Telemedicine for Pre-Employment Medical Examinations and Follow-Up Visits on Board Ships: A Narrative Review on the Feasibility
Abstract
1. Introduction
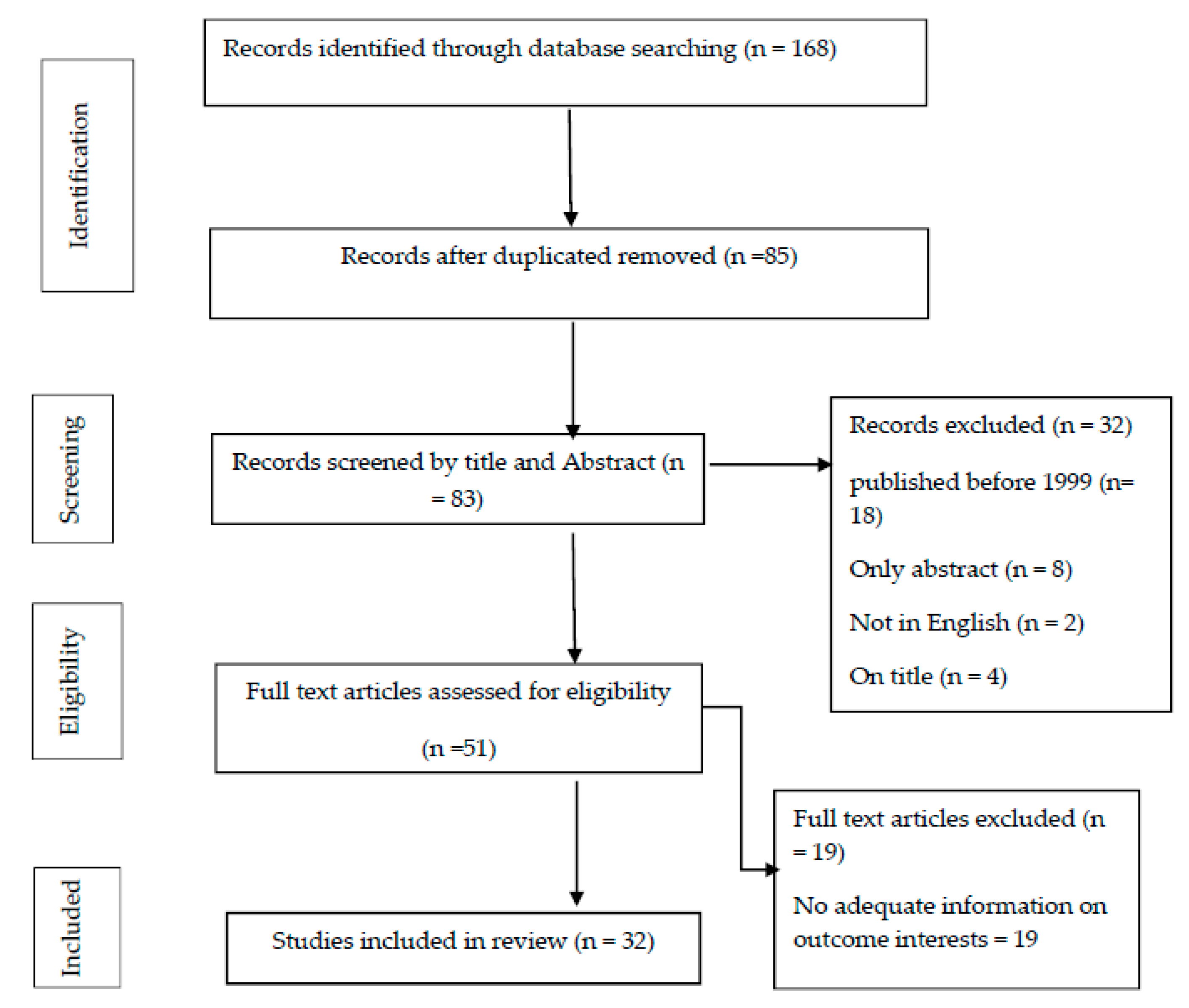
2. Materials and Methods
3. Telemedicine in Different Medical Examinations/Tests
3.1. Electrocardiogram (ECG)
3.2. Spirometry
3.3. Blood Glucose Monitoring
3.4. Urine Analysis
4. Legal Implications of Telemedicine
5. Recommendations
- PEME: ECG, spirometry, measurement of vital signs (blood pressure, heart rate, and temperature), oxygen saturation assessed by a pulse oximeter, blood glucose measurement by glucometer, and urinalysis are tests that can be monitored remotely in some cases even without medical assistance. These tests are currently used for the general population in different medical specialties. We thus suggest using them both for PEME visits and/or for periodic checks of seafarers aboard ships, provided that on board there is the necessary technological resource training.
- Follow-up visits: Telemedical Maritime Assistance Services (TMAS) doctors can make multiple medical visits a single patient, guaranteeing appropriate evaluation standards. They can also follow the same patient for the necessary time by monitoring over time without the need for large displacements and without the need to visit inside the ships in person. The technological equipment should provide a secure and high-speed internet connection; a clinical telemedicine software that acts as a hub capable of sending the patient’s vital parameters to the doctor; devices capable of monitoring the patient’s body parameters; and, finally, an ad hoc training program with periodic simulations. If fitted onboard, these systems could also help a TMAS doctor make a correct diagnosis and plan adequate treatment.
- Future activities: the possibility of carrying out preventive medicine tests using telemedicine technologies could be considered in the future as a fundamental element for remote maritime preventive medicine practice. Specific experimental studies of devices integrated into platforms, protocols, and patient satisfaction should be conducted, possibly using targeted comparisons with traditional systems.
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- A Health Telematics Policy in Support of WHO’s Health-for-All Strategy for Global Health Development; Report of the WHO Group Consultation on Health Telematics; World Health Organization: Geneva, Switzerland, 1997; pp. 11–16.
- Sagaro, G.G.; Amenta, F. Past, present, and future perspectives of telemedical assistance at sea: A systematic review. Int. Marit. Health 2020, 71, 97–104. [Google Scholar] [CrossRef]
- Craig, J.; Patterson, V. Introduction to the practice of telemedicine. J. Telemed. Telecare 2005, 11, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Telemedicine: Opportunities and Developments in Member States; Report on the Second Global Survey on EHealth; World Health Organization: Geneva, Switzerland, 2009.
- Combi, C.; Pozzani, G.; Pozzi, G. Telemedicine for Developing Countries. Appl. Clin. Inform. 2016, 7, 1025–1050. [Google Scholar] [CrossRef]
- International Labour Organisation. Medical Advice at Sea Recommendation, 1958 (No. 106). Available online: https://www.ilo.org/dyn/normlex/en/f?p=NORMLEXPUB:12100:0::NO::P12100_ILO_CODE:R106 (accessed on 20 July 2020).
- Bloor, M.; Thomas, M.; Lane, T. Health risks in the global shipping industry: An overview. Health Risk Soc. 2000, 2, 329–340. [Google Scholar] [CrossRef]
- Oldenburg, M.; Baur, X.; Schlaich, C. Occupational Risks and Challenges of Seafaring. J. Occup. Health 2010, 52, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Hemmingsson, T.; Lundberg, I.; Nilsson, R.; Allebeck, P. Health-related selection to seafaring occupations and its effects on morbidity and mortality. Am. J. Ind. Med. 1997, 31, 662–668. [Google Scholar] [CrossRef]
- Nittari, G.; Tomassoni, D.; Di Canio, M.; Traini, E.; Pirillo, I.; Minciacchi, A.; Amenta, F. Overweight among seafarers working on board merchant ships. BMC Public Health 2019, 19. [Google Scholar] [CrossRef]
- Jaremin, B.; Kotulak, E.; Starnawska, M.; Tomaszunas, S. Causes and Circumstances of Deaths of Polish Seafarers During Sea Voyages. J. Travel Med. 1996, 3, 91–95. [Google Scholar] [CrossRef]
- Yılmaz, F. Marine Mi-Gjosa. An Analysis of Marine Casualties of Turkish Flagged Ships and Effects on Sea-Men. Available online: http://www.gmoshipmar.org/jvi.aspx?pdir=gmo&plng=eng&un=GMO-99608&look4= (accessed on 20 July 2020).
- Lalić, H. Occupational medicine professor’s participation in erasmus+: Academic staff exchange programme. Coll Antropol. 2017, 41, 305–308. [Google Scholar]
- Williams, A.M.; Bhatti, U.F.; Alam, H.B.; Nikolian, V.C. The role of telemedicine in postoperative care. mHealth 2018, 1–9. [Google Scholar] [CrossRef]
- Adler-Milstein, J.; Kvedar, J.; Bates, D.W. Telehealth Among US Hospitals: Several Factors, Including State Reimbursement and Licensure Policies, Influence Adoption. Health Aff. 2014, 33, 207–215. [Google Scholar] [CrossRef]
- Withnall, R.D.J.; Smith, M.; Graham, D.J.; Morris, L.E. Telemedicine in the UK Defence Medical Services: Time for an upgrade? J. R. Army Med. Corps 2016, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Wilson, L.S.; Maeder, A. Recent Directions in Telemedicine: Review of Trends in Research and Practice. Health Inform. Res. 2015, 21, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Mph, H.S.S.; Hamline, M.Y.; Gosdin, M.M.; Kair, L.R.; Weinberg, G.M.; Marcin, J.P.; Rosenthal, J.L. Acceptability, Usability, and Effectiveness: A Qualitative Study Evaluating a Pediatric Telemedicine Program. Acad. Emerg. Med. 2019, 26, 1022–1033. [Google Scholar] [CrossRef]
- Srinivasan, R.; Ben-Pazi, H.; Dekker, M.; Cubo, E.; Bloem, B. Telemedicine for Hyperkinetic Movement Disorders. Tremor and Other Hyperkinetic Movements. Tremor. Other. Hyperkinetic. Mov. 2020, 1–8. [Google Scholar] [CrossRef]
- Demaerschalk, B.M.; Berg, J.; Chong, B.W.; Gross, H.; Nystrom, K.; Adeoye, O.; Schwamm, L.; Wechsler, L.; Whitchurch, S. American Telemedicine Association: Telestroke Guidelines. Telemed. eHealth 2017, 376–389. [Google Scholar] [CrossRef]
- Hazenberg, C.E.V.B.; De Stegge, W.B.A.; Van Baal, S.G.; Moll, F.L.; Bus, S.A. Telehealth and telemedicine applications for the diabetic foot: A systematic review. Diabetes Metab. Res. Rev. 2020, e3247. [Google Scholar] [CrossRef] [PubMed]
- Bashshur, R.L.; Shannon, G.W.; Bashshur, N.; Yellowlees, P.M. The Empirical Evidence for Telemedicine Interventions in Mental Disorders. Telemed. eHealth 2016, 22, 87–113. [Google Scholar] [CrossRef] [PubMed]
- Endler, M.; Lavelanet, A.; Cleeve, A.; Ganatra, B.; Gomperts, R.; Gemzell-Danielsson, K. Telemedicine for medical abortion: A systematic review. BJOG Int. J. Obstet. Gynaecol. 2019, 126, 1094–1102. [Google Scholar] [CrossRef] [PubMed]
- Abel, E.A.; Shimada, S.L.; Wang, K.; Ramsey, C.; Skanderson, M.; Erdos, J.; Godleski, L.; Houston, T.K.; Brandt, C.A.; Whealin, J.; et al. Dual Use of a Patient Portal and Clinical Video Telehealth by Veterans with Mental Health Diagnoses: Retrospective, Cross-Sectional Analysis. J. Med. Internet Res. 2018, 20. [Google Scholar] [CrossRef] [PubMed]
- Spencer, T.; Noyes, E.; Biederman, J. Telemedicine in the Management of ADHD: Literature Review of Telemedicine in ADHD. J. Atten. Disord. 2019, 24, 3–9. [Google Scholar] [CrossRef]
- International Labour Organisation. Guidelines on the Medical Examinations of Seafarers Sectoral Activities Pro-gramme. Available online: www.ilo.org/publns (accessed on 23 December 2020).
- Legislative Decree n. 81. Available online: https://www.gazzettaufficiale.it/eli/id/2008/04/30/008G0104/sg (accessed on 20 July 2020).
- Legislative Decree n. 271. Available online: https://www.gazzettaufficiale.it/eli/id/1999/08/09/099G0350/sg (accessed on 20 July 2020).
- Legislative Decree n. 626. Available online: https://www.gazzettaufficiale.it/eli/id/1994/11/12/094G0610/sg (accessed on 20 July 2020).
- De Rosa, C.; Di Mizio, G.; Ricci, P. Accidents and occupational diseases in seafarers: Role of health surveillance. Soc Def. 2005, 84, 129–136. [Google Scholar]
- Mahdi, S.S.; Amenta, F. Eighty years of CIRM. A journey of commitment and dedication in providing maritime medical assistance. Int. Marit. Health 2016, 67, 187–195. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Iannitti, T.; Di Cerbo, A.; Morales-Medina, J.C.; Palmieri, B. Narrative review of telemedicine consultation in medical practice. Patient Prefer. Adherence 2015, 9, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Molinari, G.; Molinari, M.; Di Biase, M.; Brunetti, N.D. Telecardiology and its settings of application: An update. J. Telemed. Telecare 2017, 24, 373–381. [Google Scholar] [CrossRef]
- Inglis, S.C.; Clark, R.A.; McAlister, F.A.; Ball, J.; LeWinter, C.; Cullington, D.; Stewart, S.; Cleland, J.G. Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database Syst. Rev. 2010. [Google Scholar] [CrossRef]
- Lin, C.-T.; Chang, K.-C.; Lin, C.-L.; Chiang, C.-C.; Lu, S.-W.; Chang, S.-S.; Lin, B.-S.; Liang, H.-Y.; Chen, R.-J.; Lee, Y.-T.; et al. An Intelligent Telecardiology System Using a Wearable and Wireless ECG to Detect Atrial Fibrillation. IEEE Trans. Inf. Technol. Biomed. 2010, 14, 726–733. [Google Scholar] [CrossRef] [PubMed]
- Ong, M.K.; Romano, P.S.; Edgington, S.; Aronow, H.U.; Auerbach, A.D.; Black, J.T.; De Marco, T.; Escarce, J.J.; Evangelista, L.S.; Hanna, B.; et al. Effectiveness of Remote Patient Monitoring After Discharge of Hospitalized Patients with Heart Failure: The Better Effectiveness After Transition–Heart Failure (BEAT-HF) Randomized Clinical Trial. JAMA Intern. Med. 2016, 176, 310–318. [Google Scholar] [CrossRef]
- Chaudhry, S.I.; Mattera, J.A.; Curtis, J.P.; Spertus, J.A.; Herrin, J.; Lin, Z.; Phillips, C.O.; Hodshon, B.V.; Cooper, L.S.; Krumholz, H.M. Telemonitoring in Patients with Heart Failure. N. Engl. J. Med. 2010, 363, 2301–2309. [Google Scholar] [CrossRef]
- Majumder, S.; Mondal, T.K.; Deen, M.J. Wearable Sensors for Remote Health Monitoring. Sensors 2017, 17, 130. [Google Scholar] [CrossRef] [PubMed]
- Sohn, S.; Helms, T.M.; Pelleter, J.T.; Müller, A.; Kröttinger, A.I.; Schöffski, O. Costs and Benefits of Personalized Healthcare for Patients with Chronic Heart Failure in the Care and Education Program “Telemedicine for the Heart”. Telemed. eHealth 2012, 18, 198–204. [Google Scholar] [CrossRef] [PubMed]
- De Lazzari, C.; Pisanelli, D.M.; D’Ambrosi, A.; Genuini, I.; Fedele, F. Telecardiology in Italy: Current realizations and future prospects. Front Artif. Intell. Appl. 2011, 231, 315–330. [Google Scholar] [CrossRef]
- De Lazzari, C.; Genuini, I.; Gatto, M.C.; Cinque, A.; Mancone, M.; D’Ambrosi, A.; Silvetti, E.; Fusto, A.; Pisanelli, D.M.; Fedele, F. Screening high school students in Italy for sudden cardiac death prevention by using a telecardiology device: A retrospective observational study. Cardiol. Young 2016, 27, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Lupi, L.; Glisenti, F.; Papa, I.; Arabia, G.; Piazzani, M.; Fabbricatore, D.; Castiello, A.; Madureri, A.; Nodari, S. P4234A telemonitoring program for screening and primary and secondary prevention of cardiovascular disease. Eur. Heart J. 2018, 39, 860. [Google Scholar] [CrossRef]
- Yeong, K.S.; Kang, D.M.; Kim, J.I. 802 Spirometry longitudinal data analysis software (spirola) for respiratory disease prevention among shipyard welders in South Korea. Respir. Disord. 2018, 91, A460. [Google Scholar]
- Wheatley, J. Spirometry: Key to the diagnosis of respiratory disorders. Med. J. Aust. 2017, 207, 422–424. [Google Scholar] [CrossRef] [PubMed]
- Molina-Bastos, C.G.; Gadenz, S.D.; Angela, M.; Moreira, F. Telespirometry in primary health care: A randomized clinical trial in southern Brazil (research protocol). J. Bras. Telessaúde Rio Jan. 2016, 4, 82–83. [Google Scholar]
- Averame, G.; Bonavia, M.; Ferri, P.; Moretti, A.M.; Fogliani, V.; Cricelli, C.; Canonica, G.W.; Grassi, C.; Paggiaro, P.L.; Rossi, A. Office spirometry can improve the diagnosis of obstructive airway disease in primary care setting. Respir. Med. 2009, 103, 866–872. [Google Scholar] [CrossRef][Green Version]
- De Toledo, P.; Jimenez, S.; Del Pozo, F. A telemedicine system to support a new model for care of chronically ill patients. J. Telemed. Telecare 2002, 8, 17–19. [Google Scholar] [CrossRef]
- Alrajab, S.; Smith, T.; Owens, M.; Areno, J.P.; Caldito, G. A Home Telemonitoring Program Reduced Exacerbation and Healthcare Utilization Rates in COPD Patients with Frequent Exacerbations. Telemed. eHealth 2012, 18, 772–776. [Google Scholar] [CrossRef]
- Jouneau, S.; Dres, M.; Guerder, A.; Bele, N.; Bellocq, A.; Bernady, A.; Berne, G.; Bourdin, A.; Brinchault, G.; Burgel, P.R.; et al. Management of acute exacerbations of chronic obstructive pulmonary disease (COPD). Guidelines from the Société de pneumologie de langue française (summary). Rev. Mal. Respir. 2017, 34, 282–322. [Google Scholar] [CrossRef] [PubMed]
- Vitacca, M.; Rossin, M.; Assoni, G.; Baratti, D.; Zanardini, M.; Ruocco, G.; Quinto, T.; Bernasconi, A.; Scalvini, S.; Colombo, F. Tele-assistance Respiratory Card: Feasibility of Self-Reporting in Patients with Severe COPD. Telemed. eHealth 2013, 19, 99–103. [Google Scholar] [CrossRef]
- Ohberg, F.; Wadell, K.; Blomberg, A.; Claesson, K.; Edstrom, U. Home-Based System for Recording Pulmonary Function and Disease-Related Symptoms in Patients with Chronic Obstructive Pulmonary Disease, COPD-A Pilot Study. SM J. Pulm. Med. 2016, 2, 1011. [Google Scholar]
- Kupczyk, M.; Hofman, A.; Kołtowski, Ł.; Kuna, P.; Łukaszyk, M.; Buczyłko, K.; Bodzenta-Łukaszyk, A.; Nastałek, P.; Soliński, M.; Dąbrowiecki, P. Home self-monitoring in patients with asthma using a mobile spirometry system. J. Asthma 2020, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Redlich, C.A.; Tarlo, S.M.; Hankinson, J.L.; Townsend, M.C.; Eschenbacher, W.L.; Von Essen, S.G.; Sigsgaard, T.; Weissman, D.N. Official American Thoracic Society Technical Standards: Spirometry in the Occupational Setting. Am. J. Respir. Crit. Care Med. 2014, 189, 983–993. [Google Scholar] [CrossRef]
- Stout, J.W.; Smith, K.; Zhou, C.; Solomon, C.; Dozor, A.J.; Garrison, M.M.; Mangione-Smith, R. Learning from a Distance: Effectiveness of Online Spirometry Training in Improving Asthma Care. Acad. Pediatr. 2012, 12, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Fung, A.G.; Tan, L.; Duong, T.N.; Schivo, M.; Littlefield, L.; Delplanque, J.-P.; Davis, C.E.; Kenyon, N.J.; Fung, T. Design and Benchmark Testing for Open Architecture Reconfigurable Mobile Spirometer and Exhaled Breath Monitor with GPS and Data Telemetry. Diagnostics 2019, 9, 100. [Google Scholar] [CrossRef]
- Bruttomesso, D.; Laviola, L.; Avogaro, A.; Bonora, E.; Del Prato, S.; Frontoni, S.; Orsi, E.; Rabbone, I.; Sesti, G.; Purrello, F. The use of real time continuous glucose monitoring or flash glucose monitoring in the management of diabetes: A consensus view of Italian diabetes experts using the Delphi method. Nutr. Metab. Cardiovasc. Dis. 2019, 29, 421–431. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Gutierrez, R.; Gonzalez-Gonzalez, J.G.; Zuñiga-Hernandez, J.A.; McCoy, R.G. Benefits and harms of intensive glycemic control in patients with type 2 diabetes. BMJ 2019, 367, l5887. [Google Scholar] [CrossRef]
- Hannemann-Pohl, K.; Kampf, S.C. Automation of Urine Sediment Examination: A Comparison of the Sysmex UF-100 Automated Flow Cytometer with Routine Manual Diagnosis (Microscopy, Test Strips, and Bacterial Culture). Clin. Chem. Lab. Med. 1999, 37, 753–764. [Google Scholar] [CrossRef]
- Langlois, M.R.; Delanghe, J.R.; Steyaert, S.R.; Everaert, K.C.; De Buyzere, M.L. Automated Flow Cytometry Compared with an Automated Dipstick Reader for Urinalysis. Clin. Chem. 1999, 45, 118–122. [Google Scholar] [CrossRef]
- Mohammadi, S.; Maeki, M.; Mohamadi, R.M.; Ishida, A.; Tani, H.; Tokeshi, M. An instrument-free, screen-printed paper microfluidic device that enables bio and chemical sensing. Analyst 2015, 140, 6493–6499. [Google Scholar] [CrossRef]
- Ginardi, R.V.H.; Saikhu, A.; Sarno, R.; Sunaryono, D.; Kholimi, A.S.; Shanty, R.N.T. Intelligent Method for Dipstick Urinalysis Using Smartphone Camera. In Lecture Notes in Computer Science; Springer: Berlin, Germany, 2014; Volume 8407, pp. 66–77. [Google Scholar]
- Lee, D.-S.; Jeon, B.G.; Ihm, C.; Park, J.-K.; Jung, M.Y. A simple and smart telemedicine device for developing regions: A pocket-sized colorimetric reader. Lab Chip 2011, 11, 120–126. [Google Scholar] [CrossRef]
- Soldat, D.J.; Barak, P.; Lepore, B.J. Microscale Colorimetric Analysis Using a Desktop Scanner and Automated Digital Image Analysis. J. Chem. Educ. 2009, 86, 617–620. [Google Scholar] [CrossRef]
- Montangero, M. Determining the Amount of Copper(II) Ions in a Solution Using a Smartphone. J. Chem. Educ. 2015, 92, 1759–1762. [Google Scholar] [CrossRef]
- Nittari, G.; Khuman, R.; Baldoni, S.; Pallotta, G.; Battineni, G.; Sirignano, A.; Amenta, F.; Ricci, G. Telemedicine Practice: Review of the Current Ethical and Legal Challenges. Telemed. J. E Health 2020, 26, 1427–1437. [Google Scholar] [CrossRef]
- Pirillo, I.; Amenta, F.; Sirignano, A.; Ricci, G. Cross-border healthcare: Implementation of Directive 2011/24/EU and National Contact Point in Italy. Travel. Med. Infect. Dis. 2017, 18, 79–80. [Google Scholar] [CrossRef]
| Area of Application | Medical Examination/Test | Purpose of Application | Outcome | Reference(s) |
|---|---|---|---|---|
| Telecardiology | Electrocardiogram (ECG) |
|
| Molinari G. et al. [33] Inglis S.C. et al. [34] Lin C.T. et al. [35] Ong M.K. et al. [36] Herrin J. et al. [37] Majumder S. et al. [38] Sohn S. et al. [39] De Lazzari C. et al. [40] De Lazzari C. et al. [41] Lupi, L. et al. [42] |
| Telespirometry | Spirometric test |
|
| Kim et al. [43] Zealand N. [44] Molina-bastos C.G. et al. [45] Averame G. et al. [46] Toledo P.D. et al. [47] Owens M. et al. [48] Jouneau S. et al. [49] Vitacca M. et al. [50] Ohberg F. et al. [51] Kupczyk M. et al. [52] Redlich C.A. et al. [53] Stout J.W. et al. [54] Fung A.G. et al. [55] |
| Tele-diabetology | Blood glucose monitoring |
|
| Bruttomesso D. et al. [56] Rodriguez-Gutierrez R. et al. [57] |
| Telenephrology | Urinalysis |
|
| Hannemann-Pohl K. et al. [58] Langlois M.R. et al. [59] Mohammadi S. et al. [60] Ginardi R.V.H. et al. [61] Lee D.S. et al. [62] Soldat D.J. et al. [63] Montangero M [64] |
| Features | Medical Examination | Periodicity | Telemedicine Modality | Equipment |
|---|---|---|---|---|
| General well-being | Medical history | Annual basis | Video, e-mail | Telemedicine devices |
| Noise | Audiometry test | Annual basis | Audio, video | Telemedical devices |
| General well-being Stress-related | Electrocardiogram (ECG), spirometry, urinalysis | Every six months | Still image Video | Telemedical devices |
| Vibrations | Postural evaluation: manual handling of loads | Annual basis | Video | Telemedicine devices |
| Exposure to toxic substances | Blood chemistry tests aimed at checking cardiovascular and renal function (blood count, blood sugar, liver and kidney function, lipid structure); leukocyte formula, urinalysis, determination of urinary hydroxypyrene. | Annual basis | E-mail, audio, video | Telemedicine devices |
| Pulse oximetry, blood pressure | Every month | Video, e-mail | Telemedical devices | |
| Postural workload | Body mass index evaluation; postural evaluation | Annual basis | Video | Telemedical devices |
| Fatigue and stress assessment | Electrocardiogram and saturimetry for fatigue; stress assessment, see the appropriate section of this protocol | Annual basis | Video, e-mail | Telemedical devices |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sagaro, G.G.; Di Canio, M.; Talevi, E.; Amenta, F. Telemedicine for Pre-Employment Medical Examinations and Follow-Up Visits on Board Ships: A Narrative Review on the Feasibility. Healthcare 2021, 9, 69. https://doi.org/10.3390/healthcare9010069
Sagaro GG, Di Canio M, Talevi E, Amenta F. Telemedicine for Pre-Employment Medical Examinations and Follow-Up Visits on Board Ships: A Narrative Review on the Feasibility. Healthcare. 2021; 9(1):69. https://doi.org/10.3390/healthcare9010069
Chicago/Turabian StyleSagaro, Getu Gamo, Marzio Di Canio, Emanuele Talevi, and Francesco Amenta. 2021. "Telemedicine for Pre-Employment Medical Examinations and Follow-Up Visits on Board Ships: A Narrative Review on the Feasibility" Healthcare 9, no. 1: 69. https://doi.org/10.3390/healthcare9010069
APA StyleSagaro, G. G., Di Canio, M., Talevi, E., & Amenta, F. (2021). Telemedicine for Pre-Employment Medical Examinations and Follow-Up Visits on Board Ships: A Narrative Review on the Feasibility. Healthcare, 9(1), 69. https://doi.org/10.3390/healthcare9010069








