Evaluation of a Prehospital Rotation by Senior Residents: A Web-Based Survey
Abstract
1. Introduction
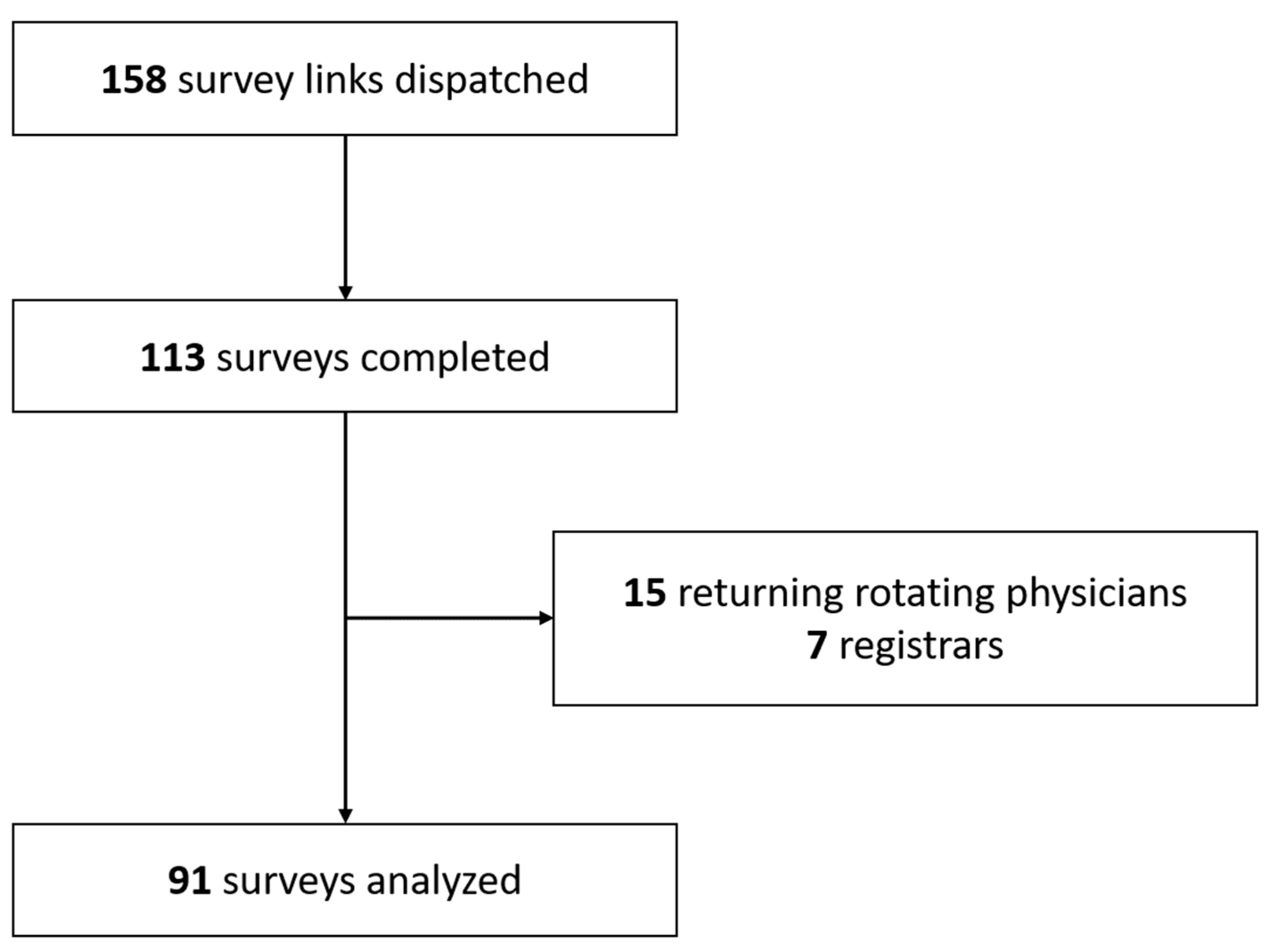
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Data
- From 2011 to 2018, a system based on a Joomla 1.6 (progressively updated to version 2.5) platform (Open Source Matters, New York, NY, USA) was used. The questionnaire was administered using the Survey Force Deluxe 3 component (Joomplace, Minsk, Belarus). Unique links were generated by this component, before being manually embedded in e-mails along with a standard accompanying message.
- Starting 2019, a Joomla 3 platform was used, and e-mails were automatically generated by the AcyMailing 5 component (Acyba, Lyon, France). The unique links redirected to a questionnaire created under CommunitySurvey Pro 5 (CoreJoomla, Hyberabad, India).
2.3. Inclusion and Exclusion Criteria
2.4. Outcomes
2.5. Data Curation, Data Availability and Statistical Analysis
3. Results
4. Discussion
4.1. Main considerations
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lockey, D. International EMS systems: Geographical lottery and diversity but many common challenges. Resuscitation 2009, 80, 722. [Google Scholar] [CrossRef]
- Yeguiayan, J.M.; Garrigue, D.; Binquet, C.; Jacquot, C.; Duranteau, J.; Martin, C.; Rayeh, F.; Riou, B.; Bonithon-Kopp, C.; Freysz, M. Medical pre-hospital management reduces mortality in severe blunt trauma: A prospective epidemiological study. Crit. Care 2011, 15, R34. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, T.; Ohashi-Fukuda, N.; Kondo, Y.; Hayashida, K.; Kukita, I. Association of prehospital advanced life support by physician with survival after out-of-hospital cardiac arrest with blunt trauma following traffic collisions Japanese registry-based study. JAMA Surg. 2018, 153. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, A.; Steinmetz, J.; Wissenberg, M.; Torp-Pedersen, C.; Lippert, F.K.; Hove, L.; Lohse, N. Association between prehospital physician involvement and survival after out-of-hospital cardiac arrest: A Danish nationwide observational study. Resuscitation 2016, 108, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Goto, Y.; Funada, A.; Goto, Y. Impact of prehospital physician-led cardiopulmonary resuscitation on neurologically intact survival after out-of-hospital cardiac arrest: A nationwide population-based observational study. Resuscitation 2019, 136, 38–46. [Google Scholar] [CrossRef]
- Hirano, Y.; Abe, T.; Tanaka, H. Efficacy of the presence of an emergency physician in prehospital major trauma care: A nationwide cohort study in Japan. Am. J. Emerg. Med. 2019, 37, 1605–1610. [Google Scholar] [CrossRef] [PubMed]
- Popal, Z.; Bossers, S.M.; Terra, M.; Schober, P.; de Leeuw, M.A.; Bloemers, F.W.; Giannakopoulos, G.F. Effect of Physician-Staffed Emergency Medical Services (P-EMS) on the Outcome of Patients with Severe Traumatic Brain Injury: A Review of the Literature. Prehosp. Emerg. Care 2019, 23, 730–739. [Google Scholar] [CrossRef]
- Custalow, C.B.; Armacost, M.; Honigman, B. Unique Curriculum for Emergency Medicine Residents as Medical Directors for Rural Out-of-hospital Agencies. Acad. Emerg. Med. 2000, 7, 674–678. [Google Scholar] [CrossRef]
- Crewdson, K.; Lockey, D.J.; Røislien, J.; Lossius, H.M.; Rehn, M. The success of pre-hospital tracheal intubation by different pre-hospital providers: A systematic literature review and meta-analysis. Crit. Care 2017, 21, 31. [Google Scholar] [CrossRef]
- Ramadanov, N.; Klein, R.; Aguilar Valdez, A.D.; Behringer, W. Medication Appropriateness in Prehospital Care. Emerg. Med. Int. 2019, 2019, 1–5. [Google Scholar] [CrossRef]
- Bossers, S.M.; Schwarte, L.A.; Loer, S.A.; Twisk, J.W.R.; Boer, C.; Schober, P. Experience in prehospital endotracheal intubation significantly influences mortality of patients with severe traumatic brain injury: A systematic review and meta-analysis. PLoS ONE 2015, 10, e0141034. [Google Scholar] [CrossRef] [PubMed]
- Luftman, K.; Aydelotte, J.; Rix, K.; Ali, S.; Houck, K.; Coopwood, T.B.; Teixeira, P.; Eastman, A.; Eastridge, B.; Brown, C.V.R.; et al. PTSD in those who care for the injured. Injury 2017, 48, 293–296. [Google Scholar] [CrossRef] [PubMed]
- Sand, M.; Hessam, S.; Bechara, F.G.; Sand, D.; Vorstius, C.; Bromba, M.; Stockfleth, E.; Shiue, I. A pilot study of quality of life in German prehospital emergency care physicians. J. Res. Med. Sci. 2016, 21, 133. [Google Scholar] [CrossRef] [PubMed]
- Murray, E.; Krahé, C.; Goodsman, D. Are medical students in prehospital care at risk of moral injury? Emerg. Med. J. 2018, 35, 590–594. [Google Scholar] [CrossRef] [PubMed]
- Martin-Gill, C.; Roth, R.N.; Mosesso, V.N. Resident field response in an emergency medicine prehospital care rotation. Prehosp. Emerg. Care 2010, 14, 370–376. [Google Scholar] [CrossRef] [PubMed]
- Houry, D.E.; Pons, P.T. The value of the out-of-hospital experience for emergency medicine residents. Ann. Emerg. Med. 2000, 36, 391–393. [Google Scholar] [CrossRef]
- Crowe, R.P.; Wagoner, R.L.; Rodriguez, S.A.; Bentley, M.A.; Page, D. Defining Components of Team Leadership and Membership in Prehospital Emergency Medical Services. Prehosp. Emerg. Care 2017, 21, 645–651. [Google Scholar] [CrossRef]
- Mantha, A.; Coggins, N.L.; Mahadevan, A.; Strehlow, R.N.; Strehlow, M.C.; Mahadevan, S.V. Adaptive leadership curriculum for Indian paramedic trainees. Int. J. Emerg. Med. 2016, 9, 1–7. [Google Scholar] [CrossRef]
- Chan, M.; Fehlmann, C.A.; Pasquier, M.; Suppan, L.; Savoldelli, G. Endotracheal Intubation Success Rate in an Urban, Supervised, Resident-Staffed Emergency Mobile System: An 11-Year Retrospective Cohort Study. J. Clin. Med. 2020, 9, 238. [Google Scholar] [CrossRef]
- Sanchez, B.; Hirzel, A.H.; Bingisser, R.; Ciurea, A.; Exadaktylos, A.; Lehmann, B.; Matter, H.; Meier, K.; Osterwalder, J.; Sieber, R.; et al. State of Emergency Medicine in Switzerland: A national profile of emergency departments in 2006. Int. J. Emerg. Med. 2013, 6, 23. [Google Scholar] [CrossRef]
- Gartner, B.A.; Fehlmann, C.; Suppan, L.; Niquille, M.; Rutschmann, O.T.; Sarasin, F. Effect of noninvasive ventilation on intubation risk in prehospital patients with acute cardiogenic pulmonary edema. Eur. J. Emerg. Med. 2019, 27, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Niquille, M.; Suppan, L.; Larribau, R. Performance de l’indication à l’envoi d’un SMUR en premier échelon au sein d’un centre de communication médicale d’urgence paramédicalisé. Available online: https://www.urgencesdirectinfo.com/medias/voir/performance-de-l-indication-a-l-envoi-d-un-smur-en-premier-echelon-au-sein-d-un-centre-de-communication-medicale-d-urgence-paramedicalise/4646 (accessed on 28 December 2020).
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef] [PubMed]
- Swiss Confederation CC 810.30 Federal Act of 30 September 2011 on Research Involving Human Beings (Human Research Act, HRA). Available online: https://www.admin.ch/opc/en/classified-compilation/20061313/index.html (accessed on 12 May 2020).
- Formation Postgraduée: Évaluation par les Médecins-Assistants 2010. Available online: https://siwf.ch/siwf-umfrage-weiterbildungsqualitaet/2010/?act=0&l=2&c=3155&jsessionid=fmh_d98add5a-36bf-43cf-a797-0348dafbda0a_0 (accessed on 28 December 2020).
- Prehospital Rotation Utility Dataset 2020. Available online: https://commons.datacite.org/doi.org/10.17632/hsrrjp88pc.1 (accessed on 28 December 2020).
- Shah, A.; Carter, T.; Kuwani, T.; Sharpe, R. Simulation to develop tomorrow’s medical registrar. Clin. Teach. 2013, 10, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Barchiesi, M.; Leidi, F. The impact of different models of resident supervision on patient safety and resident education. Intern. Emerg. Med. 2019, 14, 793–795. [Google Scholar] [CrossRef] [PubMed]
- Sheng, A.Y.; Clark, A.; Amanti, C. Supervision of Resident Physicians. Emerg. Med. Clin. N. Am. 2020, 38, 339–351. [Google Scholar] [CrossRef] [PubMed]
- Ford, K.; Menchine, M.; Burner, E.; Arora, S.; Inaba, K.; Demetriades, D.; Yersin, B. Leadership and Teamwork in Trauma and Resuscitation. West. J. Emerg. Med. 2016, 17, 549–556. [Google Scholar] [CrossRef]
- Hunziker, S.; Johansson, A.C.; Tschan, F.; Semmer, N.K.; Rock, L.; Howell, M.D.; Marsch, S. Teamwork and Leadership in Cardiopulmonary Resuscitation. J. Am. Coll. Cardiol. 2011, 57, 2381–2388. [Google Scholar] [CrossRef]
- Schewe, J.-C.; Kappler, J.; Dovermann, K.; Graeff, I.; Ehrentraut, S.F.; Heister, U.; Hoeft, A.; Weber, S.U.; Muenster, S. Diagnostic accuracy of physician-staffed emergency medical teams: A retrospective observational cohort study of prehospital versus hospital diagnosis in a 10-year interval. Scand. J. Trauma. Resusc. Emerg. Med. 2019, 27, 36. [Google Scholar] [CrossRef] [PubMed]
- Evans, K.; Geduld, H.; Stassen, W. Attitudes of prehospital providers on transport decision-making in the management of patients with a suicide attempt refusing care: A survey based on the Mental Health Care Act of 2002. S. Afr. J. Psychiatr. 2018, 24, 1156. [Google Scholar] [CrossRef]
- Mix, F.; Myers, L.A.; Luke, A.; Sztajnkrycer, M.D. Pediatric Prehospital Refusal of Medical Assistance: Association with Suspected Abuse or Neglect. Prehosp. Emerg. Care 2017, 21, 688–692. [Google Scholar] [CrossRef]
- ERBAY, H. Some Ethical Issues in Prehospital Emergency Medicine. Turkish J. Emerg. Med. 2014, 14, 193–198. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, G.S.; Rahmani, R.; Fitzgerald, P.C.; Chang, R.; McCarthy, R.J. The Association Between Frequency of Self-Reported Medical Errors and Anesthesia Trainee Supervision. Anesth. Analg. 2013, 116, 892–897. [Google Scholar] [CrossRef] [PubMed]
- Sauter, T.C.; Hautz, W.E.; Hostettler, S.; Brodmann-Maeder, M.; Martinolli, L.; Lehmann, B.; Exadaktylos, A.K.; Haider, D.G. Interprofessional and interdisciplinary simulation-based training leads to safe sedation procedures in the emergency department. Scand. J. Trauma. Resusc. Emerg. Med. 2016, 24, 97. [Google Scholar] [CrossRef] [PubMed]
- Risgaard, B.; Draegert, C.; Baekgaard, J.S.; Steinmetz, J.; Rasmussen, L.S. Impact of Physician-staffed Helicopters on Pre-hospital Patient Outcomes: A systematic review. Acta Anaesthesiol. Scand. 2020, 64, 691–704. [Google Scholar] [CrossRef] [PubMed]
- Raatiniemi, L.; Liisanantti, J.; Tommila, M.; Moilanen, S.; Ohtonen, P.; Martikainen, M.; Voipio, V.; Reitala, J.; Iirola, T. Evaluating helicopter emergency medical missions: A reliability study of the HEMS benefit and NACA scores. Acta Anaesthesiol. Scand. 2017, 61, 557–565. [Google Scholar] [CrossRef]
- Crewdson, K.; Rehn, M.; Lockey, D. Airway management in pre-hospital critical care: A review of the evidence for a ‘top five’ research priority. Scand. J. Trauma. Resusc. Emerg. Med. 2018, 26, 89. [Google Scholar] [CrossRef]
- Peters, J.H.; Smulders, P.S.H.; Moors, X.R.J.; Bouman, S.J.M.; Meijs, C.M.E.M.; Hoogerwerf, N.; Edwards, M.J.R. Are on-scene blood transfusions by a helicopter emergency medical service useful and safe? A multicentre case–control study. Eur. J. Emerg. Med. 2019, 26, 128–132. [Google Scholar] [CrossRef]
- Den Hartog, D.; Romeo, J.; Ringburg, A.N.; Verhofstad, M.H.J.; Van Lieshout, E.M.M. Survival benefit of physician-staffed Helicopter Emergency Medical Services (HEMS) assistance for severely injured patients. Injury 2015, 46, 1281–1286. [Google Scholar] [CrossRef]
- Hart, P.L.; Spiva, L.; Baio, P.; Huff, B.; Whitfield, D.; Law, T.; Wells, T.; Mendoza, I.G. Medical-surgical nurses’ perceived self-confidence and leadership abilities as first responders in acute patient deterioration events. J. Clin. Nurs. 2014, 23, 2769–2778. [Google Scholar] [CrossRef][Green Version]
- Koka, A.; Suppan, L.; Cottet, P.; Carrera, E.; Stuby, L.; Suppan, M. Teaching NIHSS to Paramedics, E-learning vs Video: A Randomized Controlled Trial (Preprint). J. Med. Internet Res. 2020, 22, 6. [Google Scholar] [CrossRef]
- Suppan, M.; Gartner, B.; Golay, E.; Stuby, L.; White, M.; Cottet, P.; Abbas, M.; Iten, A.; Harbarth, S.; Suppan, L. Teaching Adequate Prehospital Use of Personal Protective Equipment During the COVID-19 Pandemic: Development of a Gamified e-Learning Module. JMIR Serious Games 2020, 8, e20173. [Google Scholar] [CrossRef] [PubMed]
- Yule, S.; Flin, R.; Maran, N.; Rowley, D.; Youngson, G.; Paterson-Brown, S. Surgeons’ Non-technical Skills in the Operating Room: Reliability Testing of the NOTSS Behavior Rating System. World J. Surg. 2008, 32, 548–556. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Anesthesiology Residents (N = 30) | Emergency Medicine Residents (N = 16) | Internal Medicine Residents (N = 45) | |
|---|---|---|---|---|
| Years since graduation (median, Q1;Q3) | 4 (4;6) | 4 (3;5) | 4 (4;5) | |
| Target specialty 1 | ||||
| Anesthesiology (n, %) | 30 (100%) | 3 (19%) | 2 (4%) | |
| Internal Medicine (n, %) | 1 (3%) | 11 (69%) | 44 (98%) | |
| Other (n, %) | 2 (7%) | 5 (31%) | 7 (16%) | |
| Target emergency certification | ||||
| Prehospital (n, %) | 22 (73%) | 7 (44%) | 12 (27%) | |
| In-hospital (n, %) | 3 (10%) | 7 (44%) | 11 (24%) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suppan, L.; Chan, M.; Gartner, B.; Regard, S.; Campana, M.; Chatellard, G.; Cottet, P.; Larribau, R.; Sarasin, F.P.; Niquille, M. Evaluation of a Prehospital Rotation by Senior Residents: A Web-Based Survey. Healthcare 2021, 9, 24. https://doi.org/10.3390/healthcare9010024
Suppan L, Chan M, Gartner B, Regard S, Campana M, Chatellard G, Cottet P, Larribau R, Sarasin FP, Niquille M. Evaluation of a Prehospital Rotation by Senior Residents: A Web-Based Survey. Healthcare. 2021; 9(1):24. https://doi.org/10.3390/healthcare9010024
Chicago/Turabian StyleSuppan, Laurent, Michèle Chan, Birgit Gartner, Simon Regard, Mathieu Campana, Ghislaine Chatellard, Philippe Cottet, Robert Larribau, François Pierre Sarasin, and Marc Niquille. 2021. "Evaluation of a Prehospital Rotation by Senior Residents: A Web-Based Survey" Healthcare 9, no. 1: 24. https://doi.org/10.3390/healthcare9010024
APA StyleSuppan, L., Chan, M., Gartner, B., Regard, S., Campana, M., Chatellard, G., Cottet, P., Larribau, R., Sarasin, F. P., & Niquille, M. (2021). Evaluation of a Prehospital Rotation by Senior Residents: A Web-Based Survey. Healthcare, 9(1), 24. https://doi.org/10.3390/healthcare9010024






