Effective Risk Communication for Public Health Emergency: Reflection on the COVID-19 (2019-nCoV) Outbreak in Wuhan, China
Abstract
1. Introduction
2. Method
2.1. Data Source
2.2. Message-Centered Approach
3. Case Description: Outbreak Management of COVID-19 in Wuhan, China
3.1. Background
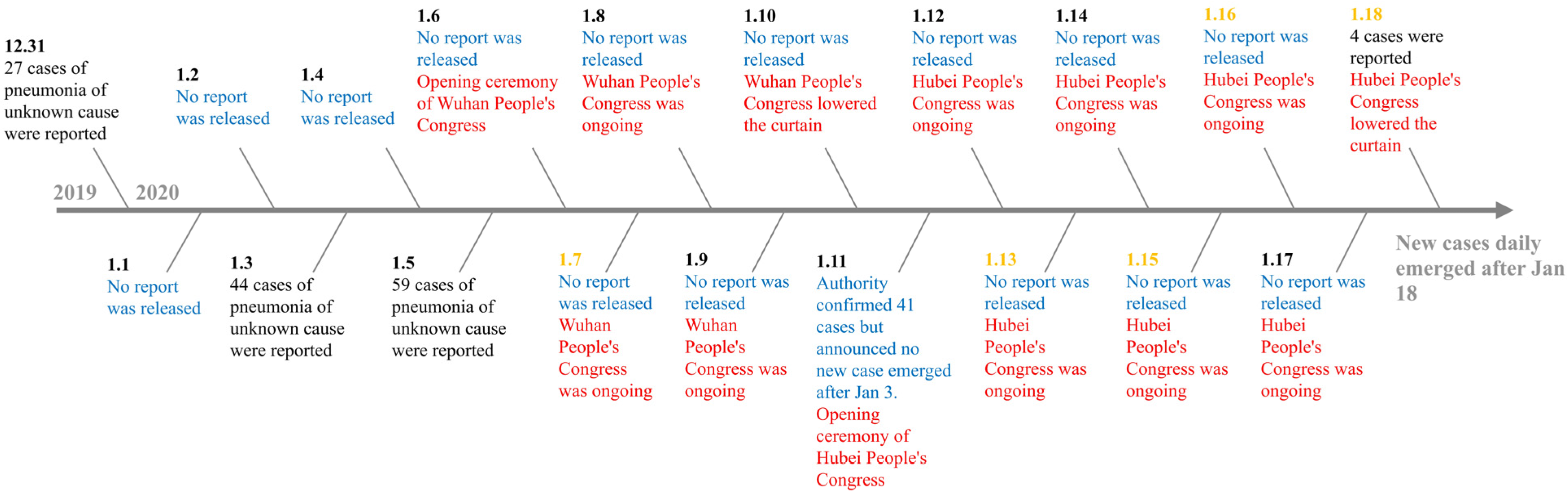
3.2. Risk Communication Timeline of COVID-19 Outbreak Management
4. Analysis on Risk Communication in COVID-19 Management: A Message-Centered Approach
4.1. Infuse Risk Communication into Policy Decisions
4.2. Present Risk Messages with Honesty
4.3. Account for the Uncertainty Inherent in Risk
4.4. Acknowledge Diverse Levels of Risk Tolerance
5. Principles for Effective Risk Communication: Lessons from Wuhan
5.1. Accessibility and Openness of Risk Information
5.2. Communicate Early and Often About Risk
5.3. Strategic Method for Communicating Uncertainty
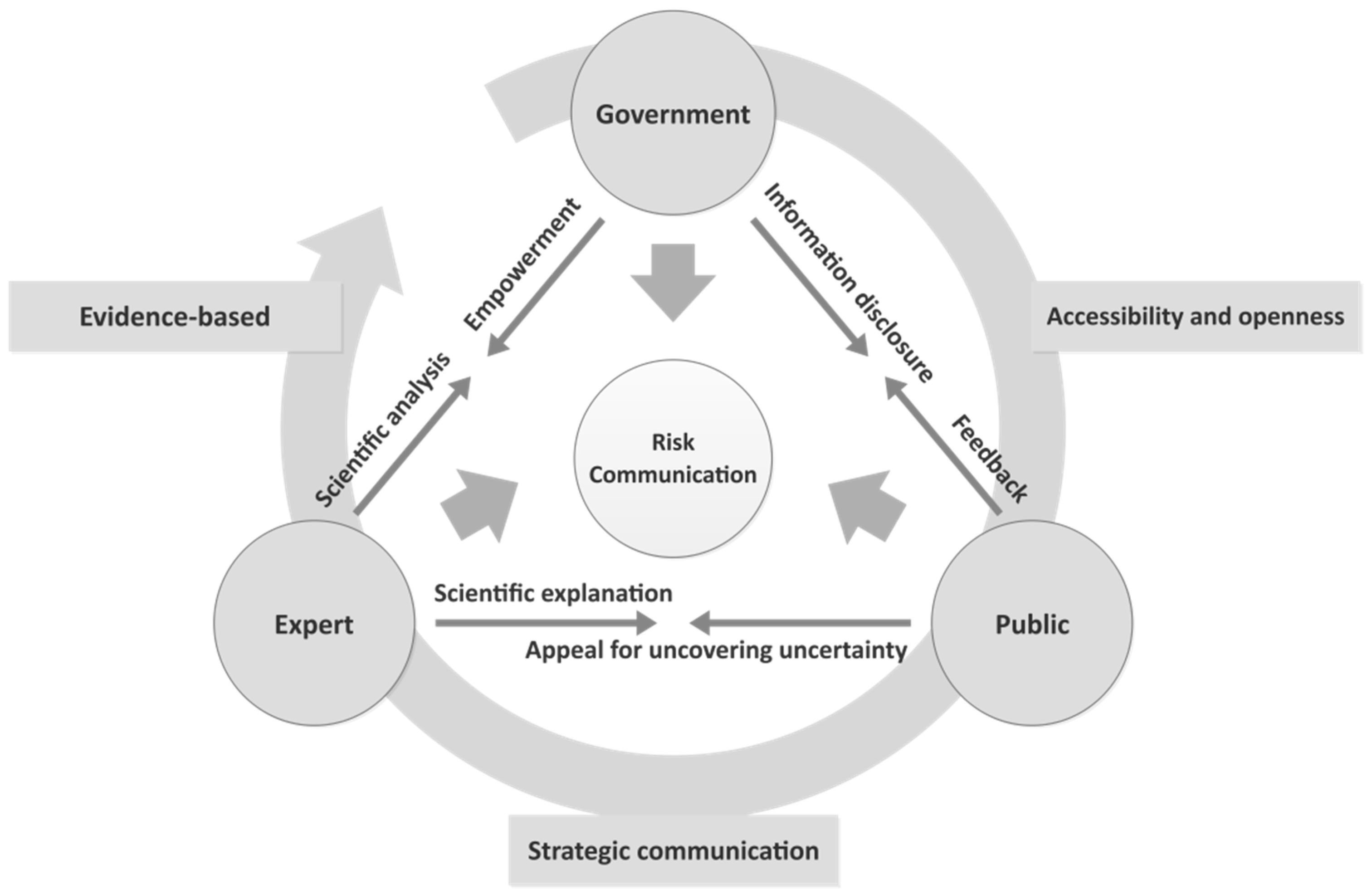
6. Discussion: A Simplified Model of Government–Expert–Public Risk Communication
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Society for Risk Analysis. Available online: https://onlinelibrary.wiley.com/doi/toc/10.1002/1539-6924.risk-analysis-and-coronaviruses (accessed on 10 February 2020).
- Kenis, P.; Schol, L.G.; Kraaj-Dirkzwager, M.M.; Timen, A. Appropriate Governance Responses to Infectious Disease Threats: Developing Working Hypotheses. Risk Hazards Crisis 2019, 10, 275–293. [Google Scholar] [CrossRef]
- Campbell-lendrum, D.; Manga, L.; Bagayoko, M.; Sommerfeld, J. Climate change and vector-borne diseases: What are the implications for public health research and policy? Philos. Trans. R. Soc. B 2015, 370, 20130552. [Google Scholar] [CrossRef] [PubMed]
- Frewer, L. The public and effective risk communication. Toxicol. Lett. 2004, 149, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Árvai, J.; Rivers, L., III. Effective Risk Communication; Routledge: London, UK, 2014; p. 3. [Google Scholar]
- Sin, M.S.Y. Masking fears: SARS and the politics of public health in China. Crit. Public Health 2016, 26, 88–98. [Google Scholar] [CrossRef]
- Kavanagh, M.M. Authoritarianism, outbreak, and information politics. Lancet 2020, 5, PE135–PE136. [Google Scholar] [CrossRef]
- Sellnow, T.L.; Ulmer, R.R.; Seeger, M.W.; Littlefield, R.S. Effective Risk Communication: A Message-Centered Approach; Springer: New York, NY, USA, 2009. [Google Scholar]
- Dynamic Situation of Outbreak Management. Available online: http://www.nhc.gov.cn/xcs/yqfkdt/gzbd_index.shtml (accessed on 10 February 2020).
- Wuhan Municipal Health Commission. Available online: http://wjw.wuhan.gov.cn/front/web/ztzl/801 (accessed on 10 February 2020).
- Special Report. Available online: https://m.yicai.com/news/100495596.html?native.theme=1 (accessed on 12 February 2020).
- Action for Combatting Novel Coronavirus Pneumonia Outbreak. Available online: http://www.xinhuanet.com/politics/xxgzbdgrdfyyq/index.htm (accessed on 10 February 2020).
- Special Report. Available online: http://china.caixin.com/2020-01-30/101509478.html (accessed on 11 February 2020).
- How do Experts’ Opinions Influence the Decision Making for Control the Novel Coronavirus? Available online: http://news.sina.com.cn/c/2020-03-10/doc-iimxxstf7791853.shtml (accessed on 10 March 2020).
- Interview to Zeng Guang. Available online: https://new.qq.com/omn/20200130/20200130A04YF400.html (accessed on 5 February 2020).
- Tang, B.; Wang, X.; Li, Q.; Bragazzi, N.L.; Tang, S.; Xiao, Y.; Wu, J. Estimation of the Transmission Risk of 2019-nCoV and Its Implication to Public Health Interventions. Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3525558 (accessed on 10 February 2020).
- Zhao, S.; Lin, Q.; Ran, J.; Musa, S.S.; Yang, G.; Wang, W.; Lou, Y.; Gao, D.; Yang, L.; He, D.; et al. Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: A data-driven analysis in the early phase of the outbreak. Int. J. Infect. Dis. 2020, 92, 214–217. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.; Normile, D. New SARS-like virus in China triggers alarm. Science 2020, 367, 234–235. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Tang, G.; Zhang, L.; Corlett, R.T. Decoding the Evolution and Transmissions of the Novel Pneumonia Coronavirus (SARS-CoV-2) Using whole Genomic Data. Available online: http://www.chinaxiv.org/abs/202002.00033 (accessed on 22 February 2020).
- Xu, X.; Chen, P.; Wang, J.; Feng, J.; Zhou, H.; Li, X.; Zhong, W.; Hao, P. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci. China Life Sci. 2020, 63, 457–460. [Google Scholar] [CrossRef] [PubMed]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef]
- Guan, W.; Ni, Z.; Hu, Y.; Liang, W.; Ou, C.; He, J.; Liu, L.; Shan, H.; Lei, C.; Hui, D.S.C.; et al. Clinical Characteristics of 2019 Novel Coronavirus Infection in China. Available online: https://www.medrxiv.org/content/10.1101/2020.02.06.20020974v1 (accessed on 22 February 2020).
- Read, J.M. Novel Coronavirus 2019-nCoV: Early Estimation of Epidemiological Parameters and Epidemic Predictions. Available online: https://doi.org/10.1101/2020.01.23.20018549 (accessed on 1 February 2020).
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus–Infected Pneumonia. Available online: https://www.nejm.org/doi/pdf/10.1056/NEJMoa2001316?articleTools=true (accessed on 1 February 2020).
- Renn, O. The role of risk communication and public dialogue for improving risk management. Risk Decision Policy 1998, 3, 5–30. [Google Scholar] [CrossRef]
- IRGC. Introduction to the IRGC Risk Governance Framework, Revised Version; International Risk Governance Center: Lausanne, Switzerland, 2017; p. 27. [Google Scholar]
- Buckley, C.; Myers, S.L. As New Coronavirus Spread, China’s Old Habits Delayed Fight. New York Times Website. Available online: https://www.nytimes.com/2020/02/01/world/asia/china-coronavirus.html?_ga=2.72446106.827276418.1581872988-2133314739.1581872988 (accessed on 10 February 2020).
- Pfeffer, J.; Salancik, G.R. The External Control of Organizations: A Resource Dependence Perspective; Harper and Row: New York, NY, USA, 1978; p. 1. [Google Scholar]
- Morgan, M.G.; Fischoff, B.; Bostrom, A.; Atman, C.J. Risk Communication: The Mental Models Approach; Cambridge University Press: New York, NY, USA, 2001. [Google Scholar]
- Yang, Z.; Zeng, Z.; Wang, K.; Wong, S.S.; Liang, W.; Zanin, M. Modified SEIR and AI prediction of the epidemics trend of COVID-19 in China under public health interventions. J. Thorac. Dis. 2020. [Google Scholar] [CrossRef]
- Green, M.S.; Zenilman, J.; Cohen, D. Risk Assessment and Risk Communication Strategies in Bioterrorism Preparedness Communication Strategies; Springer: New York, NY, USA, 2005; p. 105. [Google Scholar]
- Statistic of Rumors Refuting. Available online: https://vp.fact.qq.com/home?ADTAG=wx.kyk%20 (accessed on 10 March 2020).
- China Coronavirus: Misinformation Spreads Online about Origin and Scale. Available online: https://www.bbc.com/news/blogs-trending-51271037 (accessed on 10 February 2020).
- Renn, O. Risk Governance: Coping with Uncertainty in a Complex World; Earthscan: London, UK, 2008. [Google Scholar]
- Conrow, E.H. Effective Risk Management; American Institute of Aeronautics & Astronautics: Reston, FL, USA, 2003; pp. 22–74. [Google Scholar]
- Snapping up Shuanghuanglian at Midnight, the Media and Public Ought to Think Deeply. Available online: https://news.sina.cn/gn/2020-02-01/detail-iimxxste8037653.d.html?vt=4 (accessed on 15 February 2020).
- Breakwell, G.M. The Psychology of Risk; Cambridge University Press: Cambridge, UK, 2007. [Google Scholar]
- Lundgren, R.E.; McMakin, A.H. Risk Communication: A Handbook for Communicating Environmental, Safety, and Health Risks; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2013. [Google Scholar]
- Buckley, C. Chinese Doctor, Silenced after Warning of Outbreak, Dies form Coronavirus. Available online: https://www.nytimes.com/2020/02/06/world/asia/chinese-doctor-Li-Wenliang-coronavirus.html?searchResultPosition=1 (accessed on 13 February 2020).
- Garrick, J.; Gekler, W.C. The Analysis, Communication, and Perception of Risk; Springer Science Business Media: New York, NY, USA, 1991; p. 213. [Google Scholar]
- Veland, H.; Aven, T. Risk communication in the light of different risk perspectives. Reliabil. Eng. Syst. Saf. 2013, 110, 34–40. [Google Scholar] [CrossRef]
- Dhami, M.K. Towards an evidence-based approach to communicating uncertainty in intelligence analysis. Intell. Natl. Secur. 2018, 33, 257–272. [Google Scholar] [CrossRef]
- Covello, V.T.; McCallum, D.B.; Pavlova, M. Effective Risk Communication: The Role and Responsibility of Government and Nongovernment Organizations; Springer: New York, NY, USA, 1987. [Google Scholar]
- Charlebois, S.; Summan, A. A risk communication model for food regulatory agencies in modern society. Trends Food Sci. Technol. 2015, 45, 153–165. [Google Scholar] [CrossRef]
- European Food Safety Authority. When Food Is Cooking Up a Storm—Proven Recipes for Risk Communications 2017. Available online: http://www.efsa.europa.eu/en/corporate/pub/riskcommguidelines170524 (accessed on 13 February 2020).
- Boholm, Å. Risk communication as government agency organizational practice. Risk Anal. 2019, 39, 1695–1707. [Google Scholar] [CrossRef] [PubMed]
- Savage, L.J. The theory of statistical decision. J. Am. Stat. Assoc. 1951, 46, 55–67. [Google Scholar] [CrossRef]
- French, S. Expert judgment, meta-analysis, and participatory risk analysis. Decis. Anal. 2012, 9, 119–127. [Google Scholar] [CrossRef]
- Tucker, W.T.; Ferson, S. Strategies for risk communication evolution, evidence, experience. Ann. N. Y. Acad. Sci. 2008, 1128, IX–XII. [Google Scholar] [CrossRef] [PubMed]
- Gesser-Edelsburg, A.; Shir-Raz, Y.; Hayek, S.; Sassoni-Bar Lev, O. What does the public know about ebola? the public’s risk perceptions regarding the current ebola outbreak in an as-yet unaffected country. Am. J. Infect. Control 2015, 43, 669–675. [Google Scholar] [CrossRef] [PubMed]
- Pengpai News. Available online: https://mp.weixin.qq.com/s/IwbIdlID3pzSQeGKcm4NCQ (accessed on 23 February 2020).
| Best Practices for Risk Communication | Description |
|---|---|
| Infuse risk communication into policy decisions | Policies about risk may evolve and be communicated in a variety of ways. Decision making needs to be based on constant risk communication. |
| Treat risk communication as a process | Effective risk communication is a dynamic, interactive, and adaptive process. |
| Account for the uncertainty inherent in risk | Using equivocal messages to convey risk information. |
| Design risk messages to be culturally sensitive | Risk communication should fit specific features of the audience. These features include gender, education, age, and culture. |
| Acknowledge diverse levels of risk tolerance | People have widely varying capacities to process risk messages, including scientific and technical understandings of risk. |
| Involve the public in dialogue about risk | Risk communication dialogues should involve collaborations between the government, industry, and citizens that are open, inclusive, and deliberative. |
| Present risk messages with honesty | Risk communication should be an open, honest, and frank process, instead of essentially manipulative. |
| Meet risk perception needs by remaining open and accessible to the public | Honest communication is accessible and open as well, which means that the public can receive messages by various channels. |
| Collaborate and coordinate about risk with credible information sources | Coordination of risk communication strategies requires information sharing and establishing networks of working relationships between groups and agencies. |
| Date | Internal Communication | External Communication | Other Events Related to COVID-19 Information Disclosure |
|---|---|---|---|
| 27 December 2019 | Initial report: A doctor named Zhang Jixian reported cases related to COVID-19 to the Health Commissions of Wuhan and Hubei Province. | ||
| 29 to 30 December 2019 | Initial investigation: The Health Commission of Wuhan required that all medical institutions must investigate patients who have such unknown pneumonia privately. | Private whistleblowing: An ophthalmologist named Li Wenliang used social media to whistleblow that seven cases associated with SARS were identified and that detailed experimentation was ongoing. | |
| 31 December 2019 | Action at the Central level: The National Health Commission’s initial action for organizing a group to investigate the outbreak. | Initial announcement: The Health Commission of Wuhan publicly announced the outbreak but highlighted that there was no evidence of human-to-human transmission, that no medical workers were infected, and that this outbreak could be prevented and controlled. | |
| 1 January 2020 | “Attacking the rumor”: Li Wenliang and a further seven doctors were interrogated for “spreading rumors”. | ||
| 3 to 5 January 2020 | Further Evidence submitted: An academic group from Fudan University, Shanghai, found the SARS-like coronavirus and submitted the finding to the National Health Commission on 5 January. | Official announcement: Official announcement repeatedly conveyed that there was no evidence of human-to-human transmission, that no medical workers were infected, and that this outbreak was preventable and controllable. | |
| 6 January 2020 | Response at the Central level: The Chinese Center for Disease Control and Prevention (CCDC) activated II Level Response of Public Health Emergency. | ||
| 7 January 2020 | Supreme direction: The Leader of the Chinese Communist Party (CCP), Xi Jinping, arranged countermeasures to respond to this outbreak. | Official explanation on confirming a new coronavirus: Chinese official media announced there is a new coronavirus that has emerged in Wuhan. | |
| 10 January 2020 | Scientific explanation and risk assessment from expert: A medical expert at Peking University indicated that the outbreak can be controlled. | ||
| 15 January 2020 | Upgrading the response at the Central level: CCDC activated the highest I Level Response of Public Health Emergency. | ||
| 16 January 2020 | Official risk assessment: Wuhan municipal authority informed that there is low risk in persistent person-to-person transmission. | ||
| 17 January 2020 | Divergence in the epidemiological investigation: An academic group from Hong Kong University found evidence of person-to-person transmission and infection without symptoms. An expert named Kwok-Yung Yeun reported the finding to CCDC. | ||
| 20 January 2020 | Supreme command: CCP’s leader, Xi, required local governments to highly focus on controlling the outbreak by applying proper measures. | Verified epidemiological characteristics of COVID-19 from the academic community: A famous respiratory physician, Zhong Nanshan, confirmed the evidence of person-to-person transmission. | |
| 22 January 2020 | Response at the provincial level: Hubei Province activated II Level Response for Emergency. | ||
| 23 January 2020 | The Wuhan government officially announced that the whole city would be under large-scale quarantine at 10 a.m., which meant the beginning of formal and comprehensive management on this outbreak. | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, L.; Li, H.; Chen, K. Effective Risk Communication for Public Health Emergency: Reflection on the COVID-19 (2019-nCoV) Outbreak in Wuhan, China. Healthcare 2020, 8, 64. https://doi.org/10.3390/healthcare8010064
Zhang L, Li H, Chen K. Effective Risk Communication for Public Health Emergency: Reflection on the COVID-19 (2019-nCoV) Outbreak in Wuhan, China. Healthcare. 2020; 8(1):64. https://doi.org/10.3390/healthcare8010064
Chicago/Turabian StyleZhang, Liwei, Huijie Li, and Kelin Chen. 2020. "Effective Risk Communication for Public Health Emergency: Reflection on the COVID-19 (2019-nCoV) Outbreak in Wuhan, China" Healthcare 8, no. 1: 64. https://doi.org/10.3390/healthcare8010064
APA StyleZhang, L., Li, H., & Chen, K. (2020). Effective Risk Communication for Public Health Emergency: Reflection on the COVID-19 (2019-nCoV) Outbreak in Wuhan, China. Healthcare, 8(1), 64. https://doi.org/10.3390/healthcare8010064





