COVID-19-Related Fear, Risk Perception, and Safety Behavior in Individuals with Diabetes
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Propensity Score Matching
2.3. Assessment Instruments
2.4. Statistical Analyses
3. Results
3.1. Participant Characteristics
3.2. Generalized Anxiety and Depressive Symptoms
3.3. COVID-19-Related Fear, Subjective Level of Information, and Safety Behavior
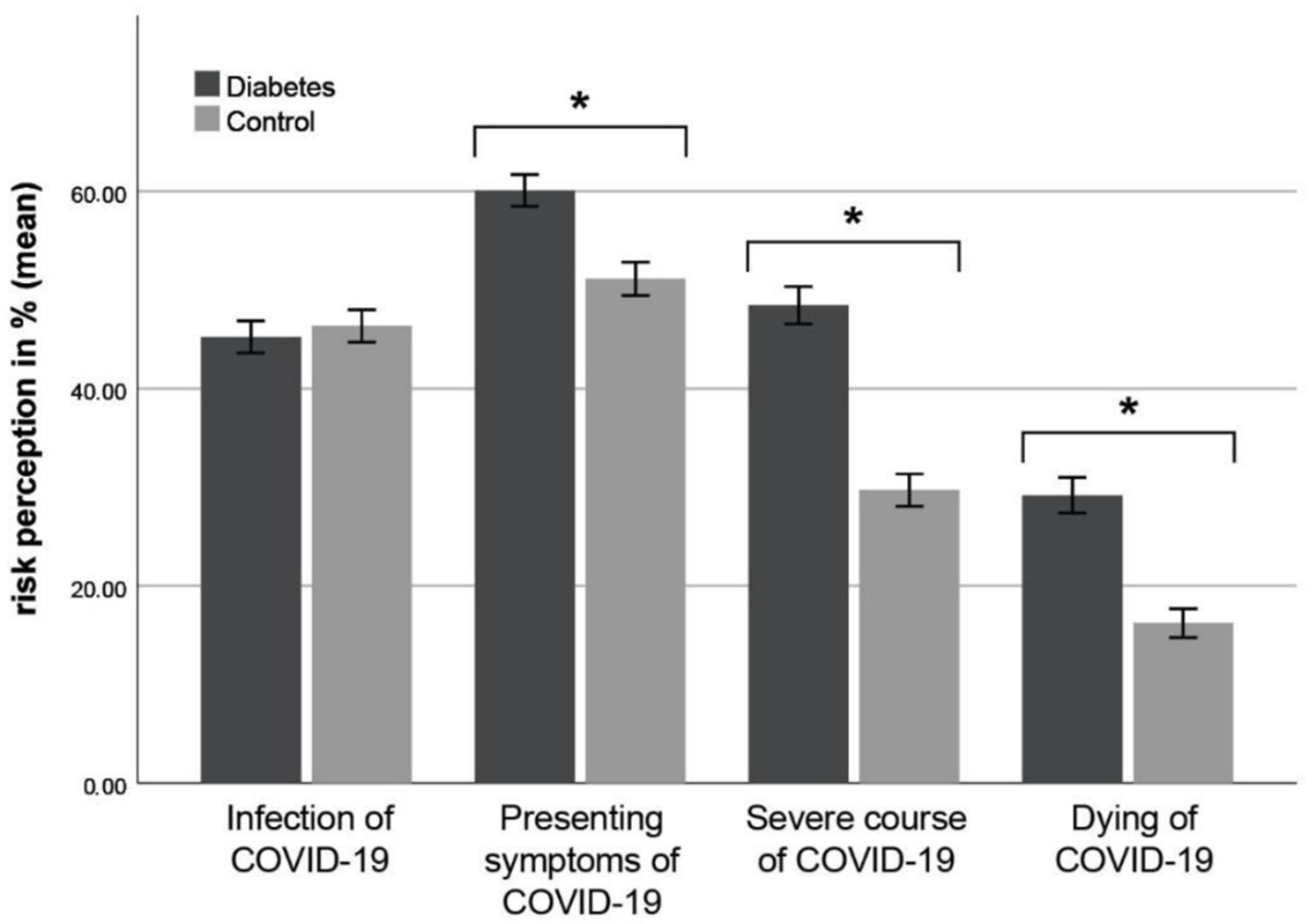
3.4. Subjective Risk Perception
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO (World Health Organization). Coronavirus Disease (COVID-19) Dashboard 2021. Available online: https://covid19.who.int/ (accessed on 14 February 2021).
- Yang, J.; Zheng, Y.; Gou, X.; Pu, K.; Chen, Z.; Guo, Q.; Ji, R.; Wang, H.; Wang, Y.; Zhou, Y. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: A systematic review and meta-analysis. Int. J. Infect. Dis. 2020, 94, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Cariou, B.; Hadjadj, S.; Wargny, M.; Pichelin, M.; Al-Salameh, A.; Allix, I.; Amadou, C.; Arnault, G.; Baudoux, F.; Bauduceau, B.; et al. Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: The CORONADO study. Diabetologia 2020, 63, 1500–1515. [Google Scholar] [CrossRef] [PubMed]
- Guo, W.; Li, M.; Dong, Y.; Zhou, H.; Zhang, Z.; Tian, C.; Qin, R.; Wang, H.; Shen, Y.; Du, K.; et al. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab. Res. Rev. 2020, 36, e3319. [Google Scholar] [CrossRef] [PubMed]
- Pal, R.; Bhadada, S.K. COVID-19 and diabetes mellitus: An unholy interaction of two pandemics. Diabetes Metab. Syndr. 2020, 14, 513–517. [Google Scholar] [CrossRef] [PubMed]
- Bäuerle, A.; Teufel, M.; Musche, V.; Weismüller, B.; Kohler, H.; Hetkamp, M.; Dörrie, N.; Schweda, A.; Skoda, E.-M. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: A cross-sectional study in Germany. J. Public Health (Oxf.) 2020, 42, 672–678. [Google Scholar] [CrossRef] [PubMed]
- Forte, G.; Favieri, F.; Tambelli, R.; Casagrande, M. The Enemy Which Sealed the World: Effects of COVID-19 Diffusion on the Psychological State of the Italian Population. J. Clin. Med. 2020, 9, 1802. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef]
- Rajkumar, R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatr. 2020, 52, 102066. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef]
- Fiorillo, A.; Gorwood, P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry 2020, 63, e32. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K.; et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Nouwen, A.; Winkley, K.; Twisk, J.; Lloyd, C.E.; Peyrot, M.; Ismail, K.; Pouwer, F. for the European Depression in Diabetes (EDID) Research Consortium. Type 2 diabetes mellitus as a risk factor for the onset of depression: A systematic review and meta-analysis. Diabetologia 2010, 53, 2480–2486. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.; Stone, M.A.; Peters, J.L.; Davies, M.J.; Khunti, K. The prevalence of co-morbid depression in adults with Type 2 diabetes: A systematic review and meta-analysis. Diabet. Med. 2006, 23, 1165–1173. [Google Scholar] [CrossRef] [PubMed]
- Grigsby, A.B.; Anderson, R.J.; Freedland, K.E.; Clouse, R.E.; Lustman, P.J. Prevalence of anxiety in adults with diabetes. J. Psychosom. Res. 2002, 53, 1053–1060. [Google Scholar] [CrossRef]
- Stuart, E.A.; Cole, S.R.; Bradshaw, C.P.; Leaf, P.J. The use of propensity scores to assess the generalizability of results from randomized trials. J. R. Stat. Soc. 2011, 174, 369–386. [Google Scholar] [CrossRef] [PubMed]
- Austin, P.C. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar. Behav. Res. 2011, 46, 399–424. [Google Scholar] [CrossRef]
- Löwe, B.; Decker, O.; Müller, S.; Brähler, E.; Schellberg, D.; Herzog, W.; Herzberg, P.Y. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med. Care 2008, 46, 266–274. [Google Scholar] [CrossRef]
- Löwe, B.; Kroenke, K.; Gräfe, K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J. Psychosom. Res. 2005, 58, 163–171. [Google Scholar] [CrossRef]
- Löwe, B.; Decker, O.; Müller, S.; Brähler, E.; Schellberg, D.; Herzog, W.; Herzberg, P.Y. COVID-19-Related Fear and Health-Related Safety Behavior in Oncological Patients. Front. Psychol. 2020, 11, 1984. [Google Scholar] [CrossRef]
- Hetkamp, M.; Schweda, A.; Bäuerle, A.; Weismüller, B.; Kohler, H.; Musche, V.; Dörrie, N.; Schöbel, C.; Teufel, M.; Skoda, E.-M. Sleep disturbances, fear, and generalized anxiety during the COVID-19 shut down phase in Germany: Relation to infection rates, deaths, and German stock index DAX. Sleep Med. 2020, 75, 350–353. [Google Scholar] [CrossRef]
- Skoda, E.-M.; Bäuerle, A.; Schweda, A.; Dörrie, N.; Musche, V.; Hetkamp, M.; Kohler, H.; Teufel, M.; Weismüller, B. Severely increased generalized anxiety, but not COVID-19-related fear in individuals with mental illnesses: A population based cross-sectional study in Germany. Int. J. Soc. Psychiatry 2020. 0020764020960773. [Google Scholar] [CrossRef]
- Stuart, E.A.; King, G.; Imai, K.; Ho, D. MatchIt: Nonparametric preprocessing for parametric causal inference. J. Stat. Softw. 2011, 42, 1–28. [Google Scholar] [CrossRef]
- Wilcox, R.R. Introduction to robust estimation and hypothesis testing. In Statistical Modeling and Decision Science; Academic Press: Cambridge, MA, USA, 2011. [Google Scholar]
- Hinz, A.; Klein, A.M.; Brähler, E.; Glaesmer, H.; Luck, T.; Riedel-Heller, S.G.; Wirkner, K.; Hilbert, A. Psychometric evaluation of the Generalized Anxiety Disorder Screener GAD-7, based on a large German general population sample. J. Affect. Disord. 2017, 210, 338–344. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.-Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int. J. Ment. Health Addict. 2020, 1–9. [Google Scholar] [CrossRef]
- Harper, C.A.; Satchell, L.P.; Fido, D.; Latzman, R.D. Functional Fear Predicts Public Health Compliance in the COVID-19 Pandemic. Int. J. Ment. Health Addict. 2020, 1–14. [Google Scholar] [CrossRef]
- Pakpour, A.H.; Griffiths, M.D. The fear of COVID-19 and its role in preventive behaviors. J. Concurr. Disord. 2020, 2, 58–63. [Google Scholar]
- Holman, N.; Knighton, P.; Kar, P.; O’Keefe, J.; Curley, M.; Weaver, A.; Barron, E.; Bakhai, C.; Khunti, K.; Wareham, N.J.; et al. Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: A population-based cohort study. Lancet Diabetes Endocrinol. 2020, 8, 823–833. [Google Scholar] [CrossRef]
- 30. Robert Koch Institut. SARS-CoV-2 Steckbrief zur Coronavirus-Krankheit-2019 (COVID-19) 2020. Available online: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Steckbrief.html (accessed on 6 October 2020).
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases from the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239–1242. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Byrne, C.D.; Zheng, M.H.; Targher, G. Diabetes as a risk factor for greater COVID-19 severity and in-hospital death: A meta-analysis of observational studies. Nutr. Metab. Cardiovasc Dis. 2020, 30, 1236–1248. [Google Scholar] [CrossRef] [PubMed]
- Bundeszentrale für gesundheitliche Aufklärung (BZgA). Diabetes und Coronavirus—Informationen über das SARS-CoV-2 für Menschen mit Diabetes 2020. Available online: https://www.deutsche-diabetes-gesellschaft.de/fileadmin/user_upload/06_Gesundheitspolitik/04_Aktivitaeten/Corona-Update/20200805-flyer_wickelfalz_Corona-BZgA.pdf (accessed on 6 October 2020).
- Bäuerle, A.; Graf, J.; Jansen, C.; Dörrie, N.; Junne, F.; Teufel, M.; Skoda, E.-M. An e-mental health intervention to support burdened people in times of the COVID-19 pandemic: CoPE It. J. Public Health (Oxf.) 2020, 42, 647–648. [Google Scholar] [CrossRef] [PubMed]
- Mak, I.W.; Chu, C.M.; Pan, P.C.; Yiu, M.G.; Chan, V.L. Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry 2009, 31, 318–326. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Diabetes Patients | Healthy Controls | ||
|---|---|---|---|---|
| N | % | N | % | |
| Sex | ||||
| Female | 188 | 74.3 | 196 | 77.5 |
| Male | 65 | 25.7 | 57 | 22.5 |
| Age | ||||
| 18–34 years | 62 | 24.5 | 68 | 26.8 |
| 35–54 years | 131 | 51.8 | 136 | 53.8 |
| 55–74 years | 59 | 23.4 | 47 | 18.6 |
| >74 years | 1 | 0.4 | 2 | 0.8 |
| Marital status | ||||
| Single | 64 | 25.3 | 66 | 26.1 |
| Married | 117 | 46.2 | 119 | 47.0 |
| In a relationship | 55 | 21.7 | 50 | 19.8 |
| Divorced/separated | 14 | 5.5 | 15 | 5.9 |
| Widowed | 3 | 1.2 | 3 | 1.2 |
| Educational level | ||||
| University education | 72 | 28.5 | 71 | 28.1 |
| Higher education entrance qualification | 87 | 34.4 | 84 | 33.2 |
| Intermediate secondary education | 63 | 24.9 | 57 | 22.5 |
| Lower secondary education | 29 | 11.5 | 38 | 15.0 |
| No qualification | 2 | 0.8 | 3 | 1.2 |
| City size | ||||
| 100,000 residents | 84 | 33.2 | 89 | 35.2 |
| 20,000 residents | 72 | 28.5 | 68 | 26.9 |
| 5000 residents | 41 | 16.2 | 37 | 14.6 |
| <5000 residents | 56 | 22.1 | 59 | 23.3 |
| Diabetes mellitus diagnosis | ||||
| Type 1 diabetes | 169 | 66.8 | - | - |
| Type 2 diabetes | 74 | 29.2 | - | - |
| Other diabetes diagnosis | 10 | 4.0 | - | - |
| Assessment of diabetes control | ||||
| Good | 126 | 49.8 | - | - |
| Average | 107 | 42.3 | - | - |
| Not good | 14 | 5.5 | - | - |
| I can’t tell | 6 | 2.4 | - | - |
| Accompanying illness(es) | ||||
| None | 122 | 48.2 | - | - |
| One | 54 | 21.3 | - | - |
| Two | 30 | 11.9 | - | - |
| More than two | 47 | 18.6 | - | - |
| Mental disorder(s) | ||||
| No | 184 | 72.7 | ||
| Yes | 69 | 27.3 | ||
| Total | 253 | 100.0 | 253 | 100.0 |
| Assessment instruments | Diabetes Patients (n = 253) | Healthy Controls (n = 253) | Statistical Analyses | ||
|---|---|---|---|---|---|
| M (SD) | M (SD) | t | p | d | |
| GAD-7 | 6.09 (5.20) | 6.45 (5.02) | −0.800 | 0.424 | - |
| PHQ-2 | 1.50 (1.75) | 1.56 (1.67) | −0.389 | 0.697 | - |
| COVID-19-related fear | 4.81 (1.69) | 4.35 (2.04) | 2.780 | 0.006 | 0.246 |
| Subjective level ofinformation | 5.83 (0.94) | 5.67 (1.19) | 1.647 | 0.100 | - |
| ASB | 5.86 (1.15) | 5.52 (1.65) | 2.757 | 0.006 | 0.239 |
| DSB | 2.92 (1.35) | 2.68 (1.31) | 2.084 | 0.038 | 0.180 |
| Diabetes Mellitus Diagnosis | Healthy Controls | ||||
|---|---|---|---|---|---|
| Type I (n = 169) | Type II (n = 74) | Other (n = 10) | (n = 253) | (n = 253) | |
| GAD-7 | |||||
| <5 | 78 (46.2%) | 34 (45.9%) | 6 (60.0%) | 118 (46.6%) | 103 (40.7%) |
| ≥5 | 52 (30.8%) | 20 (27.0%) | 2 (20.0%) | 74 (29.2%) | 93 (36.8%) |
| ≥10 | 29 (17.2%) | 11 (14.9%) | 1 (10.0%) | 41 (16.2%) | 39 (15.4%) |
| ≥15 | 10 (5.9%) | 9 (12.2%) | 1 (10.0%) | 20 (7.9%) | 18 (7.1%) |
| PHQ-2 | |||||
| <3 | 136 (80.5%) | 55 (74.3%) | 8 (80.0%) | 199 (78.7%) | 204 (80.6%) |
| ≥3 | 33 (19.5%) | 19 (25.7%) | 2 (20.0%) | 54 (21.3%) | 49 (19.4%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Musche, V.; Kohler, H.; Bäuerle, A.; Schweda, A.; Weismüller, B.; Fink, M.; Schadendorf, T.; Robitzsch, A.; Dörrie, N.; Tan, S.; et al. COVID-19-Related Fear, Risk Perception, and Safety Behavior in Individuals with Diabetes. Healthcare 2021, 9, 480. https://doi.org/10.3390/healthcare9040480
Musche V, Kohler H, Bäuerle A, Schweda A, Weismüller B, Fink M, Schadendorf T, Robitzsch A, Dörrie N, Tan S, et al. COVID-19-Related Fear, Risk Perception, and Safety Behavior in Individuals with Diabetes. Healthcare. 2021; 9(4):480. https://doi.org/10.3390/healthcare9040480
Chicago/Turabian StyleMusche, Venja, Hannah Kohler, Alexander Bäuerle, Adam Schweda, Benjamin Weismüller, Madeleine Fink, Theresa Schadendorf, Anita Robitzsch, Nora Dörrie, Susanne Tan, and et al. 2021. "COVID-19-Related Fear, Risk Perception, and Safety Behavior in Individuals with Diabetes" Healthcare 9, no. 4: 480. https://doi.org/10.3390/healthcare9040480
APA StyleMusche, V., Kohler, H., Bäuerle, A., Schweda, A., Weismüller, B., Fink, M., Schadendorf, T., Robitzsch, A., Dörrie, N., Tan, S., Teufel, M., & Skoda, E.-M. (2021). COVID-19-Related Fear, Risk Perception, and Safety Behavior in Individuals with Diabetes. Healthcare, 9(4), 480. https://doi.org/10.3390/healthcare9040480







