Acceptability and Feasibility of a Sedentary Behavior Reduction Program during Pregnancy: A Semi-Experimental Study
Abstract
1. Introduction
2. Materials and Methods
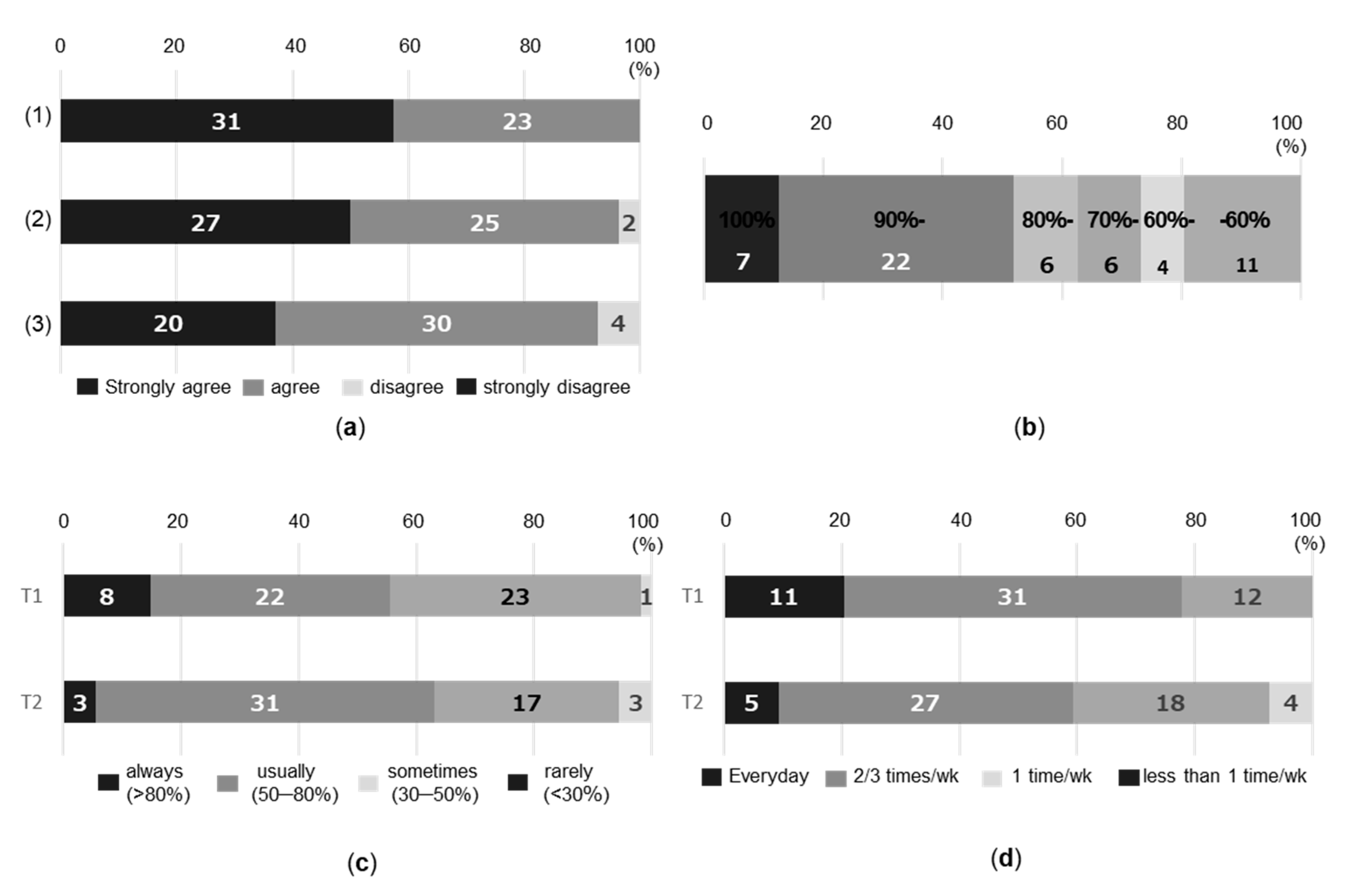
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Nascimento, S.L.; Surita, F.G.; Cecatti, J.G. Physical exercise during pregnancy: A systematic review. Curr. Opin. Obstet. Gynecol. 2012, 24, 387–394. [Google Scholar] [CrossRef] [PubMed]
- Poudevigne, M.S.; O‘Connor, P.J. Physical activity and mood during pregnancy. Med. Sci. Sports Exerc. 2005, 37, 1374–1380. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Artal, R.; O’Toole, M. Guidelines of the American College of Obstetricians and Gynecologists for exercise during pregnancy and the postpartum period. Br. J. Sports Med. 2003, 37, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Royal College of Obstetricians and Gynaecologists. Exercise in Pregnancy RCOG Statement NO 4; Royal College of Obstetricians and Gynaecologists: London, UK, 2006. [Google Scholar]
- Hesketh, K.R.; Evenson, K.R. Prevalence of U.S. Pregnant Women Meeting 2015 ACOG Physical Activity Guidelines. Am. J. Prev. Med. 2016, 51, e87–e89. [Google Scholar] [CrossRef]
- Nascimento, S.L.; Surita, F.G.; Godoy, A.C.; Kasawara, K.T.; Morais, S.S. Physical activity patterns and factors related to exercise during pregnancy: A cross sectional study. PLoS ONE 2015, 10, e0128953. [Google Scholar] [CrossRef]
- Donahue, S.M.; Zimmerman, F.J.; Starr, J.R.; Holt, V.L. Correlates of pre-pregnancy physical inactivity: Results from the pregnancy risk assessment monitoring system. Matern. Child Health J. 2010, 14, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Garnæs, K.K.; Mørkved, S.; Salvesen, Ø.; Moholdt, T. Exercise training and weight gain in obese pregnant women: A randomized controlled trial (ETIP Trial). PLoS Med. 2016, 13, e1002079. [Google Scholar] [CrossRef] [PubMed]
- Guelinckx, I.; Devlieger, R.; Mullie, P.; Vansant, G. Effect of lifestyle intervention on dietary habits, physical activity, and gestational weight gain in obese pregnant women: A randomized controlled trial. Am. J. Clin. Nutr. 2010, 91, 373–380. [Google Scholar] [CrossRef]
- Oostdam, N.; van Poppel, M.N.; Wouters, M.G.; Eekhoff, E.M.; Bekedam, D.J.; Kuchenbecker, W.K.; Quartero, H.W.; Heres, M.H.; van Mechelen, W. No effect of the FitFor2 exercise programme on blood glucose, insulin sensitivity, and birthweight in pregnant women who were overweight and at risk for gestational diabetes: Results of a randomised controlled trial. BJOG Int. J. Obstet. Gynaecol. 2012, 119, 1098–1107. [Google Scholar] [CrossRef]
- Pearce, E.E.; Evenson, K.R.; Downs, D.S.; Steckler, A. Strategies to promote physical activity during pregnancy: A systematic review of intervention evidence. Am. J. Lifestyle Med. 2013, 7, 38–50. [Google Scholar] [CrossRef]
- Currie, S.; Sinclair, M.; Murphy, M.H.; Madden, E.; Dunwoody, L.; Liddle, D. Reducing the decline in physical activity during pregnancy: A systematic review of behaviour change interventions. PLoS ONE 2013, 8, e66385. [Google Scholar] [CrossRef]
- Currie, S.; Sinclair, M.; Liddle, D.S.; Nevill, A.; Murphy, M.H. Application of objective physical activity measurement in an antenatal physical activity consultation intervention: A randomised controlled trial. BMC Public Health 2015, 15, 1259. [Google Scholar] [CrossRef] [PubMed]
- Haakstad, L.A.; Bø, K. Effect of regular exercise on prevention of excessive weight gain in pregnancy: A randomised controlled trial. Eur. J. Contracept. Reprod. Health Care 2011, 16, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Clarke, P.E.; Gross, H. Women’s behaviour, beliefs and information sources about physical exercise in pregnancy. Midwifery 2004, 20, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Connelly, M.; Brown, H.; van der Pligt, P.; Teychenne, M. Modifiable barriers to leisure-time physical activity during pregnancy: A qualitative study investigating first time mother‘s views and experiences. BMC Preg. Childbirth 2015, 15, 100. [Google Scholar] [CrossRef]
- Leiferman, J.; Swibas, T.; Koiness, K.; Marshall, J.A.; Dunn, A.L. My baby, my move: Examination of perceived barriers and motivating factors related to antenatal physical activity. J. Midwif. Women’s Health 2011, 56, 33–40. [Google Scholar] [CrossRef]
- Duncombe, D.; Wertheim, E.H.; Skouteris, H.; Paxton, S.J.; Kelly, L. Factors related to exercise over the course of pregnancy including women‘s beliefs about the safety of exercise during pregnancy. Midwifery 2009, 25, 430–438. [Google Scholar] [CrossRef]
- Otten, J.J.; Jones, K.E.; Littenberg, B.; Harvey-Berino, J. Effects of television viewing reduction on energy intake and expenditure in overweight and obese adults: A randomized controlled trial. Arch. Intern. Med. 2009, 169, 2109–2115. [Google Scholar] [CrossRef]
- Raynor, H.A.; Steeves, E.A.; Bassett, D.R., Jr.; Thompson, D.L.; Gorin, A.A.; Bond, D.S. Reducing TV watching during adult obesity treatment: Two pilot randomized controlled trials. Behav. Ther. 2013, 44, 674–685. [Google Scholar] [CrossRef]
- Gardiner, P.A.; Eakin, E.G.; Healy, G.N.; Owen, N. Feasibility of reducing older adults’ sedentary time. Am. J. Prev. Med. 2011, 41, 174–177. [Google Scholar] [CrossRef]
- Kawajiri, M.; Nakamura, Y.; Takeishi, Y.; Ito, N.; Atogami, F.; Yoshizawa, T. Longitudinal study of physical activity using an accelerometer in Japanese pregnant women. Jpn. J. Nurs. Sci. 2020, 17, e12294. [Google Scholar] [CrossRef] [PubMed]
- Cooley, D.; Pedersen, S. A pilot study of increasing nonpurposeful movement breaks at work as a means of reducing prolonged sitting. J. Environ. Public Health 2013, 2013, 128376. [Google Scholar] [CrossRef]
- Brooke, S.M.; An, H.S.; Kang, S.K.; Noble, J.M.; Berg, K.E.; Lee, J.M. Concurrent validity of wearable activity trackers under free-living conditions. J. Strength Cond. Res. 2017, 31, 1097–1106. [Google Scholar] [CrossRef]
- Japanese Ministry of Health, Labour and Welfare. For Your Well-Being During Pregnancy and Delivery. Available online: https://www.mhlw.go.jp/seisakunitsuite/bunya/kodomo/kodomo_kosodate/boshi-hoken/ninpu-01.html (accessed on 31 August 2020).
- Trost, S.G.; McIver, K.L.; Pate, R.R. Conducting accelerometer-based activity assessments in field-based research. Med. Sci. Sports Exerc. 2005, 37, S531–S543. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, K.; Hashimoto, K.; Suzuki, T. Wearable sensors corresponding to various applications healthcare field. Toshiba Rev. 2014, 69–11, 13–16. (In Japanese) [Google Scholar]
- Bauman, A.; Ainsworth, B.E.; Sallis, J.F.; Hagströmer, M.; Craig, C.L.; Bull, F.C.; Pratt, M.; Venugopal, K.; Chau, J.; Sjöström, M.; et al. The descriptive epidemiology of sitting. A 20-country comparison using the International Physical Activity Questionnaire (IPAQ). Am. J. Prev. Med. 2011, 41, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Lee, J.H.; Vittinghoff, E.; Fukuoka, Y. MHealth physical activity intervention: A randomized pilot study in physically inactive pregnant women. Matern. Child Health J. 2016, 20, 1091–1101. [Google Scholar] [CrossRef] [PubMed]
- Aspvik, N.P.; Viken, H.; Ingebrigtsen, J.E.; Zisko, N.; Mehus, I.; Wisløff, U.; Stensvold, D. Do weather changes influence physical activity level among older adults?—The Generation 100 study. PLoS ONE 2018, 13, e0199463. [Google Scholar] [CrossRef]
- Doherty, A.; Jackson, D.; Hammerla, N.; Plötz, T.; Olivier, P.; Granat, M.H.; White, T.; van Hees, V.T.; Trenell, M.I.; Owen, C.G.; et al. Large scale population assessment of physical activity using wrist worn accelerometers: The UK Biobank study. PLoS ONE 2017, 12, e0169649. [Google Scholar] [CrossRef]
- Michie, S.; Abraham, C.; Whittington, C.; McAteer, J.; Gupta, S. Effective techniques in healthy eating and physical activity interventions: A meta-regression. Health Psychol. 2009, 28, 690–701. [Google Scholar] [CrossRef]
- Charles Abraham, M.K. Writing Health Communication: An Evidence Based Guide; SAGE Publications Ltd.: New York, NY, USA, 2011. [Google Scholar]


| Characteristic 1 | Intervention (n = 56) | Control (n = 34) | p-Value | ||
|---|---|---|---|---|---|
| Age (years) | 34.4 ± 5.1 | 33.6 ± 4.8 | 0.453 | ||
| ≤35 | 31 | (55.4) | 21 | (61.8) | 0.551 |
| >35 | 25 | (44.6) | 13 | (38.2) | – |
| Pre-pregnancy BMI (kg/m2) | 21.6 ± 4.0 | 21.6 ± 2.9 | 0.945 | ||
| ≤24.5 | 49 | (87.5) | 31 | (91.2) | 0.737 |
| >24.5 | 7 | (12.5) | 3 | (8.8) | – |
| Infertility treatment | |||||
| No | 33 | (58.9) | 27 | (79.4) | 0.046 |
| Yes | 23 | (41.1) | 7 | (20.6) | – |
| Past history | |||||
| No | 34 | (60.7) | 25 | (73.5) | 0.215 |
| Yes | 22 | (39.3) | 9 | (26.5) | – |
| Thyroid disease | 8 | – | 2 | – | – |
| Gynecological disease | 5 | – | 0 | – | – |
| Hyperlipidemia | 2 | – | 0 | – | – |
| Atopic dermatitis | 1 | – | 6 | – | – |
| Other | 6 | – | 1 | – | – |
| Employment | |||||
| Maternity leave/No | 17 | (30.4) | 11 | (32.4) | 0.843 |
| Yes | 39 | (69.6) | 23 | (67.6) | – |
| Exercise habit | |||||
| No | 32 | (57.1) | 18 | (52.9) | 0.004 |
| Stopped | 24 | (42.9) | 10 | (29.4) | – |
| Yes | 0 | (0.0) | 6 | (17.6) | – |
| Parameter 1 | Intervention (n = 47) | Control (n = 33) | t-Value | p-Value | ||
|---|---|---|---|---|---|---|
| Mode of delivery | ||||||
| Vaginal delivery | 37 | (78.7) | 25 | (75.8) | – | 0.754 |
| Cesarean section | 10 | (21.3) | 8 | (24.2) | – | – |
| Breech position | 4 | – | 1 | – | – | – |
| Prior uterine surgery | 4 | – | 0 | – | – | – |
| Anomaly of rotation | 2 | – | 2 | – | – | – |
| Non-reassuring fetal status | 0 | – | 1 | – | – | – |
| Unknown | 0 | – | 4 | – | – | – |
| Hospitalization of an infant | ||||||
| No | 44 | (93.6) | 32 | (37.0) | – | 0.639 |
| Yes | 3 | (6.4) | 1 | (3.0) | – | – |
| Neonatal respiratory disorder | 3 | – | 0 | – | – | – |
| Physiologic hyperbilirubinemia | 1 | – | 0 | – | – | – |
| Pneumothorax | 0 | – | 1 | – | – | – |
| Gestational age at delivery (weeks) | 39.3 ± 1.2 | 40.0 ± 1.0 | −2.92 | 0.004 | ||
| Birth weight (g) | 3026.2 ± 377.2 | 3189.2 ± 312.1 | −2.04 | 0.045 | ||
| Total labor time (minutes) | 649.7 ± 431.8 | 818.2 ± 619.0 | −1.26 | 0.211 | ||
| Intrapartum blood loss (mL) | 594.6 ± 293.4 | 759.7 ± 549.0 | −1.46 | 0.153 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kawajiri, M.; Nakamura, Y.; Yoshida, M.; Takeishi, Y.; Masaki, A.; Iwasaki, Y.; Sato, S.; Kodera, Y.; Chiba, K.; Yoshizawa, T. Acceptability and Feasibility of a Sedentary Behavior Reduction Program during Pregnancy: A Semi-Experimental Study. Healthcare 2020, 8, 439. https://doi.org/10.3390/healthcare8040439
Kawajiri M, Nakamura Y, Yoshida M, Takeishi Y, Masaki A, Iwasaki Y, Sato S, Kodera Y, Chiba K, Yoshizawa T. Acceptability and Feasibility of a Sedentary Behavior Reduction Program during Pregnancy: A Semi-Experimental Study. Healthcare. 2020; 8(4):439. https://doi.org/10.3390/healthcare8040439
Chicago/Turabian StyleKawajiri, Maiko, Yasuka Nakamura, Mikako Yoshida, Yoko Takeishi, Ai Masaki, Yuki Iwasaki, Satomi Sato, Yuri Kodera, Kazumi Chiba, and Toyoko Yoshizawa. 2020. "Acceptability and Feasibility of a Sedentary Behavior Reduction Program during Pregnancy: A Semi-Experimental Study" Healthcare 8, no. 4: 439. https://doi.org/10.3390/healthcare8040439
APA StyleKawajiri, M., Nakamura, Y., Yoshida, M., Takeishi, Y., Masaki, A., Iwasaki, Y., Sato, S., Kodera, Y., Chiba, K., & Yoshizawa, T. (2020). Acceptability and Feasibility of a Sedentary Behavior Reduction Program during Pregnancy: A Semi-Experimental Study. Healthcare, 8(4), 439. https://doi.org/10.3390/healthcare8040439





