The Global Problem of Insufficient Sleep and Its Serious Public Health Implications
Abstract
1. Introduction
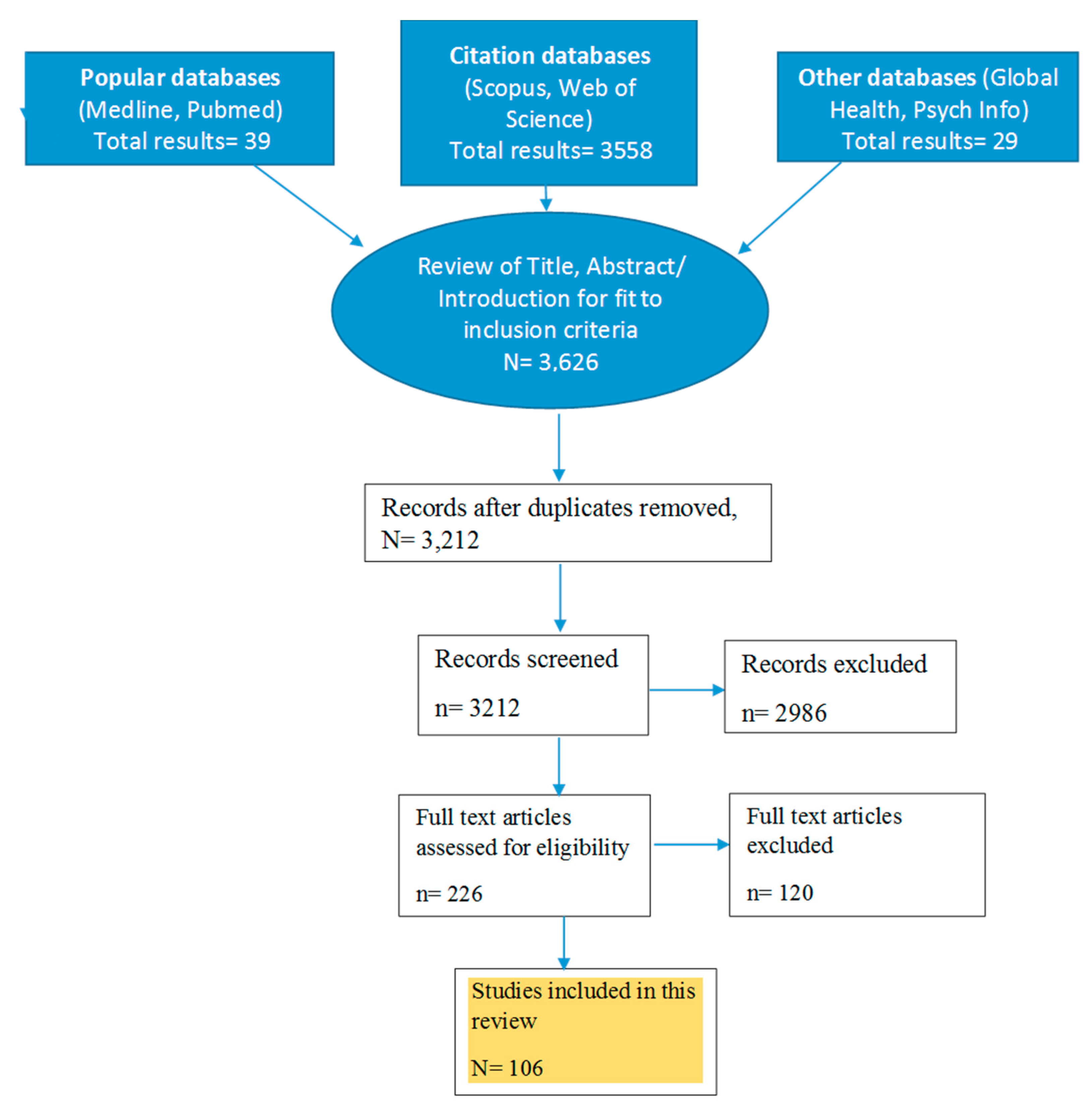
2. Materials and Methods
2.1. Epidemiology
2.2. All-Cause Mortality
2.3. Sleep Duration Recommendations by Age
2.4. Pathophysiology
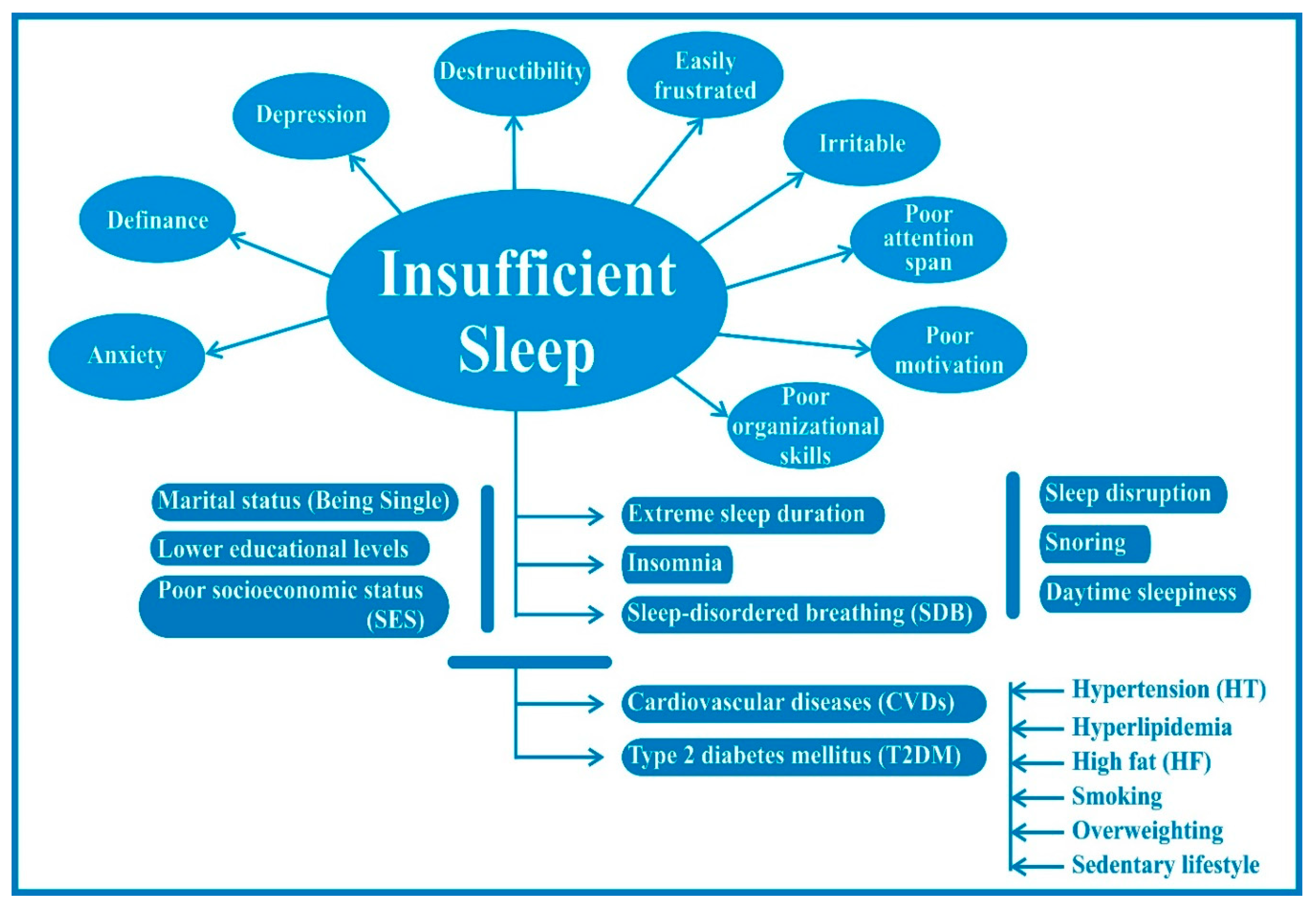
2.5. Contributing Factors
3. Results: Manifestations of Insufficient Sleep
3.1. Cognitive Effects
3.2. Mood and Judgment
3.3. Sleepiness and Microsleep
3.4. Effects on Respiratory Physiology
3.5. Wakefulness and Vigilance
3.6. Tiredness and Fatigue
3.7. Effects on Mental Health
3.8. Increased Incidence of Cardiovascular Morbidity
3.9. Effects on the Immune System
3.10. Obesity and Metabolism
3.11. Increased Risk for Diabetes Mellitus
3.12. Migraine
3.13. Clinical Burnout
3.14. Increased Risk of Cancers
3.15. Sleep-Wake Disturbances in Shift Workers
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Kochanek, K.D.; Murphy, S.L.; Xu, J.; Arias, E. Mortality in the United States, 2013. NCHS Data BriefS 2014, 178, 1–8. [Google Scholar]
- Grandner, M.A.; Hale, L.; Moore, M.; Patel, N.P. Mortality associated withshort sleep duration: The evidence, the possible mechanisms, and the future. Sleep Med. Rev. 2010, 14, 191–203. [Google Scholar] [CrossRef] [PubMed]
- Chapman, D.P.; Croft, J.B.; Liu, Y.; Perry, G.S.; Presley-Cantrell, L.R.; Ford, E.S. Excess frequent insufficient sleep in American Indians/Alaska natives. J. Environ. Public Health 2013, 2013, 259645. [Google Scholar] [CrossRef] [PubMed]
- Nielen, M.M.J.; Spronk, I.; Davids, R.; Zwaanswijk, M.; Verheij, R.A.; Korevaar, J.C. Incidentie en Prevalentie van Gezondheids Problemen in de Nederlandse Huisartsenpraktijk in 2012. NIVEL Zorgregistraties eerste lijn. Available online: https://www.nivel.nl/nl/nzr/zorgregistraties-eerstelijn (accessed on 19 December 2018).
- Spoormaker, V.I.; van den Bout, J. The prevalence of sleep disorders; relations with depression and anxiety e a pilot study. NSWO 2005, 16, 155–158. [Google Scholar]
- Kerkhof, G.A. Epidemiology of sleep and sleep disorders in The Netherlands. Sleep Med. 2017, 30, 229–239. [Google Scholar] [CrossRef] [PubMed]
- Hublin, C.; Kaprio, J.; Partinen, M.; Koskenvuo, M. Insufficient sleep—A population-based study in adults. Sleep 2001, 24, 392–400. [Google Scholar] [CrossRef] [PubMed]
- Ursin, R.; Bjorvatn, B.; Holsten, F. Sleep duration, subjective sleep need, and sleep habits of 40-to 45- year-olds in the Hordaland Health Study. Sleep 2005, 28, 1260. [Google Scholar] [CrossRef] [PubMed]
- Carskadon, M.A.; Harvey, K.; Duke, P.; Anders, T.F.; Litt, I.F.; Dement, W.C. Pubertal changes in daytime sleepiness. Sleep 1980, 2, 453–460. [Google Scholar] [PubMed]
- Loessl, B.; Valerius, G.; Kopasz, M.; Hornyak, M.; Riemann, D.; Voderholzer, U. Are adolescents chronically sleep-deprived? An investigation of sleep habits of adolescents in the Southwest of Germany. Child Care Health Dev. 2008, 34, 549–556. [Google Scholar] [CrossRef]
- Pallesen, S.; Saxvig, I.W.; Molde, H.; Sørensen, E.; Wilhelmsen-Langeland, A.; Bjorvatn, B. Brief report: Behaviorally induced insufficient sleep syndrome in older adolescents: Prevalence and correlates. J. Adolesc. 2011, 34, 391–395. [Google Scholar] [CrossRef]
- Luxton, D.D.; Greenburg, D.; Ryan, J.; Niven, A.; Wheeler, G.; Mysliwiec, V. Prevalence and impact of short sleep duration in redeployed OIF soldiers. Sleep 2011, 34, 1189–1195. [Google Scholar] [CrossRef]
- Watson, N.F.; Badr, M.S.; Belenky, G.; Bliwise, D.L.; Buxton, O.M.; Buysse, D.; Dinges, D.F.; Gangwisch, J.; Grandner, M.A.; Kushida, C.; et al. Joint consensus statement of the American academy of sleep medicine and sleep research society on the recommended amount of sleep for a healthy adult: Methodology and discussion. Sleep 2015, 38, 1161–1183. [Google Scholar] [CrossRef] [PubMed]
- Chapman, D.P.; Wheaton, A.G.; Perry, G.S.; Sturgis, S.L.; Strine, T.W.; Croft, J.B. Household demographics and perceived insufficient sleep among US adults. J. Community Health 2012, 37, 344–349. [Google Scholar] [CrossRef]
- Magee, C.A.; Iverson, D.C.; Caputi, P. Factors associated with short and long sleep. Prev. Med. 2009, 49, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Krueger, P.M.; Friedman, E.M. Sleep duration in the United States: A cross-sectional population-based study. Am. J. Epidemiol. 2009, 169, 1052–1063. [Google Scholar] [CrossRef] [PubMed]
- Kronholm, E.; Härmä, M.; Hublin, C.; Aro, A.R.; Partonen, T. Self-reported sleep duration in Finnish general population. J. Sleep Res. 2006, 15, 276–290. [Google Scholar] [CrossRef]
- Nishitani, N.; Sakakibara, H.; Akiyama, I. Short sleeping time and job stress in Japanese white-collar workers. Open Sleep J. 2013, 6, 104–109. [Google Scholar] [CrossRef][Green Version]
- Heo, Y.-S.; Chang, S.-J.; Park, S.-G.; Leem, J.-H.; Jeon, S.-H.; Lee, B.-J.; Kim, H.-C. Association between workplace risk factor exposure and sleep disturbance: Analysis of the 2nd Korean working conditions survey. Ann. Occup. Environ. Med. 2013, 25, 41. [Google Scholar] [CrossRef] [PubMed]
- Park, J.B.; Nakata, A.; Swanson, N.G.; Chun, H. Organizational factors associated with work-related sleep problems in a nationally representative sample of Korean workers. Int. Arch. Occup. Environ. Health 2013, 86, 211–222. [Google Scholar] [CrossRef] [PubMed]
- Hafner, M.; Stepanek, M.; Taylor, J.; Troxel, W.M.; van Stolk, C. Why Sleep Matters—The Economic Costs of Insufficient Sleep: A Comparative Cross-Country Analysis; RAND Corporation: Santa Monica, CA, USA, 2016. [Google Scholar]
- Chattu, V.K.; Sakhamuri, S.; Kumar, R.; BaHammam, A.; Perumal, P. Insufficient sleep: Is it time to recognize it as a major non-communicable disease? Sleep Sci. 2018, 11, 56–64. [Google Scholar] [CrossRef]
- Silva-Costa, A.; Griep, R.H.; Rotenberg, L. Associations of a short sleep duration, insufficient sleep, and insomnia with self-rated health among nurses. PLoS ONE 2015, 10, e0126844. [Google Scholar] [CrossRef] [PubMed]
- Bertisch, S.M.; Pollock, B.D.; Mittleman, M.A.; Buysse, D.J.; Bazzano, L.A.; Gottlieb, D.J.; Redline, S. Insomnia with objective short sleep duration and risk of incident cardiovascular disease and all-cause mortality: Sleep Heart Health Study. Sleep 2018, 41, zsy047. [Google Scholar] [CrossRef] [PubMed]
- Cirelli, C.; Benca, R.; Eichler, A.F. Insufficient Sleep: Definition, Epidemiology, and Adverse Outcomes. 2017. Available online: https://www.uptodate.com/contents/insufficient-sleep-definition-epidemiology-and-adverse-outcomes (accessed on 21 November 2018).
- Shearer, W.T.; Reuben, J.M.; Mullington, J.M.; Price, N.J.; Lee, B.N.; Smith, E.O.; Szuba, M.P.; Van Dongen, H.P.; Dinges, D.F. Soluble TNF-alpha receptor 1 and IL-6 plasma levels in humans subjected to the sleep deprivation model of spaceflight. J. Allergy Clin. Immunol. 2001, 107, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Dinges, D.F.; Douglas, S.D.; Hamarman, S.; Zaugg, L.; Kapoor, S. Sleep deprivation and human immune function. Adv. Neuroimmunol. 1995, 5, 97–110. [Google Scholar] [CrossRef]
- Aho, V.; Ollila, H.M.; Kronholm, E.; Bondia-Pons, I.; Soininen, P.; Kangas, A.J.; Hilvo, M.; Seppälä, I.; Kettunen, J.; Oikonen, M.; et al. Prolonged sleep restriction induces changes in pathways involved in cholesterol metabolism and inflammatory responses. Sci. Rep. 2016, 6, 24828. [Google Scholar] [CrossRef] [PubMed]
- Taheri, S.; Lin, L.; Austin, D.; Young, T.; Mignot, E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004, 1, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Franckle, R.L.; Falbe, J.; Gortmaker, S.; Ganter, C.; Taveras, E.M.; Land, T.; Davison, K.K. Insufficient sleep among elementary and middle school students is linked with elevated soda consumption and other unhealthy dietary behaviors. Prev. Med. 2015, 74, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Njai, R.S.; Greenlund, K.J.; Chapman, D.P.; Croft, J.B. Relationships between housing and food insecurity, frequent mental distress, and insufficient sleep among adults in 12 US States, 2009. Prev. Chronic Dis. 2014, 11, E37. [Google Scholar] [CrossRef]
- Williams, N.J.; Grandner, M.A.; Wallace, D.M.; Cuffee, Y.; Airhihenbuwa, C.; Okuyemi, K.; Ogedegbe, G.; Jean-Louis, G. Social and behavioral predictors of insufficient sleep among African Americans and Caucasians. Sleep Med. 2016, 18, 103–107. [Google Scholar] [CrossRef]
- Sabanayagam, C.; Shankar, A. The association between active smoking, smokeless tobacco, second-hand smoke exposure and insufficient sleep. Sleep Med. 2011, 12, 7–11. [Google Scholar] [CrossRef]
- Dahl, R.E. The consequences of insufficient sleep for adolescents: Links between sleep and emotional regulation. Phi Delta Kappan 1999, 80, 354–359. [Google Scholar]
- Maric, A.; Montvai, E.; Werth, E.; Storz, M.; Leemann, J.; Weissengruber, S.; Ruff, C.C.; Huber, R.; Poryazova, R.; Baumann, C.R. Insufficient sleep: Enhanced risk-seeking relates to low local sleep intensity. Ann. Neurol. 2017, 82, 409–418. [Google Scholar] [CrossRef] [PubMed]
- Taveras, E.M.; Rifas-Shiman, S.L.; Bub, K.L.; Gillman, M.W.; Oken, E. Prospective study of insufficient sleep and neurobehavioral functioning among school-age children. Acad. Pediatr. 2017, 17, 625–632. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Cho, S.J.; Cho, I.H.; Kim, S.J. Insufficient sleep and suicidality in adolescents. Sleep 2012, 35, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Oginska, H.; Pokorski, J. Fatigue and mood correlates of sleep length in three age-social groups: School children, students, and employees. Chronobiol. Int. 2006, 23, 1317–1328. [Google Scholar] [CrossRef]
- Bougard, C.; Gomez-Merino, D.; Rabat, A.; Arnal, P.; Van Beers, P.; Guillard, M.; Léger, D.; Sauvet, F.; Chennaoui, M. Daytime microsleeps during 7 days of sleep restriction followed by 13 days of sleep recovery in healthy young adults. Conscious. Cogn. 2018, 61, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Hakim, F.; Kheirandish-Gozal, L.; Gozal, D. Inflammatory pathways in children with insufficient or disordered sleep. Respir. Physiol. Neurobiol. 2011, 178, 465–474. [Google Scholar] [CrossRef]
- Khatami, R.; Landolt, H.P.; Achermann, P.; Rétey, J.V.; Werth, E.; Mathis, J.; Bassetti, C.L. Insufficient non-REM sleep intensity in narcolepsy-cataplexy. Sleep 2007, 30, 980–989. [Google Scholar] [CrossRef]
- McHill, A.W.; Hull, J.T.; Wang, W.; Czeisler, C.A.; Klerman, E.B. Chronic sleep curtailment, even without extended (>16-h) wakefulness, degrades human vigilance performance. Proc. Natl. Acad. Sci. USA 2018, 115, 6070–6075. [Google Scholar] [CrossRef]
- Owens, J.; Au, R.; Carskadon, M.; Millman, R.; Wolfson, A.; Braverman, P.K.; Adelman, W.P.; Breuner, C.C.; Levine, D.A.; Marcell, A.V.; et al. Insufficient sleep in adolescents and young adults: An update on causes and consequences. Pediatrics 2014, 134, e921–e932. [Google Scholar] [CrossRef]
- Vishnu, A.; Shankar, A.; Kalidindi, S. Examination of the association between insufficient sleep and cardiovascular disease and diabetes by race/ethnicity. Int. J. Endocrinol. 2011, 2011, 789358. [Google Scholar] [CrossRef] [PubMed]
- Grandner, M.A.; Smith, T.E.; Jackson, N.; Jackson, T.; Burgard, S.; Branas, C. Geographic distribution of insufficient sleep across the United States: A county-level hotspot analysis. Sleep Health 2015, 1, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Tanaka, H.; Fukuoka Heart Study Group. Overtime work, insufficient sleep, and risk of non-fatal acute myocardial infarction in Japanese men. Occup. Environ. Med. 2002, 59, 447–451. [Google Scholar] [CrossRef] [PubMed]
- Curtis, D.S.; Fuller-Rowell, T.E.; El-Sheikh, M.; Carnethon, M.R.; Ryff, C.D. Habitual sleep as a contributor to racial differences in cardiometabolic risk. Proc. Natl. Acad. Sci. USA 2017, 114, 8889–8894. [Google Scholar] [CrossRef] [PubMed]
- Prather, A.A.; Leung, C.W. Association of insufficient sleep with respiratory infection among adults in the United States. JAMA Intern. Med. 2016, 176, 850–852. [Google Scholar] [CrossRef] [PubMed]
- Cespedes, E.M.; Hu, F.B.; Redline, S.; Rosner, B.; Gillman, M.W.; Rifas-Shiman, S.L.; Taveras, E.M. Chronic insufficient sleep and diet quality: Contributors to childhood obesity. Obesity 2016, 24, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Markwald, R.R.; Melanson, E.L.; Smith, M.R.; Higgins, J.; Perreault, L.; Eckel, R.H.; Wright, K.P., Jr. Impact of insufficient sleep on total daily energy expenditure, food intake, and weight gain. Proc. Natl. Acad. Sci. USA 2013, 110, 5695–5700. [Google Scholar] [CrossRef] [PubMed]
- Chaput, J.P.; St-Onge, M.P. Increased food intake by insufficient sleep in humans: Are we jumping the gun on the hormonal explanation? Front. Endocrinol. 2014, 5, 116. [Google Scholar] [CrossRef] [PubMed]
- Nedeltcheva, A.V.; Kilkus, J.M.; Imperial, J.; Schoeller, D.A.; Penev, P.D. Insufficient sleep undermines dietary efforts to reduce adiposity. Ann. Intern. Med. 2010, 153, 435–441. [Google Scholar] [CrossRef]
- Penev, P.D. Update on energy homeostasis and insufficient sleep. J. Clin. Endocrinol. Metab. 2012, 97, 1792–1801. [Google Scholar] [CrossRef]
- Dutil, C.; Chaput, J.P. Inadequate sleep as a contributor to type 2 diabetes in children and adolescents. Nutr. Diabetes 2017, 7, e266. [Google Scholar] [CrossRef] [PubMed]
- Estrada, C.L.; Danielson, K.K.; Drum, M.L.; Lipton, R.B. Insufficient sleep in young patients with diabetes and their families. Biol. Res. Nurs. 2012, 14, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Geiger, S.D.; Sabanayagam, C.; Shankar, A. The relationship between insufficient sleep and self-rated health in a nationally representative sample. J. Environ. Public Health 2012, 2012, 518263. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Cho, S.J.; Kim, W.J.; Yang, K.I.; Yun, C.H.; Chu, M.K. Insufficient sleep is prevalent among migraineurs: A population-based study. J. Headache Pain 2017, 18, 50. [Google Scholar] [CrossRef] [PubMed]
- Buse, D.C.; Rains, J.C.; Fanning, K.M.; Reed, M.L.; Adams, A.M.; Pavlovic, J.M.; Lipton, R. The relationship between sleep disorders and migraine: Results from the chronic migraine epidemiology and outcomes (CaMEO) study. Neurology 2018, 90 (Suppl. 15), S43.007. [Google Scholar]
- Söderström, M.; Jeding, K.; Ekstedt, M.; Perski, A.; Akerstedt, T. Insufficient sleep predicts clinical burnout. J. Occup. Health Psychol. 2012, 17, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Elfering, A.; Kottwitz, M.U.; Tamcan, Ö.; Müller, U.; Mannion, A.F. Impaired sleep predicts onset of low back pain and burnout symptoms: Evidence from a three-wave study. Psychol. Health Med. 2018, 24, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Markt, S.C.; Grotta, A.; Nyren, O.; Adami, H.O.; Mucci, L.A.; Valdimarsdottir, U.A.; Stattin, P.; Bellocco, R.; Lagerros, Y.T. Insufficient sleep and risk of prostate cancer in a large Swedish cohort. Sleep 2015, 38, 1405–1410. [Google Scholar] [CrossRef]
- Lehrer, S.; Green, S.; Ramanathan, L.; Rosenzweig, K.E. Insufficient sleep associated with increased breast cancer mortality. Sleep Med. 2013, 14, 469. [Google Scholar] [CrossRef]
- Ahlberg, K.; Jahkola, A.; Savolainen, A.; Könönen, M.; Partinen, M.; Hublin, C.; Sinisalo, J.; Lindholm, H.; Sarna, S.; Ahlberg, J. Associations of reported bruxism with insomnia and insufficient sleep symptoms among media personnel with or without irregular shift work. Head Face Med. 2008, 4, 4. [Google Scholar] [CrossRef]
- Kervezee, L.; Cuesta, M.; Cermakian, N.; Boivin, D.B. Simulated night shift work induces circadian misalignment of the human peripheral blood mononuclear cell transcriptome. Proc. Natl. Acad. Sci. USA 2018, 115, 5540–5545. [Google Scholar] [CrossRef] [PubMed]
- Kecklund, G.; Axelsson, J. Health consequences of shift work and insufficient sleep. BMJ 2016, 355, i5210. [Google Scholar] [CrossRef] [PubMed]
- Schlafer, O.; Wenzel, V.; Högl, B. Sleep disorders among physicians on shift work. Anaesthesist 2014, 63, 844–851. [Google Scholar] [CrossRef] [PubMed]
- Ayas, N.T.; White, D.P.; Manson, J.E.; Stampfer, M.J.; Speizer, F.E.; Malhotra, A.; Hu, F.B. A prospective study of sleep duration and coronary heart disease in women. Arch. Intern. Med. 2003, 163, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Janszky, I.; Ljung, R. Shifts to and from daylight saving time and incidence of myocardial infarction. N. Engl. J. Med. 2008, 359, 1966–1968. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.C.; Burley, H.W.; Gotlib, I.H. Reduced sleep quality in healthy girls at risk for depression. J. Sleep Res. 2012, 21, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Howland, R.H. Sleep interventions for the treatment of depression. J. Psychosoc. Nurs. Ment. Health Serv. 2011, 49, 17–20. [Google Scholar] [CrossRef]
- Okun, M.L.; Luther, J.; Prather, A.A.; Perel, J.M.; Wisniewski, S.; Wisner, K.L. Changes in sleep quality, but not hormones predict time to postpartum depression recurrence. J. Affect. Disord. 2011, 130, 378–384. [Google Scholar] [CrossRef]
- O’Brien, E.M.; Mindell, J.A. Sleep and risk-taking behavior in adolescents. Behav. Sleep Med. 2005, 3, 113–133. [Google Scholar] [CrossRef]
- Catrett, C.D.; Gaultney, J.F. Possible insomnia predicts some risky behaviors among adolescents when controlling for depressive symptoms. J. Genet. Psychol. 2009, 170, 287–309. [Google Scholar] [CrossRef]
- Coulombe, J.A.; Reid, G.J.; Boyle, M.H.; Racine, Y. Concurrent associations among sleep problems, indicators of inadequate sleep, psychopathology, and shared risk factors in a population-based sample of healthy Ontario children. J. Pediatr. Psychol. 2010, 35, 790–799. [Google Scholar] [CrossRef] [PubMed]
- Lund, H.G.; Reider, B.D.; Whiting, A.B.; Prichard, J.R. Sleep patterns and predictors of disturbed sleep in a large population of college students. J. Adolesc. Health 2010, 46, 124–132. [Google Scholar] [CrossRef]
- Roberts, R.E.; Roberts, C.R.; Duong, H.T. Sleepless in adolescence: Prospective data on sleep deprivation, health and functioning. J. Adolesc. 2009, 32, 1045–1057. [Google Scholar] [CrossRef] [PubMed]
- Gupta, N.K.; Mueller, W.H.; Chan, W.; Meininger, J.C. Is obesity associated with poor sleep quality in adolescents? Am. J. Hum. Biol. 2002, 14, 762–768. [Google Scholar] [CrossRef]
- Kripke, D.F.; Garfinkel, L.; Wingard, D.L.; Klauber, M.R.; Marler, M.R. Mortality associated with sleep duration and insomnia. Arch. Gen. Psychiatry 2002, 59, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Alhola, P.; Polo-Kantola, P. Sleep deprivation: Impact on cognitive performance. Neuropsychiatr. Dis. Treat. 2007, 3, 553–567. [Google Scholar]
- Bocca, M.L.; Denise, P. Total sleep deprivation effect on disengagement of spatial attention as assessed by saccadic eye movements. Clin. Neurophysiol. 2006, 117, 894–899. [Google Scholar] [CrossRef]
- Harrison, Y.; Horne, J.A. One night of sleep loss impairs innovative thinking and flexible decision making. Organ. Behav. Hum. Decis. Process. 1999, 78, 128–145. [Google Scholar] [CrossRef]
- Beebe, D.W. Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatr. Clin. N. Am. 2011, 58, 649–665. [Google Scholar] [CrossRef]
- Wright, K.P., Jr.; Badia, P. Effects of menstrual cycle phase and oral contraceptives on alertness, cognitive performance, and circadian rhythms during sleep deprivation. Behav. Brain Res. 1999, 103, 185–194. [Google Scholar] [CrossRef]
- McCarthy, M.E.; Waters, W.F. Decreased attentional responsivity during sleep deprivation: Orienting response latency, amplitude, and habituation. Sleep 1997, 20, 115–123. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Harrison, Y.; Horne, J.A. Sleep loss and temporal memory. Q. J. Exp. Psychol. A 2000, 53, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Dinges, D.F.; Pack, F.; Williams, K.; Gillen, K.A.; Powell, J.W.; Ott, G.E.; Aptowicz, C.; Pack, A.I. Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4–5 hours per night. Sleep 1997, 20, 267–277. [Google Scholar] [PubMed]
- Killgore, W.D.; Balkin, T.J.; Wesensten, N.J. Impaired decision making following 49 h of sleep deprivation. J. Sleep Res. 2006, 15, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Curcio, G.; Ferrara, M.; De Gennaro, L. Sleep loss, learning capacity and academic performance. Sleep Med. Rev. 2006, 10, 323–337. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.; Dinges, D.F. A meta-analysis of the impact of short-term sleep deprivation on cognitive variables. Psychol Bull. 2010, 136, 375–389. [Google Scholar] [CrossRef] [PubMed]
- Saadat, H.; Bissonnette, B.; Tumin, D.; Raman, V.; Rice, J.; Barry, N.; Tobias, J. Effects of partial sleep deprivation on reaction time in anesthesiologists. Paediatr. Anaesth. 2017, 27, 358–362. [Google Scholar] [CrossRef]
- Lombardi, D.A.; Folkard, S.; Willetts, J.L.; Smith, G.S. Daily sleep, weekly working hours, and risk of work-related injury: US National Health Interview Survey (2004–2008). Chronobiol. Int. 2010, 27, 1013–1030. [Google Scholar] [CrossRef]
- De Mello, M.T.; Narciso, F.V.; Tufik, S.; Paiva, T.; Spence, D.W.; BaHammam, A.S.; Verster, J.C.; Pandi-Perumal, S.R. Sleep disorders as a cause of motor vehicle collisions. Int. J. Prev. Med. 2013, 4, 246. [Google Scholar]
- Pandi-Perumal, S.R.; Verster, J.C.; Kayumov, L.; Lowe, A.D.; Santana, M.G.; Pires, M.L.; Tufik, S.; Mello, M.T. Sleep disorders, sleepiness and traffic safety: A public health menace. Braz. J. Med. Biol. Res. 2006, 39, 863–871. [Google Scholar] [CrossRef]
- Steele, M.T.; Ma, O.J.; Watson, W.A.; Thomas, H.A., Jr.; Muelleman, R.L. The occupational risk of motor vehicle collisions for emergency medicine residents. Acad. Emerg. Med. 1999, 6, 1050–1053. [Google Scholar] [CrossRef] [PubMed]
- Drake, C.; Roehrs, T.; Breslau, N.; Johnson, E.; Jefferson, C.; Scofield, H.; Roth, T. The 10-year risk of verified motor vehicle crashes in relation to physiologic sleepiness. Sleep 2010, 33, 745–752. [Google Scholar] [CrossRef] [PubMed]
- Coren, S. Daylight saving time and traffic accidents. N. Engl. J. Med. 1996, 334, 924–925. [Google Scholar] [CrossRef] [PubMed]
- National Sleep Foundation. 2006 Teens and sleep. Sleep in America Polls; National Sleep Foundation: Washington, DC, USA, 2006; Available online: www.sleepfoundation.org/article/sleep-america-polls/2006-teens-and-sleep (accessed on 22 April 2018).
- Barnes, C.M.; Wagner, D.T. Changing to daylight saving time cuts into sleep and increases workplace injuries. J. Appl. Psychol. 2009, 94, 1305–1317. [Google Scholar] [CrossRef] [PubMed]
- Lahti, T.A.; Leppämäki, S.; Lönnqvist, J.; Partonen, T. Transition to daylight saving time reduces sleep duration plus sleep efficiency of the deprived sleep. Neurosci. Lett. 2006, 406, 174–177. [Google Scholar] [CrossRef] [PubMed]
- Kantermann, T.; Juda, M.; Merrow, M.; Roenneberg, T. The human circadian clock’s seasonal adjustment is disrupted by daylight saving time. Curr. Biol. 2007, 17, 1996–2000. [Google Scholar] [CrossRef] [PubMed]
- Kalmbach, D.A.; Arnedt, J.T.; Song, P.X.; Guille, C.; Sen, S. Sleep Disturbance and Short Sleep as Risk Factors for Depression and Perceived Medical Errors in First-Year Residents. Sleep 2017, 40. [Google Scholar] [CrossRef]
- Linde, L.; Edland, A.; Bergström, M. Auditory attention and multiattribute decision-making during a 33 h sleep-deprivation period: Mean performance and between-subject dispersions. Ergonomics 1999, 42, 696–713. [Google Scholar] [CrossRef]
- Killgore, W.D.; Kahn-Greene, E.T.; Lipizzi, E.L.; Newman, R.A.; Kamimori, G.H.; Balkin, T.J. Sleep deprivation reduces perceived emotional intelligence and constructive thinking skills. Sleep Med. 2008, 9, 517–526. [Google Scholar] [CrossRef]
- Olsen, O.K.; Pallesen, S.; Eid, J. The impact of partial sleep deprivation on moral reasoning in military officers. Sleep 2010, 33, 1086–1090. [Google Scholar] [CrossRef]
- Barnes, C.M.; Gunia, B.C.; Wagner, D.T. Sleep and moral awareness. J. Sleep Res. 2014, 24, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Vick, J.; Muchiri, E.; James, K. Insufficient Sleep and Depression in Adolescents. Family Nurse Practitioner Theses. 2015. 1. Available online: http://digitalcommons.northgeorgia.edu/fnp_etd/1 (accessed on 21 November 2018).
| Health Issues and Impairments Associated with Sleep Deprivation | Comments | References |
|---|---|---|
| Hypertension | Sleep deprivation is linked to an increased risk of hypertension | Schlafer et al., 2014 [66] |
| Cardiovascular incidents | Sleep-deprived people are at greater risk for coronary heart disease | Ayas et al., 2003 [67] |
| Increased heart attacks | Janszky and Ljung, 2008 [68] | |
| Type 2 diabetes mellitus (T2DM) | Sleep deprivation is linked to an increased risk of hypertension | Schlafer et al., 2014 [66] |
| Depression | Increases the risk of developing depression | Chen et al., 2012 [69] |
| Increases the relapse of depression | Howland, 2011 [70]; Okun et al., 2011 [71] | |
| High reporting of depressive symptoms among students | O’Brien, 2005 [72]; Catrett, 2009 [73] | |
| Anxiety, depression, and withdrawal increased depression among adolescents | Coulombe et al., 2010 [74]; Pallesen et al.,2011 [11]; Lund et al., 2010 [75]; Roberts et al., 2009 [76] | |
| Obesity | Sleep deprivation is linked to an increased risk of obesity | Schlafer et al., 2014 [66] |
| Suffer more obesity | Taheri et al., 2004 [29] | |
| Increased obesity among adolescents by 80% | Gupta et al., 2002 [77] | |
| Cancer | Linked to an increased risk of cancer | Markt S.C. et al., 2015 [61]; Lehrer S. et al., 2013 [62] |
| Mortality risks | Die at an early age | Kripe et al., 2002 [78] |
| Cognitive performance | Impairs visuomotor performance | Paula Alhola and Paivi Kantola, 2007 [79] |
| Impairment in saccadic eye movements | Bocca and Denise, 2006 [80] | |
| Increases rigid thinking, perseveration errors, and difficulties in utilizing new information in complex tasks | Harrison and Horne, 1999 [81] | |
| Affects high-level cognitive executive functions | Beebe, 2011 [82] | |
| Memory | Impaired performance in probed force memory recall and memory search | Wright and Badia, 1999 [83] McCarthy and Waters, 1997 [84] |
| Deterioration of temporal memory for recall of faces after 36 h of sleep deprivation | Harrison and Horne, 2000 [85] | |
| Mood | Suffer negative moods | Dinges et al., 1997 [86] |
| Thinking | Sleep loss produces temporary changes in cerebral metabolism, cognition, emotion, and behavior consistent with mild prefrontal lobe dysfunction | Killgore et al., 2008 [87] |
| Learning and academic performance | Poor declarative and procedural learning in students, but once sleep was optimized, improvement in academic performance noted | Curcio et al., 2006 [88] |
| Vigilance | Feedback blunting could be caused by general, downstream impairments from loss of vigilant attention due to sleep deprivation | Lim and Dinges, 2010 [89] |
| Reaction time | Greater subjective reliance on avoidance as a coping strategy was associated with greater deterioration in performance | Saadat et al., 2017 [90] |
| Personal injury | Decreased duration led to increased work-related injury | Lombardi et al., 2010 [91] |
| Traffic accidents | Increased risk of traffic accidents | de Mello et al., 2013 [92]; Pandi-Perumal et al., 2006 [93] |
| Increased traffic accidents among doctors under study | Steele et al., 1999 [94]; Schlafer et al., 2014 [66] | |
| More likely to be involved in vehicular crashes | Drake et al., 2010 [95] | |
| Increased auto accidents | Coren, 1996 [96] | |
| Increased car accidents among adolescents | National sleep foundation, 2006 [97] | |
| Industrial accidents | Increased workplace injuries | Barnes and Wagner, 2009 [98]; Lahti et al., 2006 [99]; Kantermann et al., 2007 [100] |
| Medical errors | Sleep disturbances and internship-enforced short sleep increased risk of depression development and chronicity and medical errors | Kalmbach et al. 2017 [101] |
| Decision making | Deterioration in decision-making | Linde et.al., 1999 [102] |
| Less effective in making decisions | Killgore et al., 2006 [103] | |
| Affects decision-making | Harrison, 2000 [85] | |
| Moral judgement | Moral reasoning was severely impaired during partial sleep deprivation | Olsen et. al., 2010 [104] |
| Lack of sleep is associated with low moral awareness | Christopher Barnes et al., 2014 [105] |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chattu, V.K.; Manzar, M.D.; Kumary, S.; Burman, D.; Spence, D.W.; Pandi-Perumal, S.R. The Global Problem of Insufficient Sleep and Its Serious Public Health Implications. Healthcare 2019, 7, 1. https://doi.org/10.3390/healthcare7010001
Chattu VK, Manzar MD, Kumary S, Burman D, Spence DW, Pandi-Perumal SR. The Global Problem of Insufficient Sleep and Its Serious Public Health Implications. Healthcare. 2019; 7(1):1. https://doi.org/10.3390/healthcare7010001
Chicago/Turabian StyleChattu, Vijay Kumar, Md. Dilshad Manzar, Soosanna Kumary, Deepa Burman, David Warren Spence, and Seithikurippu R. Pandi-Perumal. 2019. "The Global Problem of Insufficient Sleep and Its Serious Public Health Implications" Healthcare 7, no. 1: 1. https://doi.org/10.3390/healthcare7010001
APA StyleChattu, V. K., Manzar, M. D., Kumary, S., Burman, D., Spence, D. W., & Pandi-Perumal, S. R. (2019). The Global Problem of Insufficient Sleep and Its Serious Public Health Implications. Healthcare, 7(1), 1. https://doi.org/10.3390/healthcare7010001






