F.; Barrett, D.M.; et al. Multisystem inflammatory syndrome in children and COVID-19 are distinct presentations of SARS–CoV-2. J. Clin. Investig. 2020, 130, 5967–5975. [Google Scholar] [CrossRef]
- Sperotto, F.; Friedman, K.G.; Son, M.B.F.; VanderPluym, C.J.; Newburger, J.W.; Dionne, A. Cardiac manifestations in SARS-CoV-2-associated multisystem inflammatory syndrome in children: A comprehensive review and proposed clinical approach. Eur. J. Nucl. Med. Mol. Imaging 2021, 180, 307–322. [Google Scholar] [CrossRef]
| Reference Values | Patient 1 | Patient 2 | Patient 3 | |
|---|---|---|---|---|
| CRP (mg/L) | <5.0 | 257.6 | 119.1 | 135.1 |
| PCT (ng/mL) | <0.5 | 0.56 | 0.44 | 1.88 |
| Ferritin (ng/mL) | 15–150 | >1000 | 356.4 | 161.9 |
| D-Dimer (µg/L) | <0.5 | 10.54 | 2.46 | 1.67 |
| GOT (U/L) | <35 | 108 | 63 | 46 |
| GPT (U/L) | <35 | 72 | 68 | 35 |
| GGT (U/L) | <39 | 95 | 39 | 13 |
| Albumin (g/L) | 35–52 | 26.6 | 26.5 | |
| Troponin T (pg/mL) | <14 | 45.3 | 70.5 | 16.3 |
| Leukocytes (G/L) | 3.96–10.4 | 8.66 | 7.81 | 10.93 |
| Neutrophile Granulocytes (G/L) | 50–70% | 7.15 | 6.59 | 9.54 |
| Blood smear | No burr cells | No burr cells | No burr cells | |
| Lymphocytes (G/L) | 15–40% | 4.80 | 7.57 | 8.74 |
| sIL2Receptor (U/mL) | 158–623 | 7253 | 2361 | 2558 |
| NT-proBNP (pg/mL) | <125 | 4893 | 1520 | 1703 |
| Patient 1 | Patient 2 | Patient 3 | |
|---|---|---|---|
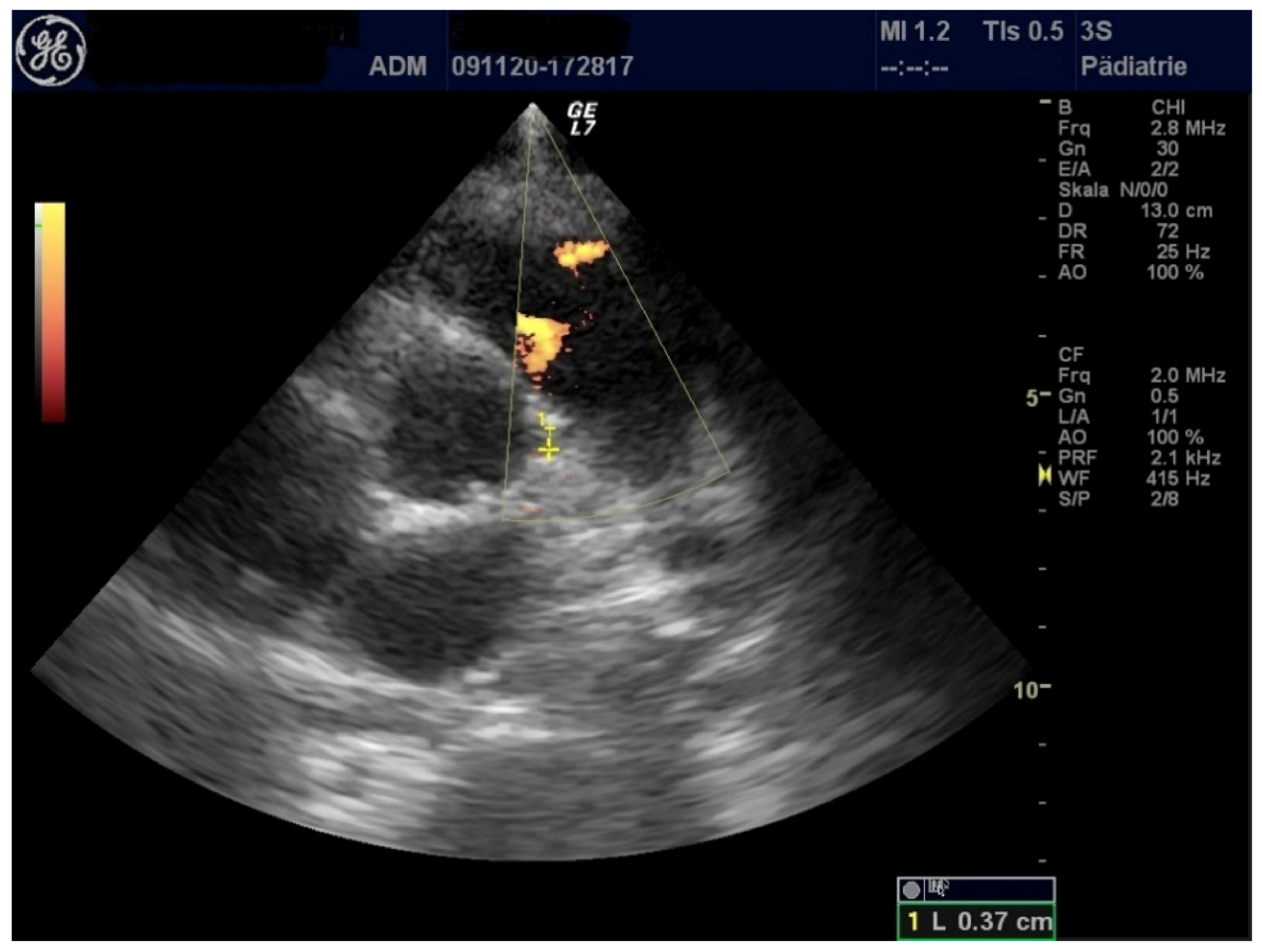
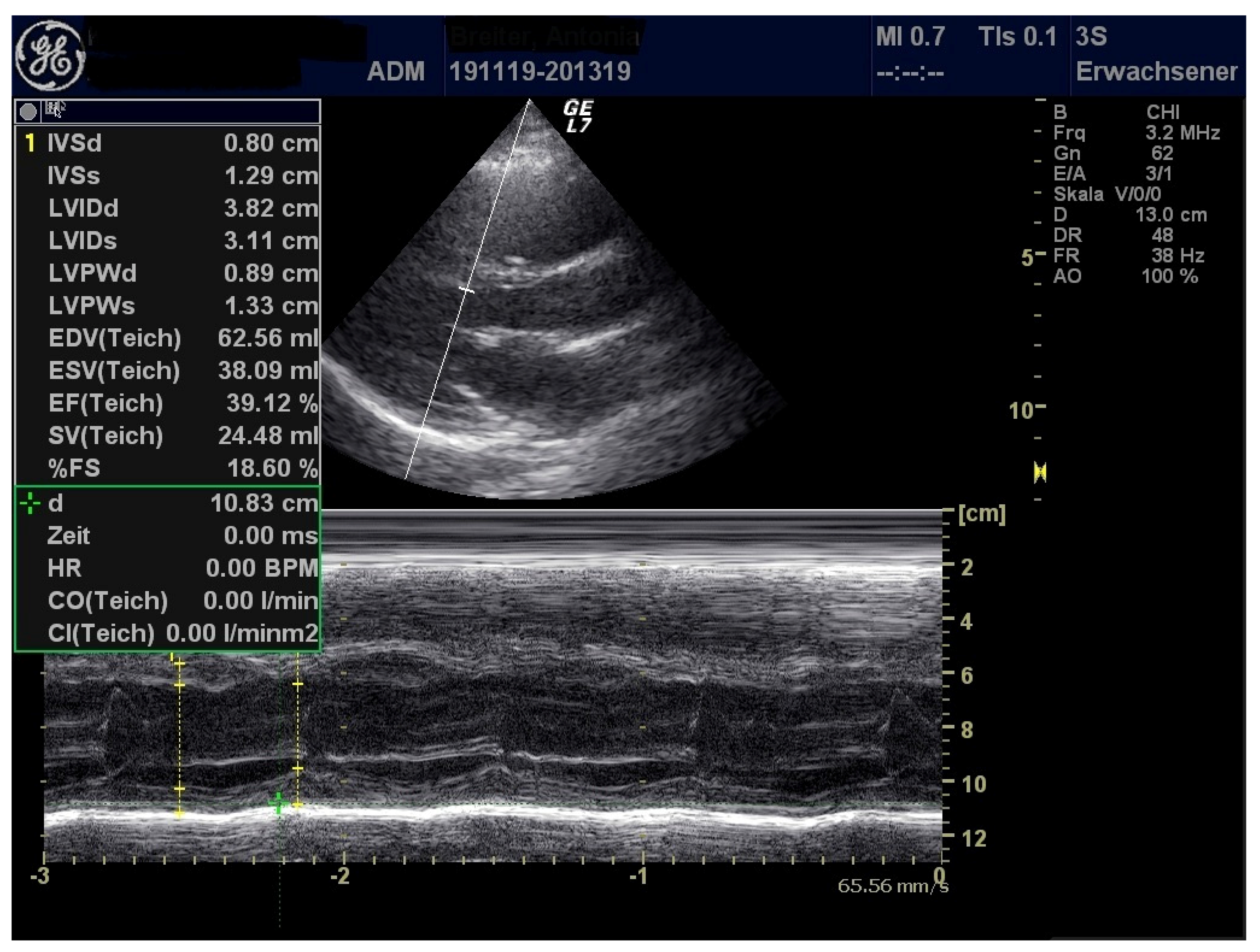
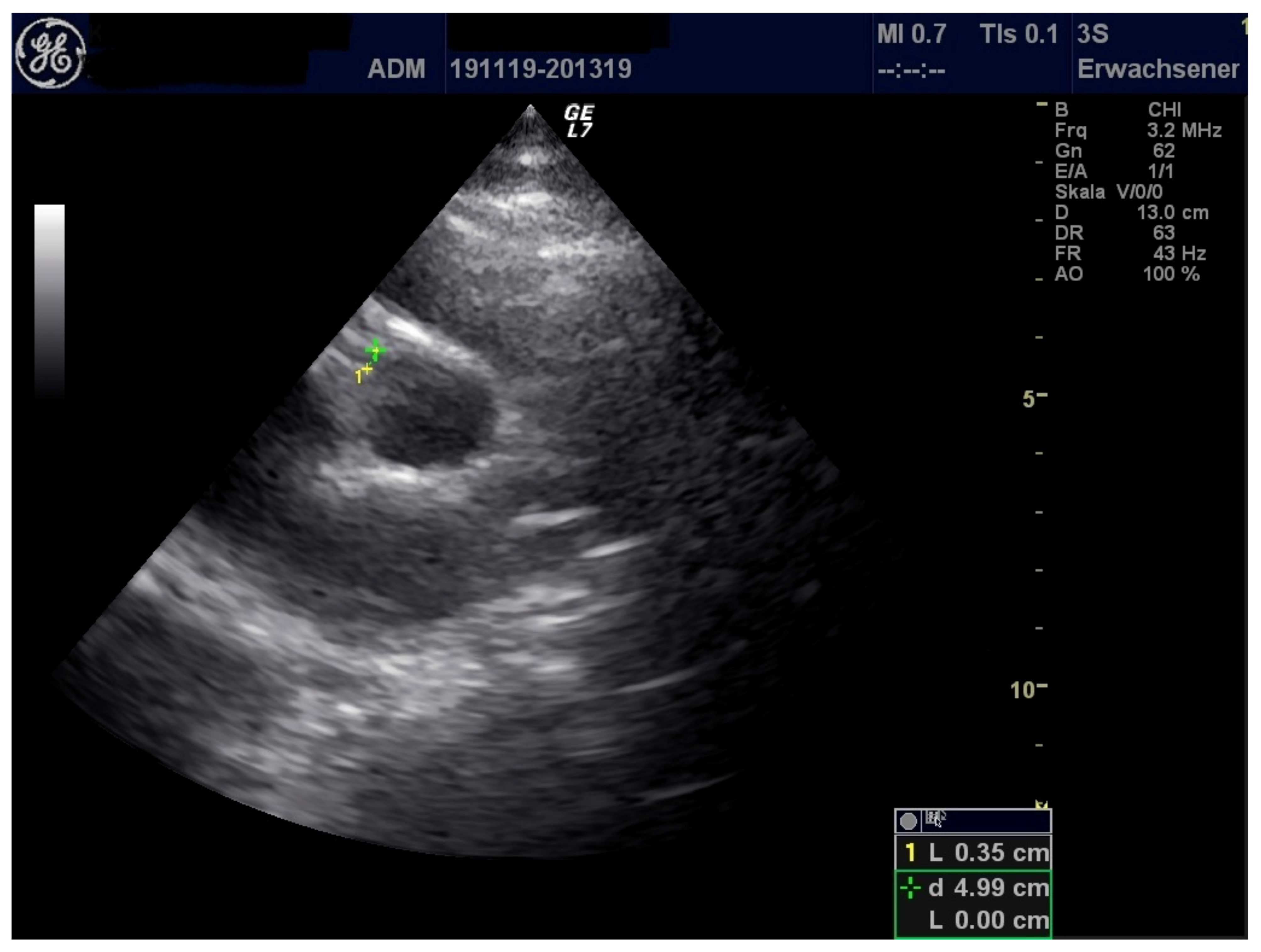
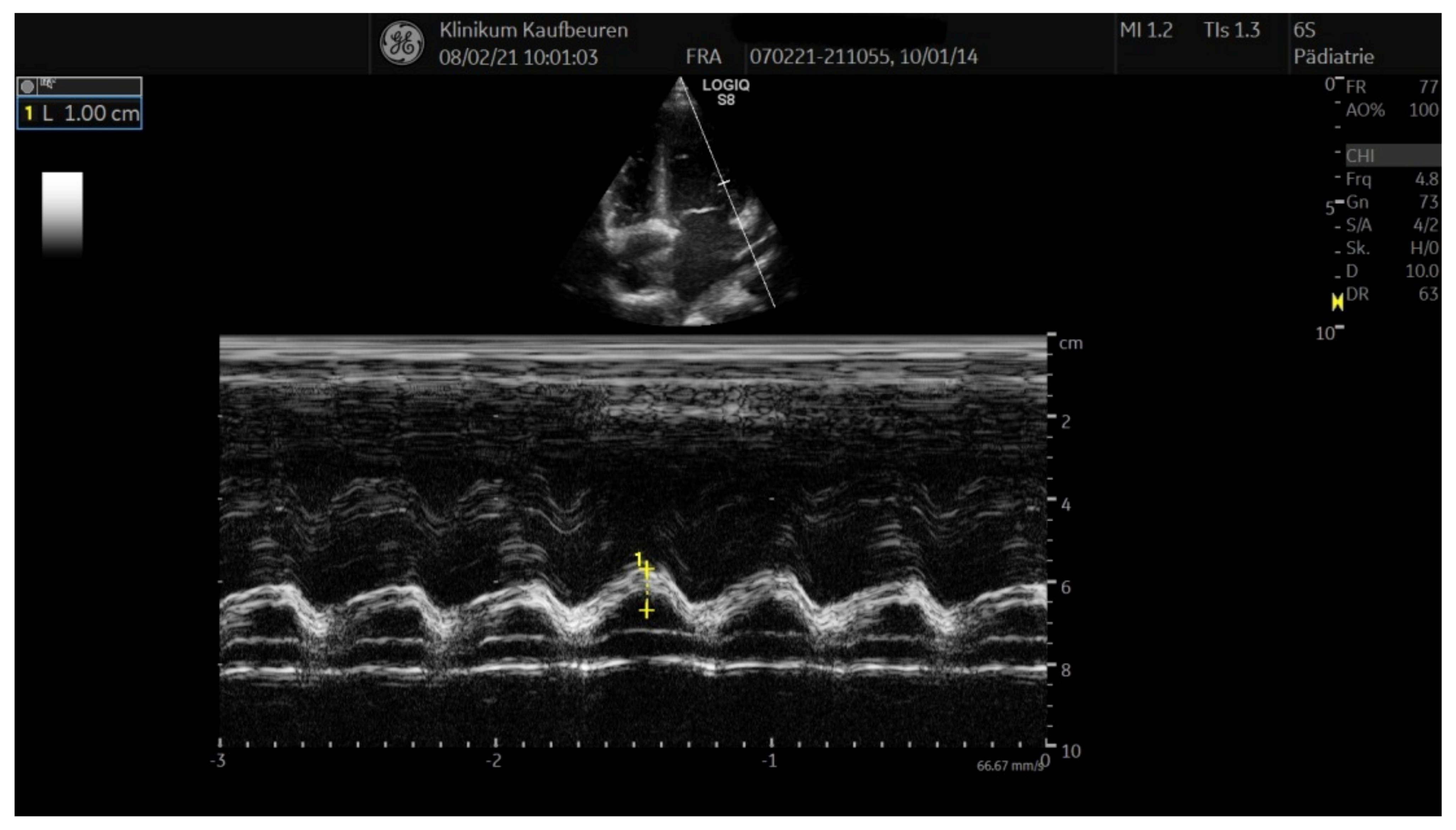
| LVEF (%) | 71 | 44 | 53 |
| FS (%) | 40 | 21.1 | 26.6 |
| MAPSE (cm) | 1.97 | 1.42 | 0.91 |
| TAPSE (cm) | 2.55 | 2.08 | 1.14 |
| LCA (mm) | 3.8 | 3.3 | 3.1 |
| RCA (mm) | 3.2 | 4.0 | 2.8 |
| Pericardial effusion (mm) | 7 | 3 | 5 |
| Pleural effusion (mm) | 9 (left), right 0 | 0 | 0 |
| Patient 1 | Patient 2 | Patient 3 | |
|---|---|---|---|
| Streptococcus group A RAD test | negative | negative | negative |
| Adenovirus IgM | negative | negative | negative |
| Adenovirs DNA | negative | negative | negative |
| CMV IgG | negative | negative | negative |
| CMV IgM | negative | negative | negative |
| EBV VCA IgG | negative | positive | positive |
| EBV VCA IgM | negative | negative | negative |
| EBV EBNA IgG | positive | positive | positive |
| SARS CoV2 IgG | positive (43.6) | positive (75.3) | positive (143) |
| SARS CoV2 RNA nasal swab (Ct value) | negative | negative | positive (34.8) |
| Blood cultures | negative | negative | negative |
| Urin cultures | negative | negative | negative |
| Reference Values | Patient 1 | Patient 2 | Patient 3 | |
|---|---|---|---|---|
| CRP (mg/L) | <5.0 | 33.5 | 40.6 | 135.4 |
| PCT (ng/mL) | <0.5 | 3.2 | n.d. | n.d. |
| Ferritin (ng/mL) | 15–150 | 422.6 | 322.9 | 192.7 |
| D-Dimer (µg/L) | <0.5 | 0.96 | 1.37 | 1.25 |
| GOT (U/L) | <35 | 37 | 39 | 36 |
| GPT (U/L) | <35 | 33 | 39 | 35 |
| GGT (U/L) | <39 | 25 | 27 | 11 |
| Troponin T (pg/mL) | < 14 | 21.9 | 7.2 | 19.2 |
| Leukocytes (G/L) | 3.96–10.4 | 7.69 | 4.28 | 11.28 |
| Neutrophile Granulocytes (G/L) | 50–70% | 5.17 | 1.88 | 9.0 |
| sIL2-Receptor (U/mL) | 158–623 | n.d. | n.d. | n.d. |
| NT-proBNP (pg/mL) | <125 | 49.4 | 503.7 | 80.3 |
| (1) |
| Patient 1 | Patient 2 | Patient 3 | |
|---|---|---|---|
| LVEF (%) | 81 | 69 | 73 |
| FS (%) | 50 | 39 | 41 |
| MAPSE (cm) | n.d. | 1.67 | 1.5 |
| TAPSE (cm) | n.d. | 2.46 | 2.08 |
| LCA (mm) | 3.7 | 3.2 | 2.8 |
| RCA (mm) | 3.3 | 3.0 | 2.4 |
| Pericardial effusion (mm) | 0 | 3–7 | <3 |
| Pleural effusion (mm) | 0 (both sides) | 0 | 0 |
| Patient 1 | Patient 2 | Patient 3 | |
|---|---|---|---|
| Gender | male | female | female |
| Age (years) | 14 | 17 | 7 |
| Ethnicity | German-Turkish | German | German |
| Co-morbidities | none | none | none |
| Co-medication | none | none | none |
| Rural District Ostallgäu | City District Kaufbeuren | |
|---|---|---|
| Total inhabitants | 171.226 | 46.199 |
| Inhabitants under 18 years | 25.247 | 7.450 |
| SARS CoV-2 positive (week 12 in 2020 to week 8 in 2021) | 404; female: 191 | 166; female: 77 |
| PIMS-TS (1 December 2020–31 August 2021) | 2 (both female) | 1 (male) |
| Rural District Ostallgäu + City District Kaufbeuren | ||
| Incidence SARS-CoV-2 positive (%) | 1.8%, 95% CI: 1.7% to 2.0% | |
| Incidence PIMS-TS (%) | 1.7%, 95% CI: 0.9% to 3.1% | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wehl, G.; Franke, J.; Frühwirth, M.; Edlinger, M.; Rauchenzauner, M. Successful Treatment of Pediatric Inflammatory Multisystem Syndrome Temporally Associated with COVID-19 (PIMS-TS) with Split Doses of Immunoglobulin G and Estimation of PIMS-TS Incidence in a County District in Southern Germany. Healthcare 2021, 9, 481. https://doi.org/10.3390/healthcare9040481
Wehl G, Franke J, Frühwirth M, Edlinger M, Rauchenzauner M. Successful Treatment of Pediatric Inflammatory Multisystem Syndrome Temporally Associated with COVID-19 (PIMS-TS) with Split Doses of Immunoglobulin G and Estimation of PIMS-TS Incidence in a County District in Southern Germany. Healthcare. 2021; 9(4):481. https://doi.org/10.3390/healthcare9040481
Chicago/Turabian StyleWehl, Götz, Jörg Franke, Martin Frühwirth, Michael Edlinger, and Markus Rauchenzauner. 2021. "Successful Treatment of Pediatric Inflammatory Multisystem Syndrome Temporally Associated with COVID-19 (PIMS-TS) with Split Doses of Immunoglobulin G and Estimation of PIMS-TS Incidence in a County District in Southern Germany" Healthcare 9, no. 4: 481. https://doi.org/10.3390/healthcare9040481
APA StyleWehl, G., Franke, J., Frühwirth, M., Edlinger, M., & Rauchenzauner, M. (2021). Successful Treatment of Pediatric Inflammatory Multisystem Syndrome Temporally Associated with COVID-19 (PIMS-TS) with Split Doses of Immunoglobulin G and Estimation of PIMS-TS Incidence in a County District in Southern Germany. Healthcare, 9(4), 481. https://doi.org/10.3390/healthcare9040481






