Use of Soft Cervical Collar among Whiplash Patients in Two Italian Emergency Departments Is Associated with Persistence of Symptoms: A Propensity Score Matching Analysis
Abstract
1. Introduction
2. Methods
2.1. Study Design
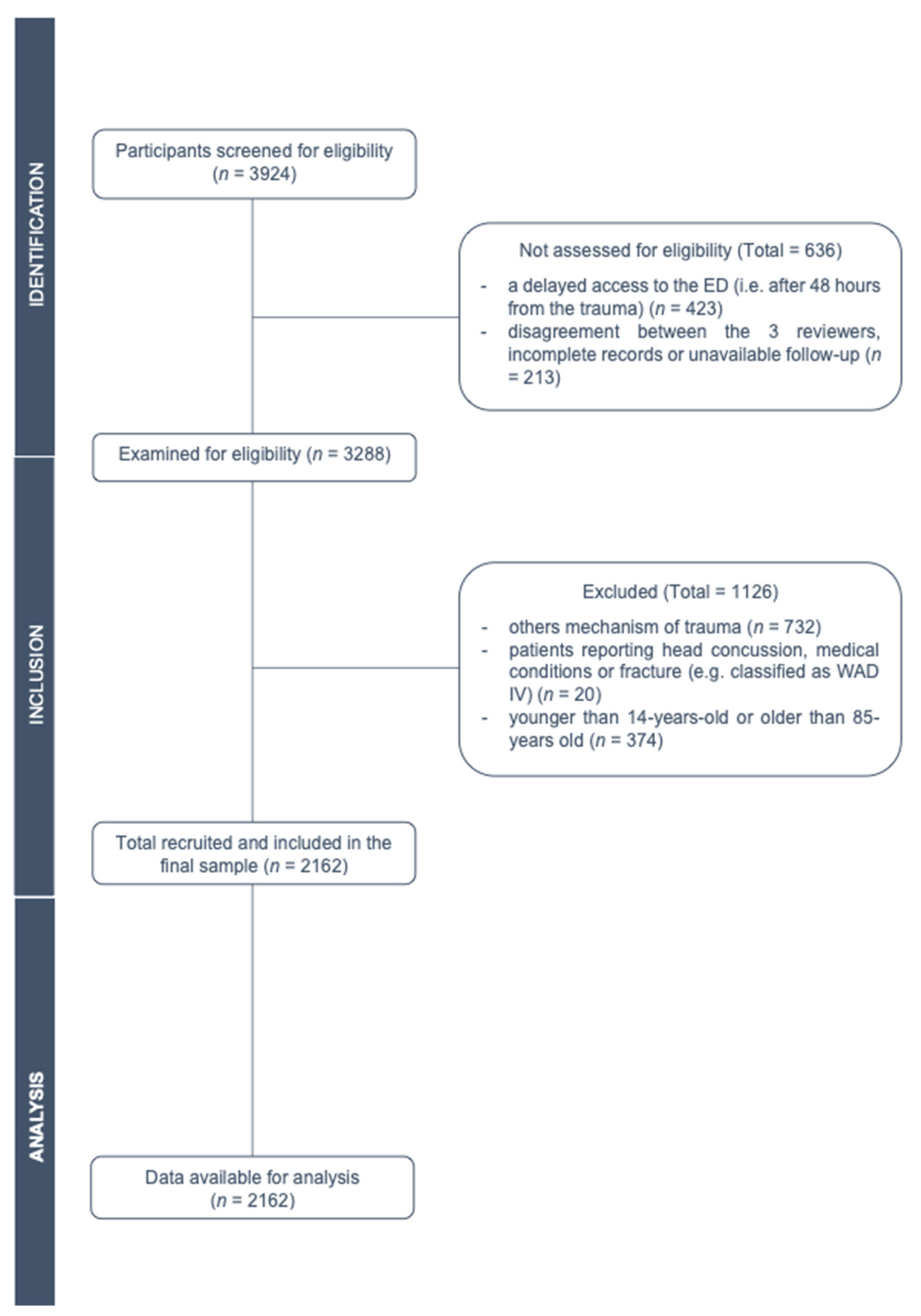
2.2. Patients Eligibility Criteria
2.3. Dataset Creation
2.4. Intervention and Outcomes
2.5. Data Processing and Analysis
3. Results
3.1. Baseline Characteristics and Clinical Variables
3.2. Variable Associated with a Return within 3 Months to the ED
3.3. Propensity Score Matching for Soft Cervical Collar Application and for the Return to the ED
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Spitzer, W.; Skovron, M.L.; Salmi, L.R.; Cassidy, J.D.; Duranceau, J.; Suissa, S.; Zeiss, E. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: Redefining “whiplash” and its management. Spine 1995, 20, 1S–73S. [Google Scholar]
- Jull, G. Whiplash Continues Its Challenge. J. Orthop. Sports Phys. Ther. 2016, 46, 815–817. [Google Scholar] [CrossRef]
- Joslin, C.C.; Khan, S.N.; Bannister, G. Long-term disability after neck injury. J. Bone Jt. Surg. Br. Vol. 2004, 86, 1032–1034. [Google Scholar] [CrossRef]
- Bussières, A.E.; Stewart, G.; Al-Zoubi, F.; Decina, P.; Descarreaux, M.; Hayden, J.; Hendrickson, B.; Hincapié, C.; Pagé, I.; Passmore, S.; et al. The Treatment of Neck Pain–Associated Disorders and Whiplash-Associated Disorders: A Clinical Practice Guideline. J. Manip. Physiol. Ther. 2016, 39, 523–564.e27. [Google Scholar] [CrossRef]
- Verhagen, A.P.; Scholten-Peeters, G.G.; Van Wijngaarden, S.; De Bie, R.; Bierma-Zeinstra, S.M. Conservative treatments for whiplash. Cochrane Database Syst. Rev. 2007, 2, CD003338. [Google Scholar] [CrossRef]
- Holm, L.W.; Carroll, L.J.; Cassidy, J.D.; Hogg-Johnson, S.; Côté, P.; Guzman, J.; Peloso, P.; Nordin, M.; Hurwitz, E.; Van Der Velde, G.; et al. The Burden and Determinants of Neck Pain in Whiplash-Associated Disorders After Traffic Collisions. Eur. Spine J. 2008, 17, 52–59. [Google Scholar] [CrossRef]
- Casellario Centrale Infortuni. Banca Dati del Fenomeno Infortunistico. Infortuni con Colpo di Frusta per Luogo di Accadimento. Available online: https://casellariosol.inail.it/RapportoStatistico/InfRcaCarInf.do?method=infortuniColpoFrustaRegioneAcc&menuId=tre_due_i (accessed on 5 September 2020).
- Häggman-Henrikson, B.; Lampa, E.; Marklund, S.; Wänman, A. Pain and Disability in the Jaw and Neck Region following Whiplash Trauma. J. Dent. Res. 2016, 95, 1155–1160. [Google Scholar] [CrossRef]
- Côté, P.; Wong, J.J.; Sutton, D.; Shearer, H.M.; Mior, S.; Randhawa, K.; Ameis, A.; Carroll, L.; Nordin, M.; Yu, H.; et al. Management of neck pain and associated disorders: A clinical practice guideline from the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Eur. Spine J. 2016, 25, 2000–2022. [Google Scholar] [CrossRef] [PubMed]
- Pajediene, E.; Janusauskaite, J.; Samusyte, G.; Stasaitis, K.; Petrikonis, K.; Bileviciute-Ljungar, I. Patterns of acute whiplash-associated disorder in the Lithuanian population after road traffic accidents. J. Rehabil. Med. 2015, 47, 52–57. [Google Scholar] [CrossRef] [PubMed]
- García, D.V.; Doorduin, J.; Willemsen, A.T.; Dierckx, R.A.; Otte, A. Altered Regional Cerebral Blood Flow in Chronic Whiplash Associated Disorders. EBioMedicine 2016, 10, 249–257. [Google Scholar] [CrossRef]
- Merrick, D.; Stålnacke, B.-M. Five years post whiplash injury: Symptoms and psychological factors in recovered versus non-recovered. BMC Res. Notes 2010, 3, 190. [Google Scholar] [CrossRef]
- Elliott, J.M.; Walton, D.M. How Do We Meet the Challenge of Whiplash? J. Orthop. Sports Phys. Ther. 2017, 47, 444–446. [Google Scholar] [CrossRef]
- Coppieters, I.; De Pauw, R.; Caeyenberghs, K.; Danneels, L.; Kregel, J.; Pattyn, A.; Meeus, M.; Cagnie, B. Decreased Regional Grey Matter Volume in Women with Chronic Whip-lash-Associated Disorders: Relationships with Cognitive Deficits and Disturbed Pain Processing. Pain Phys. 2017, 20, E1025–E1051. Available online: http://www.ncbi.nlm.nih.gov/pubmed/29149149 (accessed on 4 August 2020). [CrossRef]
- Sterling, M. Physiotherapy management of whiplash-associated disorders (WAD). J. Physiother. 2014, 60, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Ritchie, C.; Hendrikz, J.; Jull, G.; Elliott, J.; Sterling, M. External Validation of a Clinical Prediction Rule to Predict Full Recovery and Ongoing Moderate/Severe Disability Following Acute Whiplash Injury. J. Orthop. Sports Phys. Ther. 2015, 45, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Ritchie, C.; Sterling, M. Recovery Pathways and Prognosis After Whiplash Injury. J. Orthop. Sports Phys. Ther. 2016, 46, 851–861. [Google Scholar] [CrossRef]
- Söderlund, A.; Löfgren, M.; Stålnacke, B.-M. Predictors before and after multimodal rehabilitation for pain acceptance and engagement in activities at a 1-year follow-up for patients with whiplash-associated disorders (WAD)—A study based on the Swedish Quality Registry for Pain Rehabilitation (SQRP). Spine J. 2018, 18, 1475–1482. [Google Scholar] [CrossRef]
- Campbell, L.; Smith, A.; McGregor, L.; Sterling, M. Psychological Factors and the Development of Chronic Whiplash–associated Disorder(s). Clin. J. Pain 2018, 34, 755–768. [Google Scholar] [CrossRef]
- Strudwick, K.; McPhee, M.; Bell, A.; Martin-Khan, M.; Russell, T. Review article: Best practice management of neck pain in the emergency department (part 6 of the musculoskeletal injuries rapid review series). Emerg. Med. Australas. 2018, 30, 754–772. [Google Scholar] [CrossRef]
- Carlesso, L.C.; MacDermid, J.C.; Gross, A.R.; Walton, D.M.; Santaguida, P.L. Treatment preferences amongst physical therapists and chiropractors for the management of neck pain: Results of an international survey. Chiropr. Man. Ther. 2014, 22, 11. [Google Scholar] [CrossRef]
- Rosenfeld, M.; Seferiadis, A.; Carlsson, J.; Gunnarsson, R.K. Active Intervention in Patients with Whiplash-Associated Disorders Improves Long-Term Prognosis. Spine 2003, 28, 2491–2498. [Google Scholar] [CrossRef] [PubMed]
- Bonk, A.D.; Ferrari, R.; Giebel, G.D.; Edelan, M.; Huser, R. Prospective, randomized, controlled study of active versus collar, and the natural history for whiplash injury, in Germany. J. Musculoskelet. Pain. 2000, 8, 123–132. [Google Scholar] [CrossRef]
- Kongsted, A.; Qerama, E.; Kasch, H.; Bendix, T.; Winther, F.; Korsholm, L.; Jensen, T.S. Neck Collar, “Act-as-Usual” or Active Mobilization for Whiplash Injury? Spine 2007, 32, 618–626. [Google Scholar] [CrossRef]
- Christensen, S.W.M.; Skou, S.T. Letter to the Editor concerning “The role of non-rigid cervical collar in pain relief and functional restoration after whiplash injury: A systematic review and a pooled analysis of randomized controlled trials” by Ricciardi L.; et al. (Eur Spine J; [2019] 28:1821–1828). Eur. Spine J. 2020, 29, 1191–1192. [Google Scholar] [CrossRef] [PubMed]
- Ricciardi, L.; Stifano, V.; D’Arrigo, S.; Polli, F.M.; Olivi, A.; Sturiale, C.L. The role of non-rigid cervical collar in pain relief and functional restoration after whiplash injury: A systematic review and a pooled analysis of randomized controlled trials. Eur. Spine J. 2019, 28, 1821–1828. [Google Scholar] [CrossRef]
- Christensen, S.W.M.; Rasmussen, M.B.; Jespersen, C.L.; Sterling, M.; Skou, S.T. Soft-collar use in rehabilitation of whiplash-associated disorders—A systematic review and meta-analysis. Musculoskelet. Sci. Pract. 2021, 55, 102426. [Google Scholar] [CrossRef] [PubMed]
- Muzin, S.; Isaac, Z.; Walker, J.; El Abd, O.; Baima, J. When should a cervical collar be used to treat neck pain? Curr. Rev. Musculoskelet. Med. 2008, 1, 114–119. [Google Scholar] [CrossRef]
- Crawford, J.R.; Khan, R.J.; Varley, G.W. Early management and outcome following soft tissue injuries of the neck—A randomised controlled trial. Injury 2004, 35, 891–895. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef]
- Borchgrevink, G.E.; Kaasa, A.; McDonagh, D.; Stiles, T.C.; Haraldseth, O.; Lereim, I. Acute Treatment of Whiplash Neck Sprain Injuries. Spine 1998, 23, 25–31. [Google Scholar] [CrossRef]
- Vassiliou, T.; Kaluza, G.; Putzke, C.; Wulf, H.; Schnabel, M. Physical therapy and active exercises—An adequate treatment for prevention of late whiplash syndrome? Pain 2006, 124, 69–76. [Google Scholar] [CrossRef]
- Schnabel, M.; Ferrari, R.; Vassiliou, T.; Kaluza, G. Randomised, controlled outcome study of active mobilisation compared with collar therapy for whiplash injury. Emerg. Med. J. 2004, 21, 306–310. [Google Scholar] [CrossRef]
- Hawryluk, G.W.J.; Manley, G.T. Classification of traumatic brain injury. past, present, and future. In Handbook of Clinical Neurology; Elsevier B.V.: Amsterdam, The Netherlands, 2015; Volume 127, pp. 15–21. [Google Scholar] [CrossRef]
- Mckee, A.C.; Daneshvar, D.H. The neuropathology of traumatic brain injury. In Handbook of Clinical Neurology; Elsevier B.V.: Amsterdam, The Netherlands, 2015; Volume 127, pp. 45–66. [Google Scholar] [CrossRef]
- Teasdale, G.; Maas, A.; Lecky, F.; Manley, G.; Stocchetti, N.; Murray, G. The Glasgow Coma Scale at 40 years: Standing the test of time. Lancet Neurol. 2014, 13, 844–854. [Google Scholar] [CrossRef]
- Offman, J.E.R.H.; Ower, W.I.R.M.; Wolfson, A.B.; Odd, K.N.H.T.; Zucker, M.I. Validity of a Set of Clinical Criteria to Rule Out Injury to the Cervical Spine in Patients with Blunt Trauma. N. Engl. J. Med. 2000, 343, 94–99. [Google Scholar] [CrossRef]
- Stiell, I.G.; Wells, G.A.; Vandemheen, K.L.; Clement, C.M.; Lesiuk, H.; De Maio, V.J.; Laupacis, A.; Schull, M.; McKnight, R.D.; Verbeek, R.; et al. The Canadian C-Spine Rule for Radiography in Alert and Stable Trauma Patients. JAMA 2001, 286, 1841–1848. [Google Scholar] [CrossRef] [PubMed]
- Schrader, H.; Stovner, L.J.; Ferrari, R. Chronic whiplash syndrome—An overview. Tidsskr. Den Nor. Legeforening 2002, 122, 1296–1299. [Google Scholar]
- Gandelman-Marton, R.; Arlazoroff, A.; Dvir, Z. Postural stability in patients with different types of head and neck trauma in comparison to healthy subjects. Brain Inj. 2016, 30, 1612–1616. [Google Scholar] [CrossRef] [PubMed]
- Sterling, M.; Hendrikz, J.; Kenardy, J. Similar factors predict disability and posttraumatic stress disorder trajectories after whiplash injury. Pain 2011, 152, 1272–1278. [Google Scholar] [CrossRef] [PubMed]
- Treleaven, J. Dizziness, Unsteadiness, Visual Disturbances, and Postural Control. Spine 2011, 36, S211–S217. [Google Scholar] [CrossRef]
- Austin, P.C.; Grootendorst, P.; Anderson, G.M. A comparison of the ability of different propensity score models to balance measured variables between treated and untreated subjects: A Monte Carlo study. Stat. Med. 2006, 26, 734–753. [Google Scholar] [CrossRef]
- Rosenbaum, P.R.; Rubin, D.B. The Central Role of the Propensity Score in Observational Studies for Causal Effects. Vol 70.; 1083. Available online: http://biomet.oxfordjournals.org/ (accessed on 4 August 2020).
- Wong, J.J.; Côté, P.; Shearer, H.M.; Carroll, L.J.; Yu, H.; Varatharajan, S.; Southerst, D.; Van Der Velde, G.; Jacobs, C.; Taylor-Vaisey, A. Clinical practice guidelines for the management of conditions related to traffic collisions: A systematic review by the OPTIMa Collaboration. Disabil. Rehabil. 2014, 37, 471–489. [Google Scholar] [CrossRef]
- Girotto, D.; Ledić, D.; Strenja-Linić, I.; Peharec, S. Clinical and medicolegal characteristics of neck injuries. Coll. Antropol. 2011, 35, 187–190. [Google Scholar]
- Lamb, S.E.; Gates, S.; Williams, M.A.; Williamson, E.M.; Mt-Isa, S.; Withers, E.J.; Castelnuovo, E.; Smith, J.; Ashby, D.; Cooke, M.W.; et al. Emergency department treatments and physiotherapy for acute whiplash: A pragmatic, two-step, randomised controlled trial. Lancet 2013, 381, 546–556. [Google Scholar] [CrossRef]
- Skillgate, E.; Côté, P.; Cassidy, J.D.; Boyle, E.; Carroll, L.; Holm, L.W. Effect of Early Intensive Care on Recovery from Whiplash-Associated Disorders: Results of a Population-Based Cohort Study. Arch. Phys. Med. Rehabil. 2016, 97, 739–746. [Google Scholar] [CrossRef]
- Southerst, D.; Nordin, M.C.; Côté, P.; Shearer, H.M.; Varatharajan, S.; Yu, H.; Wong, J.J.; Sutton, D.A.; Randhawa, K.A.; van der Velde, G.M.; et al. Is exercise effective for the management of neck pain and associated disorders or whiplash-associated disorders? A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Spine J. 2016, 16, 1503–1523. [Google Scholar] [CrossRef]
- Castaldo, M.; Catena, A.; Chiarotto, A.; Fernández-De-Las-Peñas, C.; Arendt-Nielsen, L. Do Subjects with Whiplash-Associated Disorders Respond Differently in the Short-Term to Manual Therapy and Exercise than Those with Mechanical Neck Pain? Pain Med. 2016, 18, 791–803. [Google Scholar] [CrossRef] [PubMed]
- Krogh, S.; Kasch, H. Whiplash injury results in sustained impairments of cervical muscle function: A one-year prospective, controlled study. J. Rehabil. Med. 2018, 50, 548–555. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y.; Huang, J.; Li, F.; Hu, L. Investigation of the Effect of Neck Muscle Active Force on Whiplash Injury of the Cervical Spine. Appl. Bionics Biomech. 2018, 2018, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Dehner, C.; Hartwig, E.; Strobel, P.; Scheich, M.; Schneider, F.; Elbel, M.; Kinzl, L.; Kramer, M. Comparison of the Relative Benefits of 2 Versus 10 Days of Soft Collar Cervical Immobilization After Acute Whiplash Injury. Arch. Phys. Med. Rehabil. 2006, 87, 1423–1427. [Google Scholar] [CrossRef]
- Karlsson, A.; Peolsson, A.; Elliott, J.; Romu, T.; Ljunggren, H.; Borga, M.; Leinhard, O.D. The relation between local and distal muscle fat infiltration in chronic whiplash using magnetic resonance imaging. PLoS ONE 2019, 14, e0226037. [Google Scholar] [CrossRef] [PubMed]
- Elliot, D. Surgical Management of Painful Peripheral Nerves. Clin. Plast. Surg. 2014, 41, 589–613. [Google Scholar] [CrossRef]
- Karlsson, A.; Leinhard, O.D.; Åslund, U.; West, J.; Romu, T.; Smedby, Ö.; Zsigmond, P.; Peolsson, A. An Investigation of Fat Infiltration of the Multifidus Muscle in Patients with Severe Neck Symptoms Associated with Chronic Whiplash-Associated Disorder. J. Orthop. Sports Phys. Ther. 2016, 46, 886–893. [Google Scholar] [CrossRef] [PubMed]
- Walton, D.M. An Overview of Systematic Reviews on Prognostic Factors in Neck Pain: Results from the International Collaboration on Neck Pain (ICON) Project. Open Orthop. J. 2013, 7, 494–505. [Google Scholar] [CrossRef] [PubMed]
- Anstey, R.; Kongsted, A.; Kamper, S.; Hancock, M. Are People with Whiplash-Associated Neck Pain Different from People with Nonspecific Neck Pain? J. Orthop. Sports Phys. Ther. 2016, 46, 894–901. [Google Scholar] [CrossRef] [PubMed]
- Courtney, D.M. Assessment and Management of Whiplash from the Emergency and Acute Care Setting: Care, Questions, and Future Global Research Needs. J. Orthop. Sports Phys. Ther. 2016, 46, 822–825. [Google Scholar] [CrossRef]
- Barati, K.; Arazpour, M.; Vameghi, R.; Abdoli, A.; Farmani, F. The Effect of Soft and Rigid Cervical Collars on Head and Neck Immobilization in Healthy Subjects. Asian Spine J. 2017, 11, 390–395. [Google Scholar] [CrossRef]
- Gross, A.R.; Kaplan, F.; Huang, S.; Khan, M.; Santaguida, P.L.; Carlesso, L.C.; MacDermid, J.C.; Walton, D.M.; Kenardy, J.; Söderlund, A.; et al. Psychological Care, Patient Education, Orthotics, Ergonomics and Prevention Strategies for Neck Pain: An Systematic Overview Update as Part of the ICON§ Project. Open Orthop. J. 2013, 7, 530–561. [Google Scholar] [CrossRef]
- van der Velde, G.; Yu, H.; Paulden, M.; Côté, P.; Varatharajan, S.; Shearer, H.M.; Wong, J.J.; Randhawa, K.; Southerst, D.; Mior, S.; et al. Which interventions are cost-effective for the management of whiplash-associated and neck pain-associated disorders? A systematic review of the health economic literature by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Spine J. 2016, 16, 1582–1597. [Google Scholar] [CrossRef]
- Fritz, J. Toward Improving Outcomes in Whiplash: Implementing New Directions of Care. J. Orthop. Sports Phys. Ther. 2017, 47, 447–448. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.; Ritchie, C.; Pedler, A.; McCamley, K.; Roberts, K.; Sterling, M. Exercise induced hypoalgesia is elicited by isometric, but not aerobic exercise in individuals with chronic whiplash associated disorders. Scand. J. Pain 2017, 15, 14–21. [Google Scholar] [CrossRef]
- Schnabel, P.-D.D.M.; Weber, M.; Vassiliou, T.; Mann, D.; Kirschner, M.; Gotzen, L.; Kaluza, G. Diagnostik und therapie akuter beschwerden nach “HWS-Distorsion” in Deutsch-land. Ergebnisse einer umfrage an chirurgischen und unfallchirurgischen kliniken in Deutschland. Unfallchirurg 2004, 107, 300–306. [Google Scholar] [CrossRef]
- Giebel, G.D.; Edelmann, R.H.M. Sprain of the Cervical Spine: Early Functional vs. Immobilization Treatment. Zentralbl Chir 1997, 122, 517–521. [Google Scholar]
- Cassidy, J.D.; Carroll, L.; Côté, P.; Frank, J.W. Does Multidisciplinary Rehabilitation Benefit Whiplash Recovery? Spine 2007, 32, 126–131. [Google Scholar] [CrossRef]
- Côté, P.; Hogg-Johnson, S.; Cassidy, J.D.; Carroll, L.; Frank, J.W.; Bombardier, C. Early aggressive care and delayed recovery from whiplash: Isolated finding or reproducible result? Arthritis Rheum. 2007, 57, 861–868. [Google Scholar] [CrossRef]
- Pennie, B.; Agambar, L. Whiplash injuries. A trial of early management. J. Bone Jt. Surgery. Br. Vol. 1990, 72, 277–279. [Google Scholar] [CrossRef][Green Version]
- Gennis, P.; Miller, L.; Gallagher, E.J.; Giglio, J.; Carter, W.; Nathanson, N. The Effect of Soft Cervical Collars on Persistent Neck Pain in Patients with Whiplash Injury. Acad. Emerg. Med. 1996, 3, 568–573. [Google Scholar] [CrossRef]
- Teasell, R.W.; McClure, A.; Walton, D.; Pretty, J.; Salter, K.; Meyer, M.; Sequeira, K.; Death, B. A Research Synthesis of Therapeutic Interventions for Whiplash-Associated Disorder (WAD): Part 3—Interventions for Subacute WAD. Pain Res. Manag. 2010, 15, 305–312. [Google Scholar] [CrossRef] [PubMed]
- State Insurance Regulatory Authority. Guidelines for the Management of Acute Whiplash-Associated Disorders—For Health Professionals. Sidney: Third Edition 2014. Available online: https://www.sira.nsw.gov.au/resources-library/motor-accident-resources/publications/for-professionals/whiplash-resources/SIRA08104-Whiplash-Guidelines-1117-396479.pdf (accessed on 18 July 2021).
- Savović, J.; Jones, H.; Altman, D.; Harris, R.; Jűni, P.; Pildal, J.; Als-Nielsen, B.; Balk, E.; Gluud, C.; Gluud, L.L.; et al. Influence of reported study design characteristics on intervention effect estimates from randomised controlled trials: Combined analysis of meta-epidemiological studies. Health Technol. Assess. 2012, 16, 1–82. [Google Scholar] [CrossRef]
- Kamper, S.J. Control Groups: Linking Evidence to Practice. J. Orthop. Sports Phys. Ther. 2018, 48, 905–906. [Google Scholar] [CrossRef] [PubMed]
- Kenardy, J.; Heron-Delaney, M.; Warren, J.; Brown, E.A. Effect of Mental Health on Long-Term Disability After a Road Traffic Crash: Results from the UQ SuPPORT Study. Arch. Phys. Med. Rehabil. 2015, 96, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Kenardy, J.; Heron-Delaney, M.; Bellamy, N.; Sterling, M.; Connelly, L. The University of Queensland study of physical and psychological outcomes for claimants with minor and moderate injuries following a road traffic crash (UQ SuPPORT): Design and methods. Eur. J. Psychotraumatol. 2014, 5. [Google Scholar] [CrossRef]
- Pink, J.; Petrou, S.; Williamson, E.; Williams, M.; Lamb, S.E. Economic and Health-Related Quality of Life Outcomes of Whiplash Associated Disorders. Spine 2016, 41, 1378–1386. [Google Scholar] [CrossRef] [PubMed]
- Carroll, L.J.; Holm, L.W.; Hogg-Johnson, S.; Côté, P.; Cassidy, J.D.; Haldeman, S.; Nordin, M.; Hurwitz, E.L.; Carragee, E.J.; van der Velde, G.; et al. Course and Prognostic Factors for Neck Pain in Whiplash-Associated Disorders (WAD). J. Manip. Physiol. Ther. 2009, 32, S97–S107. [Google Scholar] [CrossRef]
- Connelly, L.B. The Nature of Whiplash in a Compensable Environment: Injury, Disability, Rehabilitation, and Compensation Systems. J. Orthop. Sports Phys. Ther. 2017, 47, 503–508. [Google Scholar] [CrossRef]
- Hill, J.C.; Whitehurst, D.G.; Lewis, M.; Bryan, S.; Dunn, K.M.; Foster, N.E.; Konstantinou, K.; Main, C.J.; Mason, E.; Somerville, S.; et al. Comparison of stratified primary care management for low back pain with current best practice (STarT Back): A randomised controlled trial. Lancet 2011, 378, 1560–1571. [Google Scholar] [CrossRef]
- Rondoni, A.; Rossettini, G.; Ristori, D.; Gallo, F.; Strobe, M.; Giaretta, F.; Battistin, A.; Testa, M. Intrarater and Inter-rater Reliability of Active Cervical Range of Motion in Patients with Nonspecific Neck Pain Measured with Technological and Common Use Devices: A Systematic Review with Meta-regression. J. Manip. Physiol. Ther. 2017, 40, 597–608. [Google Scholar] [CrossRef] [PubMed]
- Ritchie, C.; Smith, A.; Sterling, M. Medical and allied health service use during acute and chronic post-injury periods in whiplash injured individuals. BMC Health Serv. Res. 2020, 20, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Brownson, R.C.; Colditz, G.A.; Proctor, E.K. Oxford Scholarship Online Dissemination and Implementation Research in Health: Translate Science to Practice; 2012; pp. 1–25. Available online: https://oxford.universitypressscholarship.com/view/10.1093/acprof:oso/9780199751877.001.0001/acprof-9780199751877 (accessed on 4 August 2020). [CrossRef]
- Mourad, F.; Patuzzo, A.; Tenci, A.; Turcato, G.; Faletra, A.; Valdifiori, G.; Gobbo, M.; Maselli, F.; Milano, G. Management of whiplash-associated disorder in the Italian emergency department: The feasibility of an evidence-based continuous professional development course provided by physiotherapists. Disabil. Rehabil. 2020, 2020, 1–8. [Google Scholar] [CrossRef]
- Hutting, P.N.; Kerry, P.R.; Kranenburg, P.R.; Mourad, P.F.; Taylor, P.A. Assessing Vascular Function in Patients with Neck Pain, Headache, and/or Orofacial Pain: Part of the Job Description of All Physical Therapists. J. Orthop. Sports Phys. Ther. 2021, 51, 418–421. [Google Scholar] [CrossRef] [PubMed]
- Mourad, F.; Giovannico, G.; Maselli, F.; Bonetti, F.; Fernández-De-Las-Peñas, C.; Dunning, J. Basilar impression presenting as intermittent mechanical neck pain: A rare case report. BMC Musculoskelet. Disord. 2016, 17, 1–5. [Google Scholar] [CrossRef]
- Mourad, F.; Lopez, G.; Cataldi, F.; Maselli, F.; Pellicciari, L.; Salomon, M.; Kranenburg, H.; Kerry, R.; Taylor, A.; Hutting, N. Assessing Cranial Nerves in Physical Therapy Practice: Findings from a Cross-Sectional Survey and Implication for Clinical Practice. Healthcare 2021, 9, 1262. [Google Scholar] [CrossRef]
- Taylor, A.; Mourad, F.; Kerry, R.; Hutting, N. A guide to cranial nerve testing for musculoskeletal clinicians. J. Man. Manip. Ther. 2021, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Elkin, B.S.; Elliott, J.M.; Siegmund, G.P. Whiplash Injury or Concussion? A Possible Biomechanical Explanation for Concussion Symptoms in Some Individuals Following a Rear-End Collision. J. Orthop. Sports Phys. Ther. 2016, 46, 874–885. [Google Scholar] [CrossRef] [PubMed]
- Sedgwick, P. Retrospective cohort studies: Advantages and disadvantages. BMJ 2014, 348, g1072. [Google Scholar] [CrossRef]
- Corte di Cassazione, Sezione 3 Civile. Sentenza 19 Gennaio 2018, n. 1272. Available online: https://www.webgiuridico.it/sentenze2018/1272-2018.htm (accessed on 30 September 2021).
| Grade | Clinical Presentation |
|---|---|
| 0 | No complaint about neck pain No physical signs |
| I | Neck complaint of pain: Stiffness or tenderness only Non-physical signs |
| II | Neck complaint Musculoskeletal signs, including: Decreased range of motion Point tenderness |
| III | Neck complaint Neurological signs, including: Decreased or absent tendon reflexes Muscles weakness Sensory deficits |
| IV | Neck complaint and fracture or dislocation |
| Variables | Soft Cervical Collar | No Soft Cervical Collar | p-Value |
|---|---|---|---|
| Patients, n (%) | 1847 (85.4) | 315 (14.6) | |
| Age, years, median (IQR) | 40 (28–52) | 38 (27–49) | 0.026 |
| Gender, n (%) Female Male | 133 (42.2) 182 (57.8) | 1031 (55.8) 816 (44.2) | <0.001 * |
| Time of access in ED, n (%) Within 3 h Within 12 h Over 12–48 h | 1001 (54.2) 223 (12.1) 620 (33.6) | 178 (56.5) 42 (13.5) 95 (30.1) | 0.200 |
| Dangerous mechanism of trauma, n (%) | 36 (11.4) | 136 (7.4) | 0.018 * |
| Trauma related to airbag blast, n (%) | 630 (34.1) | 106 (33.6) | 0.901 |
| Trauma related to acute intoxication, n (%) | 12 (3.8) | 10 (0.5) | <0.001 * |
| Alteration of the consciousness at the first evaluation in ED, n (%) | 8 (2.5) | 10 (0.5) | 0.002 * |
| Neck pain at the first evaluation in ED, n (%) | 267 (84.8) | 1765 (95.6) | <0.001 * |
| Thoracic/Lumbar pain at the first evaluation in ED, n (%) | 122 (38.7) | 686 (37.1) | 0.614 |
| Limbs paresthesia at the first evaluation in ED, n (%) | 6 (1.9) | 51 (2.8) | 0.453 |
| Presence of midline cervical spine tenderness at CE, n (%) | 118 (37.5) | 648 (35.1) | 0.444 |
| Presence of cervical muscles tenderness at CE, n (%) | 93 (29.5) | 596 (32.3) | 0.360 |
| Presence of upper trapezius tenderness at CE, n (%) | 56 (17.8) | 687 (37.2) | <0.001 * |
| Presence of pain during active cervical rotation at CE, n (%) | 64 (20.3) | 473 (25.6) | 0.048 * |
| Presence of active cervical rotation <45 degrees at CE, n (%) | 14 (4.4) | 135 (7.3) | 0.070 |
| Grade of WAD 1, n (%) 0 I II III | 45 (14.3) 152 (48.3) 112 (35.6) 6 (1.9) | 53 (2.9) 865 (46.8) 877 (47.5) 52 (2.8) | <0.001 * |
| Variables | No Return | Return within 3 Months | p-Value |
|---|---|---|---|
| Patients, n (%) | 1998 (92.4) | 164 (7.6) | |
| Age, years, median (IQR) | 38 (27–50) | 38 (29–48) | 0.821 |
| Gender, n (%) Female Male | 1058 (53) 940 (47) | 106 (64.6) 58 (35.4) | 0.004 * |
| Use of soft cervical collar, n (%) | 1691 (84.6) | 156 (95.1) | <0.001 * |
| Days of soft cervical collar positioning, median (IQR) | 7 (5–8) | 8 (6–10) | 0.022 * |
| Dangerous mechanism of trauma, n (%) | 148 (7.4) | 24 (14.6) | 0.002 * |
| Trauma related to airbag blast, n (%) | 661 (33.1) | 64 (39) | 0.220 |
| Trauma related to acute intoxication, n (%) | 20 (1.0) | 2 (1.2) | 0.681 |
| Alteration of the consciousness at the first evaluation in ED, n (%) | 16 (0.8) | 2 (1.2) | 0.642 |
| Neck pain at the first evaluation in ED, n (%) | 1876 (93.9) | 156 (95.1) | 0.675 |
| Thoracic/Lumbar pain at the first evaluation in ED, n (%) | 730 (36.5) | 78 (47.6) | 0.006 * |
| Limbs paresthesia at the first evaluation in ED, n (%) | 51 (2.6) | 6 (3.7) | 0.440 |
| Presence of midline cervical spine tenderness at CE, n (%) | 716 (35.8) | 50 (30.5) | 0.175 |
| Presence of cervical muscles tenderness at CE, n (%) | 640 (32.0) | 49 (29.9) | 0.602 |
| Presence of upper trapezius tenderness at CE, n (%) | 672 (33.6) | 71 (43.3) | 0.016 * |
| Presence of pain during active cervical rotation at CE, n (%) | 478 (23.9) | 59 (36.0) | 0.001 * |
| Presence of active cervical rotation <45 degrees at CE, n (%) | 121 (6.1) | 28 (17.1) | <0.001 * |
| Grade of WAD 1, n (%) 0 I II III | 94 (4.7) 952 (47.6) 901 (45.1) 51 (2.6) | 4 (2.4) 65 (39.6) 88 (53.7) 7 (4.3) | 0.003 * |
| Variables | No Soft Cervical Collar | Soft Cervical Collar | p-Value |
|---|---|---|---|
| Patients, n (%) | 98 (50.0) | 98 (50.0) | |
| Age, years, median (IQR) | 45 (28–54) | 36 (23–51) | 0.055 |
| Gender, n (%) Female Male | 47 (48.0) 51 (52.0) | 57 (58.2) 41 (41.8) | 0.126 |
| Dangerous mechanism of trauma, n (%) | 11 (11.2) | 18 (18.4) | 0.227 |
| Trauma related to airbag blast, n (%) | 51 (51.9) | 44 (45.0) | 0.625 |
| Trauma related to acute intoxication, n (%) | 9 (9.2) | 7 (7.1) | 0.795 |
| Alteration of the consciousness at the first evaluation in ED, n (%) | 8 (8.2) | 7 (7.1) | 1.000 |
| Neck pain at the first evaluation in ED, n (%) | 87 (88.8) | 84 (85.7) | 0.669 |
| Thoracic/Lumbar pain at the first evaluation in ED, n (%) | 47 (48.0) | 42 (42.9) | 0.566 |
| Limbs paresthesia at the first evaluation in ED, n (%) | 6 (6.1) | 5 (5.1) | 1.000 |
| Presence of midline cervical spine tenderness at CE, n (%) | 43 (43.9) | 46 (46.9) | 0.776 |
| Presence of cervical muscles tenderness at CE, n (%) | 37 (37.8) | 44 (44.9) | 0.384 |
| Presence of upper trapezius tenderness at CE, n (%) | 26 (26.5) | 29 (29.6) | 0.751 |
| Presence of pain during active cervical rotation at CE, n (%) | 43 (43.9) | 47 (48.0) | 0.667 |
| Presence of active cervical rotation <45 degrees at CE, n (%) | 13 (13.3) | 13 (13.3) | 1.000 |
| Grade of WAD 1, n (%) 0 I II III | 9 (9.2) 24 (24.5) 59 (60.2) 6 (6.1) | 6 (6.1) 32 (32.7) 54 (55.1) 6 (6.1) | 0.585 |
| Variables | No Return | Return within 3 Months | p-Value |
|---|---|---|---|
| Patients, n (%) | 165 (84.2) | 31 (15.8) | |
| Age, years, median (IQR) | 40 (25–54) | 42 (28–46) | 0.373 |
| Gender, n (%) Female Male | 86 (52.1) 79 (47.9) | 18 (58.1) 13 (41.9) | 0.563 |
| Positioning of soft cervical collar, n (%) | 73 (44.2) | 25 (80.6) | <0.001 * |
| Days of soft cervical collar positioning, median (IQR) | 0 (0–7) | 7 (3–9) | <0.001 * |
| Dangerous mechanism of trauma, n (%) | 20 (12.1) | 9 (29.0) | 0.025 |
| Trauma related to airbag blast, n (%) | 69 (42.1) | 25 (80.0) | 0.039 |
| Trauma related to acute intoxication, n (%) | 14 (8.5) | 2 (6.5) | 0.753 |
| Alteration of the consciousness at the first evaluation in ED, n (%) | 13 (7.9) | 2 (6.5) | 1.000 |
| Neck pain at the first evaluation in ED, n (%) | 145 (87.9) | 26 (83.9) | 0.559 |
| Thoracic/Lumbar pain at the first evaluation in ED, n (%) | 74 (44.8) | 15 (48.4) | 0.844 |
| Limbs paresthesia at the first evaluation in ED, n (%) | 10 (6.1) | 1 (3.2) | 1.000 |
| Presence of midline cervical spine tenderness at CE, n (%) | 78 (47.3) | 11 (35.5) | 0.245 |
| Presence of cervical muscles tenderness at CE, n (%) | 71 (43.0) | 10 (32.3) | 0.322 |
| Presence of upper trapezius tenderness at CE, n (%) | 42 (25.5) | 13 (41.9) | 0.080 |
| Presence of pain during active cervical rotation at CE, n (%) | 72 (43.6) | 18 (58.1) | 0.170 |
| Presence of active cervical rotation <45 degrees at CE, n (%) | 19 (11.5) | 7 (22.6) | 0.143 |
| Grade of WAD 1, n (%) 0 I II III | 14 (8.5) 47 (28.5) 94 (57.0) 10 (6.1) | 1 (3.2) 9 (29.0) 19 (61.3) 2 (6.5) | 0.856 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mourad, F.; Rossettini, G.; Galeno, E.; Patuzzo, A.; Zolla, G.; Maselli, F.; Ciolan, F.; Guerra, M.; Tosato, G.; Palese, A.; et al. Use of Soft Cervical Collar among Whiplash Patients in Two Italian Emergency Departments Is Associated with Persistence of Symptoms: A Propensity Score Matching Analysis. Healthcare 2021, 9, 1363. https://doi.org/10.3390/healthcare9101363
Mourad F, Rossettini G, Galeno E, Patuzzo A, Zolla G, Maselli F, Ciolan F, Guerra M, Tosato G, Palese A, et al. Use of Soft Cervical Collar among Whiplash Patients in Two Italian Emergency Departments Is Associated with Persistence of Symptoms: A Propensity Score Matching Analysis. Healthcare. 2021; 9(10):1363. https://doi.org/10.3390/healthcare9101363
Chicago/Turabian StyleMourad, Firas, Giacomo Rossettini, Erasmo Galeno, Alberto Patuzzo, Giuseppe Zolla, Filippo Maselli, Federica Ciolan, Michele Guerra, Giacomo Tosato, Alvisa Palese, and et al. 2021. "Use of Soft Cervical Collar among Whiplash Patients in Two Italian Emergency Departments Is Associated with Persistence of Symptoms: A Propensity Score Matching Analysis" Healthcare 9, no. 10: 1363. https://doi.org/10.3390/healthcare9101363
APA StyleMourad, F., Rossettini, G., Galeno, E., Patuzzo, A., Zolla, G., Maselli, F., Ciolan, F., Guerra, M., Tosato, G., Palese, A., Testa, M., Ricci, G., Zaboli, A., Bonora, A., & Turcato, G. (2021). Use of Soft Cervical Collar among Whiplash Patients in Two Italian Emergency Departments Is Associated with Persistence of Symptoms: A Propensity Score Matching Analysis. Healthcare, 9(10), 1363. https://doi.org/10.3390/healthcare9101363










