The Impact of Teammates’ Online Reputations on Physicians’ Online Appointment Numbers: A Social Interdependency Perspective
Abstract
:1. Introduction
2. Materials and Methods
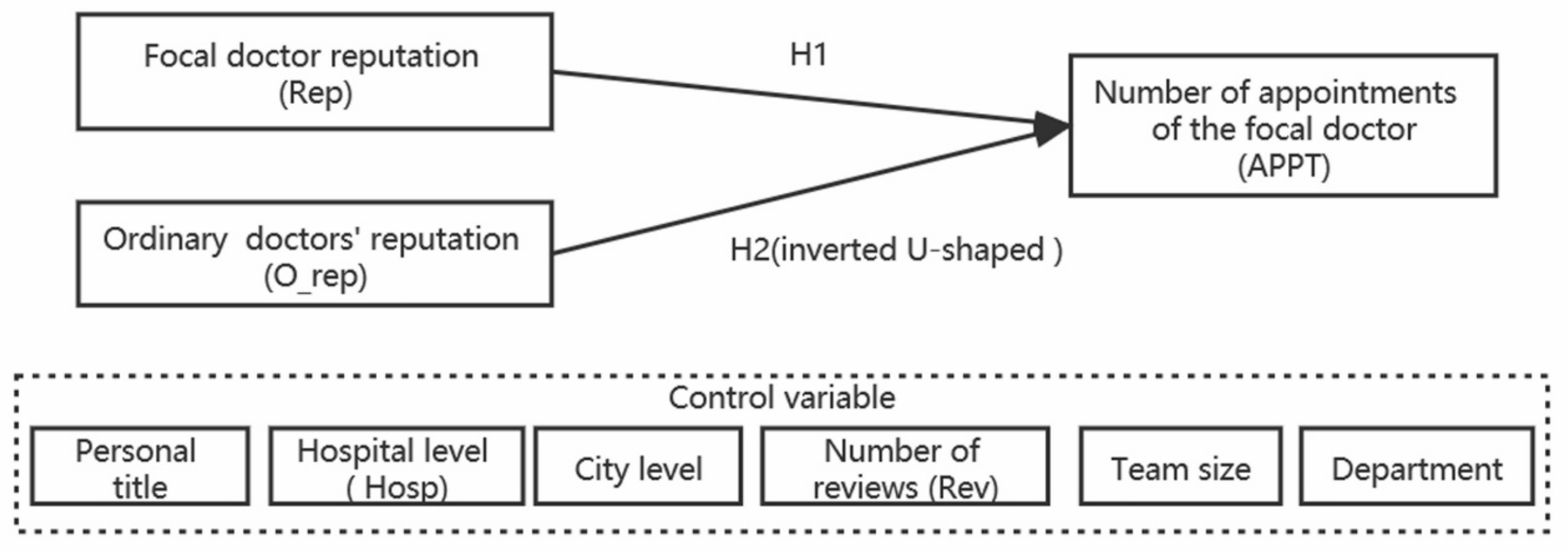
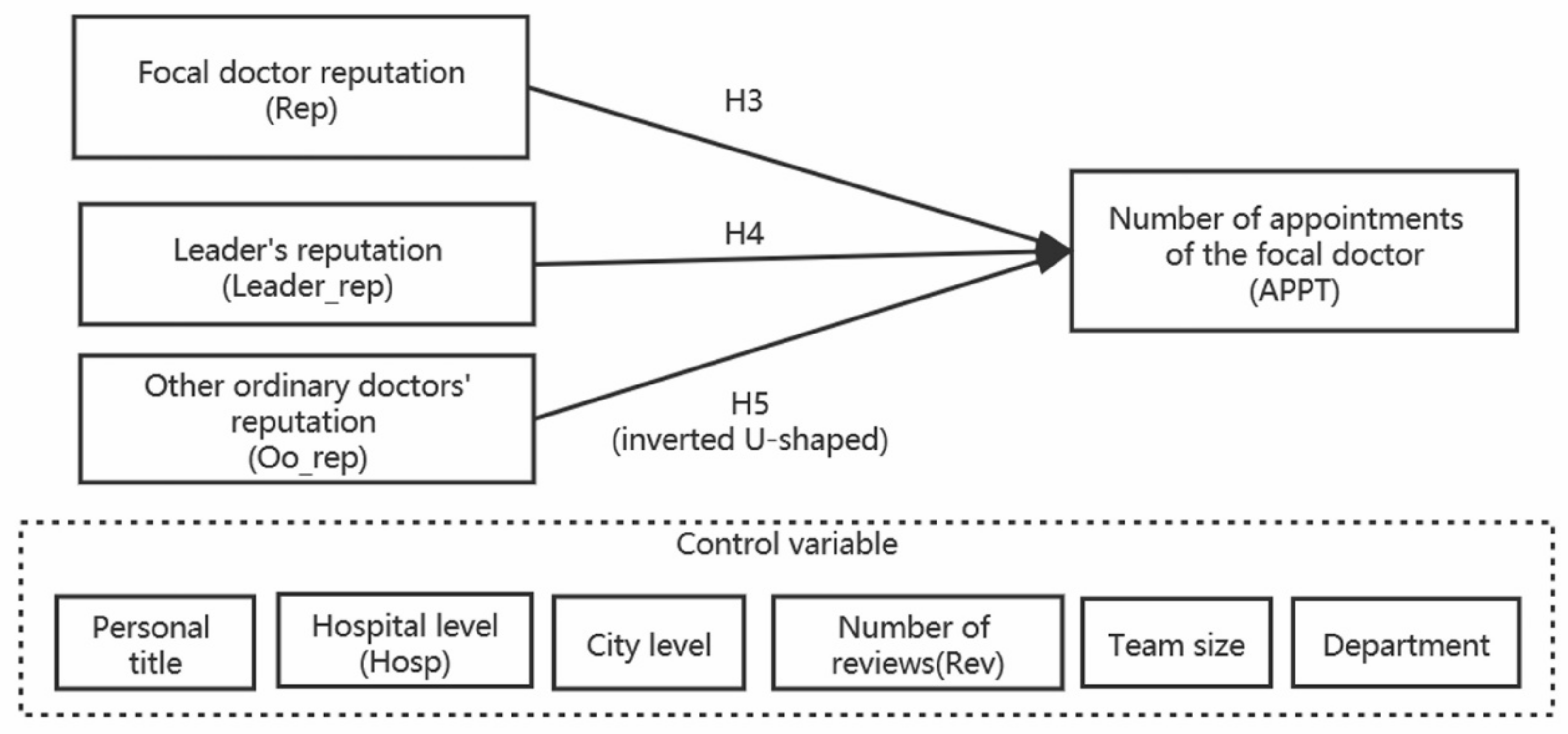
2.1. Research Model and Hypotheses Development
2.1.1. Hypotheses of Leaders
2.1.2. Hypotheses of Ordinary Doctors
2.2. Research Methodology
2.2.1. Variables’ Design
2.2.2. Empirical Model and Test Method
3. Results
3.1. Results for Leaders
3.1.1. Descriptive Statistic and Correlation for Leaders
3.1.2. Regression Results of Leader’s Research Model
3.2. Results for Ordinary Doctors
3.2.1. Descriptive Statistic and Correlation for Ordinary Doctors
3.2.2. Regression Results of Ordinary Doctors’ Research Model
4. Discussion
5. Conclusions
5.1. Key Findings
5.2. Implications for Research
5.3. Practical Significance
6. Limitations and Future Work
Author Contributions
Funding
Conflicts of Interest
References
- Salas, E.; Zajac, S.; Marlow, S.L. Transforming Health Care One Team at a Time: Ten Observations and the Trail Ahead. Group Organ. Manag. 2018, 43, 357–381. [Google Scholar] [CrossRef]
- Moyal, A. Team practice in multi-professional healthcare homes: A division of labour under medical control. Rev. Fr. Aff. Soc. 2020, 1, 103–123. [Google Scholar] [CrossRef]
- Schmutz, J.B.; Meier, L.L.; Manser, T. How effective is teamwork really? The relationship between teamwork and performance in healthcare teams: A systematic review and meta-analysis. BMJ Open 2019, 9, e028280. [Google Scholar] [CrossRef] [Green Version]
- Lacagnina, S.; Moore, M.; Mitchell, S. The Lifestyle Medicine Team: Health Care That Delivers Value. Am. J. Lifestyle Med. 2018, 12, 479–483. [Google Scholar] [CrossRef]
- Berry, L.L.; Beckham, D. Team-Based Care at Mayo Clinic: A Model for ACOs. J. Health Manag. 2014, 59, 9–13. [Google Scholar] [CrossRef]
- El-Awaisi, A.; O’Carroll, V.; Koraysh, S.; Koummich, S.; Huber, M. Perceptions of who is in the healthcare team? A content analysis of social media posts during COVID-19 pandemic. J. Interprof. Care 2020, 34, 622–632. [Google Scholar] [CrossRef] [PubMed]
- Rosen, M.A.; DiazGranados, D.; Dietz, A.S.; Benishek, L.E.; Thompson, D.; Pronovost, P.J.; Weaver, S.J. Teamwork in healthcare: Key discoveries enabling safer, high-quality care. Am. Psychol. 2018, 73, 433–450. [Google Scholar] [CrossRef]
- Johnson, A.; Nguyen, H.; Groth, M.; White, L. Reaping the Rewards of Functional Diversity in Healthcare Teams: Why Team Processes Improve Performance. Group Organ. Manag. 2018, 43, 440–474. [Google Scholar] [CrossRef] [Green Version]
- Maynard, M.T.; Mathieu, J.E.; Rapp, T.L.; Gilson, L.L.; Kleiner, C. Team leader coaching intervention: An investigation of the impact on team processes and performance within a surgical context. J. Appl. Psychol. 2020. [Google Scholar] [CrossRef]
- Samuriwo, R.; Laws, E.; Webb, K.; Bullock, A.D. “I didn’t realise they had such a key role.” Impact of medical education curriculum change on medical student interactions with nurses: A qualitative exploratory study of student perceptions. Adv. Health Sci. Educ. 2019, 25, 75–93. [Google Scholar] [CrossRef] [Green Version]
- Li, H.; Fang, Y.; Lim, K.H.; Wang, Y. Platform-Based Function Repertoire, Reputation, and Sales Performance of E-Marketplace Sellers. MIS Q. 2019, 43, 207–236. [Google Scholar] [CrossRef] [Green Version]
- Anagnostopoulou, S.C.; Buhalis, D.; Kountouri, I.L.; Manousakis, E.G.; Tsekrekos, A.E. The impact of online reputation on hotel profitability. Int. J. Contemp. Hosp. Manag. 2020, 32, 20–39. [Google Scholar] [CrossRef] [Green Version]
- Youness, C.; Valette-Florence, P.; Herrmann, J.-L. The Effects of Customer-Based Online Reputation on WOM and WPP: The Mediating Role of BRQ: An Abstract. In Proceedings of the 2008 Academy of Marketing Science (AMS) Annual Conference, Porto, Portugal, 26–29 June 2018; pp. 893–894. [Google Scholar]
- Al-Yazidi, S.; Berri, J.; Al-Qurishi, M.; Al-Alrubaian, M. Measuring Reputation and Influence in Online Social Networks: A Systematic Literature Review. IEEE Access 2020, 8, 1. [Google Scholar] [CrossRef]
- Tadelis, S. Reputation and Feedback Systems in Online Platform Markets. Annu. Rev. Econ. 2016, 8, 321–340. [Google Scholar] [CrossRef] [Green Version]
- Gavilan, D.; Avello, M.; Martinez-Navarro, G. The influence of online ratings and reviews on hotel booking consideration. Tour. Manag. 2018, 66, 53–61. [Google Scholar] [CrossRef]
- Luca, M. Reviews, Reputation, and Revenue: The Case of Yelp.com; Harvard Business School NOM Unit Working Paper: Boston, MA, USA, 2016. [Google Scholar]
- Patel, S.; Cain, R.; Neailey, K.; Hooberman, L.; Alemi, F.; Lagu, T. Exploring Patients’ Views Toward Giving Web-Based Feedback and Ratings to General Practitioners in England: A Qualitative Descriptive Study. J. Med. Internet Res. 2016, 18, e217. [Google Scholar] [CrossRef] [Green Version]
- Burkle, C.M.; Keegan, M.T. Popularity of internet physician rating sites and their apparent influence on patients’ choices of physicians. BMC Health Serv. Res. 2015, 15, 416. [Google Scholar] [CrossRef] [Green Version]
- Gu, D.; Yang, X.; Li, X.; Jain, H.K.; Liang, C. Understanding the Role of Mobile Internet-Based Health Services on Patient Satisfaction and Word-of-Mouth. Int. J. Environ. Res. Public Health 2018, 15, 1972. [Google Scholar] [CrossRef] [Green Version]
- Davydovich, A.R.; Shmeleva, T.V.; Syrkova, I.S. The medical organization of primary care: Competitiveness and reputation. Probl. Soc. Hyg. Public Health Hist. Med. 2020, 28, 729–735. [Google Scholar] [CrossRef]
- Sattler, H.; Völckner, F.; Riediger, C.; Ringle, C.M. The impact of brand extension success drivers on brand extension price premiums. Int. J. Res. Mark. 2010, 27, 319–328. [Google Scholar] [CrossRef]
- Platow, M.J.; Grace, D.M.; Smithson, M.J. Examining the Preconditions for Psychological Group Membership. Soc. Psychol. Pers. Sci. 2011, 3, 5–13. [Google Scholar] [CrossRef]
- Koffka, K. Principles of Gestalt Psychology. A Harbinger Book; Harbinger: London, UK, 2005; Volume 20, pp. 623–628. [Google Scholar]
- Kurt, L. A Dynamic Theory of Personality. J. Nerv. Ment. Dis. 1936, 85, 612–613. [Google Scholar]
- Polley, R.B.; McGrath, J.E. Groups: Interaction and Performance. Adm. Sci. Q. 1984, 29, 469. [Google Scholar] [CrossRef]
- Johnson, D.W.; Johnson, R.T. Cooperation and Competition: Theory and Research; Interaction Book Company: Edina, MN, USA, 1989; p. viii, 253. [Google Scholar]
- Johnson, D.W.; Johnson, R.T. An Educational Psychology Success Story: Social Interdependence Theory and Cooperative Learning. Educ. Res. 2009, 38, 365–379. [Google Scholar] [CrossRef] [Green Version]
- Bruner, M.W.; Eys, M.; Evans, M.B.; Wilson, K. Interdependence and Social Identity in Youth Sport Teams. J. Appl. Sport Psychol. 2015, 27, 351–358. [Google Scholar] [CrossRef]
- Bertucci, A.; Johnson, D.W.; Johnson, R.T.; Conte, S. The Effects of Task and Resource Interdependence on Achievement and Social Support: An Exploratory Study of Italian Children. J. Psychol. 2011, 145, 343–360. [Google Scholar] [CrossRef]
- Colasante, A.; García-Gallego, A.; Morone, A.; Temerario, T. The Utopia of Cooperation: Does Intra-Group Competition Drive out Free Riding? 2017. Available online: http://www.doctreballeco.uji.es/wpficheros/Colasante_et_al_08_2017.pdf (accessed on 23 November 2020).
- Rogelberg, S.G. The SAGE Encyclopedia of Industrial and Organizational Psychology, 2nd ed.; SAGE Publication Inc.: Charlotte, NC, USA, 2017. [Google Scholar]
- Wu, H.; Lu, N. How your colleagues’ reputation impact your patients’ odds of posting experiences: Evidence from an online health community. Electron. Commer. Res. Appl. 2016, 16, 7–17. [Google Scholar] [CrossRef]
- Deng, Z.; Hong, Z.; Zhang, W.; Evans, R.M.; Chen, Y.; Hao, H.; Bidmon, S.; Li, L. The Effect of Online Effort and Reputation of Physicians on Patients’ Choice: 3-Wave Data Analysis of China’s Good Doctor Website. J. Med. Internet Res. 2019, 21, e10170. [Google Scholar] [CrossRef]
- Liu, X.; Chen, M.; Li, J.; Ma, L. How to Manage Diversity and Enhance Team Performance: Evidence from Online Doctor Teams in China. Int. J. Environ. Res. Public Health 2019, 17, 48. [Google Scholar] [CrossRef] [Green Version]
- Wu, H.; Lu, N. Service provision, pricing, and patient satisfaction in online health communities. Int. J. Med. Inform. 2018, 110, 77–89. [Google Scholar] [CrossRef]
- Montani, F.; Vandenberghe, C.; Khedhaouria, A.; Courcy, F. Examining the inverted U-shaped relationship between workload and innovative work behavior: The role of work engagement and mindfulness. Hum. Relat. 2019, 73, 59–93. [Google Scholar] [CrossRef]
- Rezvani, E.; Assaf, A.G.; Uysal, M.; Lee, M. Learning from own and others: The moderating role of performance aspiration. Int. J. Hosp. Manag. 2019, 81, 113–119. [Google Scholar] [CrossRef]
- Lind, J.T.; Mehlum, H. With or Without U? The Appropriate Test for a U-Shaped Relationship*. Oxf. Bull. Econ. Stat. 2010, 72, 109–118. [Google Scholar] [CrossRef] [Green Version]
| Variables | Variables Symbol | Explanation |
|---|---|---|
| Dependent variable | APPT | The cumulative number of patients who have made a appointment with the focal doctor. |
| Independent | Rep | Reputation of the focal doctor was obtained by averaging the number of likes and score of the focal doctor after standardization. |
| variables | O_rep | The average reputation of other doctors in the team except the focal doctor, that is, the average reputation of all ordinary doctors. It is calculated as follows. For each team, we first sum up the reputation of all members of the team, then subtract the reputation of the focal doctor, and divide the value obtained by the number of team members minus 1. |
| O_rep2 | The square of the average reputation of all ordinary doctors on the team. | |
| Control variables | Title | 1 to 5, with 1 being the lowest and 5 being the highest. |
| City | 1 to 7, with 1 being the lowest and 7 the highest. | |
| Hosp | 1 to 4, with 1 being the lowest and 4 the highest. | |
| Rev | The number of reviews received by the focal doctor. | |
| TeamSize | The number of people of the team. |
| Variables | Variables Symbol | Explanation |
|---|---|---|
| Dependent variable | APPT | The cumulative number of patients who have made an appointment with the focal doctor. |
| Rep | Reputation of the focal doctor was obtained by averaging the number of likes and score of the focal doctor after standardization. | |
| Independent | Leader_rep | The reputation of the leader physician on the team. |
| variables | Oo_rep | The average reputation of other doctors in the team except the focal doctor and the leader doctor, that is, the average reputation of other ordinary doctors except the focal doctor. For each team, we first sum up the reputation of all members of the team, then subtract the reputation of the focal doctor and the reputation of the leader doctor, and divide the value obtained by the number of people in the team minus the value after 2. |
| Oo_rep2 | The square of the average reputation of other ordinary doctors on the team. | |
| Control variables | Title | 1 to 5, with 1 being the lowest and 5 being the highest. |
| City | 1 to 7, with 1 being the lowest and 7 the highest. | |
| Hosp | 1 to 4, with 1 being the lowest and 4 the highest. | |
| Rev | The number of reviews received by the focal doctor. | |
| TeamSize | The number of people of the team. |
| Variable | Obs | Mean | Std. Dev. | Min | Max |
|---|---|---|---|---|---|
| APPT | 6103 | 543.64 | 2538.225 | 0.00 | 63,812 |
| Rep | 6103 | 0.196 | 1.072 | −0.353 | 25.498 |
| O_rep | 6103 | −0.094 | 0.831 | −0.489 | 20.558 |
| O_rep2 | 6103 | 0.699 | 6.849 | 0.00 | 422.621 |
| Rev | 6103 | 54.337 | 267.715 | 0.00 | 11,328 |
| TeamSize | 6103 | 5.107 | 3.025 | 1 | 88 |
| Title | 6103 | 4.774 | 0.433 | 1 | 5 |
| Hosp | 6103 | 2.978 | 0.164 | 1 | 3 |
| City | 6103 | 5.397 | 1.244 | 1 | 7 |
| Variables | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) |
|---|---|---|---|---|---|---|---|---|---|
| (1) APPT | 1.000 | ||||||||
| (2) Rep | 0.515 | 1.000 | |||||||
| (3) O_rep | 0.377 | 0.374 | 1.000 | ||||||
| (4) O_rep2 | 0.114 | 0.073 | 0.672 | 1.000 | |||||
| (5) Rev | 0.810 | 0.543 | 0.346 | 0.120 | 1.000 | ||||
| (6) TeamSize | 0.082 | 0.159 | 0.047 | −0.014 | 0.103 | 1.000 | |||
| (7) Title | 0.048 | 0.073 | 0.052 | 0.010 | 0.025 | 0.112 | 1.000 | ||
| (8) Hosp | 0.022 | 0.023 | 0.028 | 0.009 | 0.015 | 0.002 | 0.053 | 1.000 | |
| (9) City | 0.197 | 0.270 | 0.227 | 0.026 | 0.177 | 0.022 | 0.026 | −0.038 | 1.000 |
| (1) | (2) | |
|---|---|---|
| model1 | model2 | |
| Title | 0.233 *** | 0.218 *** |
| (0.0591) | (0.0589) | |
| City | 0.328 *** | 0.306 *** |
| (0.0199) | (0.0198) | |
| Hosp | 0.212 | 0.178 |
| (0.146) | (0.142) | |
| lnRev | 0.992 *** | 0.898 *** |
| (0.0178) | (0.0304) | |
| lnTeamSize | 0.167 ** | 0.164 ** |
| (0.0804) | (0.0802) | |
| Rep | 0.0455 | |
| (0.0527) | ||
| O_rep | 0.472 *** | |
| (0.0689) | ||
| O_rep2 | −0.0364 *** | |
| (0.0115) | ||
| _cons | −3.326 *** | −2.825 *** |
| (0.529) | (0.521) | |
| N | 6103 | 6103 |
| R2 | 0.552 | 0.559 |
| Dependent Variable: APPT | ||
|---|---|---|
| Test: H1: Inverse U Shape vs. H0: Monotone or U Shape | ||
| Specification: f(x) = x^2 Extreme Point: 6.477339 | ||
| Lower bound | Upper bound | |
| Interval | −0.4888113 | 20.55774 |
| Slope | 0.507623 | −1.026038 |
| t-value | 6.543666 | −2.408667 |
| p > |t| | 3.25 × 10-11 | 0.0080203 |
| Overall test of presence of a Inverse U shape: t-value = 2.4 p > |t| = 0.00802 | ||
| 95% Fieller interval for extreme point: [4.5529598; 13.757446] | ||
| Variable | Obs | Mean | Std. Dev. | Min | Max |
|---|---|---|---|---|---|
| APPT | 25,040 | 254.081 | 1,846.458 | 0 | 70,117 |
| Rep | 25,040 | −0.048 | 0.713 | −0.353 | 26.053 |
| Leader rep | 25,040 | 0.016 | 0.827 | −0.479 | 13.106 |
| Oo rep | 25,040 | 0.027 | 0.815 | −0.329 | 34.38 |
| Oo rep2 | 25,040 | 0.666 | 12.253 | 0 | 1182.011 |
| Rev | 25,040 | 30.975 | 220.643 | 0 | 12,499 |
| TeamSize | 25,040 | 7.326 | 7.553 | 2 | 88 |
| Title | 25,040 | 3.678 | 0.915 | 1 | 5 |
| Hosp | 25,040 | 2.958 | 0.241 | 1 | 3 |
| City | 25,040 | 5.381 | 1.277 | 1 | 7 |
| Variables | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) |
|---|---|---|---|---|---|---|---|---|---|---|
| (1) APPT | 1.000 | |||||||||
| (2) Rep | 0.497 | 1.000 | ||||||||
| (3) Leader_rep | 0.252 | 0.360 | 1.000 | |||||||
| (4) Oo_rep | 0.301 | 0.358 | 0.318 | 1.000 | ||||||
| (5) Oo_rep2 | 0.058 | 0.040 | 0.026 | 0.658 | 1.000 | |||||
| (6) Rev | 0.716 | 0.530 | 0.217 | 0.244 | 0.048 | 1.000 | ||||
| (7) TeamSize | 0.015 | 0.031 | 0.296 | 0.004 | −0.015 | 0.018 | 1.000 | |||
| (8) Title | 0.110 | 0.184 | −0.001 | 0.061 | 0.002 | 0.057 | −0.062 | 1.000 | ||
| (9) Hosp | 0.023 | 0.038 | −0.115 | 0.002 | 0.003 | 0.004 | −0.243 | 0.090 | 1.000 | |
| (10) City | 0.138 | 0.247 | 0.237 | 0.197 | 0.010 | 0.113 | −0.088 | 0.070 | −0.023 | 1.000 |
| (3) | (4) | |
|---|---|---|
| Model3 | Model4 | |
| Title | 0.493 *** | 0.512 *** |
| (0.0118) | (0.0114) | |
| City | 0.234 *** | 0.175 *** |
| (0.00751) | (0.00727) | |
| Hosp | 0.216 *** | 0.319 *** |
| (0.0327) | (0.0325) | |
| lnRev | 0.810 *** | 0.548 *** |
| (0.0120) | (0.0324) | |
| lnTeamSize | 0.113 *** | −0.0153 |
| (0.0229) | (0.0230) | |
| Rep | 0.334 *** | |
| (0.0836) | ||
| Leader_rep | 0.316 *** | |
| (0.0243) | ||
| Oo_rep | 0.481 *** | |
| (0.0364) | ||
| Oo_rep2 | −0.0194 *** | |
| (0.00396) | ||
| _cons | −3.560 *** | −3.116 *** |
| (0.142) | (0.138) | |
| N | 25,040 | 25,002 |
| R2 | 0.492 | 0.525 |
| Dependent Variable: APPT | ||
|---|---|---|
| Test: H1: Inverse U shape vs. H0: Monotone or U Shape | ||
| Specification: f(x) = x ^ 2 Extreme Point: 12.38148 | ||
| Lower bound | Upper bound | |
| Interval | −11.46711 | 34.38039 |
| Slope | 0.92726 | −0.8553423 |
| t-value | 7.7152 | −3.468163 |
| p > |t| | 6.25 × 10−15 | 0.0002625 |
| Overall test of presence of a Inverse U shape: t-value = 3.47 p > |t| = 0.000262 | ||
| 95% Fieller interval for extreme point: [9.6079864; 18.563818] | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, J.; Zhang, X.; Kong, J.; Wu, L. The Impact of Teammates’ Online Reputations on Physicians’ Online Appointment Numbers: A Social Interdependency Perspective. Healthcare 2020, 8, 509. https://doi.org/10.3390/healthcare8040509
Liu J, Zhang X, Kong J, Wu L. The Impact of Teammates’ Online Reputations on Physicians’ Online Appointment Numbers: A Social Interdependency Perspective. Healthcare. 2020; 8(4):509. https://doi.org/10.3390/healthcare8040509
Chicago/Turabian StyleLiu, Jingfang, Xin Zhang, Jun Kong, and Liangyu Wu. 2020. "The Impact of Teammates’ Online Reputations on Physicians’ Online Appointment Numbers: A Social Interdependency Perspective" Healthcare 8, no. 4: 509. https://doi.org/10.3390/healthcare8040509
APA StyleLiu, J., Zhang, X., Kong, J., & Wu, L. (2020). The Impact of Teammates’ Online Reputations on Physicians’ Online Appointment Numbers: A Social Interdependency Perspective. Healthcare, 8(4), 509. https://doi.org/10.3390/healthcare8040509






