1. Introduction
The recent crisis that the entire world is facing caused by COVID-19, a pandemic that has forced all organizations, whether public or private, to rethink their mission and vision. Thus, the efficacy of the healthcare sector depends greatly on the rapidity to adapt to the new dramatic situation. Before the World Health Organisation (WHO) had declared the COVID-19, a pandemic crisis, on 11 March 2020, Algeria had the situation under control, although the first two cases were registered on 25 February 2020. The rapid evolution of the pandemic coronavirus crisis requires that the common strategies should be oriented toward ensuring the health of the population and a continuous assessment of the events to give priority to future needs. The situation in Algeria is not far from the rest of the world, with a total of 55,081 cases and 1880 deaths recorded until 22 October 2020, with a mortality rate of 11.70% [
1]. This high rate represents a threat to the national health situation of the country that leads to making a study to understand how the healthcare sector is dealing with this crisis and what are the available and efficient managerial tools to help managers and healthcare staff to better control facilities [
2].
The international statistics of WHO [
3] place Algeria in the fourth position in Africa (with 50,914 cases) after South Africa (with 669,498 cases), Ethiopia (with 72,700 cases), and Uganda (with 7364 cases) with a total of 1,172,342 confirmed cases and 25,481 deaths in the continent as the last update.
Watkins et al. [
4] analysed the impact of the pandemic situation on SMEs from Australia and they observed that only six per cent of Australian SMEs had a plan for avoiding the pandemic crisis. Thus, the other 39 per cent consider that the pandemic has no impact on their business and over 60 percent called upon the need to prepare a viable strategy to tackle a pandemic situation. As a result, in 2007, the Australian SMEs were not prepared for a pandemic situation and 13 years later SMEs worldwide are in the same situation.
Watkins et al. [
5] considered that a strategy for the pandemic situation among SMEs depends on the perception of the risk level and the resources that are available to prepare and frame the strategy.
Ivo Hristov and Antonio Chirico [
6] identified the impact of key performance indicators (KPIs) on company performance in the framework of sustainable strategies and they arrived at the conclusion that existing literature does not provide ample evidence about how to address the crises from managerial perspective.
At this moment, healthcare managers, officials, and policymakers are seeking to answer the following questions:
How will we manage to streamline the healthcare sector in real-time to overcome this pandemic generated by the novel coronavirus?
Can KPIs be used as a tool enabling a quick reaction of the healthcare sector’s facilities to the adverse effects of COVID-19?
What is the possible set of KPIs that leaders in the healthcare sector are required to check in order to deal with the consequences of the virus and re-establish “normality” in the social and business environment?
The answers to these questions were found in the last months from many scholars around the world from economic point of view, but not from the healthcare sector perspective [
7,
8,
9,
10]
These analyses motivated us to approach this pandemic crisis from another perspective based on KPIs as instruments of human competencies in the fight against this enemy.
The range of factors affecting sustainability performance is varied, from the small details to the big issues in healthcare facilities. Thus, most of them are not obvious to the decision makers (e.g., maintenance and building design) because of lack of technical skills (e.g., attention towards the aspects of bioclimatic passive strategies and incorrect architectural and flexible layouts, which often limit the clinical processes and causes the decrease of performance and sustainability criteria) [
11].
The use of KPIs as tools to improve the effect of public health measures and as indicators of the measures that need to change in function of true morbidity and mortality rates.
3. Methodology
To select the KPIs, we have conducted in-depth interviews with four health management experts and one assistant professor from the Faculty of Medicine of Constantine 3 Salah Boubnider University to discuss and identify a list from the extracted indicators of literature review (185). The first set of indicators was developed from the literature review: 158 indicators were extracted from the discussions with the experts and were selected, then 62 indicators were divided into four main domains for sustainability assessment: social, economic, technical, and internal processes. The selected indicators were used to design the questionnaire for the first round of the Delphi method.
In the second stage, in consensus with Galanis [
30], we employed the Delphi method in two rounds. In the first round, 20 public hospitals and managers for each hospital have been chosen to participate in the research, as they were involved in sustainability. The questionnaires were distributed to managers to investigate the implication of KPI’s for primary healthcare facilities’ sustainability performance.
In the second round, we distributed the questionnaires to the same hospitals’ managers, and, in this stage, we eliminated the indicators with the lowest mean scores. After we received the feedback from the managers, we reduced the number of KPIs (we eliminated 22 indicators) and 41 KPIs were included in the final setup of our research.
This quantitative study has been conducted from the first week of recording the first three cases of COVID-19 disease in Algeria until the end of August 2020; investigation was made in two main wilayas: El Taref and Constantine, including different type of facilities: university hospital, public hospital centers, and neighbourhood’s healthcare facilities.
During February–August 2020, a total of 300 questionnaires were distributed to Algerian hospitals that were identified as very important hospitals in the framework of the pandemic coronavirus. In total, 210 completed responses (response rate of 70 percent) were collected from medical staff who are directly involved in the battle with this invisible enemy. Respondents were required to evaluate the importance of every KPIs using a five-point Likert scale (1—not important at all to 5—very important).
We chose to use the SmartPLS [
31] method to analyse the data and we started the research by assessing the measurement model to ensure that each construct’s KPIs are reliable and valid.
3.1. Sample
The 88 respondents (41.9%) were from facilities situated in El Taref and 122 respondents (58.1%) from facilities situated in Constantine. The gender of the respondents was balanced with 96 females (45.7%) and 114 males (54.3%). The age of the respondents was distributed as follows: 21.4% between ages of 25 and 35 years, 37.6% between ages of 36 and 45 years, 24.3 between ages of 46 and 55 years, and 16.7% between ages of 56 years and over (M = 2.36; SD = 0.999).
A total of 109 respondents participated in the pilot study and at the final of this study all 41 KPIs were retained because they registered a loading factor above the threshold of 0.70 (
Appendix E), in consensus with Sarstedt et al. [
32].
3.2. Measures
We started the research by assessing the measurement model to ensure that each construct’s KPIs are reliable and valid.
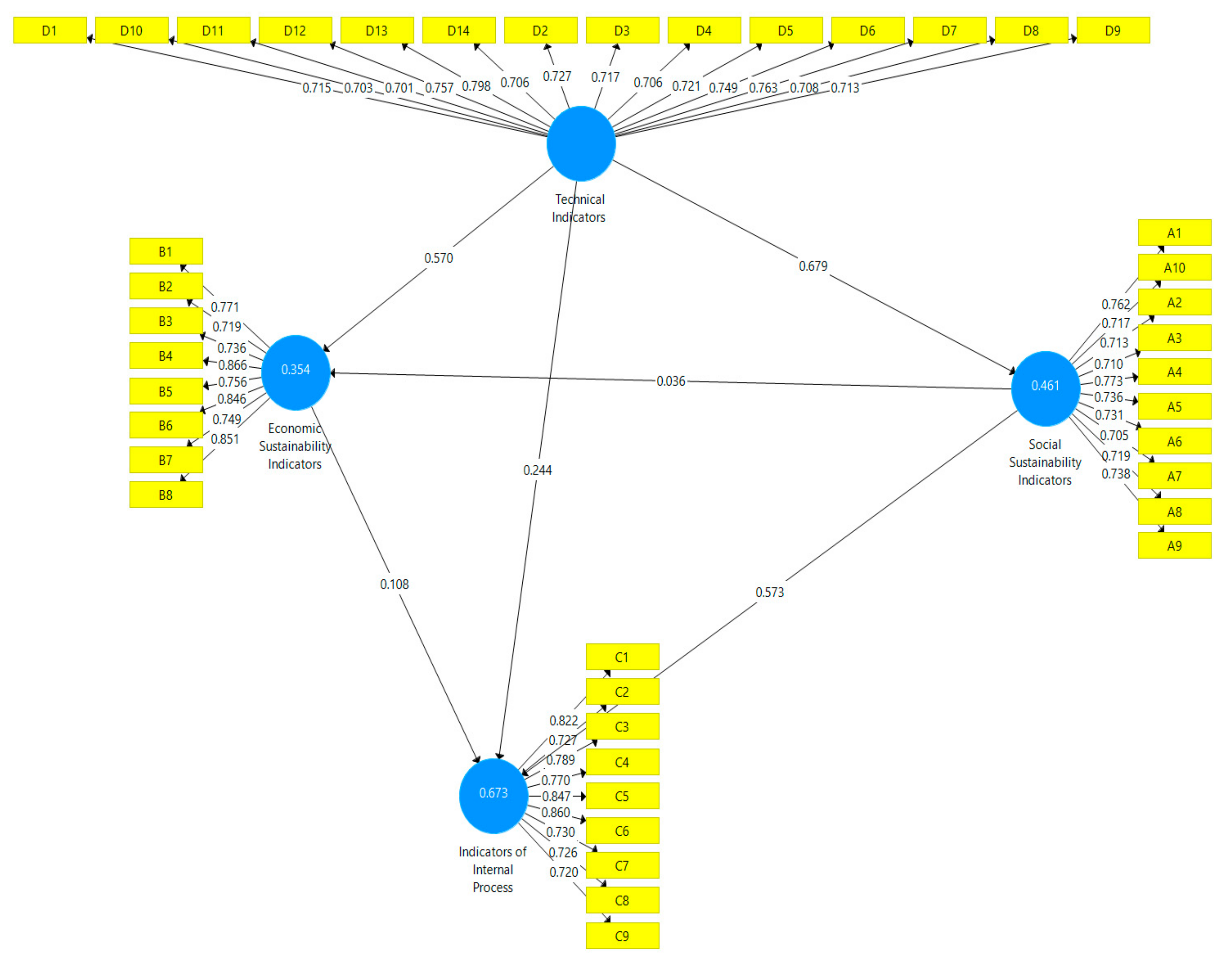
Internal consistency of the research model was assessed by partial least squares structural equation modelling (PLS-SEM), we started by examining the indicator loadings [
32], ranging from 0.701 to 0.866 and indicating that the KPIs have a very good degree of reliability (
Appendix E).
Next, we calculated the “reliability indicators” and higher values indicate increased levels of reliability. The main indicators exceed the minimum threshold of 0.7 [
33] as follows: Cronbach’s Alpha that measures internal consistency reliability ranged from 0.903 to 0.932 and represent good to very good reliability levels of KPIs, Dijkstra-Henseler’s rho_A ranged from 0.907 to 0.934 [
34] and composite reliability (CR) ranged from 0.920 to 0.940. Thus, all the values exceed the minimum threshold value of 0.7 for all variables indicating that the measurement model has good reliability (
Table 1).
The descriptive statistics indicate the values of the mean and we observe that a mean value of 4.01 out of 5 suggests that most of the respondents mainly agreed that IIP is very important KPIs for the healthcare system in a pandemic situation. Meanwhile, the SSI registered the lowest value (3.86) and an explanation consists of the particularity of this period and on pressure existing on medical personnel.
The pressure is reflected on value of loading factor of the IIP-C6 (Medical errors = 0.860), followed by IIP-C5 (Clinical errors = 0.847); IIP-C1 (Medication errors −0.822); IIP-C3 (Mortality rate = 0.789); IIP-C4 (Infection rate = 0.770) and finally IIP-C9 (Laboratory test time = 0.720).
The standard deviation shows that there are no relevant differences among the KPIs as the values are close to one another for ESI, IIP, and TI (ranged from 0.648 to 0.673); only SSI registered a value above 0.770.
We evaluated the extent to which any selected construct differs from the others and we tested the “convergent validity” and we used the average variance extracted values that are greater than 0.5 (from 0.530 to 0.622) and validate the latent variables for our model composition, in consensus with Hair et al. [
35].
Average variance extracted (AVE) analysis was conducted for evaluating if we have a good convergent discriminant validity and if each construct exceeds the threshold value of 0.50. The result proves that all KPIs are retained.
The results prove that the indicators of internal process have the highest value of Cronbach alpha (0.918) which highlights the importance of this group of indicators in the context of the current pandemic coronavirus crisis.
We continued to assess the “discriminant validity” by calculating the Fornell and Larcker [
36] criterion and for proving the relevance of the structural model. The highest correlation was registered between ESI-ESI (0.788) and the lowest correlation was registered between ESI-SSI (0.423).
In order to consolidate the assessment of the discriminant validity in variance-based structural equation modelling we used Heterotrait–Monotrait ratio (HTMT), which is considered superior to previous indicators [
37] as Fornell–Larcker criterion and (partial) cross-loadings (
Table 2).
The results show that the values of HTMT were smaller than 0.90 (ranged from 0.420 to 0.848), which means that this ratio meets the requirements of the Henseler et al. [
38]. In order to sum, the model assessments prove a good evidence of validity and reliability.
4. Results and Discussion
The correlation between KPIs was used for verifying the relationship between all variables (
Table 3).
The correlations between variables reveal to us that the age of respondents negatively influences three KPIs (IIP, ESI, and TI) and prove that under pressure the experience of the medical personnel is important for the decision-making process. The age of respondents is positively correlated with patient satisfaction, because no matter their age, the healthcare system employees are devoted to their job and to their patients.
The gender of respondents and the location directly and negatively influence two KPI’s (ESI and TI) and directly and positively influence the other two KPIs (SSI and IIP). These correlations prove that the practical KPIS as ESI and TI are perceived as having a negative influence on decision-making process under pressure.
The location is an important variable, because the patients with COVID-19 are in some regions and they are treated in hospitals specially designated for this disease. Algeria has a public healthcare sector and it is accessible and free of charge for all citizens, financed by the government, given Algeria’s young population. In close alignment with this long-term strategy, the government maintains an intensive immunization program.
The correlations between IIP and the other three KPIs are positive and prove that internal process is developed for the purpose of patient satisfaction (0.783) and considering the consequences of the infection with COVID-19, IIP is related to facilities of the hospital (0.685) in terms of qualitative and especially, quantitative KPIs.
We analyse the results and we first test the collinearity of the research model and we observe that the variance inflation factor VIF values ranged from 1.897 (Hospital readmission rate) to 3.852 (Indoor air quality) and is within the limits recommended by Hair et al. [
35].
The results prove that there is no collinearity problem interfering with our KPIs and we continued to evaluate the research model by interpreting the coefficient of determination (R2),
f2, and
P. The coefficient of determination between 0.25 and 0.50 is considered good and above 0.50 are considered very well.
Figure 1 shows values of R
2, ranged from 0.254 to 0.673. In conclusion, the predictive power of the model and R
2.
We arrived at the conclusion that all the KPIs are valid and reliable and we assess the research model and test the hypotheses (
Table 4).
The resulting effect size value of each KPI in the model ranges from 0.001 to 0.855, which are included in the category of very small to large [
39]. The value of goodness of fit that is generated through the standardized root mean squared residual (SRMR) is equal to 0.08, which means that our model fits the empirical data [
40]. We also tested our hypotheses with the coefficient parameter and the significant value generated from the 95% bias-corrected confidence intervals of each KPI.
The path coefficients provide significant value (at the p 0.05 level), only the relationship SSI -> ESI is not supported. Thus, the value of the coefficient (T) to the relationship SSI -> ESI is 0.491 with a p-value < 0.623. In conclusion, all hypotheses are supported except for the second hypothesis.
The particularities of our study due to the pandemic crisis do not allow us to affirm that our results support previous studies, because not many studies related to KPIs were developed during the pandemic crisis.
We can link these results to the pandemic crisis when the communication process and human factors are more important than economic and material factors. Hospital performance is a reference to key performance indicators (KPIs), especially to IIP and TI as promoters of ESI and SSI, because in this period quantitative assessments of hospitals became an indicator of the capacity of them to achieve the new goals by making efficient use of the limited resources available in the crisis period. This signifies that TI can be used to improve SSI and the ESI have a positive effect on IIP.
Healthcare facilities all over the world are dealing with major challenges to keep operating in a performing way during crisis time especially when it’s facing a world pandemic such as Covid-19. This pandemic coronavirus took by surprise both the decision-makers and the employees who faced an unpredictable enemy and impossible to be controlled. The fact that many organizations, public or private, were forced to discontinue their activity for an unspecified period of time has created a state of panic and uncertainty, upsetting society at all levels.
Our findings proved that KPIs play an important role in increasing the performance of healthcare systems, and, especially during the pandemic coronavirus crisis (
Appendix F).
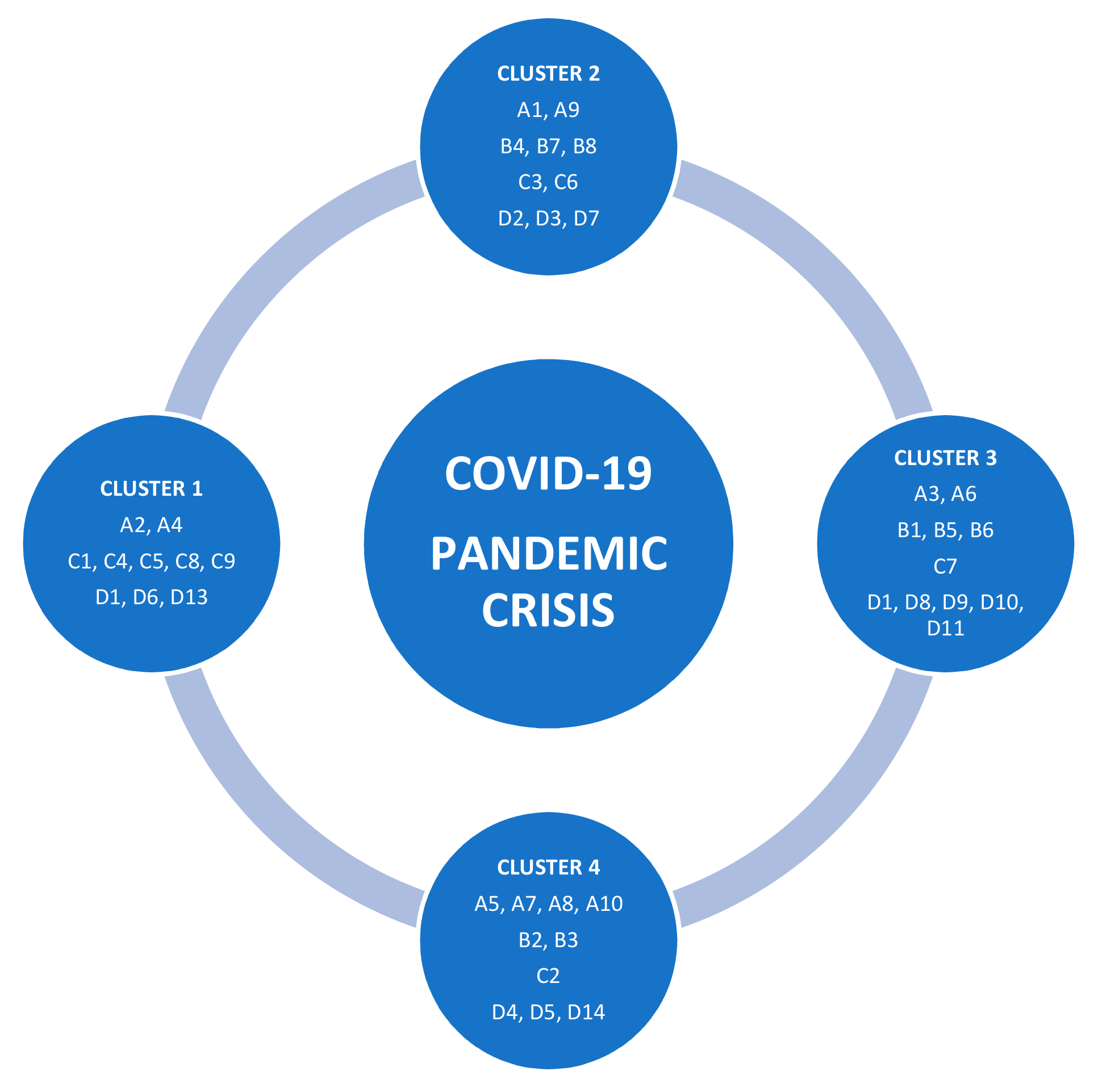
Figure 2 shows the four clusters of KPIs that can be a priority for hospital managers in a crisis period and every cluster includes different KPIs ranked by importance.
The first cluster includes 10 KPIs, two KPIs of SSI (related to the average hospital stay and on patient waiting time), five KPIs of IIP (related to clinical and medication errors, infection rate, average length of stay in the emergency room, and laboratory test time), and the other three KPIs are from TI as indoor air quality, sufficient air conditioning, and location of the facility.
This cluster proves the importance of this indicator in a crisis because under pressure and in very stressful conditions the decisions made by doctors concerning medical prescriptions or dozes might be mistaken [
41]. Clinical errors tracking and assessment appears to be significant in crisis time and can affect the medical staff and equipment’s effectiveness. The sufficient air conditioning allows checking the sufficiency of air out of the facility’s HVAC system to ensure the well-being of staff and patients inside the healthcare facility. This indicator is crucial for the patients because one of the causes of death is insufficiency respiratory. Waiting time in the emergency room shows the value of assessing this metric in order to set less waiting time targets in crisis time.
These findings are in consensus with the findings of Mohamed Khalifa and Parwaiz Khalid [
12] who considered that patient safety and infection control rates are very important indicators to gauge the quality of the healthcare system.
The second cluster comprises the other 10 KPIs as follow: two KPIs of SSI that measure the patient satisfaction and patient transfer rate to other facilities, three KPIs of ESI that indicate average care costs of insured patients, cost of work-staff and current cost per bed; two KPIs of IIP related to mortality rate and to medical errors, and three KPIs of TI concerning natural light penetration, vertical circulation and degree of thermal comfort. Patient satisfaction measures the degrees to which the medical service responds to patients’ expectations is a high priority for the management strategy in a pandemic crisis. Mortality rate measures the rate of deaths while in a world pandemic and it is considered a structural tool for decision-making and setting the facility’s strategy to deal with the crisis according to the given number. The degree of thermal comfort could affect or be affected by other technical and internal processes indicators related to the wellbeing inside the facility.
The third cluster includes 11 KPIs structured by categories as following: two KPIs of SSI (related to hospital readmission rate and to waiting time in the emergency room); three KPIs of ESI including average hospital expenses, cost of drugs, and equipment and also average care costs; one KPI of IIP (waiting time for admission to the operating room), and five KPIs of TI (waste management, energy and emissions control, quality of the building envelope, artificial lighting, and water consumption).
The cost of drugs and equipment needs to be taken into consideration because of the increasing of needed medicines, supplies, and special equipment as in a crisis, and to be correlated to the patient waiting time in a crisis that is also important because every patient needs medical care as soon as possible when he/she arrives at the facility to avoid any complications could expose his/her lives to danger. Quality of the building envelope plays a key role in the healthcare environment inside the facility as it controls directly other technical indicators ranked.
The fourth cluster includes 10 KPIs as follows: four KPIs of SSI (patient safety, rate of vacant patients in beds, patient complaint rate, and the number of new patients); two KPIs of ESI concerning average maintenance costs and costs per payer; one KPI of IIP related to bed occupancy rate and three KPIs of TI (acoustic insulation, distributions of medical devices, and hierarchy of functional spaces). The rate of vacant patients in beds allows the facility managers to set their priorities and to make decisions like patients transfer to other departments or facilities. The number of new patients indicates the particularity of this pandemic crisis because it is limited to receive more patients in the facility, because of the virus, which needs to be followed to make sure that the facility is ready for offering care to an expected number of patients. The hierarchy of functional spaces underlines every daily movement of the staff between rooms, controlling, services, and departments. As a result, such a metric gives more flexibility and performance in hard times where every second counts inside the healthcare facility.
The respondents considered as very important two indicators: infection rate and patient safety, because controlling infection rates and applying protocols in healthcare facilities is considered a key practice when facing pandemics. In this situation, patient complaint rate, like the patient’s satisfaction, is not a high priority for healthcare facilities in a pandemic situation.
Waiting time for admission to the operating room gives the facility’s managers a clear vision about the target time to set surgical operations to increase the internal processes performance, going to cost of work-staff that is considered as a lower priority in these circumstances.
Laboratory test time was not considered as a high priority indicator, and this might be justified by the healthcare facilities protocols in case of a pandemic crisis as test samples and results are oriented to the big test labs in the country such as Pasteur Institute.
Our results confirm the findings of McCance et al. [
42] that analysed the eight KPIs clustered within the person-centered processes domain of the framework, and these KPIs were related to patient satisfaction, confidence, and implication in the decision-making process about his/her care.
To prepare action plans for in time strategies and to implement them successfully, the healthcare facilities continue to look for appropriate strategy implementation tools. Consequently, the measurement systems are used to evaluate the effects of the healthcare facilities actions. The role of such system is to support the management process as well as the process of implementation of the hospital’s strategy, which should include not only solid technical and economic factors (particularly financial measures), but also the requirements of the corporate social responsibility and sustainable development standards, as well as the employee relations and value management requirements [
43].
One solution is to use KPIs and keep controlling performance and sustainability through dashboards and scorecards to make frequent and continuous evaluation for the outputs to ensure a better crisis management for healthcare facilities and to make the strategic objectives to be achieved clearer and more convenient. In the case of Algeria, we did not find previous studies about KPIs for evaluation in healthcare facilities from a managerial perspective. For this reason, we consider this study important and it can add a real value to the research, because it helps the managers to evaluate sustainability performance of healthcare facilities in crises.
5. Conclusions
Our findings prove the opportunity for healthcare system employees and not only for hospital managers, to identify critical KPIs in a short period of time and with lower costs. It is very important to consider that the IIP are situated in the first place, which gives us an idea about the priorities of healthcare staff in a crisis. We recommend focalizing the improvements in the areas with high potential to propagate the factors of the pandemic crisis.
In the framework of a pandemic crisis, the performance of healthcare systems is related to its capacity to quickly respond to danger generated by COVID-19. In this period, it is difficult to adapt to an existing model, because the variables are completely different, and the weaknesses of hospitals are also different.
The practical implications are underlined by our model that provides hospitals’ manager’s solutions for the decision making process under pressure indicating the ways of improvements of quality of medical services by implementing suitable KPIs. Thus, these clusters of KPIs can be used as tools for developing sustainable healthcare systems not only in Algeria but also in developing countries that need financial material and human support to overcome the pandemic crises.
Our study fills the gap in the literature concerning the correlations between KPIs in the healthcare sector during a pandemic crisis. Moreover, the managers can establish realistic goals by using KPIs taking into account their level of importance as early-warning indicators that can point out forthcoming changes in the evolution of the crisis. Healthcare managers can use the clusters KPIs to evaluate executive performance and to develop strategies for saving lives.
In the last years, the KPIs were found as representative of overall healthcare systems around the world [
24]. Paradoxically, the qualitative differences between healthcare systems around the world are reduced by the particularities of the crisis, because a crisis is a negative phenomenon at globally level and its repercussions are more or less evaluated by KPIs [
27]. Moreover, during a pandemic crisis, the information plays an important role in reducing physiological and mental impact on the people [
44] and for this reason, it is necessary to use the KPIs clusters in a flexible way and to adapt them to healthcare facilities [
45].
The results could provide a guide to hospitals’ decision-makers in order to have under control the situation of the Algerian healthcare system [
46] and for the other countries healthcare systems, because our findings are in consensus with the results of the other researchers [
47,
48,
49]
The limitations of our study are related to the sample size, because, considering the short period of analysis, we used a relatively small sample size, from Algerian hospitals and the findings should be critically analysed by considering the specificity of Algeria.
This study only analysed the relationship between four groups of KPIs without testing the direct impact of these KPIs on the performance of the Algerian hospitals.
Our Clusters of KPIs model can be adapted to healthcare systems from different countries, but it is important that every healthcare facility choose its own KPIs taking into account their human, financial and technical resources [
50].
Future research should be oriented to testing the role of KPIs in the improvement of the hospitals’ performance in relationship with the social responsibility and with the improvements of the commitment of the healthcare systems employees.