Published Research on Burnout in Nursing in Spain in the Last Decade: Bibliometric Analysis
Abstract
1. Introduction
2. Methods
2.1. Procedure
2.2. Data Analysis
3. Results
3.1. Number of Publications Per Year and Selection of Journals
3.2. Review of Studies Performed in Spain
3.3. Co-Authorship Map of Studies Done in Spain and Variables Related to Burnout
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Mira, J.J.; Guilabert, M.; Pérez, V. La medida de la experiencia del paciente en el contexto de una atención centrada en el propio paciente [The measure of patient experience in the context of patient-centered care]. Med. Prev. 2018, 23, 5–11. [Google Scholar]
- Zafra-Ramírez, N.; Pérez-Milena, A.; Valverde-Bolívar, F.J.; Rodríguez-Bayón, A.; Delgado-Rodríguez, M. Oferta de actividades preventivas propuestas por médicos residentes de Medicina Familiar en Atención Primaria y su relación con las habilidades comunicacionales [Accomplishment of preventive activities proposed by resident doctors of Family Medicine in Primary Care and its relationship with communication skills]. Aten. Primaria 2019, 51, 562–570. [Google Scholar] [CrossRef] [PubMed]
- García, T.; Rodríguez, C.; Rodríguez, J.; Fernández, A.; Richarte, V.; Ramos-Quiroga, A. Psychosocial Profiles of Adults with ADHD: A Comparative Study of Prison and Outpatient Psychiatric Samples. Eur. J. Psychol. Appl. Leg. Context 2019, 11, 41–49. [Google Scholar] [CrossRef]
- Verdugo, M.A.; Fernández, M.; Gómez, L.E.; Amor, A.; Aza, A. Predictive factors of quality of life in acquired brain injury. Int. J. Clin. Health Psychol. 2019, 19, 189–197. [Google Scholar] [CrossRef]
- Kim, S.; Jung, H.; Kim, Y. Emotional labor experienced of ward nurses. J. Korean Soc. Occup. Environ. Hyg. 2016, 26, 377–387. [Google Scholar] [CrossRef]
- Lee, E.K.; Ji, E.J. The moderating role of leader-member Exchange in the relationships between emotional labor and burnout in clinical nurses. Asian Nurs. Res. 2018, 12, 56–61. [Google Scholar] [CrossRef]
- López-García, C.; Ruiz-Hernández, J.A.; Llor-Zaragoza, L.; Llor-Zaragoza, P.; Jiménez-Barbero, J.A. User Violence and Psychological Well-being in Primary Health-Care Professionals. Eur. J. Psychol. Appl. Leg. Context 2018, 10, 57–63. [Google Scholar] [CrossRef]
- Nespereira-Campuzano, T.; Vázquez-Campo, M. Inteligencia emocional y manejo del estrés en profesionales de Enfermería del Servicio de Urgencias hospitalarias [Emotional intelligence and stress management in Nursing professionals in a hospital emergency department]. Enferm. Clin. 2017, 27, 172–178. [Google Scholar] [CrossRef]
- White, E.M.; Aiken, L.H.; Sloane, D.M.; McHugh, M.D. Nursing home work environment, care quality, registered nurse burnout and job dissatisfaction. Geriatr. Nurs. 2019, 41, 158–164. [Google Scholar] [CrossRef]
- Dall’Ora, C.; Griffiths, P.; Ball, J.; Simon, M.; Aiken, L.H. Association of 12 h shifts and nurses’ job satisfaction, burnout and intention to leave: Findings from a cross-sectional study of 12 European countries. BMJ Open 2015, 5, e008331. [Google Scholar] [CrossRef]
- Gázquez, J.J.; Pérez-Fuentes, M.C.; Molero, M.M.; Oropesa, N.F.; Simón, M.M.; Saracostti, M. Sleep Quality and the Mediating Role of Stress Management on Eating by Nursing Personnel. Nutrients 2019, 11, 1731. [Google Scholar] [CrossRef]
- Pérez-Fuentes, M.C.; Molero, M.M.; Simón, M.M.; Gázquez, J.J. Analysis of Sociodemographic and Psychological Variables Involved in Sleep Quality in Nurses. Int. J. Environ. Res. Public Health 2019, 16, 3846. [Google Scholar] [CrossRef] [PubMed]
- Brandolim, N.; Neves, S.; Viseu, J.N.; Dieter, C.; Guerreiro, M.; Domingues, R.B. Depression and quality of life in older adults: Mediation effect of sleep quality. Int. J. Clin. Health Psychol. 2018, 18, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Szczygiel, D.D.; Mikolajczak, M. Emotional Intelligence Buffers the Effects of Negative Emotions on Job Burnout in Nursing. Front. Physiol. 2018, 9, 2649. [Google Scholar] [CrossRef]
- Martos, A.; Pérez-Fuentes, M.C.; Molero, M.M.; Gázquez, J.J.; Simón, M.M.; Barragán, A.B. Burnout y engagement en estudiantes de Ciencias de la Salud [Burnout and engagement in students of health sciences]. Eur. J. Investig. Health Psychol. Educ. 2018, 8, 23–36. [Google Scholar] [CrossRef]
- Reche, C.; De Francisco, C.; Martínez-Rodríguez, A.; Ros-Martínez, A. Relationship among sociodemographic and sport variables, exercise dependence, and burnout: A preliminary study in athletes. An. Psicol. (Spain) 2018, 34, 398–404. [Google Scholar] [CrossRef]
- Rodríguez, F.J. Burnout or the emotional impact of working with special populations. Rev. Esp. Sanid. Penit. 2018, 20, 38–39. [Google Scholar]
- Vizoso-Gómez, C.; Arias-Gundín, O. Resiliencia, optimismo y burnout académico en estudiantes universitarios [Resilience, optimism and academic burnout in university students]. Eur. J. Educ. Psychol. 2018, 11, 47–59. [Google Scholar] [CrossRef]
- Navarro, D.; Ayechu, A.; Huarte, I. Prevalencia del síndrome de burnout y factores asociados a dicho síndrome en los profesionales sanitarios de Atención Primaria [Prevalence of burnout syndrome and its associated factors in Primary Care staff]. Semergen 2015, 4, 191–198. [Google Scholar] [CrossRef]
- Montgomery, A.; Panagopoulou, E.; Esmail, A.; Richards, T.; Maslach, C. Burnout in healthcare: The case for organisational change. BMJ 2019, 366, l4774. [Google Scholar] [CrossRef]
- Poghosyan, L.; Clarke, S.P.; Finlayson, M.; Aiken, L.H. Nurse burnout and quality of care: Cross-national investigation in six countries. Res. Nurs. Health 2010, 33, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Mealer, M.; Burnham, E.L.; Goode, C.J.; Rothbaum, B.; Moss, M. The prevalence and impact of post traumatic stress disorder and burnout syndrome in nurses. Depress. Anxiety 2009, 26, 1118–1126. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C.; Leiter, M.P. Burnout. In Encyclopedia of Mental Health, 2nd ed.; Friedman, H., Ed.; Elsevier: Oxford, UK, 2016; pp. 222–227. [Google Scholar]
- Konstantinou, A.K.; Bonotis, K.; Sokratous, M.; Siokas, V.; Dardiotis, E. Burnout Evaluation and Potential Predictors in a Greek Cohort of Mental Health Nurses. Arch. Psychiatr. Nurs. 2018, 32, 449–456. [Google Scholar] [CrossRef] [PubMed]
- Dall’Ora, C.; Ball, J.; Reinius, M.; Grffiths, P. Burnout in nursing: A theoretical review. Hum. Resour. Health 2020, 18, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Fuentes, M.C.; Molero, M.M.; Gázquez, J.J.; Simón, M.M. Analysis of burnout predictors in nursing: Risk and protective psychological factors. Eur. J. Psychol. Appl. Leg. Context 2019, 11, 33–40. [Google Scholar] [CrossRef]
- Bagnall, A.M.; Jones, R.; Akter, H.; Woodall, J. Interventions to Prevent Burnout in High. Risk Individuals: Evidence Review; Public Health England: London, UK, 2016. [Google Scholar]
- Lee, M.A.; Ju, Y.H.; Lim, S.H. A study on the intent to leave and stay among hospital nurses in Korea: A cross-sectional survey. J. Nurs. Manag. 2020, 28, 332–341. [Google Scholar] [CrossRef]
- Ávila, J.H.; Gómez, L.T.; Montiel, M.M. Características demográficas y laborales asociadas al Síndrome de Burnout en profesionales de la salud [Demographic and occupational characteristics associated with burnout syndrome in health professionals]. Pensam. Psicológico 2010, 8, 39–52. [Google Scholar]
- Gómez-Urquiza, J.L.; Monsalve-Reyes, C.S.; San Luis-Costas, C.; Fernández-Castillo, R.; Aguayo-Estremera, R.; Cañadas-de la Fuente, G.A. Factores de riesgo y niveles de burnout en enfermeras de atención primaria: Una revisión sistemática [Risk factors and burnout levels in Primary Care nurses: A systematic review]. Aten. Primaria 2017, 49, 77–85. [Google Scholar] [CrossRef]
- Barragán, A.B.; Martos, A.; Cardila, F.; Molero, M.M.; Pérez-Fuentes, M.C.; Gázquez, J.J. Variables relacionadas y prevalencia del burnout en profesionales sanitarios [Related variables and prevalence of burnout in health professionals]. Eur. J. Health Res. 2015, 1, 5–14. [Google Scholar] [CrossRef]
- Rusca, K.; Setyowati. Prevalence of burnout syndrome among nurses in general hospitals in provincial East Java: Cross-sectional study. Enferm. Clin. 2019, 29, 362–366. [Google Scholar] [CrossRef]
- Kim, H.S.; Yeom, H.A. The association between spiritual well-being and burnout in intensive care unit nurses: A descriptive study. Intensiv. Crit. Care Nurs. 2018, 46, 92–97. [Google Scholar] [CrossRef]
- Martín, R.A. Burnout en enfermería: Prevalencia y factores relacionados en el medio hospitalario [Burnout in nursing: Prevalence and related factors in a hospital environment]. Rev. Cient. Soc. Esp. Enferm. Neurol. 2015, 41, 9–14. [Google Scholar] [CrossRef]
- Grau, A.; Flichtentrei, D.; Suner, R.; Prats, M.; Braga, F. Influencia de factores personales, profesionales y transnacionales en el sindrome de burnout en personal sanitario hispanoamericano y Español (2007) [Influence of personal, professional and transnational factors in the burnout syndrome in Hispanic American and Spanish health personnel (2007)]. Rev. Esp. Salud Pública 2009, 83, 215–230. [Google Scholar]
- Álvarez, L.; Mori, P.; Gómez, M.C. Síndrome de burnout y satisfacción laboral en enfermeras españolas en tiempo de crisis económica [Burnout Syndrome and job satisfaction among Spanish nurses at a time of economic crisis]. Metas Enferm. 2019, 22, 50–58. [Google Scholar] [CrossRef]
- Juliá-Sanchis, R.; Richart-Martínez, M.; García-Aracil, N.; José-Alcaide, L.; Piquer-Donat, T.; Castejón, M.E. Measuring the levels of burnout syndrome and empathy of Spanish emergency medical service professionals. Australas. Emerg. Care 2019, 22, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Portero, S.; Cebrino, J.; Herruzo, J.; Vaquero-Abellán, M. A multicenter study into burnout, perceived stress, job satisfaction, coping strategies, and general health among emergency department nursing staff. J. Clin. Med. 2020, 9, 1007. [Google Scholar] [CrossRef] [PubMed]
- Sanclemente, I.; Elboj, C.; Íñiguez, T. La prevención del síndrome de burnout en la enfermería española. Revisión bibliográfica [Prevention of burnout syndrome in spanish nursing. Literature review]. Nure Investig. 2016, 13, 1–6. [Google Scholar]
- Molero, M.M.; Pérez-Fuentes, M.C.; Gázquez, J.J. Analysis of the Mediating Role of Self-Efficacy and Self-Esteem on the Effect of Workload on Burnout’s Influence on Nurses’ Plans to Work Longer. Front. Psychol. 2018, 9, 2605. [Google Scholar] [CrossRef]
- Molero, M.M.; Pérez-Fuentes, M.C.; Gázquez, J.J.; Barragán, A.B. Burnout in health professionals according to their self-esteem, social support and empathy profile. Front. Psychol. 2018, 9, 424. [Google Scholar] [CrossRef]
- Taleghani, F.; Ashouri, E.; Saburi, M. Empathy, Burnout, Demographic Variables and their Relationships in Oncology Nurses. Iran. J. Nurs. Midwifery Res. 2017, 22, 41–45. [Google Scholar] [CrossRef]
- Wang, Q.; Wang, L.; Shi, M.; Li, X.; Liu, R.; Liu, J.; Zhu, M.; Wu, H. Empathy, burnout, life satisfaction, correlations and associated socio-demographic factors among Chinese undergraduate medical students: An exploratory cross-sectional study. BMC Med. Educ. 2019, 19, 341. [Google Scholar] [CrossRef] [PubMed]
- Yao, Y.; Zhao, S.; Gao, X.; An, Z.; Wang, S.; Li, H.; Li, Y.; Gao, L.; Lu, L.; Dong, Z. General self-efficacy modifies the effect of stress on burnout in nurses with different personality types. BMC Health Serv. Res. 2018, 18, 667. [Google Scholar] [CrossRef] [PubMed]
- Molero, M.; Pérez-Fuentes, M.; Atria, L.; Oropesa, N.F.; Gázquez, J.J. Burnout, Perceived Efficacy, and Job Satisfaction: Perception of the Educational Context in High School Teachers. BioMed Res. Int. 2019, 1021408. [Google Scholar] [CrossRef]
- Gorbea-Portal, S. Tendencias transdisciplinarias en los estudios métricos de la información y su relación con la gestión de la información y del conocimiento [Transdisciplinary trends in information metrics studies and its relation to the management of information and knowledge]. Perspect. Gestão Conhecimento 2013, 3, 13–27. [Google Scholar]
- Koskinen, J.; Isohanni, M.; Paajala, H.; Jaaskelainen, E.; Nieminen, P.; Koponen, H.; Tienari, P.; Miettunen, J. How to use bibliometric methods in evaluation of scientific research? An example from Finnish schizophrenia research. Nord. J. Psychiatry 2008, 62, 136–143. [Google Scholar] [CrossRef]
- Aparicio-Martínez, P.; Perea-Moreno, A.J.; Martínez-Jiménez, M.P.; Redel-Macías, M.D.; Vaquero-Abellan, M.; Pagliari, C. A bibliometric analysis of the health field regarding social networks and young people. Int. J. Environ. Res. Public Health 2019, 16, 4024. [Google Scholar] [CrossRef]
- Briganti, M.; Delnevo, C.D.; Brown, L.; Hastings, S.E.; Steinberg, M.B. Bibliometric Analysis of Electronic Cigarette Publications: 2003–2018. Int. J. Environ. Res. Public Health 2019, 16, 320. [Google Scholar] [CrossRef]
- Xuan, B.; McIntyre, R.S.; Latkin, C.A.; Thanh, H.; Thu, G.; Thi, H.L. The current research landscape on the artificial intelligence application in the management of depressive disorders: A bibliometric analysis. Int. J. Environ. Res. Public Health 2019, 16, 2150. [Google Scholar] [CrossRef]
- Carneiro, K.C.; Brito, J.; Carneiro, R.; Belarmino, A.L.; Barros, E.O.; Dantas, M.S. National scientific production on Burnout Syndrome in ICU nurses and physicians: A bibliometric study. Rev. Assoc. Med. Bras. 2019, 65, 722–729. [Google Scholar] [CrossRef]
- Marín, E.; Ortín, F.J.; Garcés de los Fayos, E.J.; Tutte, V. Análisis bibliométrico de burnout y optimismo en deporte [Bibliometric analysis ofburnout and optimism in sport]. Sport TK 2013, 2, 77–87. [Google Scholar]
- Dávila, C.D.; López-Valcárcel, B.G. Crisis económica y salud [Economic crisis and health]. Gac. Sanit. 2009, 23, 261–265. [Google Scholar] [CrossRef] [PubMed]
- Sermeus, W. Impact of the financial crisis and health workforce crisis on the sustainability of the healthcare system: What’s next? Enferm. Clin. 2012, 22, 179–181. [Google Scholar] [CrossRef] [PubMed]
- Zabalegui, A.; Cabrera, E. Economic crisis and nursing in Spain. J. Nurs. Manag. 2010, 18, 505–508. [Google Scholar] [CrossRef]
- Muñoz, J.; Del Amor, N.; Lázaro, M.; Carranza, A.; Martínez, M. Análisis de impacto de la crisis económica sobre el síndrome de Burnout y resiliencia en el personal de enfermería [Analysis of the impact of the economic crisis on Burnout syndrome and resilience in nursing personnel]. Enferm. Glob. 2017, 16, 315–335. [Google Scholar] [CrossRef][Green Version]
- World Health Organization. Burn-out an “Occupational Phenomenon”: International Classification of Diseases. 2019. Available online: https://www.who.int/mental_health/evidence/burn-out/en/ (accessed on 13 September 2020).
- Smith, K. Beyond Evidence Based Policy in Public Health: The Interplay of Ideas; Palgrave Macmillan: Basingstoke, UK, 2013. [Google Scholar]
- World Health Organization. Evaluation of the Impact of WHO Publications; WHO Evaluation Office: Ottawa, ON, Canada, 2016. [Google Scholar]
- Persson, O.R.; Danell, R.; Wiborg-Schneider, J. How to use Bibexcel for various types of bibliometric analysis. In Celebrating Scholarly Communication Studies: A Festschrift for Olle Persson at His 60th Birthday; Åström, F., Danell, R., Larsen, B., Schneider, J., Eds.; International Society for Scientometrics and Informetrics: Leuven, Belgium, 2009; pp. 9–24. [Google Scholar]
- Batagelj, V.; Mrvar, A. Pajek—A program for large network analysis. Connections 1998, 21, 47–57. [Google Scholar]
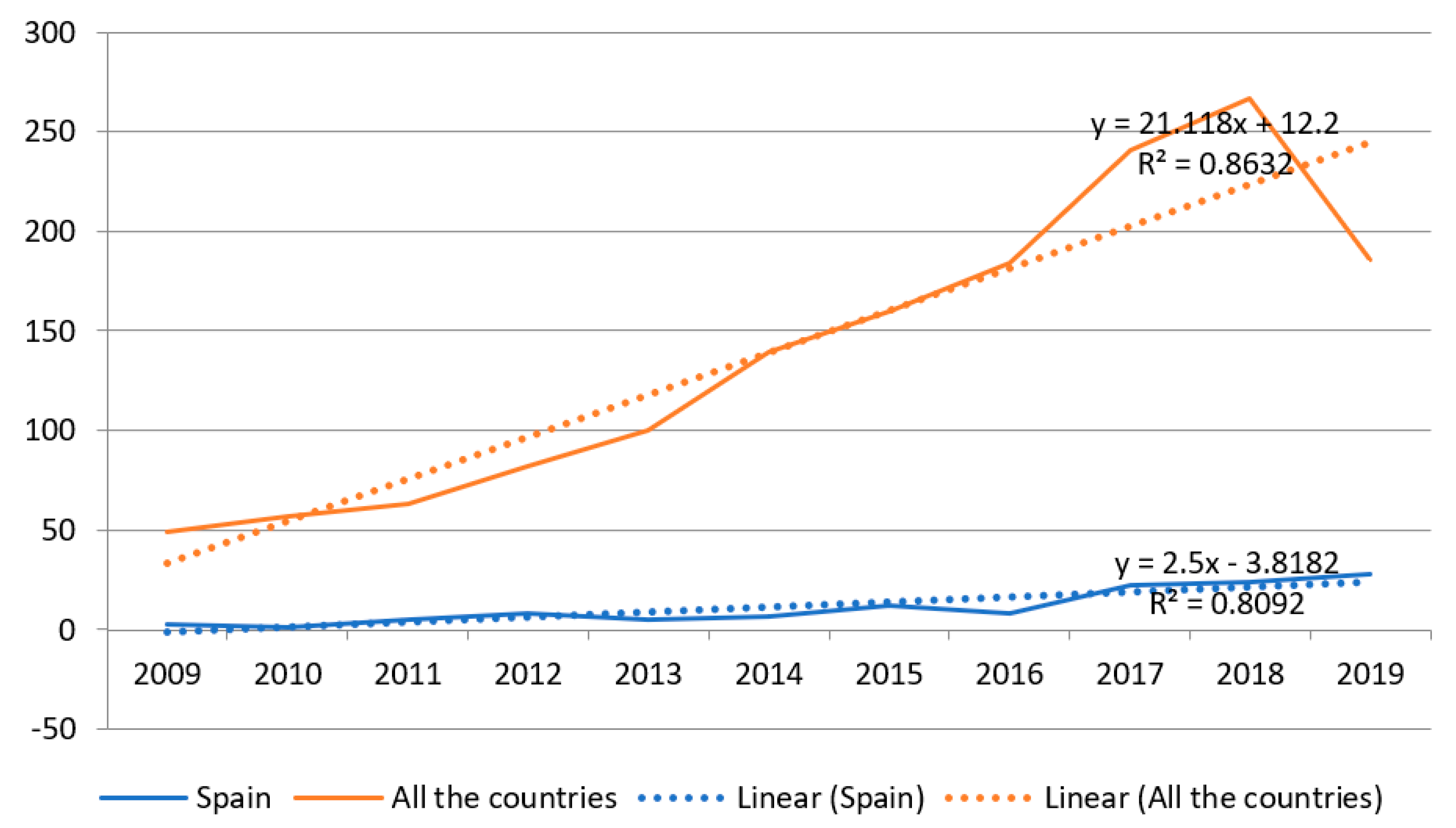




| Year | Number of Publications | Number of Publications in Spain |
|---|---|---|
| 2009 | 49 | 3 |
| 2010 | 57 | 1 |
| 2011 | 63 | 5 |
| 2012 | 82 | 8 |
| 2013 | 100 | 5 |
| 2014 | 139 | 7 |
| 2015 | 160 | 12 |
| 2016 | 184 | 8 |
| 2017 | 241 | 22 |
| 2018 | 267 | 24 |
| 2019 | 186 | 28 |
| Total | 1528 | 123 |
| Year | Number of Publications in Spain | Number of References | N References <5 Years | Price Index (%) |
|---|---|---|---|---|
| 2009 | 3 | 75 | (2005–2009) 1 | 1.33 |
| 2010 | 1 | 1 | (2006–2010) 0 | 0 |
| 2011 | 5 | 209 | (2007–2011) 3 | 1.43 |
| 2012 | 8 | 193 | (2008–2012) 3 | 1.55 |
| 2013 | 5 | 183 | (2009–2013) 6 | 3.27 |
| 2014 | 7 | 122 | (2010–2014) 3 | 2.45 |
| 2015 | 12 | 244 | (2011–2015) 9 | 3.68 |
| 2016 | 8 | 59 | (2012–2016) 2 | 3.38 |
| 2017 | 22 | 259 | (2013–2017) 33 | 12.74 |
| 2018 | 24 | 135 | (2014–2018) 21 | 15.55 |
| 2019 | 28 | 38 | (2015–2019) 38 | 100 |
| Total | 123 | 1518 | 119 | 7.83 |
| Productivity Level | N Studies | Authors | |
|---|---|---|---|
| n | % | ||
| 3 | > or =10 | 6 | 1.43 |
| 2 | 2 to 9 | 50 | 11.9 |
| 1 | 1 | 364 | 86.67 |
| Total | 420 | 100 | |
| Study Design | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Observational | Experimental | ||||||||||
| Cross-sectional | Longitudinal | Clinical trials | |||||||||
| n | % | n | % | n | % | ||||||
| 42 | 87.5 | 2 | 4.2 | 4 | 8.3 | ||||||
| Instruments | |||||||||||
| MBI | CBB | Other questionnaires | |||||||||
| n | % | n | % | n | % | ||||||
| 36 | 75 | 6 | 12.5 | 6 | 12.5 | ||||||
| Number of variables per study | |||||||||||
| Analyses with one variable | Analyses with two variables | Analyses with three variables | Analyses with four variables | Analyses with five variables | Analyses with seven variables | ||||||
| n | % | n | % | n | % | n | % | n | % | n | % |
| 14 | 29.2 | 16 | 33.3 | 10 | 20.8 | 3 | 6.3 | 4 | 8.3 | 1 | 2.1 |
| Variables | Number of Studies | Variables | Number of Studies |
|---|---|---|---|
| Aggressive behavior | 1 | Organizational behaviors | 1 |
| Altruism | 1 | Perceived social support | 2 |
| Anxiety or depression Disorders | 4 | Personality profiles | 7 |
| Autonomy | 1 | Positive and negative effect | 1 |
| Care assessment | 1 | Practice environment of the nurses | 1 |
| Communication skills | 2 | Psychological disturbance | 1 |
| Competence | 1 | Relatedness | 1 |
| Compliance | 1 | Resilience | 4 |
| Coping | 2 | Satisfaction | 3 |
| Emotional intelligence | 5 | Self-compassion | 2 |
| Empathy | 8 | Self-concept | 1 |
| Empowerment | 1 | Self-conduct | 1 |
| Engagement | 5 | Self-efficacy | 4 |
| General health | 5 | Self-esteem | 1 |
| Health problems | 1 | Self-perceived health | 1 |
| Job satisfaction | 8 | Sleep quality | 1 |
| Job strain | 1 | Subjective social support | 1 |
| Loneliness | 1 | Trauma screening | 1 |
| Mental health | 1 | Wellness in the academic context | 1 |
| Mindfulness | 1 | Work stress | 3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barragán Martín, A.B.; Molero Jurado, M.d.M.; Pérez-Fuentes, M.d.C.; Simón Márquez, M.d.M.; Sisto, M.; Gázquez Linares, J.J. Published Research on Burnout in Nursing in Spain in the Last Decade: Bibliometric Analysis. Healthcare 2020, 8, 478. https://doi.org/10.3390/healthcare8040478
Barragán Martín AB, Molero Jurado MdM, Pérez-Fuentes MdC, Simón Márquez MdM, Sisto M, Gázquez Linares JJ. Published Research on Burnout in Nursing in Spain in the Last Decade: Bibliometric Analysis. Healthcare. 2020; 8(4):478. https://doi.org/10.3390/healthcare8040478
Chicago/Turabian StyleBarragán Martín, Ana Belén, María del Mar Molero Jurado, María del Carmen Pérez-Fuentes, María del Mar Simón Márquez, Maria Sisto, and José Jesús Gázquez Linares. 2020. "Published Research on Burnout in Nursing in Spain in the Last Decade: Bibliometric Analysis" Healthcare 8, no. 4: 478. https://doi.org/10.3390/healthcare8040478
APA StyleBarragán Martín, A. B., Molero Jurado, M. d. M., Pérez-Fuentes, M. d. C., Simón Márquez, M. d. M., Sisto, M., & Gázquez Linares, J. J. (2020). Published Research on Burnout in Nursing in Spain in the Last Decade: Bibliometric Analysis. Healthcare, 8(4), 478. https://doi.org/10.3390/healthcare8040478










