Trends and Characteristics of Emergency Medical Services in Italy: A 5-Years Population-Based Registry Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting
2.2. The Emergency-Urgency Registry
2.3. Data Selection and Analysis
3. Results
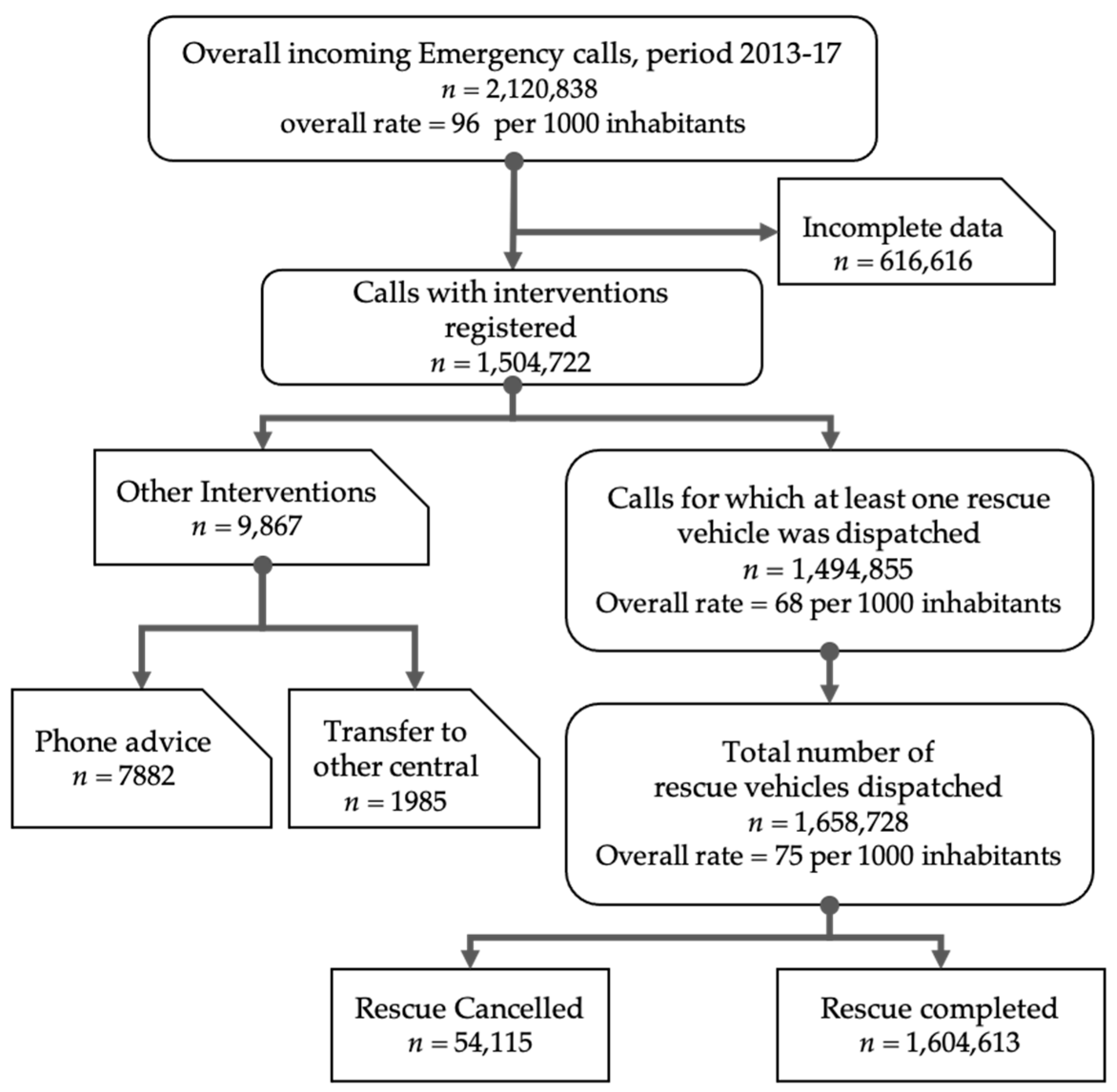
3.1. Trends in EMS Use
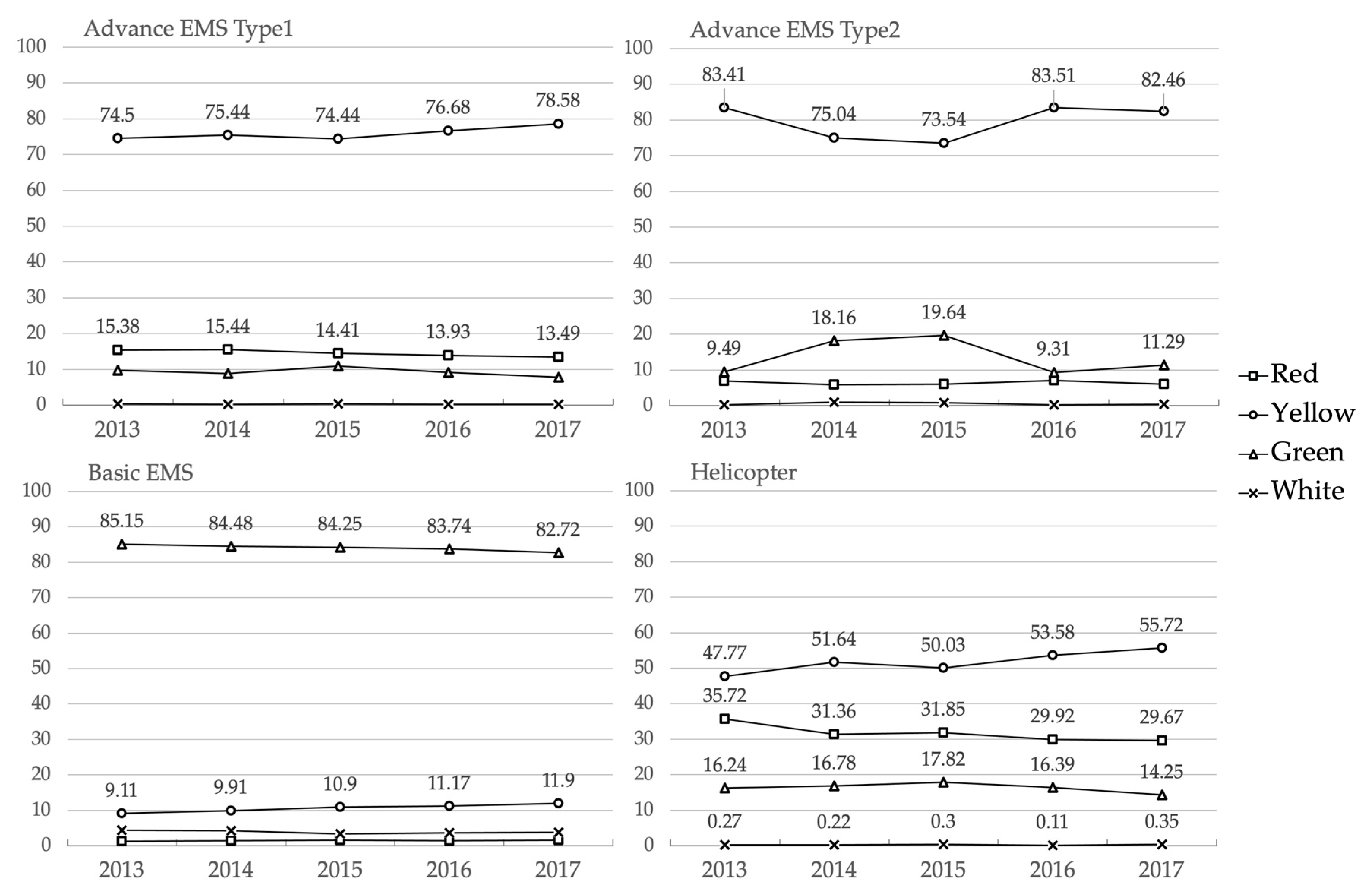
3.2. Trends in Dispatch
4. Discussion
Study Limits
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. Emergency Medical Services System in the European Union: Report of an Assessment Project Co-Ordinated by the World Health Organization; WHO Regional Office for Europe: Copenhagen, Denmark, 2008. [Google Scholar]
- Turner, J.; Coster, J.; Chambers, D.; Phung, V.-H.; Knowles, E.; Bradbury, D.; Goyder, E. What evidence is there on the effectiveness of different models of delivering urgent care? A rapid review. Health Serv. Deliv. Res. 2015, 3, 1–134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ministero della Salute. Sistema di emergenza sanitaria territoriale “118”. In Rilevazione Nazionale, Anno 2005; Ministero della Salute: Rome, Italy, 2007; pp. 1–93. [Google Scholar]
- Danielis, M.; Chittaro, M.; De Monte, A.; Trillò, G.; Durì, D. A five-year retrospective study of out-of-hospital cardiac arrest in a north-east Italian urban area. Eur. J. Cardiovasc. Nurs. 2019, 18, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Sanson, G.; Verduno, J.; Zambon, M.; Trevi, R.; Caggegi, G.D.; Di Bartolomeo, S.; Antonaglia, V. Emergency medical service treated out-of-hospital cardiac arrest: Identification of weak links in the chain-of-survival through an epidemiological study. Eur. J. Cardiovasc. Nurs. 2016, 15, 328–336. [Google Scholar] [CrossRef] [PubMed]
- Bellini, C.; Risso, F.M.; Sannia, A.; Campone, F.; Traggiai, C.; Ramenghi, L.A. A retrospective analysis of the occurrence of accidents during 20 years of neonatal transport in Liguria region, Italy. Eur. J. Emerg. Med. 2017, 24, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Palma, E.; Antonaci, D.; Colì, A.; Cicolini, G. Analysis of Emergency Medical Services Triage and Dispatch Errors by Registered Nurses in Italy. J. Emerg. Nurs. 2014, 40, 476–483. [Google Scholar] [CrossRef] [PubMed]
- Leopardi, M.; Sommacampagna, M. Emergency nursing staff dispatch: Sensitivity and specificity in detecting prehospital need for physician interventions during ambulance transport in Rovigo emergency ambulance service, Italy. Prehosp. Disaster Med. 2013, 28, 523–528. [Google Scholar] [CrossRef]
- Aringhieri, R.; Carello, G.; Morale, D. Supporting decision making to improve the performance of an Italian Emergency Medical Service. Ann. Oper. Res. 2016, 236, 131–148. [Google Scholar] [CrossRef]
- Vidale, S.; Beghi, E.; Gerardi, F.; De Piazza, C.; Proserpio, S.; Arnaboldi, M.; Bezzi, G.; Bono, G.; Grampa, G.; Guidotti, M. Time to hospital admission and start of treatment in patients with ischemic stroke in northern Italy and predictors of delay. Eur. Neurol. 2013, 70, 349–355. [Google Scholar] [CrossRef]
- Muchiutti, M.; Di, S.B.; Valent, F.; Barbone, F.; Palese, A. Assessment of the regional Emergency Medical Service of Friuli-Venezia-Giulia based on the Mattoni SSN Quality Indicators. Epidemiol. Prev. 2011, 35, 324–330. [Google Scholar]
- Ministero della Salute. Regolamento recante definizione degli standard qualitativi, strutturali, tecnologici e quantitativi relativi all’assistenza ospedaliera. In GU Serie Generale; Ministero della Salute: Rome, Italy, 2015. [Google Scholar]
- Maccari, C. La gestione dei servizi di emergenza sanitaria territoriale e le figure professionali coinvolte: Prestazioni e costi Introduzione. Ital. J. Emerg. Med. 2013, 3, 47–58. [Google Scholar]
- Semeraro, F.; Gamberini, L.; Tartaglione, M.; Mora, F.; Dell’Arciprete, O.; Cordenons, F.; Del Giudice, D.; Picoco, C.; Gordini, G. An integrated response to the impact of coronavirus outbreak on the Emergency Medical Services of Emilia Romagna. Resuscitation 2020, 151, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Spina, S.; Marrazzo, F.; Migliari, M.; Stucchi, R.; Sforza, A.; Fumagalli, R. The response of Milan’s Emergency Medical System to the COVID-19 outbreak in Italy. Lancet 2020, 395, e49–e50. [Google Scholar] [CrossRef] [Green Version]
- Diaz-Hierro, J.; Martin, J.J.M.; Arenas, A.V.; Gonzalez, M.P.; Arevalo, J.M.; Gonzalez, C.V. Evaluation of time-series models for forecasting demand for emergency health care services. Emergencias 2012, 24, 181–188. [Google Scholar]
- Peacock, P.J.; Peacock, J.L.; Victor, C.R.; Chazot, C. Changes in the emergency workload of the London Ambulance Service between 1989 and 1999. Emerg. Med. J. 2005, 22, 56–59. [Google Scholar] [CrossRef] [Green Version]
- Pittet, V.; Burnand, B.; Yersin, B.; Carron, P.-N. Trends of pre-hospital emergency medical services activity over 10 years: A population-based registry analysis. BMC Health Serv. Res. 2014, 14, 380. [Google Scholar] [CrossRef] [Green Version]
- Hagihara, A.; Hasegawa, M.; Hinohara, Y.; Abe, T.; Motoi, M. The aging population and future demand for emergency ambulances in Japan. Intern. Emerg. Med. 2013, 8, 431–437. [Google Scholar] [CrossRef]
- Shah, M.N.; Bazarian, J.J.; Lerner, E.B.; Fairbanks, R.J.; Barker, W.H.; Auinger, P.; Friedman, B. The epidemiology of emergency medical services use by older adults: An analysis of the National Hospital Ambulatory Medical Care Survey. Acad. Emerg. Med. 2007, 14, 441–447. [Google Scholar] [CrossRef]
- Andrew, E.; Nehme, Z.; Cameron, P.; Smith, K. Drivers of increasing emergency ambulance demand. Prehosp. Emerg. Care 2020, 24, 385. [Google Scholar] [CrossRef]
- Huang, W.; Wang, T.-B.; He, Y.-D.; Zhang, H.; Zhou, X.-H.; Liu, H.; Zhang, J.-J.; Tian, Z.-B.; Jiang, B.-G. Trends and characteristics in pre-hospital emergency care in Beijing from 2008 to 2017. Chin. Med. J. 2020, 133, 1268–1275. [Google Scholar] [CrossRef]
- Lowthian, J.A.; Jolley, D.J.; Curtis, A.J.; Currell, A.; Cameron, P.A.; Stoelwinder, J.U.; McNeil, J.J. The challenges of population ageing: Accelerating demand for emergency ambulance services by older patients, 1995–2015. Med. J. Aust. 2011, 194, 574–578. [Google Scholar] [CrossRef]
- Kojima, G. Frailty as a predictor of emergency department utilization among community-dwelling older people: A systematic review and meta-analysis. J. Am. Med Dir. Assoc. 2019, 20, 103–105. [Google Scholar] [CrossRef] [PubMed]
- Ukkonen, M.; Jämsen, E.; Zeitlin, R.; Pauniaho, S.-L. Emergency department visits in older patients: A population-based survey. BMC Emerg. Med. 2019, 19, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Grusd, E.; Kramer-Johansen, J. Does the Norwegian emergency medical dispatch classification as non-urgent predict no need for pre-hospital medical treatment? An observational study. Scand. J. Trauma Resusc. Emerg. Med. 2016, 24, 65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Møller, T.P.; Kjærulff, T.M.; Viereck, S.; Østergaard, D.; Folke, F.; Ersbøll, A.K.; Lippert, F.K. The difficult medical emergency call: A register-based study of predictors and outcomes. Scand. J. Trauma Resusc. Emerg. Med. 2017, 25, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mann, N.C.; Kane, L.; Dai, M.; Jacobson, K. Description of the 2012 NEMSIS Public-Release Research Dataset. Prehosp. Emerg. Care 2015, 19, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Patterson, B.W.; Smith, M.A.; Repplinger, M.D.; Pulia, M.S.; Svenson, J.E.; Kim, M.K.; Shah, M.N. Using chief complaint in addition to diagnosis codes to identify falls in the emergency department. J. Am. Geriatr. Soc. 2017, 65, E135–E140. [Google Scholar] [CrossRef]
- Andersen, M.S.; Carlsen, H.P.; Christensen, E.F. Criteria-based emergency medical dispatch of ambulances fulfils goals. Dan. Med. Bull. 2011, 58, A4336. [Google Scholar]
- Booker, M.J.; Shaw, A.R.G.; Purdy, S. Why do patients with ‘primary care sensitive’ problems access ambulance services? A systematic mapping review of the literature. BMJ Open 2015, 5. [Google Scholar] [CrossRef]
- GU Serie Generale. Conversione, con Modificazioni, del Decreto-Legge 6 Luglio 2012, n. 95: Disposizioni Urgenti per la Revisione della Spesa Pubblica con Invarianza dei Servizi ai Cittadini, Nonché Misure di Rafforzamento Patrimoniale delle Imprese del Settore Bancario; G.U.: Rome, Italy, 2012; Volume 156. [Google Scholar]
- Perlini, S.; Canevari, F.; Cortesi, S.; Sgromo, V.; Brancaglione, A.; Contri, E.; Pettenazza, P.; Salinaro, F.; Speciale, F.; Sechi, G. Emergency Department and Out-of-Hospital Emergency System (112—AREU 118) integrated response to Coronavirus Disease 2019 in a Northern Italy centre. Intern. Emerg. Med. 2020, 1–9. [Google Scholar] [CrossRef]
- Presidenza del Consiglio dei Ministri. Disposizioni Urgenti per il Potenziamento del Servizio Sanitario Nazionale in Relazione All’emergenza COVID-19; Presidenza del Consiglio dei Ministri: Rome, Italy, 2020; Volume GU Serie Generale.
- Durand, A.-C.; Gentile, S.; Devictor, B.; Palazzolo, S.; Vignally, P.; Gerbeaux, P.; Sambuc, R. ED patients: How nonurgent are they? Systematic review of the emergency medicine literature. Am. J. Emerg. Med. 2011, 29, 333–345. [Google Scholar] [CrossRef]
- Langabeer, J.R.; Champagne-Langabeer, T.; Alqusairi, D.; Kim, J.; Jackson, A.; Persse, D.; Gonzalez, M. Cost–benefit analysis of telehealth in pre-hospital care. J. Telemed. Telecare 2017, 23, 747–751. [Google Scholar] [CrossRef] [PubMed]
| EMS Calls | 2013 | 2014 | 2015 | 2016 | 2017 | Overall | p |
|---|---|---|---|---|---|---|---|
| Characteristics | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | Value |
| Private citizen | 210,433 (87.4) | 228,106 (87.0) | 283,699 (86.8) | 297,849 (87.2) | 286,627 (88.7) | 1,306,714 (87.4) | <0.001 |
| Nursing home | 8181 (3.4) | 8941 (3.4) | 11,364 (3.5) | 10,401 (3.0) | 10,026 (3.1) | 48,913 (3.3) | |
| Authority | 6973 (2.9) | 8127 (3.1) | 10,539 (3.2) | 12,086 (3.5) | 8459 (2.6) | 46,184 (3.1) | |
| GP/Paediatrician | 6039 (2.5) | 6823 (2.6) | 7991 (2.4) | 7614 (2.2) | 5594 (1.7) | 34,061 (2.3) | |
| EMS Physician | 5978 (2.5) | 7030 (2.7) | 7690 (2.3) | 6651 (1.9) | 4680 (1.4) | 32,029 (2.1) | |
| Private hospital | 516 (0.2) | 504 (0.2) | 581 (0.2) | 484 (0.1) | 515 (0.2) | 2600 (0.2) | |
| Other † | 2758 (1.1) | 2679 (1.0) | 5127 (1.6) | 6536 (1.9) | 7254 (2.2) | 24,354 (1.6) | |
| Call Time | |||||||
| 7a.m.–6:59p.m. | 155,715 (64.6) | 170,219 (64.9) | 213,938 (65.4) | 222,640 (65.2) | 211,154 (65.3) | 973,666 (65.1) | <0.001 |
| 7p.m.–6:59a.m. | 85,163 (35.4) | 91,991 (35.1) | 113,053 (34.6) | 118,981 (34.8) | 112,001 (34.7) | 521,189 (34.9) | |
| Day of the Call | |||||||
| Working days | 172,146 (71.5) | 187,564 (71.5) | 234,607 (71.8) | 245,107 (71.8) | 231,195 (71.5) | 1,070,619 (71.6) | <0.001 |
| Weekend | 68,732 (28.5) | 74,646 (28.5) | 92,384 (28.3) | 96,514 (28.3) | 91,960 (28.5) | 424,236 (28.4) | |
| Call Location | |||||||
| Home | 156,058 (64.8) | 170,211 (64.9) | 208,232 (63.6) | 215,458 (63.1) | 203 105 (62.8) | 953,064 (63.8) | <0.001 |
| Street or highway | 30,505 (12.7) | 33,399 (12.7) | 41,996 (12.8) | 45,540 (13.3) | 42,258 (13.1) | 193,698 (13.0) | |
| Public building | 8421 (3.5) | 9114 (3.5) | 11,933 (3.6) | 12,667 (3.7) | 11,749 (3.6) | 53,884 (3.6) | |
| Industrial place | 4529 (1.9) | 5046 (1.9) | 6 706 (2.0) | 6686 (2.0) | 6197 (1.9) | 29,164 (1.9) | |
| Sport building | 2386 (1.0) | 2578 (1.0) | 3 100 (1.0) | 3048 (0.9) | 2950 (0.9) | 14,062 (0.9) | |
| School | 2109 (0.8) | 2568 (1.0) | 2 807 (1.0) | 3026 (0.9) | 3009 (1.0) | 13,519 (0.9) | |
| Other locations * | 36,870 (15.3) | 39,294 (15.0) | 52,217 (16.0) | 55,196 (16.1) | 53,887 (16.7) | 237,464 (15.9) | |
| Total EMS Calls | 240,878 | 262,210 | 326,991 | 341,621 | 323,155 | 1,494,855 |
| EMS Dispatches | 2013 | 2014 | 2015 | 2016 | 2017 | Overall | p |
|---|---|---|---|---|---|---|---|
| Characteristics | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | Value |
| Number of People Involved | |||||||
| 1 | 223,558 (85.5) | 241,632 (83.8) | 297,661 (81.7) | 306,942 (80.3) | 289,034 (79.8) | 1,358,827 (81.9) | <0.001 |
| 2 | 36,740 (14.0) | 45,018 (15.6) | 61,527 (16.9) | 67479 (17.6) | 65,505 (18.1) | 276,269 (16.7) | |
| >2 | 1221 (0.5) | 1638 (0.6) | 5249 (1.4) | 7961 (2.1) | 7563 (2.1) | 23,632 (1.4) | |
| Health Problem/Injury Reported by the Caller | |||||||
| Traumatic | 52,858 (20.2) | 57,993 (20.1) | 82,319 (22.6) | 87,333 (22.8) | 82,478 (22.8) | 362,981 (21.9) | <0.001 |
| Cardiocirculatory | 40,485 (15.5) | 43,420 (15.1) | 53,185 (15.6) | 55,399 (14.5) | 58,406 (16.1) | 250,895 (15.1) | |
| Neurological | 32,083 (12.3) | 36,121 (12.5) | 43,742 (12.0) | 45,622 (11.9) | 40,798 (11.3) | 198,366 (12.0) | |
| Respiratory | 30,513 (11.7) | 33,372 (11.6) | 41,803 (11.5) | 42,060 (11.0) | 40,836 (11.3) | 188,584 (11.4) | |
| Psychiatric | 8370 (3.2) | 9508 (3.3) | 11214 (3.1) | 12,066 (3.2) | 11,196 (3.1) | 52,354 (3.2) | |
| Toxicological | 4560 (1.7) | 4704 (1.6) | 5415 (1.5) | 5722 (1.5) | 5052 (1.4) | 25,453 (1.5) | |
| Obstetric/gynaecological | 2316 (0.9) | 2316 (0.8) | 2680 (0.7) | 2956 (0.8) | 2982 (0.8) | 13,250 (0.8) | |
| Other health conditions † | 21,767 (8.3) | 23,017 (8.0) | 27,866 (7.7) | 28,750 (7.5) | 25,735 (7.1) | 127,135 (7.7) | |
| Unclear problem | 68,567 (26.2) | 77,837 (27.0) | 96,213 (26.6) | 102,474 (26.8) | 94,619 (26.1) | 439,710 (26.5) | |
| Type of Rescue Vehicle Dispatched § | |||||||
| Basic EMV | 178,346 (68.2) | 195,047 (67.7) | 246.663 (67.7) | 266,550 (69.7) | 247,751 (68.4) | 1,134,357 (68.4) | <0.001 |
| Advanced EMV type 1 | 72,892 (27.9) | 80,614 (27.9) | 101,652 (27.9) | 102,399 (26.8) | 97,305 (26.9) | 454,862 (27.4) | |
| Advanced EMV type 2 | 9197 (3.5) | 11,295 (3.9) | 13,585 (3.7) | 10,729 (2.8) | 14,502 (4.0) | 59,308 (3.6) | |
| Helicopter | 1084 (0.4) | 1332 (0.5) | 2493 (0.7) | 2664 (0.7) | 2512 (0.7) | 10,085 (0.6) | |
| Other | - | - | 44 (0.0) | 40 (0.0) | 32 (0.0) | 116 (0.0) | |
| Emergency Medical Services (EMS) Criticality Codes Assigned | |||||||
| Red | 18,829 (7.2) | 21,121 (7.3) | 26,248 (7.2) | 25,067 (6.6) | 24,154 (6.7) | 115,419 (7) | <0.001 |
| Yellow | 77,710 (29.7) | 88,885 (30.8) | 112,591 (30.9) | 117,337 (30.7) | 116,328 (32.1) | 512,851 (30.9) | |
| Green | 156,474 (59.8) | 169,327 (58.7) | 216,415 (59.4) | 229,311 (60.0) | 211,235 (58.3) | 982,762 (59.3) | |
| White | 8506 (3.3) | 8955 (3.1) | 9183 (2.5) | 10667 (2.8) | 10,385 (2.9) | 47,696 (2.9) | |
| Number of Rescue Vehicles Dispatched | |||||||
| 1 | 220,856 (84.4) | 237,064 (82.2) | 291.645 (80.0) | 303,179 (79.3) | 286,392 (79.1) | 1,339,136 (80.7) | <0.001 |
| 2 | 38,900 (14.8) | 48,602 (16.9) | 67,158 (18.4) | 72,960 (19.1) | 69,760 (19.3) | 297,380 (17.9) | |
| ≥3 | 1763 (0.8) | 2622 (0.9) | 5634 (1.6) | 6243 (1.6) | 5950 (1.6) | 22,212 (1.4) | |
| Number of patients transported per rescue vehicle | |||||||
| None | 61,300 (23.4) | 68,404 (23.7) | 92.465 (25.4) | 99,269 (26.0) | 96,873 (26.7) | 418,311 (25.2) | <0.001 |
| One person | 197,440 (75.5) | 216,918 (75.2) | 267,869 (73.5) | 279,054 (73.0) | 261,477 (72.2) | 1,222,868 (73.7) | |
| More than one person | 2669 (1.0) | 2966 (1.0) | 4103 (1.1) | 4059 (1.0) | 3752 (1.0) | 17,549 (1.1) | |
| Site of Rescue Completion | |||||||
| Hospital ED | 200,219 (76.6) | 219,884 (76.3) | 271,972 (74.6) | 282,749 (73.9) | 264,936 (73.2) | 1,239,760 (74.7) | <0.001 |
| Rendez vous | 200 (0.1) | 232 (0.1) | 195 (0.1) | 364 (0.1) | 293 (0.1) | 1284 (0.1) | |
| At home | 99 (0.0) | 22 (0.0) | 22 (0.0) | 35 (0.1) | 33 (0.0) | 211 (0.0) | |
| Morgue | 12 (0.0) | 13 (0.0) | 26 (0.0) | 19 (0.0) | 17 (0.0) | 87 (0.0) | |
| Other * | 55,456 (21.2) | 59,834 (20.7) | 79,141 (21.7) | 85,277 (22.3) | 83,563 (23.0) | 363,271 (21.9) | |
| Rescue cancelled | 5533 (2.1) | 8303 (2.9) | 13,081 (3.6) | 13,938 (3.6) | 13,260 (3.7) | 54,115 (3.3) | |
| Total Vehicle Dispatched | 261,519 | 288,288 | 365,437 | 382,382 | 362,102 | 1,658,728 | |
| Criticality | Rescue Vehicle | OR | [95%CI] | OR |
|---|---|---|---|---|
| Red | EMV type1 | 1.00 |  | |
| EMV type2 | 1.47 | [1.4–1.6] | ||
| Basic EMV | 2.04 | [2.0–2.1] | ||
| Helicopter | 2.48 | [2.3–2.7] | ||
| Yellow | EMV type1 | 1.00 | ||
| EMV type2 | 2.07 | [2.0–2.1] | ||
| Basic EMV | 6.93 | [6.8–7.1] | ||
| Helicopter | 7.22 | [6.7–7.8] | ||
| Green | EMV type1 | 1.00 | ||
| EMV type2 | 1.62 | [1.5–1.7] | ||
| Basic EMV | 3.21 | [3.1–3.3] | ||
| Helicopter | 3.64 | [3.2–4.1] | ||
| White | EMV type1 | 1.00 | ||
| EMV type2 | 2.92 | [2.3–3.7] | ||
| Basic EMV | 8.91 | [8.0–9.9] | ||
| Helicopter | 0.12 | [0.1–0.2] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Campagna, S.; Conti, A.; Dimonte, V.; Dalmasso, M.; Starnini, M.; Gianino, M.M.; Borraccino, A. Trends and Characteristics of Emergency Medical Services in Italy: A 5-Years Population-Based Registry Analysis. Healthcare 2020, 8, 551. https://doi.org/10.3390/healthcare8040551
Campagna S, Conti A, Dimonte V, Dalmasso M, Starnini M, Gianino MM, Borraccino A. Trends and Characteristics of Emergency Medical Services in Italy: A 5-Years Population-Based Registry Analysis. Healthcare. 2020; 8(4):551. https://doi.org/10.3390/healthcare8040551
Chicago/Turabian StyleCampagna, Sara, Alessio Conti, Valerio Dimonte, Marco Dalmasso, Michele Starnini, Maria Michela Gianino, and Alberto Borraccino. 2020. "Trends and Characteristics of Emergency Medical Services in Italy: A 5-Years Population-Based Registry Analysis" Healthcare 8, no. 4: 551. https://doi.org/10.3390/healthcare8040551
APA StyleCampagna, S., Conti, A., Dimonte, V., Dalmasso, M., Starnini, M., Gianino, M. M., & Borraccino, A. (2020). Trends and Characteristics of Emergency Medical Services in Italy: A 5-Years Population-Based Registry Analysis. Healthcare, 8(4), 551. https://doi.org/10.3390/healthcare8040551







