Benefits of Multiple-Intervention Pulmonary Rehabilitation to Older Adults with High-Risk Multimorbidity after Coronary Artery Bypass Grafting
Abstract
1. Introduction
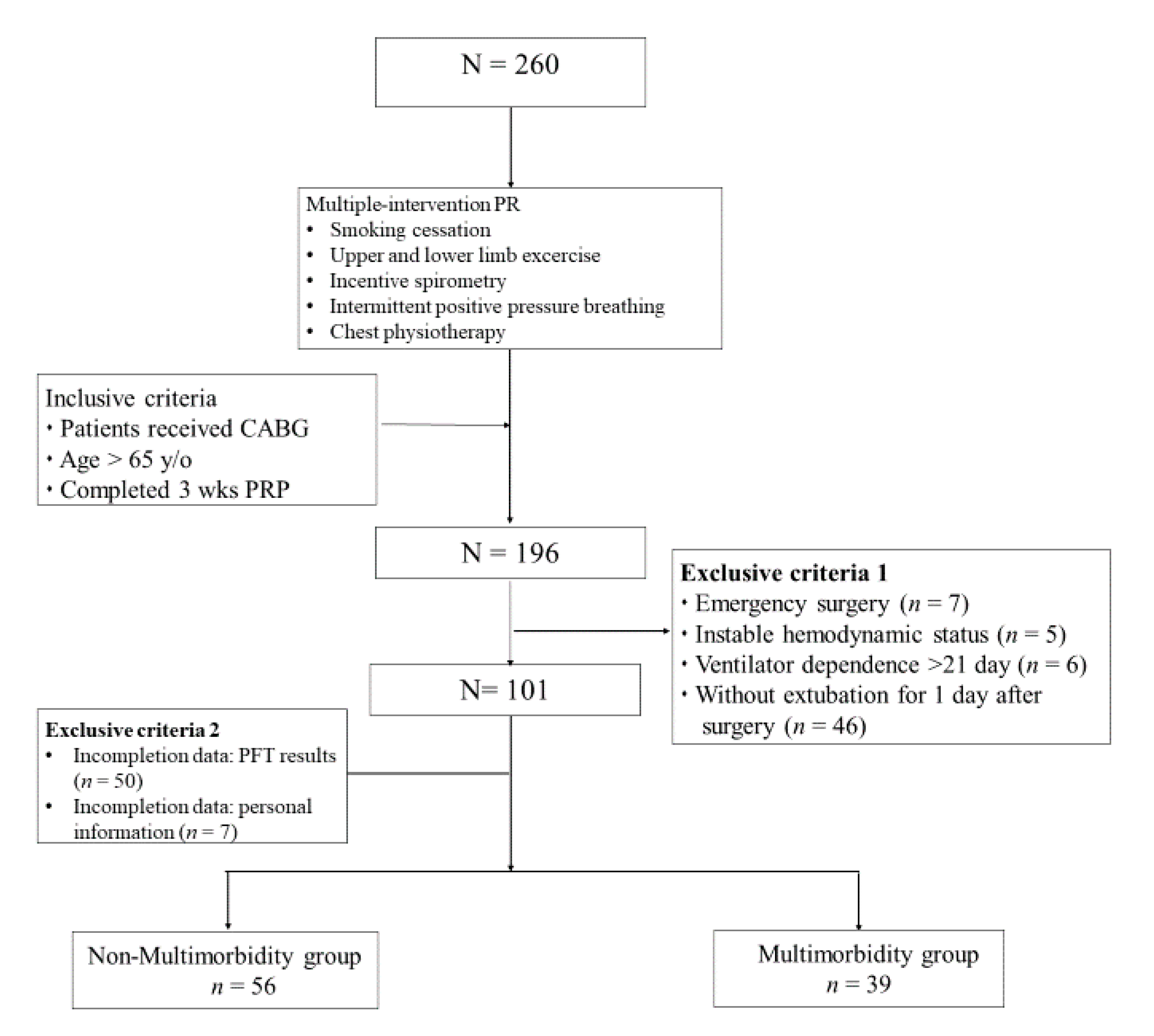
2. Materials and Methods
2.1. Study Design and Population
2.2. Multiple-Intervention Pulmonary Rehabilitation Program
2.3. Data Collection
2.4. Statistical Analyses
3. Results
3.1. Patients’ Characteristics and Complications
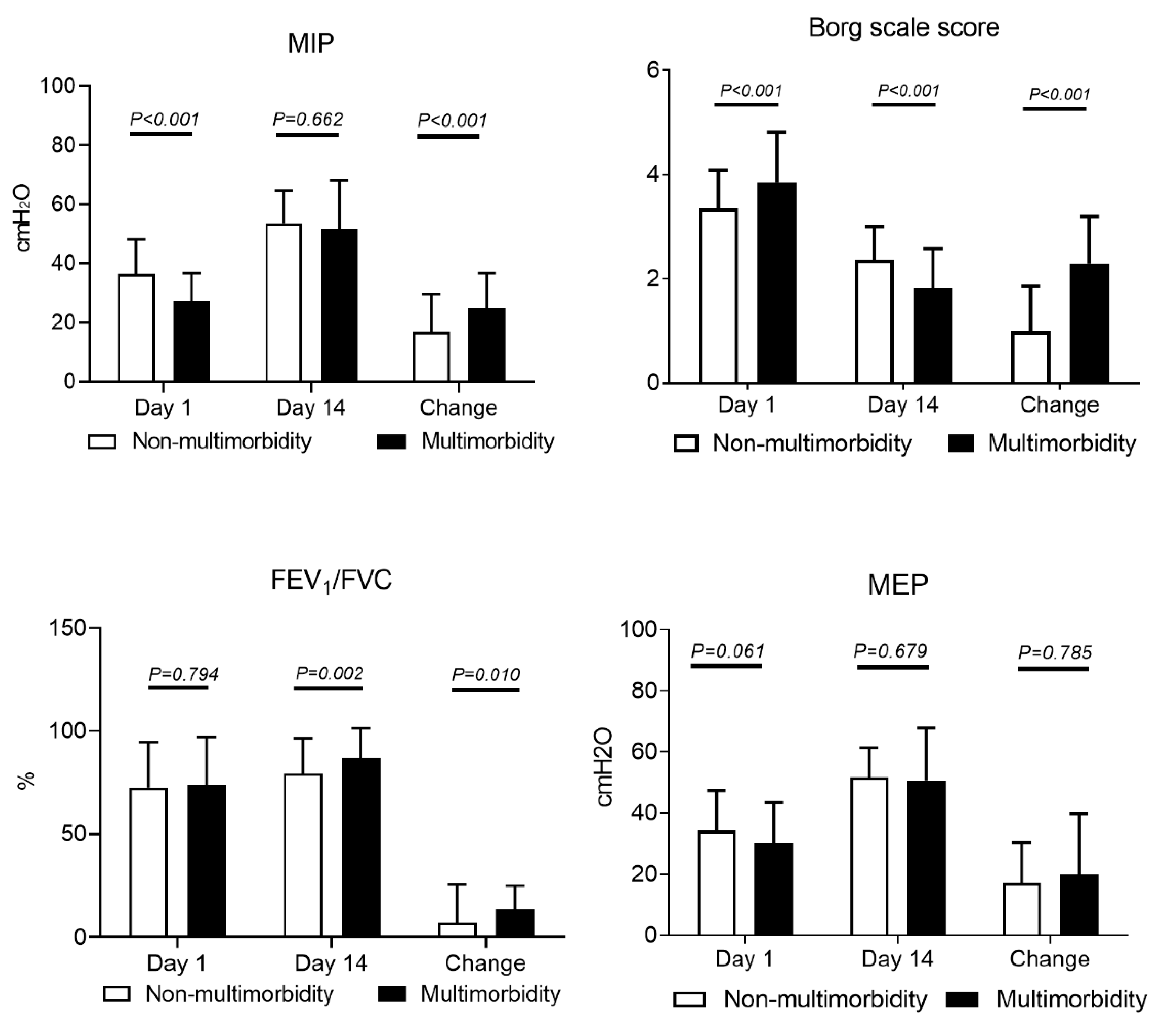
3.2. Improvement of Respiratory Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Drews, T.; Pasic, M.; Buz, S.; Unbehaun, A.; Dreysse, S.; Kukucka, M.; Mladenow, A.; Hetzer, R. Transapical aortic valve implantation after previous heart surgery. Eur. J. Cardiothorac. Surg. 2011, 39, 625–630. [Google Scholar] [CrossRef] [PubMed]
- Shad, B.; Ashouri, A.; Hasandokht, T.; Rajati, F.; Salari, A.; Naghshbandi, M.; Mirbolouk, F. Effect of multimorbidity on quality of life in adult with cardiovascular disease: A cross-sectional study. Health Qual. Life Outcomes 2017, 15, 240. [Google Scholar] [CrossRef] [PubMed]
- McKellar, S.H.; Brown, M.L.; Frye, R.L.; Schaff, H.V.; Sundt, T.M. Comparison of coronary revascularization procedures in octogenarians: A systematic review and meta-analysis. Nat. Clin. Pract. Cardiovasc. Med. 2008, 5, 738–746. [Google Scholar] [CrossRef] [PubMed]
- Northrup, W.F.; Emery, R.W.; Nicoloff, D.M.; Lillehei, T.J.; Holter, A.R.; Blake, D.P. Opposite trends in coronary artery and valve surgery in a large multisurgeon practice, 1979–1999. Ann. Thorac. Surg. 2004, 77, 488–495. [Google Scholar] [CrossRef]
- Wang, J.; Yu, W.; Zhao, D.; Liu, N.; Yu, Y. In-hospital and long-term mortality in 35,173 Chinese patients undergoing coronary artery bypass grafting in Beijing: Impact of sex, age, myocardial infarction, and cardiopulmonary bypass. J. Cardiothorac. Vasc. Anesth. 2017, 31, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Sharma, G.; Goodwin, J. Effect of aging on respiratory system physiology and immunology. Clin. Interv. Aging 2006, 1, 253–260. [Google Scholar] [CrossRef]
- Mangano, C.M.; Diamondstone, L.S.; Ramsay, J.G.; Aggarwal, A.; Herskowitz, A.; Mangano, D.T. Renal dysfunction after myocardial revascularization: Risk factors, adverse outcomes, and hospital resource utilization. The Multicenter Study of Perioperative Ischemia Research Group. Ann. Intern. Med. 1998, 128, 194–203. [Google Scholar] [CrossRef]
- Morricone, L.; Ranucci, M.; Denti, S.; Cazzaniga, A.; Isgro, G.; Enrini, R.; Caviezel, F. Diabetes and complications after cardiac surgery: Comparison with a non-diabetic population. Acta Diabetol. 1999, 36, 77–84. [Google Scholar] [CrossRef]
- Natarajan, A.; Samadian, S.; Clark, S. Coronary artery bypass surgery in elderly people. Postgrad. Med. J. 2007, 83, 154–158. [Google Scholar] [CrossRef]
- Smetana, G.W.; Lawrence, V.A.; Cornell, J.E. Preoperative pulmonary risk stratification for noncardiothoracic surgery: Systematic review for the American College of Physicians. Ann. Intern. Med. 2006, 144, 581–595. [Google Scholar] [CrossRef]
- Manapunsopee, S.; Thanakiatpinyo, T.; Wongkornrat, W.; Chuaychoo, B.; Thirapatarapong, W. Effectiveness of incentive spirometry on inspiratory muscle strength after coronary artery bypass graft surgery. Heart Lung Circ. 2019, 29, 1180–1186. [Google Scholar] [CrossRef]
- Spruit, M.A.; Singh, S.J.; Garvey, C.; ZuWallack, R.; Nici, L.; Rochester, C.; Hill, K.; Holland, A.E.; Lareau, S.C.; Man, W.D.C.; et al. An official American Thoracic Society/European Respiratory Society statement: Key concepts and advances in pulmonary rehabilitation. Am. J. Respir. Crit. Care Med. 2013, 188, e13–e64. [Google Scholar] [CrossRef]
- Türk, Y.; van Huisstede, A.; Hiemstra, P.S.; Taube, C.; Braunstahl, G.J. Pre-surgical pulmonary rehabilitation in asthma patients undergoing bariatric surgery. Obes. Surg. 2017, 27, 3055–3060. [Google Scholar] [CrossRef] [PubMed]
- Laurent, H.; Galvaing, G.; Thivat, E.; Coudeyre, E.; Aubreton, S.; Richard, R.; Kwiatkowski, F.; Costes, F.; Filaire, M. Effect of an intensive 3-week preoperative home rehabilitation programme in patients with COPD eligible for lung cancer surgery: A multicentre randomised controlled trial. BMJ Open 2017, 7, e017307. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chen, J.O.; Liu, J.F.; Liu, Y.Q.; Chen, Y.M.; Tu, M.L.; Yu, H.R.; Lin, M.C.; Lin, C.C.; Liu, S.F. Effectiveness of a perioperative pulmonary rehabilitation program following coronary artery bypass graft surgery in patients with and without COPD. Int. J. Chron. Obstruct. Pulmon. Dis. 2018, 13, 1591–1597. [Google Scholar] [CrossRef] [PubMed]
- Snowdon, D.; Haines, T.P.; Skinner, E.H. Preoperative intervention reduces postoperative pulmonary complications but not length of stay in cardiac surgical patients: A systematic review. J. Physiother. 2014, 60, 66–77. [Google Scholar] [CrossRef] [PubMed]
- Dronkers, J.; Veldman, A.; Hoberg, E.; van der Waal, C.; van Meeteren, N. Prevention of pulmonary complications after upper abdominal surgery by preoperative intensive inspiratory muscle training: A randomized controlled pilot study. Clin. Rehabil. 2008, 22, 134–142. [Google Scholar] [CrossRef]
- Hulzebos, E.H.; Smit, Y.; Helders, P.P.; van Meeteren, N.L. Preoperative physical therapy for elective cardiac surgery patients. Cochrane Database Syst. Rev. 2012, 11, Cd010118. [Google Scholar]
- Rezaianzadeh, A.; Maghsoudi, B.; Tabatabaee, H.; Keshavarzi, S.; Bagheri, Z.; Sajedianfard, J.; Gerami, H.; Rasouli, J. Factors associated with extubation time in coronary artery bypass grafting patients. Peer J. 2015, 3, e1414. [Google Scholar] [CrossRef]
- Bausewein, C.; Farquhar, M.; Booth, S.; Gysels, M.; Higginson, I.J. Measurement of breathlessness in advanced disease: A systematic review. Respir. Med. 2007, 101, 399–410. [Google Scholar] [CrossRef]
- Li, C.; Yang, W.H.; Zhou, J.; Wu, Y.; Li, Y.S.; Wen, S.H.; Huang, W.Q.; Liu, K.X. Risk factors for predicting postoperative complications after open infrarenal abdominal aortic aneurysm repair: Results from a single vascular center in China. J. Clin. Anesth. 2013, 25, 371–378. [Google Scholar] [CrossRef] [PubMed]
- Matheus, G.B.; Dragosavac, D.; Trevisan, P.; Costa, C.E.; Lopes, M.M.; Ribeiro, G.C. Inspiratory muscle training improves tidal volume and vital capacity after CABG surgery. Rev. Bras. Cir. Cardiovasc. 2012, 27, 362–369. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fagevik Olsén, M.; Hahn, I.; Nordgren, S.; Lönroth, H.; Lundholm, K. Randomized controlled trial of prophylactic chest physiotherapy in major abdominal surgery. Br. J. Surg. 1997, 84, 1535–1538. [Google Scholar] [CrossRef] [PubMed]
- Suematsu, Y.; Sato, H.; Ohtsuka, T.; Kotsuka, Y.; Araki, S.; Takamoto, S. Predictive risk factors for delayed extubation in patients undergoing coronary artery bypass grafting. Heart Vessels 2000, 15, 214–220. [Google Scholar] [CrossRef]
- Bujar-Misztal, M.; Chciałowski, A. Influence of proprioceptive neuromuscular facilitation on lung function in patients after coronary artery bypass graft surgery. Adv. Exp. Med. Biol. 2018, 1116, 11–17. [Google Scholar]
- McAlister, F.A.; Bertsch, K.; Man, J.; Bradley, J.; Jacka, M. Incidence of and risk factors for pulmonary complications after nonthoracic surgery. Am. J. Respir. Crit. Care Med. 2005, 171, 514–517. [Google Scholar] [CrossRef]
- Hulzebos, E.H.; Helders, P.J.; Favié, N.J.; De Bie, R.A.; de la Riviere, A.B.; Van Meeteren, N.L. Preoperative intensive inspiratory muscle training to prevent postoperative pulmonary complications in high-risk patients undergoing CABG surgery: A randomized clinical trial. JAMA 2006, 296, 1851–1857. [Google Scholar] [CrossRef]
- Katsura, M.; Kuriyama, A.; Takeshima, T.; Fukuhara, S.; Furukawa, T.A. Preoperative inspiratory muscle training for postoperative pulmonary complications in adults undergoing cardiac and major abdominal surgery. Cochrane Database Syst. Rev. 2015, 10, Cd010356. [Google Scholar] [CrossRef]
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef]
- Sullivan, G.M.; Feinn, R. Using effect size-or why the p value is not enough. J. Grad. Med. Educ. 2012, 4, 279–282. [Google Scholar] [CrossRef]
| Characteristics | Non-Multimorbidity Group (n = 56) | Multimorbidity Group (n = 39) | P-Value |
|---|---|---|---|
| Age (years) | 72.20 ± 7.96 | 69.18 ± 3.62 | 0.056 a |
| 65–74 | 40 (71.4%) | 34 (87.2%) | |
| ≥75 | 16 (28.6%) | 5 (12.8%) | |
| Sex | |||
| Male | 40 (71.4%) | 31 (79.5%) | 0.260 a |
| Female | 16 (28.6%) | 8 (20.5%) | |
| Body mass index (kg/m2) | |||
| ≤24 | 23 (41.1%) | 19 (48.7%) | 0.406 a |
| ≥25 | 33 (58.9%) | 20 (51.3%) | |
| Smoking index (pack-year) | 10.00 ± 20.53 | 14.36 ± 33.54 | 0.976 b |
| Coronary artery disease | 0.286 a | ||
| ≤Two-vessel CAD | 22 (39.28%) | 18 (47.4%) | |
| ≥Three-vessel CAD | 34 (60.7%) | 21 (52.6%) | |
| Surgery type | 0.572 a | ||
| Isolated CABG | 42 (75.0%) | 26 (68.4%) | |
| CABG + aortic valve | 5 (8.9%) | 4 (10.5%) | |
| CABG + mitral valve | 6 (10.7%) | 3 (7.9%) | |
| CABG + ventricular Septal repair | 3 (5.4%) | 5 (13.2%) | |
| ASA surgical risk classification | 0.007 a | ||
| 3 | 51 (91.1%) | 27 (69.2%) | |
| 4 | 5 (8.9%) | 12 (30.8%) | |
| DM | <0.001 a | ||
| No | 56 (100.0%) | 16 (41.0%) | |
| Yes | 0 (0%) | 23 (59.0%) | |
| Hypertension | 0.002 a | ||
| No | 35 (62.5%) | 12 (30.8%) | |
| Yes | 21 (37.5%) | 27 (69.2%) | |
| Chronic kidney disease | <0.001 a | ||
| No | 56 (100.0%) | 27 (69.2%) | |
| Yes | 0 (0%) | 12 (30.8%) | |
| Cerebral vascular accident | <0.001 a | ||
| No | 56 (100.0%) | 31 (79.5%) | |
| Yes | 0 (0%) | 8 (20.5%) | |
| COPD | 0.378 a | ||
| No | 22 (46.4%) | 16 (41.0%) | |
| Yes | 30 (53.6%) | 23 (59.0%) |
| Outcomes | Non-Multimorbidity Group (n = 56) | Multimorbidity Group (n = 39) | P-Value |
|---|---|---|---|
| ICU stay (days) | 3.13 ± 2.48 | 4.98 ± 1.9 | 0.003 |
| Hospital stay (days) | 19.73 ± 6.10 | 27.18 ± 11.2 | <0.001 |
| Oxygen use (days) | 0.080 | ||
| <7 days | 48 (85.7%) | 28 (71.8%) | |
| >7 days | 8 (14.3%) | 11 (28.2%) | |
| Pulmonary complications | |||
| Respiratory failure | 0 (0%) | 2 (5.1%) | 0.166 |
| Atelectasis | 15 (26.8%) | 17 (43.6%) | 0.069 |
| Pneumonia | 5 (8.9%) | 4 (10.3%) | 0.548 |
| Subcutaneous emphysema | 1 (1.8%) | 4 (10.3%) | 0.089 |
| Pneumothorax | 2 (3.6%) | 1 (2.6%) | 0.665 |
| Other complications | |||
| Urinary tract infection | 15 (26.8%) | 15 (38.5%) | 0.164 |
| Wound infection | 3 (5.4%) | 4 (10.3%) | 0.305 |
| Re-operation | 3 (5.4%) | 2 (5.1%) | 0.332 |
| Bacteremia | 1 (1.8%) | 0 (0%) | 0.589 |
| Parameters | Non-Multimorbidity Group (n = 56) | Multimorbidity Group (n = 39) | ||||
|---|---|---|---|---|---|---|
| Age (year) | 65–74 | >75 | P-Value | 65–74 | >75 | P-Value |
| MIP | 15.9 ± 13.6 | 17.8 ± 12.0 | 0.569 | 25.5 ± 9.3 | 24.7 ± 13.9 | 0.915 |
| Borg | −0.8 ± 1.0 | −1.2 ± 0.65 | 0.151 | −1.6 ± 0.8 | −2.4 ± 0.8 | 0.006 |
| FEV1/FVC (%) | 8.2 ± 19.9 | 5.9 ± 17.7 | 0.666 | 12.5 ± 12.2 | 14.2 ± 11.3 | 0.665 |
| Gender | Male | Female | Male | Female | ||
| MIP | 16.2 ± 12.6 | 18.6 ± 13.4 | 0.500 | 24.4 ± 11.3 | 27.2 ± 12.8 | 0.564 |
| Borg | −0.75 ± 0.9 | −1.5 ± 0.5 | 0.001 | −1.8 ± 0.8 | −3.0 ± 0 | 0.001 |
| FEV1/FVC (%) | 14.0 ± 16.3 | 8.7 ± 13.9 | 0.001 | 12.3 ± 12.2 | 17.5 ± 7.9 | 0.267 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, J.-F.; Lee, H.-M.; Chen, J.-O.; Fang, T.-P.; Chen, Y.-M.; Lo, C.-M.; Liu, S.-F.; Lin, H.-L. Benefits of Multiple-Intervention Pulmonary Rehabilitation to Older Adults with High-Risk Multimorbidity after Coronary Artery Bypass Grafting. Healthcare 2020, 8, 368. https://doi.org/10.3390/healthcare8040368
Liu J-F, Lee H-M, Chen J-O, Fang T-P, Chen Y-M, Lo C-M, Liu S-F, Lin H-L. Benefits of Multiple-Intervention Pulmonary Rehabilitation to Older Adults with High-Risk Multimorbidity after Coronary Artery Bypass Grafting. Healthcare. 2020; 8(4):368. https://doi.org/10.3390/healthcare8040368
Chicago/Turabian StyleLiu, Jui-Fang, Hsiu-Mei Lee, Jui-O Chen, Tien-Pei Fang, Yu-Mu Chen, Chien-Ming Lo, Shih-Feng Liu, and Hui-Ling Lin. 2020. "Benefits of Multiple-Intervention Pulmonary Rehabilitation to Older Adults with High-Risk Multimorbidity after Coronary Artery Bypass Grafting" Healthcare 8, no. 4: 368. https://doi.org/10.3390/healthcare8040368
APA StyleLiu, J.-F., Lee, H.-M., Chen, J.-O., Fang, T.-P., Chen, Y.-M., Lo, C.-M., Liu, S.-F., & Lin, H.-L. (2020). Benefits of Multiple-Intervention Pulmonary Rehabilitation to Older Adults with High-Risk Multimorbidity after Coronary Artery Bypass Grafting. Healthcare, 8(4), 368. https://doi.org/10.3390/healthcare8040368





