Panic and Trust during COVID-19: A Cross-Sectional Study on Immigrants in South Korea
Abstract
1. Introduction
Panic and Institutional Trust during the COVID-19 Pandemic
2. Materials and Methods
2.1. Study Design and Setting
2.2. Participants
2.3. Variables and Measurements
- 1.
- How much do you trust the health system in the country to fully contain the spread of COVID19?
- 2.
- How trustworthy is information provided about COVID19 by your nearest health institution?
- 3.
- How trustworthy is your local media while disseminating COVID19 related public announcements?
- 4.
- How responsive is your local community in collaborating with the instructions of health care officials?
2.4. Bias
2.5. Study Size
2.6. Procedure
3. Results
3.1. Adult Panic Severity and Trust Test Results
3.2. Panic: Immigrants vs. Koreans
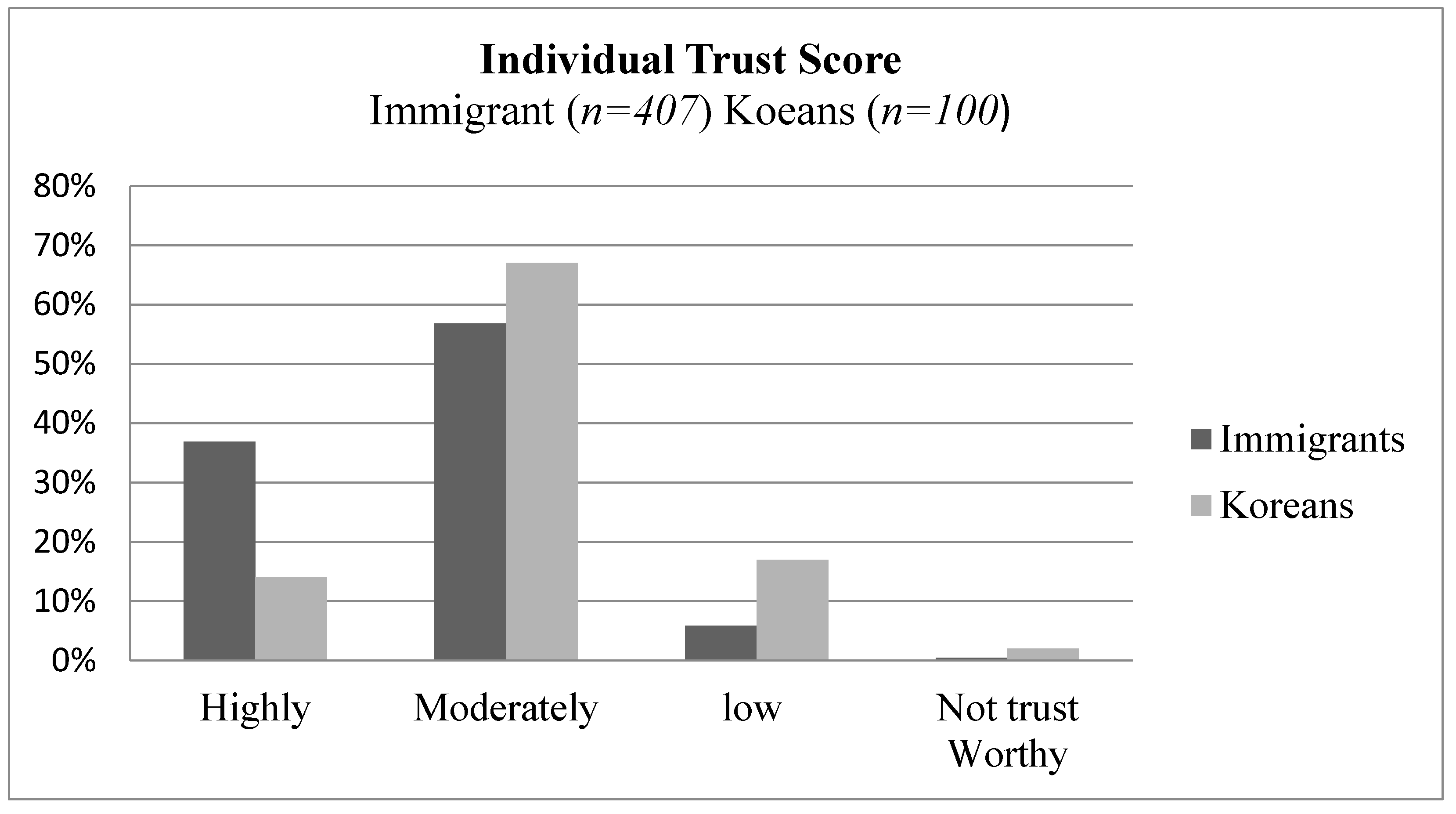
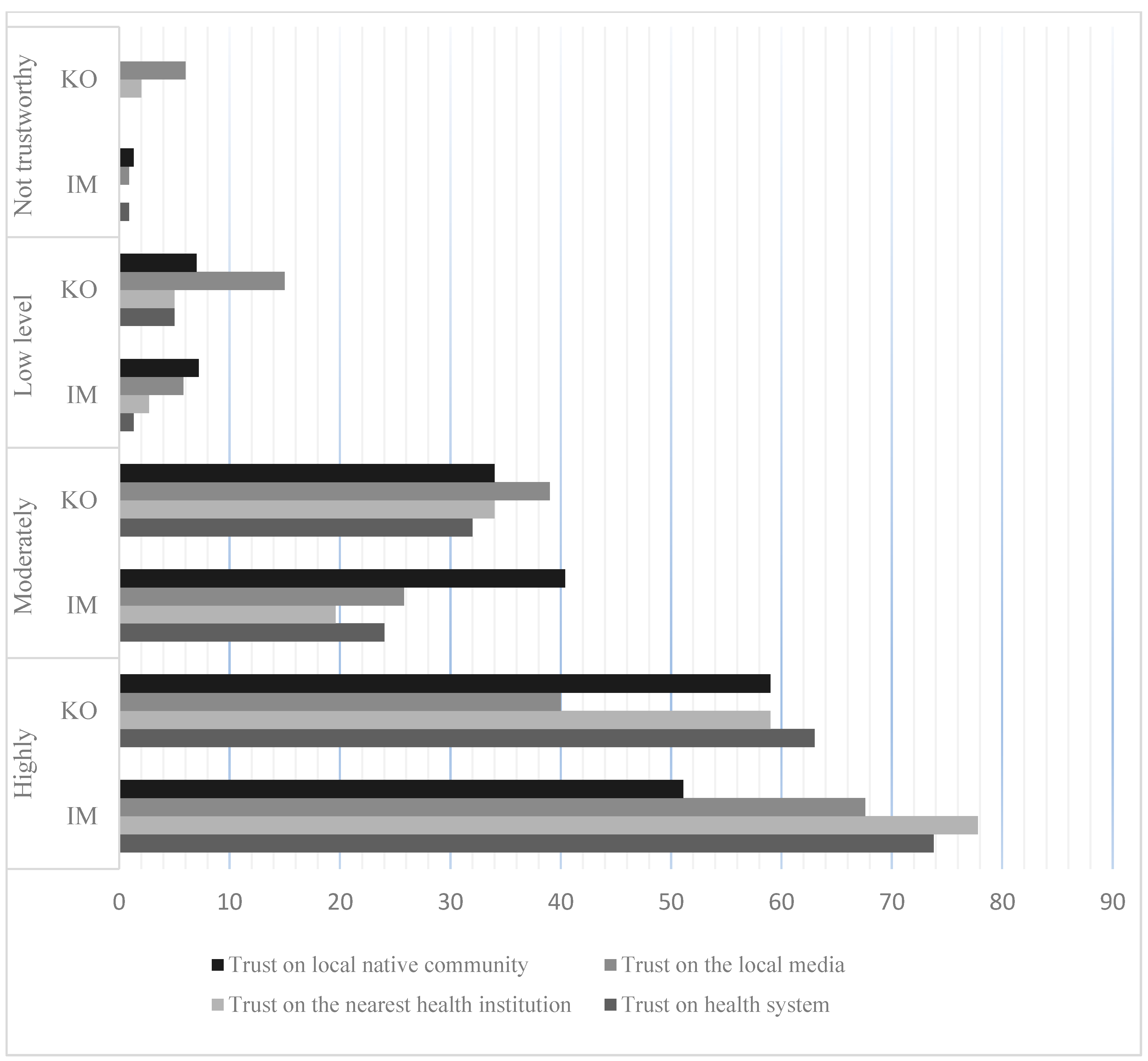
3.3. Trust: Immigrants vs. Koreans
4. Discussion
5. Conclusions
6. Limitations of the Study
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. WHO Coronavirus Disease (COVID-19) Dashboard/Republic of Korea. Available online: https://covid19.who.int/region/wpro/country/kr (accessed on 15 January 2021).
- Dudden, A.; Marks, A. South Korea Took Rapid, Intrusive Measures against Covid-19—and They Worked. The Guardian. Available online: https://www.theguardian.com/commentisfree/2020/mar/20/south-korea-rapid-intrusive-measures-covid-19 (accessed on 20 March 2020).
- Duan, L.; Zhu, G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry 2020, 7, 300–302. [Google Scholar] [CrossRef]
- Isaacs, D.; Britton, P.N.; Preisz, A. Ethical reflections on the COVID-19 pandemic: The epidemiology of panic. J. Pediatrics Child Health 2020, 56, 690. [Google Scholar] [CrossRef] [PubMed]
- Peckham, R. The COVID-19 Outbreak Has Shown We Need Strategies to Manage Panic during Epidemics. BMJ. Available online: https://blogs.bmj.com/bmj/2020/02/21/robert-peckham-covid-19-outbreak-need-strategies-manage-panic-epidemics/ (accessed on 21 February 2020).
- Nickell, L.A.; Crighton, E.J.; Tracy, C.S.; Al-Enazy, H.; Bolaji, Y.; Hanjrah, S.; Upshur, R.E. Psychosocial effects of SARS on hospital staff: Survey of a large tertiary care institution. Can. Med Assoc. J. 2004, 170, 793–798. [Google Scholar] [CrossRef]
- Maunder, R.; Hunter, J.; Vincent, L.; Bennett, J.; Peladeau, N.; Leszcz, M.; Mazzulli, T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. Can. Med. Assoc. J. 2003, 168, 1245–1251. [Google Scholar]
- Chong, M.-Y.; Wang, W.-C.; Hsieh, W.-C.; Lee, C.-Y.; Chiu, N.-M.; Yeh, W.-C.; Huang, O.-L.; Wen, J.-K.; Chen, C.-L. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br. J. Psychiatry 2004, 185, 127–133. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Xiang, Y.-T.; Yang, Y.; Li, W.; Zhang, L.; Zhang, Q.; Cheung, T.; Ng, C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020, 7, 228–229. [Google Scholar] [CrossRef]
- Strong, P. Epidemic psychology: A model. Sociol. Health Illn. 1990, 12, 249–259. [Google Scholar] [CrossRef]
- Dynes, R.R. Disasters, Collective Behavior and Social Organization; Tierney, K.J., Ed.; University of Delaware Press: Newark, DE, USA, 1994. [Google Scholar]
- Glass, T.A.; Schoch-Spana, M. Bioterrorism and the people: How to vaccinate a city against panic. Clin. Infect. Dis. 2002, 34, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Berger, Z.D.; Evans, N.G.; Phelan, A.L.; Silverman, R.D. Covid-19: Control measures must be equitable and inclusive. BMJ 2020, 368, m1141. [Google Scholar] [CrossRef]
- Guadagno, L. Migrants and the COVID-19 Pandemic: An Initial Analysis; Migration Research Series; International Organization for Migration: Geneva, Switzerland, 2020; p. 60. [Google Scholar]
- Buchanan, L.; Patel, J.K.; Rosenthal, B.M.; Singhvi, A. Rosenthal and A. Singhvi A month of Coronavirus in New York City: See the hardest-hit areas. The New York Times, 1 April 2020. [Google Scholar]
- Collins, F.L. Caring for 300,000 temporary migrants in New Zealand is a crucial missing link in our coronavirus response. The Conversation, 26 March 2020. [Google Scholar]
- Chishti, M.; Pierce, S. Crisis within a crisis: Immigration in the United States in a time of COVID-19. Migration Information Source. The Online Journal of the Migration Policy Institute, 26 March 2020. [Google Scholar]
- Charles, C.H. Canada′s changing coronavirus border policy exposes international students′ precarious status. The Conversation, 19 March 2020. [Google Scholar]
- Chia, J.; Poh, Y.H. Amid COVID-19 crisis, Southeast Asia′s migrant workers fall through the cracks. The Diplomat, 31 March 2020. [Google Scholar]
- Arfaat, M. Rohingya refugees need a coronavirus lifeline, not an internet ban. The New Humanit, 24 March 2020. [Google Scholar]
- Bauomy, J. COVID-19 and xenophobia: Why outbreaks are often accompanied by racism. Euronews, 6 March 2020. [Google Scholar]
- White, A.R. Historical linkages: Epidemic threat, economic risk, and xenophobia. Lancet 2020, 395, 1250–1251. [Google Scholar] [CrossRef]
- Hargreaves, S.; Rustage, K.; Nellums, L.B.; McAlpine, A.; Pocock, N.; Devakumar, D.; Aldridge, R.W.; Abubakar, I.; Kristensen, K.L.; Himmels, J.W.; et al. Occupational health outcomes among international migrant workers: A systematic review and meta-analysis. Lancet Glob. Health 2019, 7, 872–882. [Google Scholar] [CrossRef]
- Liem, A.; Wang, C.; Wariyanti, Y.; A Latkin, C.; Hall, B.J. The neglected health of international migrant workers in the COVID-19 epidemic. Lancet Psychiatry 2020, 7, 20. [Google Scholar] [CrossRef]
- Islam, S.; Ferdous, M.Z.; Potenza, M.N. Panic and generalized anxiety during the COVID-19 pandemic among Bangladeshi people: An online pilot survey early in the outbreak. J. Affect. Disord. 2020, 276, 30–37. [Google Scholar] [CrossRef]
- Ventriglio, A.; Watson, C.; Bhugra, D. Pandemics, panic and prevention: Stages in the life of COVID-19 pandemic. Int. J. Soc. Psychiatry 2020, 66, 733–734. [Google Scholar] [CrossRef]
- Clark, D.M. A cognitive approach to panic. Behav. Res. Ther. 1986, 24, 461–470. [Google Scholar] [CrossRef]
- Tversky, A.; Kahneman, D. Judgment under uncertainty: Heuristics and biases. Science 1974, 185, 1124–1131. [Google Scholar] [CrossRef] [PubMed]
- Neria, Y.; Sullivan, G.M. Understanding the mental health effects of indirect exposure to mass trauma through the media. JAMA 2011, 306, 1374–1375. [Google Scholar] [CrossRef]
- Nicomedes, C.J.; Avila, R.M. An analysis on the panic during COVID-19 pandemic through an online form. J. Affect. Disord. 2020, 276, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Sherlaw, W.; Raude, J. Why the French did not choose to panic: A dynamic analysis of the public response to the influenza pandemic. Sociol. Health Illn. 2013, 35, 332–344. [Google Scholar] [CrossRef] [PubMed]
- Easton, D. A Systems Analysis of Political Life; John Wiley: New York, NY, USA, 1968. [Google Scholar]
- Bouckaert, G.; Van de Walle, S. Comparing measures of citizen trust and user satisfaction as indicators of good governance: Difficulties in linking trust and satisfaction indicators. Int. Rev. Adm. Sci. 2003, 69, 329–343. [Google Scholar] [CrossRef]
- Gopichandran, V.; Subramaniam, S.; Kalsingh, M.J. COVID-19 pandemic: A litmus test of trust in the health system. Asian Bioeth. Rev. 2020, 12, 213–221. [Google Scholar] [CrossRef]
- Bargain, O.; Aminjonov, U. Trust and Compliance to Public Health Policies in Times of COVID-19. J. Public Econ. 2020, 192, 104316. [Google Scholar] [CrossRef] [PubMed]
- Lovari, A. Spreading (dis) trust: Covid-19 misinformation and government intervention in Italy. Media Commun. 2020, 8, 458–461. [Google Scholar] [CrossRef]
- Hartley, K.; Jarvis, D.S. Policymaking in a low-trust state: Legitimacy, state capacity, and responses to COVID-19 in Hong Kong. Policy Soc. 2020, 39, 403–423. [Google Scholar] [CrossRef]
- Wong, C.M.; Jensen, O. The paradox of trust: Perceived risk and public compliance during the COVID-19 pandemic in Singapore. J. Risk Res. 2020, 23, 1021–1030. [Google Scholar] [CrossRef]
- Earle, T.C. Trust in Cooperative Risk Management: Uncertainty and Scepticism in the Public Mind; Routledge: Oxfordshire, UK, 2012. [Google Scholar]
- Earle, T.C. Trust in risk management: A model-based review of empirical research. Risk Anal. Int. J. 2010, 30, 541–574. [Google Scholar] [CrossRef]
- Röder, A.; Mühlau, P. Low expectations or different evaluations: What explains immigrants’ high levels of trust in host-country institutions? J. Ethn. Migr. Stud. 2012, 38, 777–792. [Google Scholar] [CrossRef]
- Craske, M.; Wittchen, U.; Bogels, S.; Stein, M.; Andrews, G.; Lebeu, R. Severity Measure for Panic Disorder—Adult [Measurement Instrument]. American Psychiatric Association, 2013. Available online: https://www.psychiatry.org/psychiatrists/practice/dsm/educational-resources/assessment-measures (accessed on 12 June 2020).
- Korean Immigration Service 2018. Immigration. Immigrant Policy Statistical Report. Available online: http://www.moj.go.kr/viewer/skin/doc.html?rs=/viewer/result/bbs/160&fn=temp_1548720809280100 (accessed on 12 December 2018).
- Stirling, C. Re: Covid-19: Control measures must be equitable and inclusive (letter to Editor). BMJ 2020, 368, m1141. [Google Scholar] [CrossRef]
- Ladner, D.; Katsumasa, H.; Kyuri, K. The Republic of Korea′s first 70 days of responding to the COVID-19 outbreak. Glob. Deliv. Initiat. Case Study. Available online: http://www.globaldeliveryinitiative.org/sites/default/files/case-studies/case_study_of_korea_response_to_covid19.pdf (accessed on 11 February 2020).

| Immigrants in South Korea (n = 407) | Koreans (n = 100) | ||||
|---|---|---|---|---|---|
| Item | N | % | N | % | |
| Sex | Male | 207 | 49.1 | 49 | 49 |
| Female | 200 | 50.4 | 51 | 51 | |
| Age | 18–25 | 35 | 8.6 | 9 | 9 |
| 26–35 | 225 | 55.3 | 56 | 56 | |
| 36–45 | 92 | 22.6 | 23 | 23 | |
| 46–55 | 42 | 10.3 | 10 | 10 | |
| Above 56 | 13 | 9.1 | 7 | 7 | |
| Occupation | Employed | 190 | 46.7 | 47 | 47 |
| Self-employed/Freelancer | 20 | 4.9 | 5 | 5 | |
| Student | 168 | 41.3 | 41 | 41 | |
| Unemployed | 15 | 3.7 | 4 | 4 | |
| other | 13 | 3.2 | 3 | 3 | |
| Locations | Seoul city | 181 | 44.4 | 44 | 44 |
| Daegu city | 52 | 12.7 | 13 | 13 | |
| Busan city | 42 | 10.3 | 10 | 10 | |
| Incheon city | 22 | 5.4 | 6 | 6 | |
| Gwanju city | 31 | 7.6 | 8 | 8 | |
| Gyeonggi province | 49 | 12 | 12 | 12 | |
| Gangwon province | 30 | 7.3 | 7 | 7 | |
| Nationality | China | 181 | 44.4 | ||
| USA | 43 | 10.5 | |||
| Nigeria | 23 | 5.6 | |||
| Ethiopia | 23 | 5.6 | |||
| Canada | 20 | 4.9 | |||
| Bangladesh | 18 | 4.4 | |||
| Others * | 99 | 24.3 | |||
| Item | Immigrants (n = 407) | Koreans (n = 100) | |||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| 1 | I felt moments of sudden terror, fear or fright because of the spread of COVID19 in/around my city | 1.15 | 0.98 | 1.8 | 1.3 |
| 2 | I felt anxious, worried, or nervous about getting infected with COVID19 | 1.39 | 1.06 | 2.0 | 1.35 |
| 3 | I had thoughts of losing control, dying, going crazy, or other bad things happening because of COVID19 in my area. | 0.69 | 0.99 | 1.0 | 1.1 |
| 4 | I felt a racing heart, sweaty, trouble breathing, faint, or shaky because of the spread of COVID19 in/around my city | 0.24 | 0.56 | 0.39 | 0.9 |
| 5 | I felt tense muscles, felt on edge or restless, or had trouble relaxing or trouble to sleep because of the spread of COVID19 in/around my city | 0.53 | 0.8 | 0.6 | 1.0 |
| 6 | I avoided, or did not approach or enter, situations that reminded you of the spread of COVID19 | 1.5 | 1.3 | 1.1 | 1.3 |
| 7 | I developed a new routine, or participated only minimally in social activities, because of the fear of getting infected by COVID19 | 2.56 | 1.2 | 2.50 | 1.23 |
| 8 | I spent a lot of time preparing for situations in which I might avoid the troubles of getting infected by COVID19 | 1.81 | 1.3 | 2.1 | 0.84 |
| 9 | I distracted myself to avoid thinking about the current situations of COVID19 in my area. | 1.46 | 1.28 | 0.8 | 0.9 |
| 10 | I needed help to cope with the fear of COVID19 spreading rapidly (e.g., alcohol or medication, superstitious objects, prayer, other people) | 0.89 | 1.18 | 0.56 | 0.94 |
| Item | Group | n | Mean Rank | Sum of | U | p | |
|---|---|---|---|---|---|---|---|
| 1 | I felt moments of sudden terror, fear or fright because of the spread of COVID19 in/around my city | IM | 405 | 237.16 | 96,049 | 13,834 | 0.000 *** |
| K | 100 | 317.16 | 31,716 | ||||
| 2 | I felt anxious, worried, or nervous about getting infected with COVID19 | IM | 407 | 241 | 98,121.50 | 15,093.5 | 0.000 *** |
| K | 100 | 306.57 | 30,656.50 | ||||
| 3 | I had thoughts of losing control, dying, going crazy, or other bad things happening because of COVID19 in my area. | IM | 407 | 245.12 | 99,764 | 16,736 | 0.002 ** |
| K | 100 | 290.14 | 29,014 | ||||
| 4 | I felt a racing heart, sweaty, trouble breathing, faint, or shaky because of the spread of COVID19 in/around my city | IM | 407 | 251.68 | 102,433.50 | 19,405.5 | 0.291 |
| K | 100 | 263.45 | 26,344.50 | ||||
| 5 | I felt tense muscles, felt on edge or restless, or had trouble relaxing or trouble to sleep because of the spread of COVID19 | IM | 407 | 254.17 | 103,447 | 20,281 | 0.951 |
| K | 100 | 253.31 | 25,331 | ||||
| 6 | I avoided, or did not approach or enter, situations that reminded me of the spread of COVID19 | IM | 407 | 262.15 | 106,697 | 17,031 | 0.009 ** |
| K | 100 | 220.81 | 22,081 | ||||
| 7 | I developed a new routine, or participated only minimally in social activities, because of the fear of getting infected by COVID19 | IM | 407 | 255.48 | 103,978.50 | 19,749.5 | 0.635 |
| K | 100 | 248.00 | 24,799.50 | ||||
| 8 | I spent a lot of time preparing for situations in which I might avoid the troubles of getting infected by COVID19 | IM | 407 | 244.81 | 99,636 | 16,608 | 0.005 ** |
| K | 99 | 289.24 | 28,635 | ||||
| 9 | I distracted myself to avoid thinking about the current situations of COVID19 in my area. | IM | 407 | 220.85 | 89,884 | 6856 | 0.000 *** |
| K | 100 | 388.94 | 38,894 | ||||
| 10 | I needed help to cope with the fear of COVID19 spreading rapidly (e.g., alcohol or medication, superstitious objects, prayer, other people) | IM | 407 | 261.88 | 106,586.50 | 17,141.5 | 0.007 ** |
| K | 100 | 221.92 | 22,191.50 |
| Item | Group | n | Mean Rank | Sum of | U | p | |
|---|---|---|---|---|---|---|---|
| 1 | Trust on health system | IM | 407 | 294.45 | 119,840 | 3888 | 0.000 *** |
| K | 100 | 89.38 | 8938 | ||||
| 2 | Trust on the nearest health institution | IM | 407 | 296.20 | 120,554 | 3174 | 0.000 *** |
| K | 100 | 82.24 | 8224 | ||||
| 3 | Trust on the local media | IM | 407 | 293.99 | 119,654 | 4074 | 0.000 *** |
| K | 100 | 91.24 | 9124 | ||||
| 4 | Trust on local native community | IM | 403 | 284.65 | 114,713.5 | 6992.5 | 0.000 *** |
| K | 100 | 120.43 | 12,042.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoon, M.S.; Feyissa, I.F.; Suk, S.-W. Panic and Trust during COVID-19: A Cross-Sectional Study on Immigrants in South Korea. Healthcare 2021, 9, 199. https://doi.org/10.3390/healthcare9020199
Yoon MS, Feyissa IF, Suk S-W. Panic and Trust during COVID-19: A Cross-Sectional Study on Immigrants in South Korea. Healthcare. 2021; 9(2):199. https://doi.org/10.3390/healthcare9020199
Chicago/Turabian StyleYoon, Myeong Sook, Israel Fisseha Feyissa, and So-Won Suk. 2021. "Panic and Trust during COVID-19: A Cross-Sectional Study on Immigrants in South Korea" Healthcare 9, no. 2: 199. https://doi.org/10.3390/healthcare9020199
APA StyleYoon, M. S., Feyissa, I. F., & Suk, S.-W. (2021). Panic and Trust during COVID-19: A Cross-Sectional Study on Immigrants in South Korea. Healthcare, 9(2), 199. https://doi.org/10.3390/healthcare9020199







