Development of a Logic Model for a Programme to Reduce the Magnetic Resonance Imaging Rate for Non-Specific Lower Back Pain in a Tertiary Care Centre
Abstract
1. Highlights
- Early access for lower back pain (LBP) for physiotherapy treatment will result in better patient’s reported outcomes.
- Successful implementation of this logic model will result in efficient utilisation of spine clinic.
2. Introduction
3. A Logic Model for Decreasing the MRI Rate of Persons with CLBP in Saudi Arabia
3.1. Development
3.2. The Context
3.3. Determinants
3.4. The Problem
3.5. The Evidence-Based Intervention
3.6. Proposed Study Objectives
- Promote patients’ accessibility to spine and physiotherapy services.
- Screening patients who present no red flag and early referral to physiotherapy will reduce the waiting time for patients with need for spine surgical intervention.
- Achieve higher levels of satisfaction among patients and staff.
- Early studies in Saudi Arabia showed an acceptability to physiotherapy referals without having MRI imaging [19]. Therefore, we aim to achieve high satisfaction among patients and healthcare workers with implementation of this program.
3.7. Proposed Study Sitting
3.8. Proposed Study Management Team
3.9. Partners and Stakeholders
3.10. Process Evaluation Objectives
- All musculoskeletal (MSK) physiotherapists will complete training to screen for risk factors for serious pathology (i.e., red flags) that require referrals to other services and for psychosocial risk factors (i.e., yellow flags). Physiotherapists have the competencies necessary to identify patients who present with serious pathology [31,32,33,34] and psychosocial impairments [35,36,37] and to refer patients to appropriate medical services.
- Trained physiotherapists will receive training to use the software required to make referrals in the electronic referral system.
- Trained physiotherapists and spine surgeons will complete additional training in their inter-professional education and collaborative practice. Despite the belief held by healthcare providers that they work in collaboration with other providers, they might use their skills to achieve a common goal but might not be fully aware of the clinical skills and roles of the other team members involved in the patient care. This lack of awareness may lead to the under-utilisation of other healthcare providers’ skills and capabilities, which could have a negative effect on the quality of care. Inter-professional education is an interactive learning experience of providers from more than one healthcare profession, which offers opportunities to improve the collaborative process and, eventually, patient care [36].
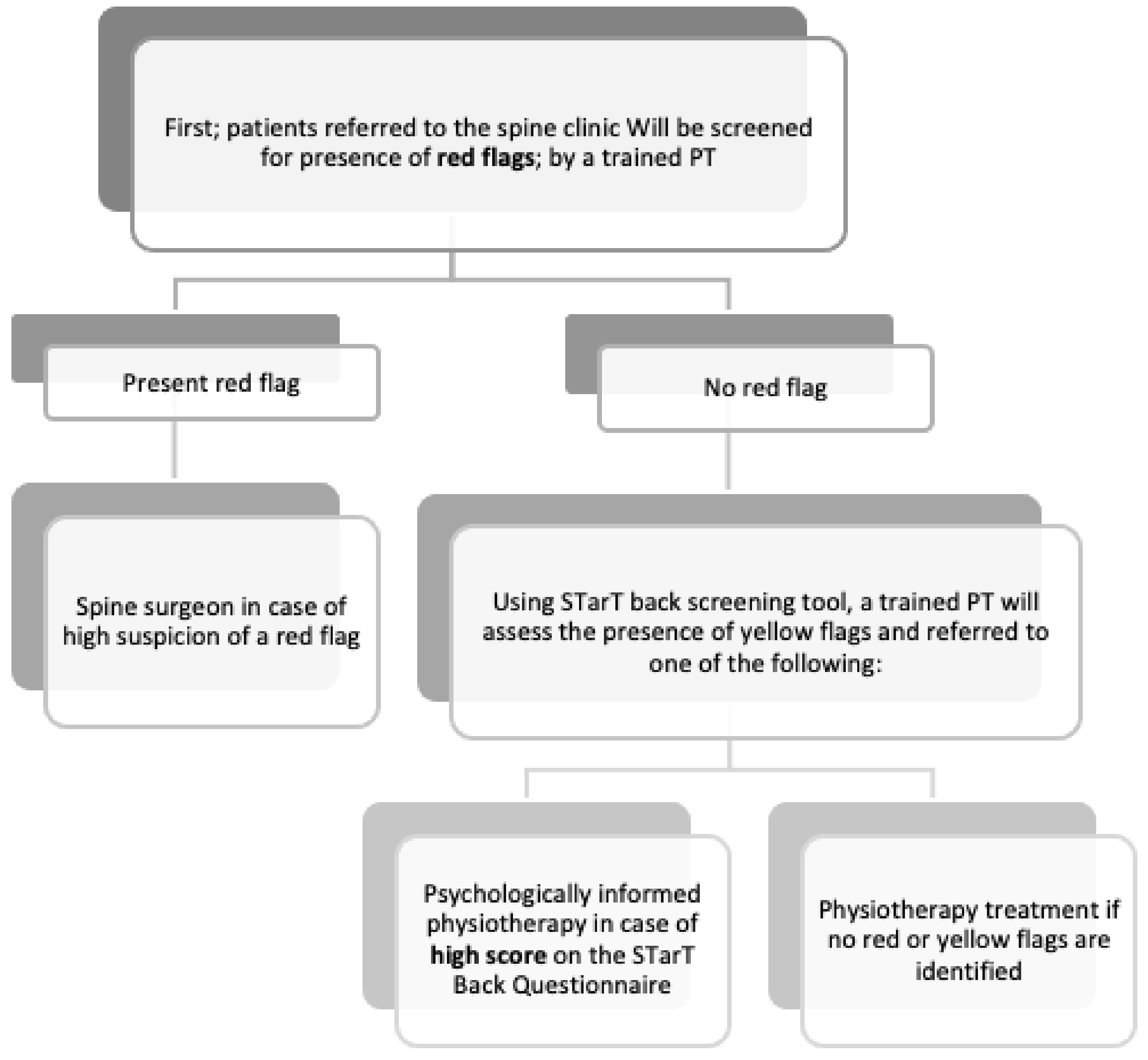
- After completing the aforementioned training, a physiotherapist will evaluate all patients on their first visit to the spine clinic and triage them (if needed) as candidates for surgery and consultation with a spine surgeon. The remaining patients will be screened for psychosocial risk factors using the STarT Back Screening Tool and subsequently referred to the appropriate service, i.e., physiotherapy or a psychologically informed physiotherapy intervention (see Figure 1).
- Prior to referral to the physiotherapy outpatient department, all patients will be educated by the screening physiotherapist about ways to manage their back pain and the importance of staying active. Patients identified as being at high or medium risk, according to the STarT Back Screening Tool, will receive psychosocial support in the form of a combined physical and psychologically informed physiotherapy intervention provided by the physiotherapy department.
3.11. Proposed Study Data Collection and Outcome Measures
3.12. Process Outcomes
- By the end of the pilot (6 months), there will be a 25% reduction in MRI referrals.
- By the end of the pilot (6 months), the waiting time to see a spine surgeon will decrease by 30%.
- By the end of the pilot (6 months), the accessibility of physiotherapy interventions will increase 30%.
- A clinically significant decrease in disability and pain outcomes.
- A clinically significant increase in self-efficacy and quality of life outcomes.
- By the end of the pilot (6 months), 90% of the patients will report a high level of satisfaction with the clinic.
3.13. Strategies and Activities
3.14. First Strategy
3.15. Second Strategy
3.16. Third Strategy
4. Evaluation
4.1. Initial Evaluation
- Number of LBP patients referred to the spine surgeon and time to access the service;
- Number of LBP patients referred to other specialists;
- Percentage and number of LBP patients referred to physiotherapy by spine surgeon and time to access the service;
- Percentage and number of LBP patients referred for MRIs.
4.2. Process Evaluation
- Percentage of patients referred to a spine surgeon.
- Percentage of patients referred to other specialists.
- Percentage of patients referred for physiotherapy.
- Percentage of patients referred for MRIs.
- Satisfaction level of the patients.
4.3. Impact Evaluation
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Waddell, G. Occupational health guidelines for the management of low back pain at work: Evidence review. Occup. Med. (Chic Ill) 2001, 51, 124–135. [Google Scholar] [CrossRef]
- Koes, B.W.; van Tulder, M.; Lin, C.-W.C.; Macedo, L.G.; McAuley, J.; Maher, C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. In Eur. Spine J.; 2010; 19, pp. 2075–2094. Available online: https://pubmed.ncbi.nlm.nih.gov/20602122 (accessed on 17 January 2021). [CrossRef]
- Stochkendahl, M.J.; Kjaer, P.; Hartvigsen, J.; Kongsted, A.; Aaboe, J.; Andersen, M.; Andersen, M.Ø.; Fournier, G.; Højgaard, B.; Jensen, M.B.; et al. National Clinical Guidelines for non-surgical treatment of patients with recent onset low back pain or lumbar radiculopathy. Eur. Spine J. 2017, 27, 60–75. [Google Scholar] [CrossRef]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef]
- Foster, N.E.; Anema, J.R.; Cherkin, D.; Chou, R.; Cohen, S.P.; Gross, D.P.; Ferreira, P.H.; Fritz, J.M.; Koes, B.W.; Peul, W.; et al. Prevention and treatment of low back pain: Evidence, challenges, and promising directions. Lancet 2018, 391, 2368–2383. [Google Scholar] [CrossRef]
- Buchbinder, R.; van Tulder, M.; Öberg, B.; Costa, L.M.; Woolf, A.; Schoene, M.; Croft, P. Low back pain: A call for action. Lancet 2018, 391, 2384–2388. [Google Scholar] [CrossRef]
- Webster, B.S.; Bauer, A.Z.; Choi, Y.; Cifuentes, M.; Pransky, G.S. Iatrogenic consequences of early magnetic resonance imaging in acute, work-related, disabling low back pain. Spine (Phila Pa 1976) 2013, 38, 1939–1946. Available online: https://pubmed.ncbi.nlm.nih.gov/23883826 (accessed on 15 January 2021). [CrossRef]
- Dagenais, S.; Galloway, E.K.; Roffey, D.M. A systematic review of diagnostic imaging use for low back pain in the United States. Spine J. 2014, 14, 1036–1048. [Google Scholar] [CrossRef]
- Jenkins, H.J.; Hancock, M.J.; French, S.D.; Maher, C.G.; Engel, R.M.; Magnussen, J.S. Effectiveness of interventions designed to reduce the use of imaging for low-back pain: A systematic review. CMAJ 2015, 187, 401–408. Available online: https://pubmed.ncbi.nlm.nih.gov/25733741 (accessed on 12 November 2020). [CrossRef] [PubMed]
- Berg, L.; Hellum, C.; Gjertsen, Ø.; Neckelmann, G.; Johnsen, L.G.; Storheim, K.; Brox, J.I.; Eide, G.E.; Espeland, A.; The Norwegian Spine Study Group. Do more MRI findings imply worse disability or more intense low back pain? A cross-sectional study of candidates for lumbar disc prosthesis. Skelet. Radiol. 2013, 42, 1593–1602. [Google Scholar] [CrossRef]
- Chou, R.; Fu, R.; Carrino, J.A.; Deyo, R.A. Imaging strategies for low-back pain: Systematic review and meta-analysis. Lancet 2009, 373, 463–472. [Google Scholar] [CrossRef]
- Kochen, M.M.; Blozik, E.; Scherer, M.; Chenot, J.-F. Imaging for low-back pain. Lancet 2009, 373, 436–437. [Google Scholar] [CrossRef]
- Alhowimel, A.; Alotaibi, M.; Coulson, N.; Radford, K. Psychosocial consequences of diagnosing nonspecific low-back pain radiologically: A qualitative study. Physiother. Theory Pract. 2020, 1–7. [Google Scholar] [CrossRef]
- Zusman, M. Belief reinforcement: One reason why costs for low back pain have not decreased. J. Multidiscip. Healthc. 2013, 6, 197–204. Available online: https://pubmed.ncbi.nlm.nih.gov/23717046 (accessed on 17 January 2021). [CrossRef]
- Serbic, D.; Pincus, T. Diagnostic uncertainty and recall bias in chronic low back pain. Pain 2014, 155, 1540–1546. [Google Scholar] [CrossRef]
- Fritz, J.M.; Brennan, G.P.; Hunter, S.J. Physical Therapy or Advanced Imaging as First Management Strategy Following a New Consultation for Low Back Pain in Primary Care: Associations with Future Health Care Utilization and Charges. Health Serv. Res. 2015, 50, 1927–1940. Available online: https://pubmed.ncbi.nlm.nih.gov/25772625 (accessed on 17 January 2021). [CrossRef]
- Blackmore, C.C.; Mecklenburg, R.S.; Kaplan, G.S. Effectiveness of Clinical Decision Support in Controlling Inappropriate Imaging. J. Am. Coll. Radiol. 2011, 8, 19–25. [Google Scholar] [CrossRef]
- Srinivas, S.V.; Deyo, R.A.; Berger, Z.D. Application of “Less Is More” to Low Back Pain. Arch Intern. Med. 2012, 172, 1016–1020. [Google Scholar] [CrossRef]
- Alhowimel, A.; Alotaibi, M.; Coulson, N.; Radford, K. Feasibility Study and Process Evaluation of MRI Plus Physiotherapy vs. Physiotherapy Alone in Non-Specific Chronic Low Back Pain among Patients in Saudi Arabia; Research Square: Durham, NC, USA, 2020. [Google Scholar] [CrossRef]
- Fritz, J.M.; Childs, J.D.; Wainner, R.S.; Flynn, T.W. Primary Care Referral of Patients with Low Back Pain to Physical Therapy. Spine (Phila Pa 1976) 2012, 37, 2114–2121. [Google Scholar] [CrossRef]
- Maeng, D.D.; Graboski, A.; Allison, P.L.; Fisher, D.Y.; Bulger, J.B. Impact of a value-based insurance design for physical therapy to treat back pain on care utilization and cost. J. Pain Res. 2017, 10, 1337–1346. Available online: https://pubmed.ncbi.nlm.nih.gov/28615965 (accessed on 12 November 2020). [CrossRef] [PubMed]
- Frogner, B.K.; Harwood, K.; Andrilla, C.H.A.; Schwartz, M.; Pines, J.M. Physical Therapy as the First Point of Care to Treat Low Back Pain: An Instrumental Variables Approach to Estimate Impact on Opioid Prescription, Health Care Utilization, and Costs. Health Serv. Res. 2018, 53, 4629–4646. Available online: https://pubmed.ncbi.nlm.nih.gov/29790166 (accessed on 1 December 2020). [CrossRef] [PubMed]
- Samsson, K.S.; Larsson, M.E.H. Physiotherapy triage assessment of patients referred for orthopaedic consultation—Long-term follow-up of health-related quality of life, pain-related disability and sick leave. Man. Ther. 2015, 20, 38–45. [Google Scholar] [CrossRef]
- Macfarlane, G.J.; Thomas, E.; Croft, P.R.; Papageorgiou, A.C.; Jayson, M.I.V.; Silman, A.J. Predictors of early improvement in low back pain amongst consulters to general practice: The influence of pre-morbid and episode-related factors. Pain 1999, 80, 113–119. [Google Scholar] [CrossRef]
- Crook, J.; Milner, R.; Schultz, I.Z.; Stringer, B. Determinants of Occupational Disability Following a Low Back Injury Handbook of Complex Occupational Disability Claims; Springer: New York, NY, USA, 2008; pp. 169–189. [Google Scholar] [CrossRef]
- Rihn, J.A.; Hilibrand, A.S.; Radcliff, K.; Kurd, M.; Lurie, J.; Blood, E.; Albert, T.J.; Weinstein, J.N. Duration of symptoms resulting from lumbar disc herniation: Effect on treatment outcomes: Analysis of the Spine Patient Outcomes Research Trial (SPORT). J. Bone Jt. Surg. Am. 2011, 93, 1906–1914. Available online: https://pubmed.ncbi.nlm.nih.gov/22012528 (accessed on 1 December 2020). [CrossRef] [PubMed]
- Smith, J.D.; Li, D.H.; Rafferty, M.R. The Implementation Research Logic Model: A method for planning, executing, reporting, and synthesizing implementation projects. Implement. Sci. 2020, 15, 84. Available online: https://pubmed.ncbi.nlm.nih.gov/32988389 (accessed on 17 January 2021). [CrossRef]
- Kindrachuk, D.R.; Fourney, D.R. Spine surgery referrals redirected through a multidisciplinary care pathway: Effects of nonsurgeon triage including MRI utilization. J. Neurosurg. Spine 2014, 20, 87–92. [Google Scholar] [CrossRef]
- Rampersaud, R.Y.; Bidos, A.; Fanti, C.L.; Young, B.W.; Drew, B.M.; Puskas, D.A. Preliminary Report from the Ontario Interprofessional Spine Assessment and Education Clinics (ISAEC). Spine J. 2014, 14, S40. [Google Scholar] [CrossRef]
- Zarrabian, M.; Bidos, A.; Fanti, C.; Young, B.; Drew, B.; Puskas, D.; Rampersaud, R. Improving spine surgical access, appropriateness and efficiency in metropolitan, urban and rural settings. Can. J. Surg. 2017, 60, 342–348. Available online: https://pubmed.ncbi.nlm.nih.gov/30246685 (accessed on 15 January 2021). [CrossRef]
- Jette, D.U.; Ardleigh, K.; Chandler, K.; McShea, L. Decision-Making Ability of Physical Therapists: Physical Therapy Intervention or Medical Referral. Phys. Ther. 2006, 86, 1619–1629. [Google Scholar] [CrossRef]
- Jette, D.U.; Halbert, J.; Iverson, C.; Miceli, E.; Shah, P. Use of Standardized Outcome Measures in Physical Therapist Practice: Perceptions and Applications. Phys. Ther. 2009, 89, 125–135. [Google Scholar] [CrossRef]
- Ferguson, F.; Holdsworth, L.; Rafferty, D. Low back pain and physiotherapy use of red flags: The evidence from Scotland. Physiotherapy 2010, 96, 282–288. [Google Scholar] [CrossRef]
- Leerar, P.J.; Boissonnault, W.; Domholdt, E.; Roddey, T. Documentation of Red Flags by Physical Therapists for Patients with Low Back Pain. J. Man. Manip. Ther. 2007, 15, 42–49. [Google Scholar] [CrossRef]
- Haggman, S.; Maher, C.G.; Refshauge, K.M. Screening for Symptoms of Depression by Physical Therapists Managing Low Back Pain. Phys. Ther. 2004, 84, 1157–1166. [Google Scholar] [CrossRef]
- Singla, M.; Jones, M.; Edwards, I.; Kumar, S. Physiotherapists’ assessment of patients’ psychosocial status: Are we standing on thin ice? A qualitative descriptive study. Man. Ther. 2015, 20, 328–334. [Google Scholar] [CrossRef]
- Nicholas, M.K.; Linton, S.J.; Watson, P.J.; Main, C.J. Early Identification and Management of Psychological Risk Factors (“Yellow Flags”) in Patients with Low Back Pain: A Reappraisal. Phys. Ther. 2011, 91, 737–753. [Google Scholar] [CrossRef]
- Delgado, D.A.; Lambert, B.S.; Boutris, N.; McCulloch, P.C.; Robbins, A.B.; Moreno, M.R.; Harris, J.D. Validation of Digital Visual Analog Scale Pain Scoring With a Traditional Paper-based Visual Analog Scale in Adults. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2018, 2, e088. Available online: https://pubmed.ncbi.nlm.nih.gov/30211382 (accessed on 11 December 2020). [CrossRef]
- Maki, D.; Rajab, E.; Watson, P.J.; Critchley, D.J. Cross-cultural Translation, Adaptation, and Psychometric Testing of the Roland-Morris Disability Questionnaire Into Modern Standard Arabic. Spine (Phila Pa 1976) 2014, 39, E1537–E1544. [Google Scholar] [CrossRef]
- Chiarotto, A.; Vanti, C.; Cedraschi, C.; Ferrari, S.; de Lima e Sà Resende, F.; Ostelo, R.W.; Pillastrini, P. Responsiveness and Minimal Important Change of the Pain Self-Efficacy Questionnaire and Short Forms in Patients with Chronic Low Back Pain. J. Pain 2016, 17, 707–718. [Google Scholar] [CrossRef]
- Algarni, F.S.; Alotaibi, A.N.; Altowaijri, A.M.; Al-Sobayel, H. Cross-Cultural Adaptation and Validation of the Arabic Version of Musculoskeletal Health Questionnaire (MSK-HQ-Ar). Int. J. Environ. Res. Public Health 2020, 17, 5168. Available online: https://pubmed.ncbi.nlm.nih.gov/32709115 (accessed on 2 February 2021). [CrossRef]
| Demographics and Disease-Related Characteristics | Baseline | At Discharge |
|---|---|---|
| Sex (M/F), no. (%) | √ | |
| Age (years) | √ | |
| Lower back pain duration (months) | √ | |
| Smoking (current (average per week)/previous (average per week)/never) | √ | |
| Diabetes (y/n) | √ | |
| Cardiovascular disease (y/n) | √ | |
| Dyslipidaemia (or treatment for this) (y/n) | √ | |
| Mental disorder (depression, anxiety) (y/n) | √ | |
| Height (cm) | √ | |
| Weight (kg) | √ | |
| Patient-reported outcome measures | ||
| Visual Analog Scale, VAS (0–10) | √ | √ |
| Roland Morris disability scale | √ | √ |
| Pain self-efficacy | √ | √ |
| Start back assessment tool | √ | |
| MSK-HQ | √ | √ |
| Satisfaction | ||
| Satisfaction survey | √ | |
| Determents | Actions | Outputs | Outcome | Impact |
|---|---|---|---|---|
Intervention Characteristics
|
|
|
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alhowimel, A.; Alodaibi, F.; Alotaibi, M.; Alamam, D.; Alsobayel, H.; Fritz, J. Development of a Logic Model for a Programme to Reduce the Magnetic Resonance Imaging Rate for Non-Specific Lower Back Pain in a Tertiary Care Centre. Healthcare 2021, 9, 238. https://doi.org/10.3390/healthcare9020238
Alhowimel A, Alodaibi F, Alotaibi M, Alamam D, Alsobayel H, Fritz J. Development of a Logic Model for a Programme to Reduce the Magnetic Resonance Imaging Rate for Non-Specific Lower Back Pain in a Tertiary Care Centre. Healthcare. 2021; 9(2):238. https://doi.org/10.3390/healthcare9020238
Chicago/Turabian StyleAlhowimel, Ahmed, Faris Alodaibi, Mazyad Alotaibi, Dalyah Alamam, Hana Alsobayel, and Julie Fritz. 2021. "Development of a Logic Model for a Programme to Reduce the Magnetic Resonance Imaging Rate for Non-Specific Lower Back Pain in a Tertiary Care Centre" Healthcare 9, no. 2: 238. https://doi.org/10.3390/healthcare9020238
APA StyleAlhowimel, A., Alodaibi, F., Alotaibi, M., Alamam, D., Alsobayel, H., & Fritz, J. (2021). Development of a Logic Model for a Programme to Reduce the Magnetic Resonance Imaging Rate for Non-Specific Lower Back Pain in a Tertiary Care Centre. Healthcare, 9(2), 238. https://doi.org/10.3390/healthcare9020238







