Mobile X-ray Outside the Hospital vs. X-ray at the Hospital Challenges Exposed in an Explorative RCT Study
Abstract
1. Introduction
Aim
2. Methods
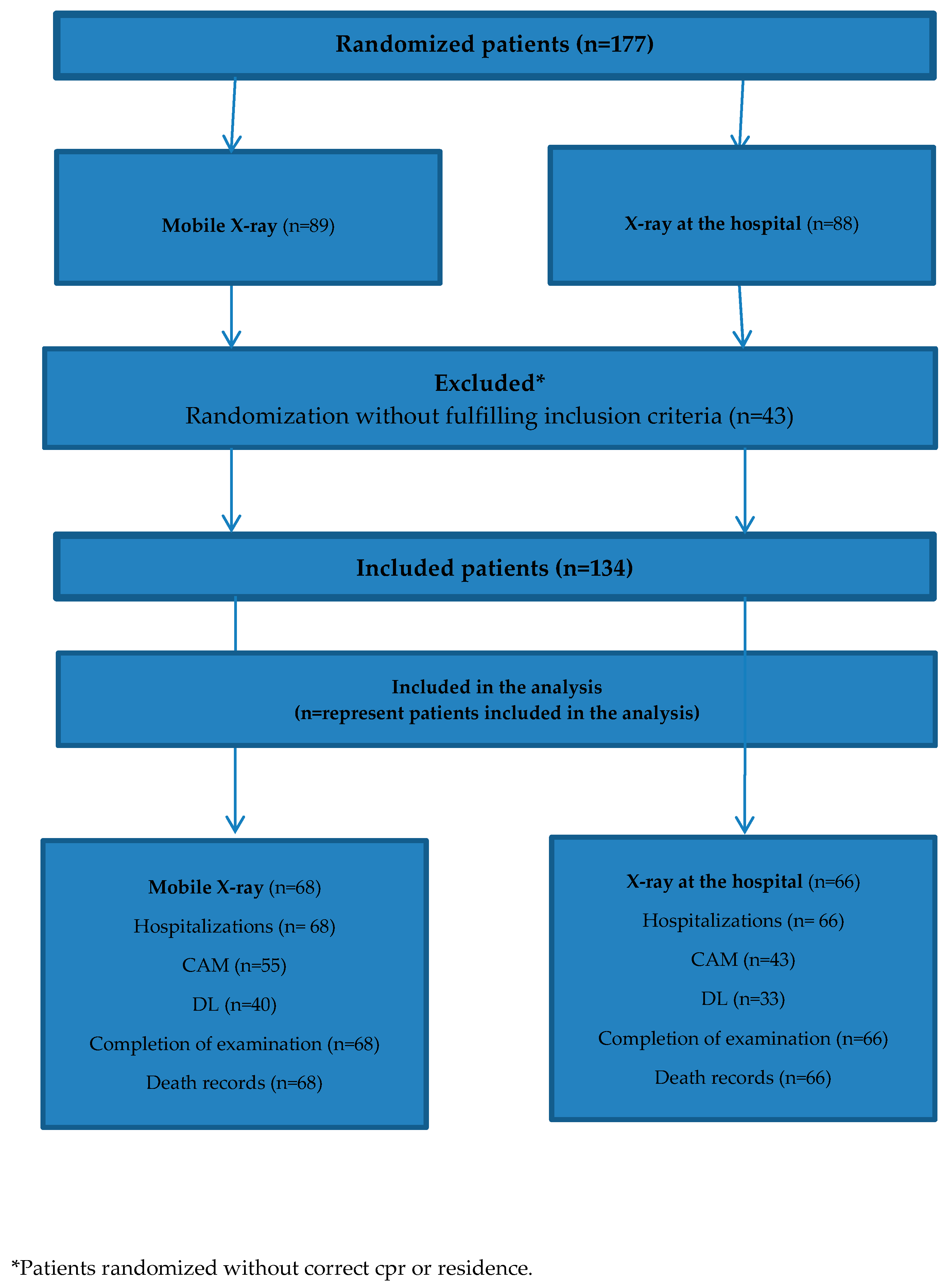
2.1. Study Design
2.2. Study Population Included
- Referred to a mobile X-ray examination.
- Living in nursing homes and homes for the elderly in Aarhus municipality.
2.3. Outcome Measures
2.3.1. Baseline
2.3.2. Primary Outcome
2.3.3. Secondary Outcomes
2.4. Randomization and Blinding
2.4.1. Intervention
2.4.2. Control
2.5. Statistical Analysis
2.6. Inclusion of Participants
- Are you satisfied with mobile X-ray?
- Do you know the quality of mobile X-ray?
- Do you understand why we have to randomize patients in the study of mobile X-ray?
- Why would you withdraw the referral of a patient?
- Could a patient be too fragile to be examined at the hospital?
2.7. Ethics Approval and Consent to Participate
3. Results
3.1. Baseline Characteristics
3.2. Primary Outcome
3.3. Secondary Outcomes
3.4. Challenges
4. Discussion
4.1. Challenges and Future Studies
4.2. Study Population and Outcome Measures
4.3. Referring Doctors
4.4. Missing Values
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Availability of Data and Material
References
- Graverholt, B.; Forsetlund, L.; Jamtvedt, G. Reducing hospital admissions from nursing homes: A systematic review. BMC Health Serv. Res. 2014, 14, 36. [Google Scholar] [CrossRef] [PubMed]
- Graverholt, B.; Riise, T.; Jamtvedt, G.; Husebo, B.S.; Nortvedt, M.W. Acute hospital admissions from nursing homes: Predictors of unwarranted variation? Scand. J. Public Health 2013, 41, 359–365. [Google Scholar] [CrossRef]
- Graverholt, B.; Riise, T.; Jamtvedt, G.; Ranhoff, A.H.; Kruger, K.; Nortvedt, M.W. Acute hospital admissions among nursing home residents: A population-based observational study. BMC Health Serv. Res. 2011, 11, 126. [Google Scholar] [CrossRef]
- Kihlgren, A.L.; Nilsson, M.; Skovdahl, K.; Palmblad, B.; Wimo, A. Older patients awaiting emergency department treatment. Scand. J. Caring Sci. 2004, 18, 169–176. [Google Scholar] [CrossRef]
- Aldridge, R.W.; Hayward, A.C.; Hemming, S.; Possas, L.; Ferenando, G.; Garber, E.; Lipman, M.; McHugh, T.D.; Story, A. Effectiveness of peer educators on the uptake of mobile X-ray tuberculosis screening at homeless hostels: A cluster randomised controlled trial. BMJ Open 2015, 5, e008050. [Google Scholar] [CrossRef]
- Datta, B.; Hazarika, A.; Shewade, H.D.; Ayyagari, K.; Kumar, A.M. Digital chest X-ray through a mobile van: Public private partnership to detect sputum negative pulmonary TB. BMC Res. Notes 2017, 10, 96. [Google Scholar] [CrossRef]
- Dozet, A.; Ivarsson, B.; Eklund, K.; Klefsgard, R.; Geijer, M. Radiography on wheels arrives to nursing homes—An economic assessment of a new health care technology in southern Sweden. J. Eval. Clin. Pract. 2016, 22, 990–997. [Google Scholar] [CrossRef] [PubMed]
- Eklund, K.; Klefsgard, R.; Ivarsson, B.; Geijer, M. Positive experience of a mobile radiography service in nursing homes. Gerontology 2012, 58, 107–111. [Google Scholar] [CrossRef]
- Kjelle, E.; Kleven, L.; Olerud, H.M.; Melberg, H.O. Cost analysis of mobile radiography services for nursing home residents in Southeast Norway. J. Eval. Clin. Pract. 2019, 25, 275–281. [Google Scholar] [CrossRef]
- Kumar, A.; Khattar, P.; Tiwari, V.K.; Shivdasani, J.P.; Dhar, N.; Nandan, D. An assessment of functioning of mobile medical units in Jharkhand. Indian J. Public Health 2009, 53, 157–160. [Google Scholar] [CrossRef] [PubMed]
- Montalto, M.; Shay, S.; Le, A. Evaluation of a mobile X-ray service for elderly residents of residential aged care facilities. Aust. Health Rev. 2015, 39, 517–521. [Google Scholar] [CrossRef] [PubMed]
- Morishita, F.; Garfin, A.M.; Lew, W.; Oh, K.H.; Yadav, R.P.; Reston, J.C.; Infante, L.L.; Acala, M.R.C.; Palanca, D.L.; Kim, H.J.; et al. Bringing state-of-the-art diagnostics to vulnerable populations: The use of a mobile screening unit in active case finding for tuberculosis in Palawan, the Philippines. PLoS ONE 2017, 12, e0171310. [Google Scholar] [CrossRef]
- Ricauda, N.A.; Tibaldi, V.; Bertone, P.; Quagliotti, E.; Tizzani, A.; Zanocchi, M.; Isaia, G.C.; Grosso, M.; Cammarota, T.; Davini, O. The RAD-HOME project: A pilot study of home delivery of radiology services. Arch. Intern. Med. 2011, 171, 1678–1680. [Google Scholar] [CrossRef] [PubMed]
- Story, A.; Aldridge, R.W.; Abubakar, I.; Stagg, H.R.; Lipman, M.; Watson, J.M.; Hayward, A.C. Active case finding for pulmonary tuberculosis using mobile digital chest radiography: An observational study. Int. J. Tuberc. Lung Dis. 2012, 16, 1461–1467. [Google Scholar] [CrossRef] [PubMed]
- Thingnes, E.; Stalsberg, R. Kvalitative aspekter ved innføring av mobile røntgentjenester til sykehjem. En studie av tre faggruppers forventninger [Qualitative aspects on establishing mobile radiography services for nursing homes. A study of three professional groups expectations]. Nordisk Tidsskrift Helseforskning 2010, 6, 14–28. [Google Scholar] [CrossRef]
- Vigeland, E.; Bohm, R.E.; Rostad, A.; Lysdahl, K.B. Mobile X-ray service for nursing homes. J. Nor. Med. Assoc. 2017, 137, 198–202. [Google Scholar]
- Loeb, M.; Carusone, S.C.; Goeree, R.; Walter, S.D.; Brazil, K.; Krueger, P.; Simor, A.; Moss, L.; Marrie, T. Effect of a clinical pathway to reduce hospitalizations in nursing home residents with pneumonia: A randomized controlled trial. JAMA 2006, 295, 2503–2510. [Google Scholar] [CrossRef]
- Loeb, M.B.; Carusone, S.B.; Marrie, T.J.; Brazil, K.; Krueger, P.; Lohfeld, L.; Simor, A.; Moss, L.; Marrie, T. Interobserver reliability of radiologists’ interpretations of mobile chest radiographs for nursing home-acquired pneumonia. J. Am. Med. Dir. Assoc. 2006, 7, 416–419. [Google Scholar] [CrossRef]
- Ottawa, O.N. Portable versus Fixed X-ray Equipment: A Review of the Clinical Effectiveness, Costeffectiveness, and Guidelines. 2016. Available online: https://www.ncbi.nlm.nih.gov/books/NBK350586/ (accessed on 29 April 2020).
- McClester Brown, M.; Sloane, P.D.; Kistler, C.E.; Reed, D.; Ward, K.; Weber, D.; Zimmerman, S. Evaluation and Management of the Nursing Home Resident with Respiratory Symptoms and an Equivocal Chest X-ray Report. J. Am. Med. Dir. Assoc. 2016, 17, 1164-e1. [Google Scholar] [CrossRef]
- Toppenberg, M.D.; Kjeldsen, A.S. Evaluation of the Pilot Project Mobile X-ray at the Department of Radiology. Aarhus Univ. Hosp. 2016, 30, 208–220. [Google Scholar]
- Toppenberg, M.; Christiansen, T.; Rasmussen, F.; Nielsen, C.; Damsgaard, E. Mobile X-ray outside the Hospital: A review. BMC Health Serv. Res. 2020. [Google Scholar] [CrossRef]
- Inouye, S.K.; van Dyck, C.H.; Alessi, C.A.; Balkin, S.; Siegal, A.P.; Horwitz, R.I. Clarifying confusion: The confusion assessment method. A new method for detection of delirium. Ann. Intern. Med. 1990, 113, 941–948. [Google Scholar] [CrossRef] [PubMed]
- Gregersen, M.; Jordansen, M.M.; Gerritsen, D.L. Overall Quality of Life (OQoL) questionnaire in frail elderly: A study of reproducibility and responsiveness of the Depression List (DL). Arch. Gerontol. Geriatr. 2015, 60, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Gerritsen, D.L.; Steverink, N.; Ooms, M.E.; Ribbe, M.W. Finding a useful conceptual basis for enhancing the quality of life of nursing home residents. Qual. Life Res. 2004, 13, 611–624. [Google Scholar] [CrossRef] [PubMed]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Kirkwood, B.R.; Sterne, S.J. Essential Medical Statistics, 2nd ed.; Blackwell Science Inc.: Malden, MA, USA, 1988. [Google Scholar]
- Higgins, J.P.; White, I.R.; Wood, A.M. Imputation methods for missing outcome data in meta-analysis of clinical trials. Clin. Trials 2008, 5, 225–239. [Google Scholar] [CrossRef]
- Sheikj, J.I.; Yesavage, J.A. Geriatric Depression Scale: Recent Evidence and Development of a Shorter Version; The Hawthorne Press: New York, NY, USA, 1986; Volume 5, pp. 165–173. [Google Scholar]
- Hocking, C.; Williams, M.; Broad, J.; Baskett, J. Sensitivity of Shah, Vanclay and Cooper’s modified Barthel Index. Clin. Rehabil. 1999, 13, 141–147. [Google Scholar] [CrossRef]
- Linn, B.S.; Linn, M.W.; Gurel, L. Cumulative illness rating scale. J. Am. Geriatr. Soc. 1968, 16, 622–626. [Google Scholar] [CrossRef]
- Gerritsen, D.L.; Steverink, N.; Ooms, M.E.; de Vet, H.C.; Ribbe, M.W. Measurement of overall quality of life in nursing homes through self-report: The role of cognitive impairment. Qual. Life Res. 2007, 16, 1029–1037. [Google Scholar] [CrossRef]
| Characteristic | Group | |
|---|---|---|
| Intervention (n = 68) | Control (n = 66) | |
| Age (mean ± SD) | 81.98 (7.28) | 84.39 (9.56) |
| Gender (male) | 24 (35%) | 24 (36%) |
| Number of diagnoses (mean) | 4.40 | 4.54 |
| Polypharmacy ≥ 5 | 48 (71%) | 49 (74%) |
| Patients examined by doctor before X-ray | 60 (90%) | 56 (85%) |
| Diagnosed with dementia (yes/no) | 27 (40%) | 30 (45%) |
| BMI ≤ 21 | 40 (59%) | 34 (52%) |
| Group | ||||
|---|---|---|---|---|
| Characteristics n = Included * | Intervention (n = 68) | Control (n = 66) | Scale | Impute Value (Worst Case Scenario in the Dataset) |
| MMSE Intervention n = 39 (57%) Control n = 30 (45%) | 22.64 (p = 0.61) | 22.37 | 0–30 | 5 |
| GDS Intervention n = 39 (57%) Control n = 30 (45%) | 2.46 (p = 0.01) | 4.07 | 0–15 points | 14 |
| MBI Intervention n = 57 (84%) Control n = 55 (83%) | 57.52 (p = 0.04) | 69.88 | 0–100 | 5 |
| CIRS G Intervention n = 57 (84%) Control n = 55 (83%) | 11.46 (p = 0.51) | 12.04 | 0–30 | 28 |
| X-ray Examination | Hospitalized | ||
|---|---|---|---|
| Yes | No | Total | |
| Mobile X-ray | 8 (11.76%) | 60 | 68 |
| X-ray at the hospital | 8 (12.12%) | 58 | 66 |
| X-ray Examination (n = 16) | Mean | 25 Percentile | 50 Percentile | 75 Percentile | 90 Percentile |
|---|---|---|---|---|---|
| Mobile X-ray | 7.63 | 3.5 | 8 | 12 | 13 |
| X-ray at the hospital | 4.50 | 1 | 1 | 6 | 19 |
| Outcome Measurement | Intervention Group (n = 68) | Control Group (n = 66) | Scale | Impute Value (Worst Measured Case) |
|---|---|---|---|---|
| CAM, delirium (yes) Intervention n = 55 (81%) Control n = 43 (65%) | 0 (p = 0.26) | 1 | Yes or no Yes is worst case | Yes |
| DL (quality of life), mean Intervention n = 40 (59%) Control n = 33 (50%) | 7.61 (p = 0.05) | 5.5 | 0–30 points 30 is worst case | 19 |
| Completion of examination Intervention n= 68 (100%) Control n = 66 (100%) | 68 (p = 0.15) | 64 | Yes/no | - |
| Death (%) Intervention n = 68 (100%) Control n = 66 (100%) | 12 (p = 0.59) | 10 | Yes/no | - |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Toppenberg, M.; Christiansen, T.; Rasmussen, F.; Nielsen, C.; Damsgaard, E.M. Mobile X-ray Outside the Hospital vs. X-ray at the Hospital Challenges Exposed in an Explorative RCT Study. Healthcare 2020, 8, 118. https://doi.org/10.3390/healthcare8020118
Toppenberg M, Christiansen T, Rasmussen F, Nielsen C, Damsgaard EM. Mobile X-ray Outside the Hospital vs. X-ray at the Hospital Challenges Exposed in an Explorative RCT Study. Healthcare. 2020; 8(2):118. https://doi.org/10.3390/healthcare8020118
Chicago/Turabian StyleToppenberg, Maria, Thomas Christiansen, Finn Rasmussen, Camilla Nielsen, and Else Marie Damsgaard. 2020. "Mobile X-ray Outside the Hospital vs. X-ray at the Hospital Challenges Exposed in an Explorative RCT Study" Healthcare 8, no. 2: 118. https://doi.org/10.3390/healthcare8020118
APA StyleToppenberg, M., Christiansen, T., Rasmussen, F., Nielsen, C., & Damsgaard, E. M. (2020). Mobile X-ray Outside the Hospital vs. X-ray at the Hospital Challenges Exposed in an Explorative RCT Study. Healthcare, 8(2), 118. https://doi.org/10.3390/healthcare8020118




