Post-Traumatic Stress Disorder in Chinese Teachers during COVID-19 Pandemic: Roles of Fear of COVID-19, Nomophobia, and Psychological Distress
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.3. Data Analysis
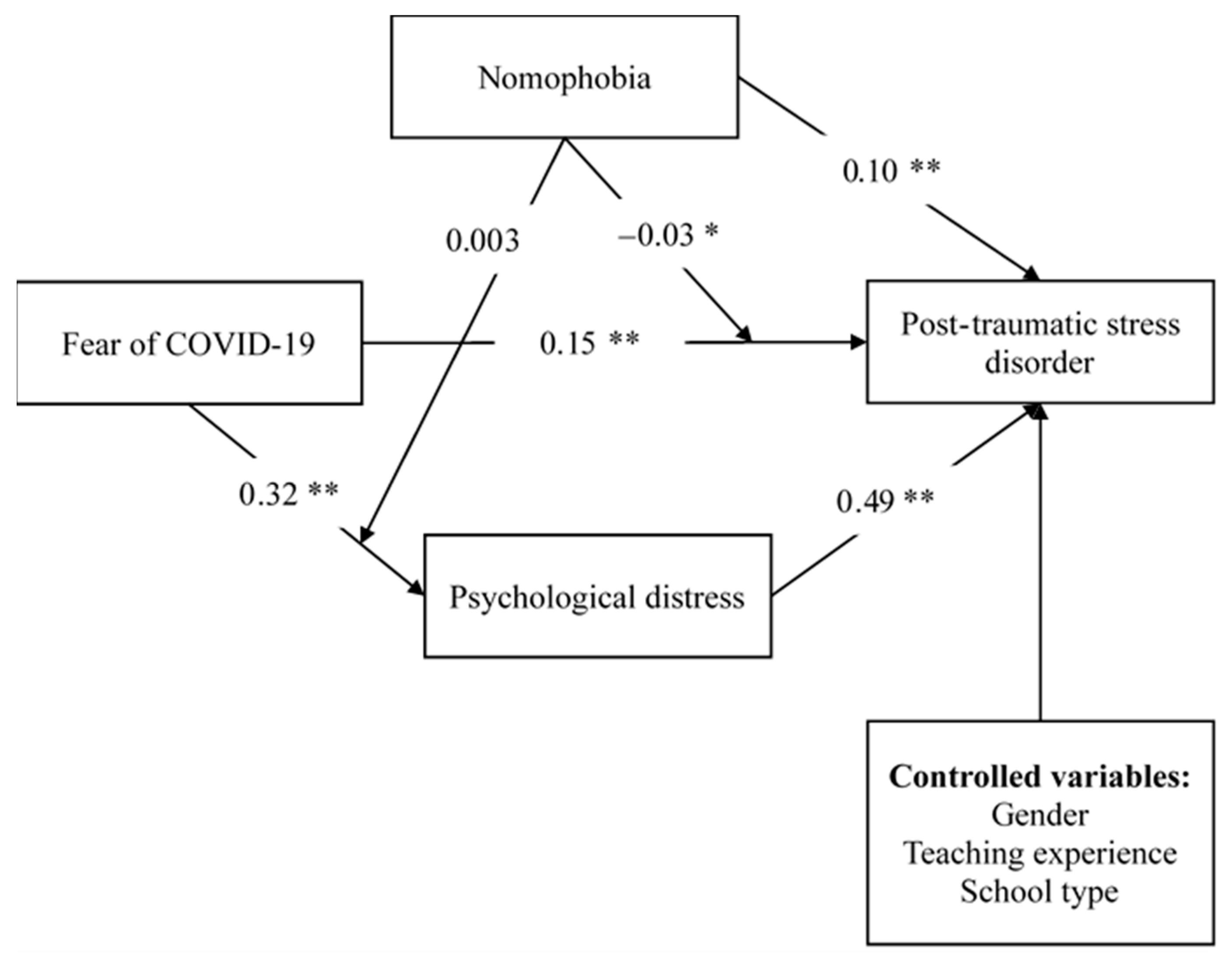
3. Results
4. Discussion
5. Implications
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Timeline of WHO’s Response to COVID-19, 2020. Available online: https://www.who.int/news/item/29-06-2020-covidtimeline. (accessed on 7 February 2020).
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [Green Version]
- Ahorsu, D.K.; Lin, C.-Y.; Pakpour, A.H. The association between health status and insomnia, mental health, and preventive behaviors: The Mediating Role of Fear of COVID-19. Gerontol. Geriatr. Med. 2020, 6, 2333721420966081. [Google Scholar] [CrossRef]
- Xiang, Y.-T.; Yang, Y.; Li, W.; Zhang, L.; Zhang, Q.; Cheung, T.; Ng, C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020, 7, 228–229. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Imani, V.; Lin, C.-Y.; Timpka, T.; Broström, A.; Updegraff, J.A.; Årestedt, K.; Griffiths, M.D.; Pakpour, A.H. Associations between fear of COVID-19, mental health, and preventive behaviours across pregnant women and husbands: An actor-partner interdependence modelling. Int. J. Ment. Health Addict. 2020, 3, 1–15. [Google Scholar] [CrossRef]
- Lee, A.M.; Wong, J.G.; McAlonan, G.M.; Cheung, V.; Cheung, C.; Sham, P.C.; Chu, C.-M.; Wong, P.-C.; Tsang, K.W.; Chua, S.E. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can. J. Psychiatry 2007, 52, 233–240. [Google Scholar] [CrossRef] [Green Version]
- McAlonan, G.M.; Lee, A.M.; Cheung, V.; Cheung, C.; Tsang, K.W.; Sham, P.C.; Chua, S.E.; Wong, J.G. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can. J. Psychiatry 2007, 52, 241–247. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Mental Health and Psychosocial Considerations during the COVID-19 Outbreak, 18 March 2020; World Health Organization: Geneva, Switzerland, 2020; Available online: https://apps.who.int/iris/bitstream/handle/10665/331490/WHO-2019-nCoV-MentalHealth-2020.1-eng.pdf (accessed on 7 February 2020).
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 1–11. [Google Scholar] [CrossRef]
- Worthington, B. Coronavirus Pandemic Fears Prompt Government to Activate Emergency Response and Extend Travel Ban. 2020. Available online: https://www.abc.net.au/news/2020-02-27/federal-government-coronavirus-pandemic-emergency-plan/12005734 (accessed on 7 February 2020).
- Fazeli, S.; Zeidi, I.M.; Lin, C.-Y.; Namdar, P.; Griffiths, M.D.; Ahorsu, D.K.; Pakpour, A.H. Depression, anxiety, and stress mediate the associations between internet gaming disorder, insomnia, and quality of life during the COVID-19 outbreak. Addict. Behav. Rep. 2020, 12, 100307. [Google Scholar]
- Zhang, H.; Shi, Y.; Jing, P.; Zhan, P.; Fang, Y.; Wang, F. Posttraumatic stress disorder symptoms in healthcare workers after the peak of the COVID-19 outbreak: A survey of a large tertiary care hospital in Wuhan. Psychiatry Res. 2020, 294, 113541. [Google Scholar] [CrossRef]
- Marinoni, G.; Van’t Land, H.; Jensen, T. The Impact of COVID-19 on Higher Education around the World. 2020. Available online: https://www.iau-aiu.net/IMG/pdf/iau_covid19_and_he_survey_report_final_may_2020.pdf (accessed on 7 February 2020).
- MacIntyre, P.D.; Gregersen, T.; Mercer, S. Language teachers’ coping strategies during the COVID-19 conversion to online teaching: Correlations with stress, wellbeing and negative emotions. System 2020, 94, 102352. [Google Scholar] [CrossRef]
- Vlachos, J.; Hertegård, E.; Svaleryd, H.B. The effects of school closures on SARS-CoV-2 among parents and teachers. Proc. Natl. Acad. Sci. USA 2021, 118, e2020834118. [Google Scholar] [CrossRef]
- Deja, M.; Denke, C.; Weber-Carstens, S.; Schröder, J.; Pille, C.E.; Hokema, F.; Falke, K.J.; Kaisers, U. Social support during intensive care unit stay might improve mental impairment and consequently health-related quality of life in survivors of severe acute respiratory distress syndrome. Crit. Care 2006, 10, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Gonzalez, A.; Rasul, R.; Molina, L.; Schneider, S.; Bevilacqua, K.; Bromet, E.J.; Luft, B.J.; Taioli, E.; Schwartz, R. Differential effect of Hurricane Sandy exposure on PTSD symptom severity: Comparison of community members and responders. Occup. Environ. Med. 2019, 76, 881–887. [Google Scholar] [CrossRef] [Green Version]
- Sher, L. Recognizing Post-Traumatic Stress Disorder. QJM Int. J. Med. 2014, 97, 1–5. [Google Scholar]
- Association, A.P. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Publishing: Arlington, VA, USA, 2013. [Google Scholar]
- Tang, W.; Hu, T.; Hu, B.; Jin, C.; Wang, G.; Xie, C.; Chen, S.; Xu, J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 2020, 274, 1–7. [Google Scholar] [CrossRef]
- Jung, H.; Jung, S.Y.; Lee, M.H.; Kim, M.S. Assessing the presence of post-traumatic stress and turnover intention among nurses post–Middle East respiratory syndrome outbreak: The importance of supervisor support. Workplace Health Saf. 2020, 68, 337–345. [Google Scholar] [CrossRef]
- Liang, L.; Gao, T.; Ren, H.; Cao, R.; Qin, Z.; Hu, Y.; Li, C.; Mei, S. Post-traumatic stress disorder and psychological distress in Chinese youths following the COVID-19 emergency. J. Health Psychol. 2020, 25, 1164–1175. [Google Scholar] [CrossRef]
- Di Crosta, A.; Palumbo, R.; Marchetti, D.; Ceccato, I.; La Malva, P.; Maiella, R.; Cipi, M.; Roma, P.; Mammarella, N.; Verrocchio, M.C. Individual differences, economic stability, and fear of contagion as risk factors for PTSD symptoms in the COVID-19 emergency. Front. Psychol. 2020, 11, 2329. [Google Scholar] [CrossRef]
- Bhattacharya, S.; Bashar, M.A.; Srivastava, A.; Singh, A. Nomophobia: No mobile phone phobia. J. Fam. Med. Prim. Care 2019, 8, 1297. [Google Scholar] [CrossRef]
- Beaunoyer, E.; Dupéré, S.; Guitton, M.J. COVID-19 and digital inequalities: Reciprocal impacts and mitigation strategies. Comput. Hum. Behav. 2020, 111, 106424. [Google Scholar] [CrossRef]
- Contractor, A.A.; Frankfurt, S.B.; Weiss, N.H.; Elhai, J.D. Latent-level relations between DSM-5 PTSD symptom clusters and problematic smartphone use. Comput. Hum. Behav. 2017, 72, 170–177. [Google Scholar] [CrossRef]
- Farooqui, I.A.; Pore, P.; Gothankar, J. Nomophobia: An emerging issue in medical institutions? J. Ment. Health 2018, 27, 438–441. [Google Scholar] [CrossRef]
- Samaha, M.; Hawi, N.S. Relationships among smartphone addiction, stress, academic performance, and satisfaction with life. Comput. Hum. Behav. 2016, 57, 321–325. [Google Scholar] [CrossRef]
- Tams, S.; Legoux, R.; Léger, P.-M. Smartphone withdrawal creates stress: A moderated mediation model of nomophobia, social threat, and phone withdrawal context. Comput. Hum. Behav. 2018, 81, 1–9. [Google Scholar] [CrossRef]
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J. Trauma Stress 2015, 28, 489–498. [Google Scholar] [CrossRef]
- Bovin, M.J.; Marx, B.P.; Weathers, F.W.; Gallagher, M.W.; Rodriguez, P.; Schnurr, P.P.; Keane, T.M. Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders–fifth edition (PCL-5) in veterans. Psychol. Assess. 2016, 28, 1379. [Google Scholar] [CrossRef]
- Fung, H.W.; Chan, C.; Lee, C.Y.; Ross, C.A. Using the post-traumatic stress disorder (PTSD) checklist for DSM-5 to screen for PTSD in the Chinese context: A pilot study in a psychiatric sample. J. Evid.-Based Soc. Work 2019, 16, 643–651. [Google Scholar] [CrossRef]
- Weathers, F.; Litz, B.; Keane, T.; Palmieri, P.; Marx, B.; Schnurr, P. The PTSD Checklist for DSM-5 (PCL-5): National Center for PTSD; National Center for PTSD: Boston, MA, USA, 2020. [Google Scholar]
- Ahorsu, D.K.; Lin, C.-Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and initial validation. Int. J. Ment. Health Addict. 2020, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Chang, K.-C.; Hou, W.-L.; Pakpour, A.H.; Lin, C.-Y.; Griffiths, M.D. Psychometric testing of three COVID-19-related scales among people with mental illness. Int. J. Ment. Health Addict. 2020, 12, 1–13. [Google Scholar] [CrossRef]
- Yildirim, C.; Correia, A.-P. Exploring the dimensions of nomophobia: Development and validation of a self-reported questionnaire. Comput. Hum. Behav. 2015, 49, 130–137. [Google Scholar] [CrossRef]
- Gao, Y.; Dai, H.; Jia, G.; Liang, C.; Tong, T.; Zhang, Z.; Song, R.; Wang, Q.; Zhu, Y. Translation of the Chinese version of the Nomophobia questionnaire and its validation among college students: Factor analysis. JMIR Mhealth Uhealth 2020, 8, e13561. [Google Scholar] [CrossRef] [Green Version]
- Lu, S.; Hu, S.; Guan, Y.; Xiao, J.; Cai, D.; Gao, Z.; Sang, Z.; Wei, J.; Zhang, X.; Margraf, J. Measurement invariance of the Depression Anxiety Stress Scales-21 across gender in a sample of Chinese university students. Front. Psychol. 2018, 9, 2064. [Google Scholar] [CrossRef] [Green Version]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2013. [Google Scholar]
- Lin, C.-Y.; Tsai, M.-C. Effects of family context on adolescents’ psychological problems: Moderated by pubertal timing, and mediated by self-esteem and interpersonal relationships. Appl. Res. Qual. Life 2016, 11, 907–923. [Google Scholar] [CrossRef]
- Mehta, C.R.; Patel, N.R. IBM SPSS Exact Tests; IBM Corporation: Armonk, NY, USA, 2011. [Google Scholar]
- Zhang, J.; Zhang, Y.; Du, C.; Zhu, S.; Huang, Y.; Tian, Y.; Chen, D.; Li, H.; Gong, Y.; Zhang, M. Prevalence and risk factors of posttraumatic stress disorder among teachers 3 months after the Lushan earthquake: A cross-sectional study. Medicine 2016, 95, e4298. [Google Scholar] [CrossRef]
- Satici, B.; Gocet-Tekin, E.; Deniz, M.E.; Satici, S.A. Adaptation of the Fear of COVID-19 Scale: Its association with psychological distress and life satisfaction in Turkey. Int. J. Ment. Health Addict. 2020, 1–9. [Google Scholar] [CrossRef]
- Labrague, L.J.; de Los Santos, J.A.A. Fear of COVID-19, psychological distress, work satisfaction and turnover intention among frontline nurses. J. Nurs. Manag. 2020, 29, 395–403. [Google Scholar] [CrossRef]
- Lin, C.-Y.; Broström, A.; Griffiths, M.D.; Pakpour, A.H. Investigating mediated effects of fear of COVID-19 and COVID-19 misunderstanding in the association between problematic social media use, psychological distress, and insomnia. Internet Interv. 2020, 21, 100345. [Google Scholar] [CrossRef]
- Aperribai, L.; Crotalaria, L.; Aguirre, T.; Verche, E.; Borges, A. Teacher’s physical activity and mental health during lockdown due to the COVID-2019 pandemic. Front. Psychol. 2020, 11, 2673. [Google Scholar] [CrossRef]
- Huo, L.; Zhou, Y.; Li, S.; Ning, Y.; Zeng, L.; Liu, Z.; Zhang, X.Y. Burnout and its relationship with depressive symptoms in medical staff during the COVID-19 epidemic in China. Front. Psychol. 2021, 12, 544. [Google Scholar] [CrossRef]
- Malureanu, A.; Panisoara, G.; Lazar, I. The relationship between self-confidence, self-efficacy, grit, usefulness, and ease of use of elearning platforms in corporate training during the COVID-19 pandemic. Sustainability 2021, 13, 6633. [Google Scholar] [CrossRef]
- Alarcon, G.M. A meta-analysis of burnout with job demands, resources, and attitudes. J. Vocat. Behav. 2011, 79, 549–562. [Google Scholar] [CrossRef]
- Zhang, J.; Wu, W.; Zhao, X.; Zhang, W. Recommended psychological crisis intervention response to the 2019 novel coronavirus pneumonia outbreak in China: A model of West China Hospital. Precis. Clin. Med. 2020, 3, 3–8. [Google Scholar] [CrossRef] [Green Version]
- Mertens, G.; Gerritsen, L.; Duijndam, S.; Salemink, E.; Engelhard, I.M. Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March 2020. J. Anxiety Disord. 2020, 74, 102258. [Google Scholar] [CrossRef] [PubMed]
- Gorman, J.M. Fear and Anxiety: The Benefits of Translational Research; American Psychiatric Publishing: Washington, DC, USA, 2008. [Google Scholar]
- Roman, T. Supporting the mental health of preservice teachers in COVID-19 through trauma-informed educational practices and adaptive formative assessment tools. JTATE 2020, 28, 473–481. [Google Scholar]
- Demerouti, E.; Bakker, A.B.; Nachreiner, F.; Schaufeli, W.B. The job demands-resources model of burnout. J. Appl. Psychol. 2001, 86, 499. [Google Scholar] [CrossRef]
- Rubino, C.; Perry, S.J.; Milam, A.C.; Spitzmueller, C.; Zapf, D. Demand–control–person: Integrating the demand–control and conservation of resources models to test an expanded stressor–strain model. J. Occup. Health Psychol. 2012, 17, 456. [Google Scholar] [CrossRef]
- Ehlers, A.; Clark, D.M. A cognitive model of posttraumatic stress disorder. Behav. Res. Ther. 2000, 38, 319–345. [Google Scholar] [CrossRef]
| Variables | Mean (SD) or n (%) |
|---|---|
| Gender (male) | 738 (28.4) |
| School type (public) | 2591 (99.5) |
| Teaching experience in years | |
| (i) 5 years and below | 907 (34.8) |
| (ii) 6–10 years | 556 (21.4) |
| (iii) 11–15 years | 306 (11.8) |
| (iv) 16–20 years | 251 (9.6) |
| (v) 21 years and above | 583 (22.4) |
| Fear of COVID-19 Scale score | 15.40 (4.20) |
| Nomophobia Questionnaire score | 69.14 (28.84) |
| Depression, Anxiety, Stress Scale score | 30.03 (10.99) |
| 1 PTSD Checklist for DSM-5 score | 14.46 (12.66) |
| Probable 1 PTSD (yes; using a cutoff score of 31 or above) | 321 (12.3) |
| Probable 1 PTSD (yes; using cutoff score of 49 or above) | 27 (1.0) |
| r (p-Value) | |||||||
|---|---|---|---|---|---|---|---|
| Gender | School Type | Teaching Experience | FCV-19S | NMPQ | DASS-21 | PCL-5 | |
| Gender | - | ||||||
| School Type | 0.19 (<0.001) | - | |||||
| Teaching Experience | −0.35 (<0.001) | −0.18 (<0.001) | - | ||||
| FCV-19S | 0.06 (0.002) | 0.02 (0.31) | 0.03 (0.21) | - | |||
| NMPQ | 0.09 (<0.001) | <0.001 (0.998) | 0.01 (0.81) | 0.34 (<0.001) | - | ||
| DASS-21 | −0.10 (<0.001) | −0.02 (0.29) | 0.12 (<0.001) | 0.37 (<0.001) | 0.26 (<0.001) | - | |
| PCL-5 | −0.09 (<0.001) | −0.08 (<0.001) | 0.04 (0.053) | 0.37 (<0.001) | 0.28 (<0.001) | 0.58 (<0.001) | - |
| Coefficient (SE)/LLCI, ULCI (p-value) | ||
|---|---|---|
| DASS-21 (R2 = 0.18) | PCL-5 (R2 = 0.38) | |
| FCV-19S | 5.72 (0.81)/4.12, 7.30 (<0.001) | 4.75 (0.82)/3.14, 6.36 (p < 0.001) |
| NMPQ | 0.09 (0.02)/0.04, 0.14 (p < 0.001) | |
| DASS-21 | 0.57 (0.02)/0.53, 0.61 (p < 0.001) | |
| Moderated Effect of NMPQ on FCV-19S to PCL-5 | 0.001 (0.01)/−0.04, −0.0002 (p = 0.047) | |
| Moderated Effect of NMPQ on FCV-19S to DASS-21 | 0.002 (0.01)/−0.02, 0.02 (p = 0.87) | |
| Indirect Effect Via DASS-21 | 3.32 (0.33)/2.71, 4.00 a | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kukreti, S.; Ahorsu, D.K.; Strong, C.; Chen, I.-H.; Lin, C.-Y.; Ko, N.-Y.; Griffiths, M.D.; Chen, Y.-P.; Kuo, Y.-J.; Pakpour, A.H. Post-Traumatic Stress Disorder in Chinese Teachers during COVID-19 Pandemic: Roles of Fear of COVID-19, Nomophobia, and Psychological Distress. Healthcare 2021, 9, 1288. https://doi.org/10.3390/healthcare9101288
Kukreti S, Ahorsu DK, Strong C, Chen I-H, Lin C-Y, Ko N-Y, Griffiths MD, Chen Y-P, Kuo Y-J, Pakpour AH. Post-Traumatic Stress Disorder in Chinese Teachers during COVID-19 Pandemic: Roles of Fear of COVID-19, Nomophobia, and Psychological Distress. Healthcare. 2021; 9(10):1288. https://doi.org/10.3390/healthcare9101288
Chicago/Turabian StyleKukreti, Shikha, Daniel Kwasi Ahorsu, Carol Strong, I-Hua Chen, Chung-Ying Lin, Nai-Ying Ko, Mark D. Griffiths, Yu-Pin Chen, Yi-Jie Kuo, and Amir H. Pakpour. 2021. "Post-Traumatic Stress Disorder in Chinese Teachers during COVID-19 Pandemic: Roles of Fear of COVID-19, Nomophobia, and Psychological Distress" Healthcare 9, no. 10: 1288. https://doi.org/10.3390/healthcare9101288
APA StyleKukreti, S., Ahorsu, D. K., Strong, C., Chen, I.-H., Lin, C.-Y., Ko, N.-Y., Griffiths, M. D., Chen, Y.-P., Kuo, Y.-J., & Pakpour, A. H. (2021). Post-Traumatic Stress Disorder in Chinese Teachers during COVID-19 Pandemic: Roles of Fear of COVID-19, Nomophobia, and Psychological Distress. Healthcare, 9(10), 1288. https://doi.org/10.3390/healthcare9101288







