Palliative Care Professionals’ Inner Lives: Cross-Cultural Application of the Awareness Model of Self-Care
Abstract
1. Introduction
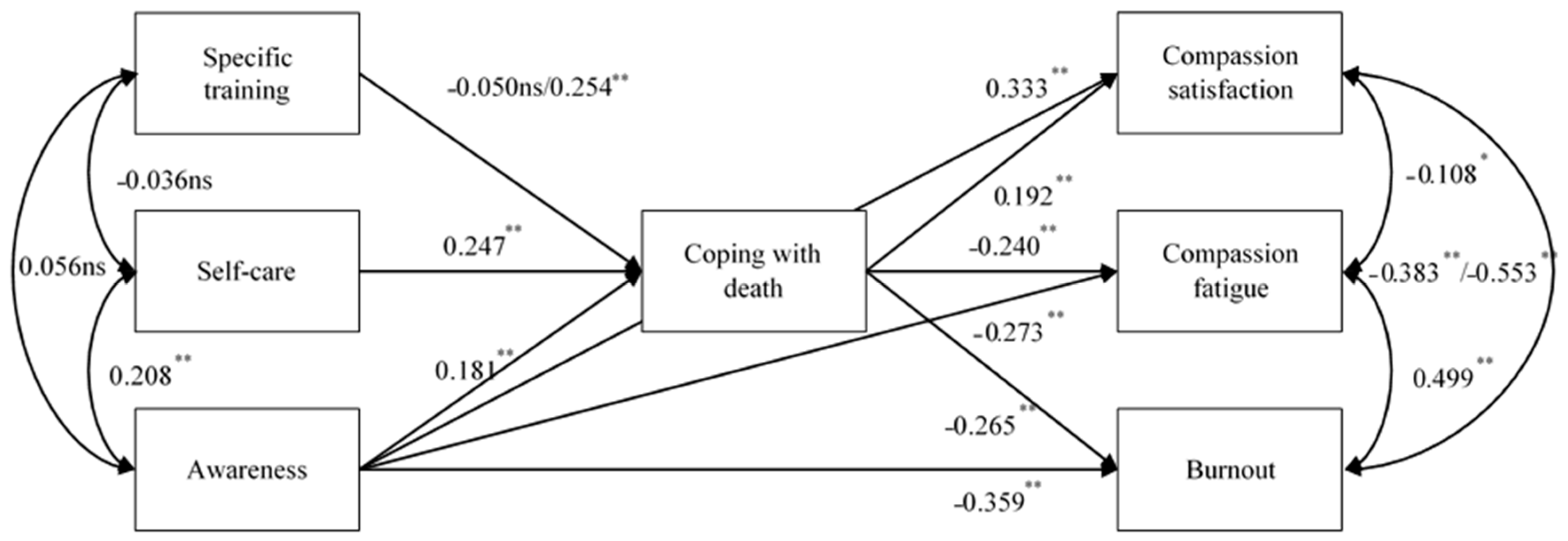
- Competence in coping with death and awareness will be positive predictors of CS and negative predictors of CF and BO.
- Having participated in training programs aimed at facing suffering and death, self-care and awareness will positively predict coping with death, and will indirectly predict professionals’ quality of life (through a mediator effect of coping).
- The three variables (training, self-care, and awareness) will show positive relationships amongst one another.
- The dimensions of the professionals’ quality of life will be interrelated: BO will be negatively related to CS and positively related to CF, whereas CS and CF will be independent.
2. Materials and Methods
2.1. Design, Procedure, and Participants
2.2. Outcomes
- (a)
- Specific training in dealing with death and dying [39], measured with a single open-ended question: “Have you done specific training to face suffering and death?”
- (b)
- The Professional Self-Care Scale (PSCS) [48], which assesses three dimensions of professionals’ self-care: physical, which refers to activities that help to maintain a healthy body; inner, which is related to activities that help to keep a healthy mind; social, pertaining to activities related to social activities that help the individual to maintain social health [48].
- (c)
- (d)
- (e)
- The Professional Quality of Life Scale (ProQOL) [54,55], which comprises three subscales: CS, which refers to the positive consequences of helping others; CF, which refers to the negative consequences of helping others; BO, a form of distress manifested by decreased work performance resulting from negative attitudes and behavior.
2.3. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Compassion—Bridging Practice and Science. Available online: http://www.compassion-training.org/ (accessed on 27 November 2020).
- Hoad, T.F. The Concise Oxford Dictionary of English Etymology; Clarendon Press: Oxford, UK, 1986; Available online: http://search.ebscohost.com/login.aspx?direct=true&AuthType=cookie,ip,shib,uid,url&db=mzh&AN=1986016865&lang=es&site=eds-live (accessed on 27 November 2020).
- Sinclair, S.; McClement, S.; Raffin-Bouchal, S.; Hack, T.F.; Hagen, N.A.; McConnell, S. Compassion in Health Care: An Empirical Model. J. Pain Symptom Manag. 2016, 51, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Larkin, P.J. Compassion: The Essence of Palliative and End-of-Life Care; Oxford University Press: New York, NY, USA, 2016; Available online: http://search.ebscohost.com/login.aspx?direct=true&AuthType=cookie,ip,shib,uid,url&db=psyh&AN=2016-05451-000&lang=es&site=eds-live (accessed on 27 November 2020).
- Vachon, M.L.S. Targeted intervention for family and professional caregivers: Attachment, empathy, and compassion. Palliat Med. 2016, 30, 101–103. [Google Scholar] [CrossRef] [PubMed]
- Najjar, N.; Davis, L.W.; Beck-Coon, K.; Doebbeling, C.C. Compassion Fatigue: A Review of the Research to Date and Relevance to Cancer-care Providers. J. Health Psychol. 2009, 14, 267–277. [Google Scholar] [CrossRef] [PubMed]
- Van Mol, M.M.C.; Kompanje, E.J.O.; Benoit, D.D.; Bakker, J.; Nijkamp, M.D. The Prevalence of Compassion Fatigue and Burnout among Healthcare Professionals in Intensive Care Units: A Systematic Review. PLoS ONE 2015, 10, e0136955. [Google Scholar] [CrossRef] [PubMed]
- Jakimowicz, S.; Perry, L.; Lewis, J. Compassion satisfaction and fatigue: A cross-sectional survey of Australian intensive care nurses. Aust. Crit. Care 2018, 31, 396–405. [Google Scholar] [CrossRef] [PubMed]
- Roney, L.N.; Acri, M.C. The Cost of Caring: An Exploration of Compassion Fatigue, Compassion Satisfaction, and Job Satisfaction in Pediatric Nurses. J. Pediatr Nurs. 2018, 40, 74–80. [Google Scholar] [CrossRef]
- Slocum-Gori, S.; Hemsworth, D.; Chan, W.W.Y.; Carson, A.; Kazanjian, A. Understanding Compassion Satisfaction, Compassion Fatigue and Burnout: A survey of the hospice palliative care workforce. Palliat. Med. 2013, 27, 172–178. [Google Scholar] [CrossRef]
- Kase, S.M.; Waldman, E.D.; Weintraub, A.S. A cross-sectional pilot study of compassion fatigue, burnout, and compassion satisfaction in pediatric palliative care providers in the United States. Palliat. Support. Care 2019, 17, 269–275. [Google Scholar] [CrossRef]
- Mira, J.J.; Carrillo, I.; Lorenzo, S.; Ferrús, L.; Silvestre, C.; Pérez-Pérez, P. The aftermath of adverse events in Spanish primary care and hospital health professionals. BMC Health Serv. Res. 2015, 9, 151. [Google Scholar] [CrossRef]
- Attree, M. Patients’ and relatives’ experiences and perspectives of “Good” and “Not so Good” quality care. J. Adv. Nurs. 2001, 33, 456–466. [Google Scholar] [CrossRef]
- Crossing the quality chasm: A new health system for the 21st century. Tar Heel Nurse 2001, 63, 19–21.
- Epstein, R.M.; Fiscella, K.; Lesser, C.S.; Stange, K.C. Why the nation needs a policy push on patient-centered health care. Health Aff. 2010, 29, 1489–1495. [Google Scholar] [CrossRef] [PubMed]
- Paterson, R. Can we mandate compassion? Hastings Cent. Rep. 2011, 41, 20–23. [Google Scholar] [CrossRef] [PubMed]
- Batt-Rawden, S.A.; Chisolm, M.S.; Anton, B.; Flickinger, T.E. Teaching empathy to medical students: An updated, systematic review. Acad. Med. 2013, 88, 1171–1177. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, S.; Beamer, K.; Hack, T.F.; McClement, S.; Raffin Bouchal, S.; Chochinov, H.M. Sympathy, empathy, and compassion: A grounded theory study of palliative care patients’ understandings, experiences, and preferences. Palliat. Med. 2017, 31, 437–447. [Google Scholar] [CrossRef]
- Kearney, M.K.; Weininger, R.B.; Vachon, M.L.S.; Harrison, R.L.; Mount, B.M. Self-care of Physicians Caring for Patients at the End of Life “Being Connected … A Key to My Survival.”. JAMA J. Am. Med. Assoc. 2009, 301, 1155–1164. [Google Scholar] [CrossRef] [PubMed]
- Samson, T.; Shvartzman, P. Association between level of exposure to death and dying and professional quality of life among palliative care workers. Palliat. Support. Care 2018, 16, 442–451. [Google Scholar] [CrossRef]
- Woolley, H.; Stein, A.; Forrest, G.C.; Baum, J.D. Cornerstone care for families of children with life-threatening illness. Dev. Med. Child. Neurol. 1991, 33, 216–224. [Google Scholar] [CrossRef]
- Hurlbut, J.M.; Robbins, L.K.; Hoke, M.M. Correlations between spirituality and health-promoting behaviors among sheltered homeless women. J. Community Health Nurs. 2011, 28, 81–91. [Google Scholar] [CrossRef]
- Kazemipour, F.; Mohd Amin, S. The impact of workplace spirituality dimensions on organisational citizenship behaviour among nurses with the mediating effect of affective organisational commitment. J. Nurs. Manag. 2012, 20, 1039–1048. [Google Scholar] [CrossRef]
- Kelley, M.M.; Chan, K.T. Assessing the role of attachment to God, meaning, and religious coping as mediators in the grief experience. Death Stud. 2012, 36, 199–227. [Google Scholar] [CrossRef] [PubMed]
- Shinbara, C.G.; Olson, L. When nurses grieve: Spirituality’s role in coping. J. Christ. Nurs. 2010, 27, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Alkema, K.; Linton, J.M.; Davies, R. A study of the relationship between self-care, compassion satisfaction, compassion fatigue, and burnout among hospice professionals. J. Soc. Work End Life Palliat. Care 2008, 4, 101–119. [Google Scholar] [CrossRef] [PubMed]
- Aycock, N.; Boyle, D. Interventions to manage compassion fatigue in oncology nursing. Clin. J. Oncol. Nurs. 2009, 13, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Henry, J.D.; Henry, L.S. The self-caring nurse. Strategies for avoiding compassion fatigue and burnout. Okla Nurse 2004, 49, 9. [Google Scholar]
- Neville, K.; Cole, D.A. The Relationships Among Health Promotion Behaviors, Compassion Fatigue, Burnout, and Compassion Satisfaction in Nurses Practicing in a Community Medical Center. JONA J. Nurs. Adm. 2013, 43, 348–354. [Google Scholar] [CrossRef] [PubMed]
- Hansen, E.M.; Eklund, J.H.; Hallén, A.; Bjurhager, C.S.; Norrström, E.; Viman, A. Does Feeling Empathy Lead to Compassion Fatigue or Compassion Satisfaction? The Role of Time Perspective. J. Psychol. 2018, 152, 630–645. [Google Scholar] [CrossRef]
- Cole, R. Meditation in palliative care--a practical tool for self-management. Palliat. Med. 1997, 11, 411–413. [Google Scholar] [CrossRef]
- Novack, D.H.; Suchman, A.L.; Clark, W.; Epstein, R.M.; Najberg, E.; Kaplan, C. Calibrating the physician. Personal awareness and effective patient care. Working Group on Promoting Physician Personal Awareness, American Academy on Physician and Patient. JAMA 1997, 278, 502–509. [Google Scholar] [CrossRef]
- Epstein, R.M. Mindful practice. JAMA 1999, 282, 833–839. [Google Scholar] [CrossRef]
- Hutchinson, T.A. (Ed.) Whole Person Care: A New Paradigm for the 21st Century; Springer-Verlag: New York, NY, USA, 2011; Available online: https://www.springer.com/gp/book/9781441994394 (accessed on 27 November 2020).
- Thieleman, K.; Cacciatore, J. Witness to suffering: Mindfulness and compassion fatigue among traumatic bereavement volunteers and professionals. Soc. Work 2014, 59, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Thompson, I.A.; Amatea, E.S.; Thompson, E.S. Personal and Contextual Predictors of Mental Health Counselors’ Compassion Fatigue and Burnout. J. Ment. Health Couns. 2014, 36, 58–77. [Google Scholar] [CrossRef]
- Holland, J.M.; Neimeyer, R.A. Reducing the risk of burnout in end-of-life care settings: The role of daily spiritual experiences and training. Palliat. Support. Care 2005, 3, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Kearney, M.K.; Weininger, R.B. Whole person self-care: Self-care from the inside out. In Whole Person Care; Hutchinson, T.A., Ed.; Springer: New York, NY, USA, 2011. [Google Scholar]
- Sansó, N.; Galiana, L.; Oliver, A.; Pascual, A.; Sinclair, S.; Benito, E. Palliative Care Professionals’ Inner Life: Exploring the Relationships Among Awareness, Self-Care, and Compassion Satisfaction and Fatigue, Burnout, and Coping With Death. J. Pain Symptom Manag. 2015, 50, 200–207. [Google Scholar] [CrossRef]
- Lynch, T.; Connor, S.; Clark, D. Mapping levels of palliative care development: A global update. J. Pain Symptom Manag. 2013, 45, 1094–1106. [Google Scholar] [CrossRef]
- Atlas de Cuidados Paliativos en Latinoamérica. Edición Cartográfica 2013. Available online: http://search.ebscohost.com/login.aspx?direct=true&AuthType=cookie,ip,shib,uid,url&db=edsoai&AN=edsoai.on1014026041&lang=es&site=eds-live (accessed on 27 November 2020).
- Wright, M.; Wood, J.; Lynch, T.; Clark, D. Mapping levels of palliative care development: A global view. J. Pain Symptom Manag. 2008, 35, 469–485. [Google Scholar] [CrossRef]
- De Paula Paz, C.R.; Reis Pessalacia, J.D.; Campos Pavone Zoboli, E.L.; Ludugério de Souza, H.; Ferreira Granja, G.; Cabral Schveitzer, M. New demands for primary health care in Brazil: Palliative care. Investig. Educ. Enferm. 2016, 34, 46–57. [Google Scholar]
- Clark, D.; Wright, M. The international observatory on end of life care: A global view of palliative care development. J. Pain Symptom Manag. 2007, 33, 542–546. [Google Scholar] [CrossRef]
- Bollen, K.A. Structural Equations with Latent Variables; John Wiley and Sons, Inc.: New York, NY, USA, 1989; Available online: https://www.scirp.org/(S(vtj3fa45qm1ean45vvffcz55))/reference/ReferencesPapers.aspx?ReferenceID=1927925 (accessed on 27 November 2020).
- Wang, J.; Wang, X. Structural Equation Modeling: Applications Using Mplus, 2nd ed.; Wiley: Hoboken, NJ, USA, 2019; 536p. [Google Scholar]
- Hayduk, L.A. Structural Equations Modeling with Lisrel; Johns Hopkins University Press: Baltimore, MD, USA, 1987. [Google Scholar]
- Galiana, L.; Oliver, A.; Sansó, N.; Benito, E. Validation of a New Instrument for Self-care in Spanish Palliative Care Professionals Nationwide. Span. J. Psychol. 2015, 18, E67. Available online: https://www.cambridge.org/core/journals/spanish-journal-of-psychology/article/validation-of-a-new-instrument-for-selfcare-in-spanish-palliative-care-professionals-nationwide/42D58EE3A97E44EDF7AD9B5E03719D79 (accessed on 19 May 2020). [CrossRef]
- Brown, K.W.; Ryan, R.M. The benefits of being present: Mindfulness and its role in psychological well-being. J. Pers Soc. Psychol. 2003, 84, 822–848. [Google Scholar] [CrossRef]
- Galiana, L.; Oliver, A.; Sansó, N.; Dolores Sancerni, M.; Tomás, J.M. Mindful attention awareness in Spanish palliative care professionals: Psychometric study with IRT and CFA models. Eur. J. Psychol. Assess. 2017, 33, 14–21. [Google Scholar] [CrossRef]
- Galiana, L.; Oliver, A.; Sansó, N.; Benito, E.; Pades, A. Confirmatory validation of the Coping with Death Scale in palliative care professionals. Med. Paliativa 2017, 24, 126–135. [Google Scholar] [CrossRef]
- Forte Camarneiro, A.P.; Rodrigues Gomes, S.M. Translation and Validation of the Coping with Death Scale: A Study with Nurses. Rev. Enferm. Ref. 2015, 4, 113–121. [Google Scholar] [CrossRef]
- Bugen, L.A. Coping: Effects of Death Education; The Final Transition; Taylor and Francis: Abingdon, UK, 2019; pp. 367–375. Available online: http://search.ebscohost.com/login.aspx?direct=true&AuthType=cookie,ip,shib,uid,url&db=edselc&AN=edselc.2-52.0-85079312367&lang=es&site=eds-live (accessed on 27 November 2020).
- Stamm, B.H. The Concise ProQOL Manual. Available online: https://proqol.org/uploads/ProQOLManual.pdf (accessed on 25 November 2020).
- Galiana, L.; Arena, F.; Oliver, A.; Sansó, N.; Benito, E. Compassion Satisfaction, Compassion Fatigue, and Burnout in Spain and Brazil: ProQOL Validation and Cross-cultural Diagnosis. J. Pain Symptom Manag. 2017, 53, 598–604. [Google Scholar] [CrossRef]
- Muthén, L.K.; Muthén, B. Mplus. In The Comprehensive Modelling Program for Applied Researchers: User’s Guide; Muthén & Muthén: Los Angeles, CA, USA, 2016. [Google Scholar]
- Little, T.D. Mean and Covariance Structures (MACS) Analyses of Cross-Cultural Data: Practical and Theoretical Issues. Multivar. Behav Res. 1997, 32, 53–76. [Google Scholar] [CrossRef]
- Hancock, G.R.; Mueller, R.O. Structural Equation Modeling: A Second Course; Information Age Publishing: Charlotte, NC, USA, 2013; p. 702. [Google Scholar]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. PLoS Med. 2007, 4, e297. [Google Scholar] [CrossRef]
- Kenny, D.A.; Kaniskan, B.; McCoach, D.B. The Performance of RMSEA in Models with Small Degrees of Freedom. Sociol. Methods Res. 2015, 44, 486–507. [Google Scholar] [CrossRef]
- Connor, S.R. The global atlas of palliative care at the end of life: An advocacy tool. Eur. J. Palliat. Care 2014, 21, 180–183. [Google Scholar]
- De Simone, G.G. Palliative care in Argentina: Perspectives from a country in crisis. J. Pain Palliat. Care Pharmacother. 2003, 17, 23–43. [Google Scholar] [CrossRef]
- Floriani, C.A.; Schramm, F.R. Moral and operational challenges for the inclusion of palliative care in primary health care. Cad. Saude Publica 2007, 23, 2072–2080. [Google Scholar] [CrossRef]
- Wasner, M.; Paal, P.; Borasio, G.D. Psychosocial care for the caregivers of primary malignant brain tumor patients. J. Soc. Work End Life Palliat. Care 2013, 9, 74–95. [Google Scholar] [CrossRef] [PubMed]
- Burton, A.; Burgess, C.; Dean, S.; Koutsopoulou, G.Z.; Hugh-Jones, S. How Effective are Mindfulness-Based Interventions for Reducing Stress Among Healthcare Professionals? A Systematic Review and Meta-Analysis. Stress Health 2017, 33, 3–13. [Google Scholar] [CrossRef] [PubMed]
- West, C.P.; Dyrbye, L.N.; Erwin, P.J.; Shanafelt, T.D. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet 2016, 388, 2272–2281. [Google Scholar] [CrossRef]
- Carroll, A.; Dowling, M. Discharge planning: Communication, education and patient participation. Br. J. Nurs. 2007, 16, 882–886. [Google Scholar] [CrossRef]

| Variables and Categories | Spain | Argentina | Brazil | |||
|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |
| Age | 46.8 | 8.87 | 43.41 | 9.69 | 37.22 | 11.1 |
| Palliative care experience (years) | 10.69 | 6.59 | 7.95 | 5.85 | 4.97 | 4.42 |
| N | % | N | % | N | % | |
| Sex | ||||||
| Women | 297 | 77.1 | 214 | 79.9 | 141 | 87.6 |
| Men | 85 | 22.1 | 51 | 18.8 | 18 | 11.2 |
| Missing | 3 | 0.8 | 6 | 2.2 | 2 | 1.2 |
| Profession | ||||||
| Doctors | 168 | 43.6 | 136 | 50.2 | 35 | 21.7 |
| Nurses | 128 | 33.2 | 39 | 14.4 | 31 | 19.3 |
| Psychologists | 55 | 14.2 | 43 | 15.9 | 40 | 24.8 |
| Assistant nurses | 15 | 4.1 | 3 | 1.1 | 0 | 0.0 |
| Social workers | 19 | 4.9 | 21 | 7.7 | 19 | 11.8 |
| Other professions | 0 | 0.0 | 22 | 8.1 | 33 | 20.5 |
| Missing | 0 | 0.0 | 7 | 2.6 | 3 | 1.9 |
| Variables and Indicators | Cronbach’s Alphas | Means (SD) | Respondents (Missing Data) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | S | A | B | S | A | B | S | A | B |
| Self-Care | 0.78 | 0.76 | 0.79 | 3.44 (0.84) | 3.26 (0.92) | 3.33 (0.91) | 356 (29) | 258 (13) | 145 (16) |
| Awareness | 0.90 | 0.88 | 0.83 | 4.71 (0.88) | 4.75 (1.02) | 4.60 (0.99) | 352 (33) | 258 (13) | 125 (36) |
| Coping with death Competence | 0.89 | 0.89 | 0.92 | 5.33 (0.80) | 5.22 (0.85) | 5.04 (1.05) | 383 (2) | 252 (19) | 130 (31) |
| Compassion satisfaction | 0.77 | 0.86 | 0.78 | 5.01 (0.51) | 5.05 (0.55) | 5.17 (0.65) | 329 (44) | 239 (32) | 121 (40) |
| Compassion fatigue | 0.78 | 0.77 | 0.75 | 2.57 (0.52) | 2.57 (0.64) | 2.50 (0.64) | 385 (0) | 240 (31) | 121 (40) |
| Burnout | 0.54 | 0.65 | 0.68 | 2.26 (0.58) | 2.29 (0.63) | 2.42 (0.66) | 329 (56) | 240 (31) | 121 (40) |
| Frequency, Yes (%) | Frequency, No (%) | Frequency, Missing Data (%) | |||||||
| Indicators | S | A | B | S | S | S | S | A | B |
| Specific training | 320 (83.1%) | 185 (67.8%) | 67 (41.6%) | 60 (15.6%) | 7 (1.8%) | 7 (1.8%) | 5 (1.3%) | 12 (4.4%) | 31 (19.3%) |
| χ2 | df | p | CFI | RMSEA | RMSEA CI | SRMR | Δχ2 | Δdf | p | ΔCFI | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Model in Spain | 27.888 | 6 | <0.001 | 0.950 | 0.097 | 0.063–0.135 | 0.039 | - | - | - | - |
| Model in Argentina | 40.636 | 6 | <0.001 | 0.914 | 0.147 | 0.106–0.192 | 0.053 | - | - | - | - |
| Model in Brazil | 10.335 | 6 | 0.111 | 0.969 | 0.074 | 0.000–0.149 | 0.051 | - | - | - | - |
| Configural model | 75.312 | 18 | <0.001 | 0.928 | 0.110 | 0.085–0.137 | 0.046 | - | - | - | - |
| Constrained model | 145.229 | 48 | <0.001 | 0.878 | 0.088 | 0.072–0.105 | 0.107 | 72.438 | 30 | <0.001 | 0.050 |
| Most parsimonious model | 104.772 | 45 | <0.001 | 0.925 | 0.071 | 0.054–0.089 | 0.085 | 33.767 | 27 | 0.173 | 0.003 |
| Variables | Spain | Argentina | Brazil |
|---|---|---|---|
| Coping with death | 0.115 | 0.208 | 0.133 |
| Compassion satisfaction | 0.241 | 0.259 | 0.208 |
| Burnout | 0.243 | 0.244 | 0.244 |
| Compassion fatigue | 0.162 | 0.194 | 0.186 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliver, A.; Galiana, L.; Simone, G.d.; Tomás, J.M.; Arena, F.; Linzitto, J.; Grance, G.; Sansó, N. Palliative Care Professionals’ Inner Lives: Cross-Cultural Application of the Awareness Model of Self-Care. Healthcare 2021, 9, 81. https://doi.org/10.3390/healthcare9010081
Oliver A, Galiana L, Simone Gd, Tomás JM, Arena F, Linzitto J, Grance G, Sansó N. Palliative Care Professionals’ Inner Lives: Cross-Cultural Application of the Awareness Model of Self-Care. Healthcare. 2021; 9(1):81. https://doi.org/10.3390/healthcare9010081
Chicago/Turabian StyleOliver, Amparo, Laura Galiana, Gustavo de Simone, José M. Tomás, Fernanda Arena, Juan Linzitto, Gladys Grance, and Noemí Sansó. 2021. "Palliative Care Professionals’ Inner Lives: Cross-Cultural Application of the Awareness Model of Self-Care" Healthcare 9, no. 1: 81. https://doi.org/10.3390/healthcare9010081
APA StyleOliver, A., Galiana, L., Simone, G. d., Tomás, J. M., Arena, F., Linzitto, J., Grance, G., & Sansó, N. (2021). Palliative Care Professionals’ Inner Lives: Cross-Cultural Application of the Awareness Model of Self-Care. Healthcare, 9(1), 81. https://doi.org/10.3390/healthcare9010081






