Desaturation during Six-Minute Walk Testing Predicts Major Morbidity Following Anatomic Lung Resection among Patients with COPD
Abstract
:1. Background
2. Methods
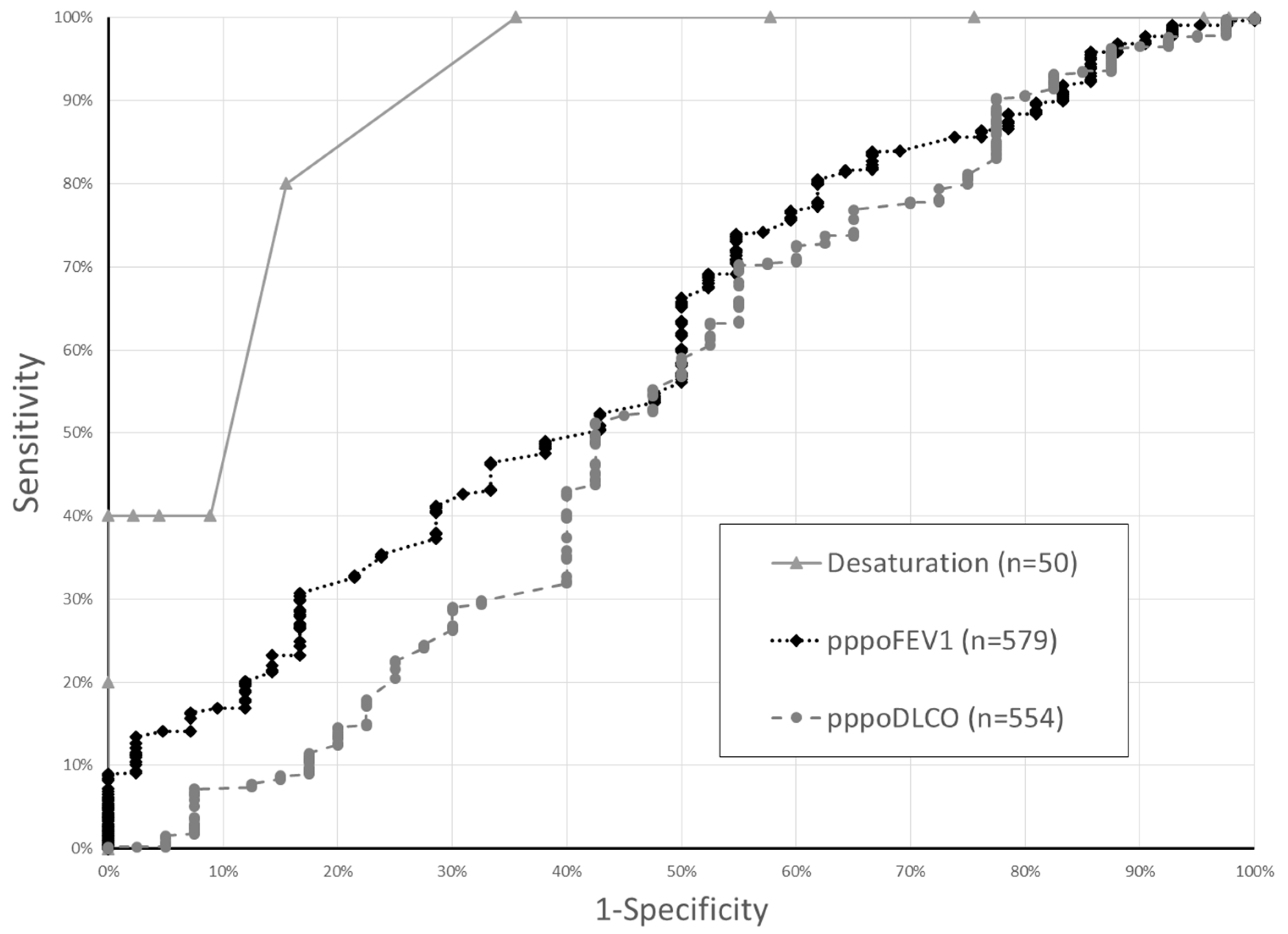
3. Results
4. Discussion/Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Brunelli, A.; Kim, A.W.; Berger, K.I.; Addrizzo-Harris, D.J. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest J. 2013, 143, e166S–e190S. [Google Scholar] [CrossRef] [PubMed]
- Berry, M.F.; Villamizar-Ortiz, N.R.; Tong, B.C.; Burfeind, W.R.; Harpole, D.H.; D’Amico, D.A.; Onaitis, D.M.W. Pulmonary function tests do not predict pulmonary complications after thoracoscopic lobectomy. Ann. Thorac. Surg. 2010, 89, 1044–1051. [Google Scholar] [CrossRef] [PubMed]
- Kachare, S.; Dexter, E.U.; Nwogu, C.; Demmy, T.L.; Yendamuri, S. Perioperative outcomes of thoracoscopic anatomic resections in patients with limited pulmonary reserve. J. Thorac. Cardiovasc. Surg. 2011, 141, 459–462. [Google Scholar] [CrossRef] [PubMed]
- Paul, S.; Andrews, W.G.; Nasar, A.; Port, J.L.; Lee, P.C.; Stiles, B.M.; Altorki, N.K. Outcomes of lobectomy in patients with severely compromised lung function (predicted postoperative diffusing capacity of the lung for carbon monoxide % ≤ 40%). Ann. Am. Thorac. Soc. 2013, 10, 616–621. [Google Scholar] [CrossRef] [PubMed]
- Ceppa, D.P.; Kosinski, A.S.; Berry, M.F.; Betty, C.D.; Harpole, D.H.; Mitchel, M.D.; D’Amico, M.D.; Onaitis, M.W. Thoracoscopic lobectomy has increasing benefit in patients with poor pulmonary function: A Society of Thoracic Surgeons Database analysis. Ann. Surg. 2012, 256, 487–493. [Google Scholar] [CrossRef] [PubMed]
- Brunelli, A.; Al Refai, M.; Monteverde, M.; Borri, A.; Salati, M.; Fianchini, A. Stair climbing test predicts cardiopulmonary complications after lung resection. Chest J. 2002, 121, 1106–1110. [Google Scholar] [CrossRef]
- Olsen, G.N.; Bolton, J.W.; Weiman, D.S.; Hornung, C.A. Stair climbing as an exercise test to predict the postoperative complications of lung resection. Two years’ experience. Chest J. 1991, 99, 587–590. [Google Scholar] [CrossRef]
- American Toracic Society Statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [CrossRef] [PubMed]
- Varela, G.; Cordovilla, R.; Jimenez, M.F.; Novoa, N. Utility of standardized exercise oximetry to predict cardiopulmonary morbidity after lung resection. Eur. J. Cardiothorac. Surg. 2001, 19, 351–354. [Google Scholar] [CrossRef]
- Hattori, K.; Matsuda, T.; Takagi, Y.; Nagaya, M.; Inoue, T.; Nishida, Y.; Nasegawa, Y.; Kawaguchy, K.; Fukui, T.; Ozeki, N.; et al. Preoperative six-minute walk distance is associated with pneumonia after lung resection. Interac. Cardiovasc. Thorac. Surg. 2017, 26, 227–283. [Google Scholar] [CrossRef] [PubMed]
- Kozower, B.D.; Sheng, S.; O’Brien, S.M.; Liptay, M.J.; Lau, C.A.; Jones, D.R.; Shahai, D.M.; Wright, C.D. STS database risk models: Predictors of mortality and major morbidity for lung cancer resection. Ann. Thorac. Surg. 2010, 90, 875–881. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, M.; Swanson, S.J.; Wright, C.D.; Chin, C.; Sheng, S.; Wisnivsky, J.; Weiser, T.S. Predictors of major morbidity and mortality after pneumonectomy utilizing the Society for Thoracic Surgeons General Thoracic Surgery Database. Ann. Thorac. Surg. 2010, 90, 927–934. [Google Scholar] [CrossRef] [PubMed]
- Mador, M.J.; Rodis, A.; Magalang, U.J. Reproducibility of Borg scale measurements of dyspnea during exercise in patients with COPD. Chest J. 1995, 107, 1590–1597. [Google Scholar] [CrossRef]
- Merkow, R.P.; Hall, B.L.; Choen, M.E.; Dimick, J.B.; Wang, E.; Chow, W.B.; Ko, C.J.; Bilmoria, K.Y. Relevance of the C-statistic when evaluating risk-adjustment models in surgery. J. Am. College Surg. 2012, 214, 822–830. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | SMWT not Performed (n = 531) | SMWT Performed (n = 50) | p-Value | |
|---|---|---|---|---|
| Age | 67.2 (67.9:60.5–75.2) | 70.0 (70.6:64.2–78.2) | 0.21 | |
| Male Sex | 223 (42.0%) | 21 (42.0%) | 1.00 | |
| Body Mass Index | 27.3 (26.7:23.1–30.8) | 27.1 (26.7:22.3–30.8) | 0.99 | |
| Hypertension | 322 (60.6%) | 28 (56.0%) | 0.52 | |
| Congestive Heart Failure | 23 (4.3%) | 5 (10.0%) | 0.07 | |
| Coronary Artery Disease | 97 (18.3%) | 16 (32.0%) | 0.02 | |
| Diabetes | 87 (16.4%) | 10 (20.0%) | 0.51 | |
| Preopchemotherapy and/or radiation | 50 (9.4%) | 5 (10.0%) | 0.89 | |
| pppoFEV1 * | 54.6 (54.5:44.2–62.6) | 49.4 (47.1:39.8–58.4) | 0.02 | |
| COPD Classification * | Mild (FEV1 ≥ 80%) | 212 (39.9%) | 11 (22.0%) | 0.024 |
| Moderate (80% > FEV1 ≥ 50%) | 281 (52.9%) | 32 (64.0%) | ||
| Severe (50% > FEV1 ≥ 30%) | 33 (6.2%) | 7 (14.0%) | ||
| Very Severe (FEV1 < 30%) | 5 (0.9%) | 0 | ||
| pppoDLCO | 49.7 (50.1:40.5–57.5) | 42.8 (43.6:37.6–50.2) | <0.01 | |
| Surgery Duration (hours) | 3.26 (30.5:2.4–3.9) | 3.24 (3.20:2.6–3.9) | 0.87 | |
| VATS | 347 (65.4%) | 26 (52.0%) | 0.06 | |
| Number of segments removed at surgery | 5.2 (5:5–5) | 5.0 (5:4–5) | 0.32 | |
| Any complication | 156 (29.4%) | 19 (38.0%) | 0.20 | |
| Major morbidity | 37 (7.0%) | 5 (10.0%) | 0.43 | |
| Death | 10 (1.9%) | 1 (2.0%) | 0.95 | |
| Test Result | Major Morbidity Occured | No Major Morbidity | p-Value |
|---|---|---|---|
| Oxygen saturation before SMWT (n = 50) * | 96.4 (1.81) | 96.4 (1.91) | 1.00 |
| Oxygen saturation after SMWT (n = 50) ** | 90 (89–92) | 94 (93–96) | 0.010 |
| SMWT Desaturation (change in SpO2) (n = 50) ** | 4 (4–10) | 2 (1–3) | 0.003 |
| Heart rate before SMWT (n = 50) * | 93.4 (9.8) | 74.4 (11.5) | 0.10 |
| Heart rate after SMWT (n = 50) ** | 113.6 (102–130) | 98.7 (87–108) | 0.13 |
| Borg Score at end of SMWT (n = 46) * | 3.20 (2.39) | 2.37 (1.28) | 0.22 |
| Distance walked (Meters) (n = 50) * | 399.2 (114.0) | 340.1 (101.7) | 0.23 |
| SMWT distance/predicted distance (n = 50) * | 0.98 (0.32) | 1.06 (0.34) | 0.63 |
| pppoFEV1 (n = 579) ** | 48.4 (39.3–58.2) | 54.6 (44.2–61.9) | 0.02 |
| pppoDLCO (n = 554) ** | 49.2 (37.4–58.2) | 49.2 (405–56.7) | 0.55 |
| Major Morbidity | OR | 95% Confidence Int | Z | p-Value | |
|---|---|---|---|---|---|
| SMWT Desaturation (change in SpO2) | 1.56 | 1.04 | 2.32 | 2.17 | 0.030 |
| pppoFEV1 | 1.00 | 0.91 | 1.10 | 0.07 | 0.943 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Towe, C.W.; Wu, K.; Khil, A.; Perry, Y.; Worrell, S.G.; Ho, V.P.; Linden, P.A. Desaturation during Six-Minute Walk Testing Predicts Major Morbidity Following Anatomic Lung Resection among Patients with COPD. Healthcare 2019, 7, 16. https://doi.org/10.3390/healthcare7010016
Towe CW, Wu K, Khil A, Perry Y, Worrell SG, Ho VP, Linden PA. Desaturation during Six-Minute Walk Testing Predicts Major Morbidity Following Anatomic Lung Resection among Patients with COPD. Healthcare. 2019; 7(1):16. https://doi.org/10.3390/healthcare7010016
Chicago/Turabian StyleTowe, Christopher W., Katherine Wu, Alina Khil, Yaron Perry, Stephanie G. Worrell, Vanessa P. Ho, and Philip A. Linden. 2019. "Desaturation during Six-Minute Walk Testing Predicts Major Morbidity Following Anatomic Lung Resection among Patients with COPD" Healthcare 7, no. 1: 16. https://doi.org/10.3390/healthcare7010016
APA StyleTowe, C. W., Wu, K., Khil, A., Perry, Y., Worrell, S. G., Ho, V. P., & Linden, P. A. (2019). Desaturation during Six-Minute Walk Testing Predicts Major Morbidity Following Anatomic Lung Resection among Patients with COPD. Healthcare, 7(1), 16. https://doi.org/10.3390/healthcare7010016





