Sleep and Cognition in Community-Dwelling Older Adults: A Review of Literature
Abstract
:1. Introduction
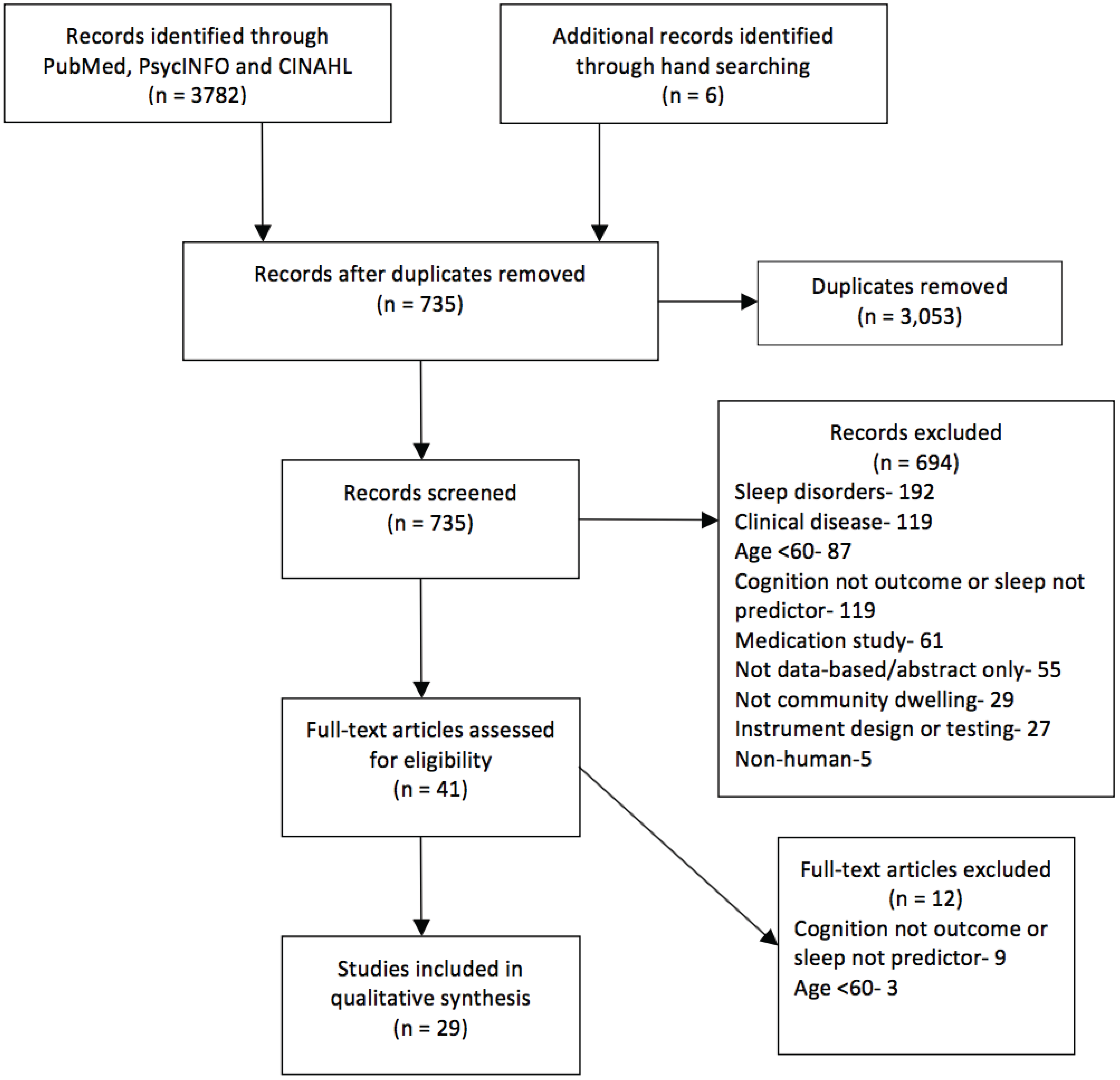
2. Methods
| Author, Year Country | Design | Sample Characteristics | Results | Exclusion Criteria/Statistical Adjustment |
|---|---|---|---|---|
| Ramos et al., (2013) [11] USA | Cross-Sectional | N—927 Mean Age—75 % Female—61 | TST: Long sleep (≥9 h) inversely associated with MMSE score and short sleep (˂6 h) not associated with MMSE score. | Statistical: Demographics, vascular factors, medications, risk for SDB, depression, alcohol consumption |
| Blackwell et al., (2006) [12] USA | Cross-Sectional | N—2932 Age—83.5 (±3.7) % Female—100 | SL: Longer SL was significantly associated with worse global cognition, attention, and executive function. WASO: Longer WASO was significantly associated with worse global cognition, attention, and executive function. SE: Lower SE was significantly associated with worse global cognition, attention, and executive function. TST: TST was significant associated with worse global cognition but was not associated with executive function or attention. | Statistical: Age, race, depression, education, BMI, health status, Hx. of stroke, Hx. of hypertension, IADL impairments, smoking, alcohol use, caffeine intake, antidepressant use, physical activity |
| Blackwell et al., (2011) [13] USA | Cross-Sectional | N—3132 Mean Age—76.4 % Female—0 | WASO: Longer objective WASO was associated with poorer global cognition, attention, and executive function. SE: Lower objective SE modeled continuously was associated with poorer attention and executive functioning but not global cognition. TST: Objective long sleep duration was associated with global cognitive functioning but not attention and executive function. Objective short sleep was not associated with global cognition, attention, or EF. Subjective short sleep (<5 h) and long sleep (>8 h) duration were associated with lower levels of global cognition. Long sleep, not short, was associated with poorer attention and executive function. The association between long sleep and global cognition, attention, and executive function disappeared after adjustment with WASO. General Sleep Problems: PSQI (>5) was not associated with global cognitive function, attention, or executive function. | Statistical: Age, race, clinic, education, depression, BMI, number of IADLs, comorbidities, antidepressant use, benzodiazepine use, alcohol use, smoking, physical activity, self-reported health status |
| Devore et al., (2014) [14] USA | Prospective | N—15,263 Mean Age—74.2 % Female—100 | TST: Short ≤5 h and long ≥9 h were associated with worse verbal fluency, working and episodic memory and global cognition score than those with 7 h sleep. An increase or decrease in sleep duration was associated with worse verbal fluency, working and episodic memory and global cognition scores. No association was found between sleep duration and cognitive decline. | Statistical: Age, education, shift-work history, smoking status, alcohol intake, physical activity, body mass index, history of high blood pressure, medical outcomes study mental health score, living alone, tranquilizer use |
| Tworoger et al., (2006) [15] USA | Cross-Sectional Longitudinal (2 years) | N—1844 Mean age—74.1 % Female—100 | TST: Cross sectionally, short sleep (≤5 h) but not long sleep (≥9 h) duration was associated with an increased risk of global cognitive impairment, and verbal fluency but not episodic memory. Longitudinally (2 years), neither short nor long sleep duration was associated with global cognition, episodic memory, or verbal fluency. General Sleep Problems: Cross-sectionally but not longitudinally, persons who had regular difficulties falling or staying were at an increased risk for poorer global cognitive impairment compared to those with occasional or rare sleep difficulties. There were no cross-sectional or longitudinal associations between sleep difficulties and episodic memory or verbal fluency. | Exclusion Criteria: Taking antidepressants, physician-diagnosis of depression, diagnosis of stroke Statistics: Age, education, smoking status, physical activity, HTN, living status, alcohol consumption, mental health index, use of tranquilizers |
| Lambaise et al., (2014) [16] USA | Cross-sectional | N—121 Mean Age—73.3 % Female—100 | SE: Lower objective SE was associated with poorer attention, executive function, and processing speed but not verbal fluency. Subjective SE not associated with attention, executive function, processing speed and verbal fluency. TST: Subjective shorter sleep time was associated with better executive function. Subjective and objective TST were not associated with attention, executive function, processing speed and verbal fluency. | Statistical: Education, race, BMI, depressive symptoms, height, weight, medication use, current hypertension, sleep medication use |
| Schmutte et al., (2007) [17] USA | Cross-Sectional | N—375 Mean Age—79.6 % Female—64.3 | SL: Persons with longer SL performed significantly worse on measures of attention, working memory, verbal fluency, and processing speed. SL was not associated with episodic memory. After statistical adjustment, longer SL was associated with only verbal fluency. TST: In univariate analyses, short sleep (˂6 h) and long sleep (˃9 h) duration were not associated with episodic memory, attention, working memory, verbal fluency, or processing speed. ANCOVA analyses for episodic memory indicate an association with longer sleep duration (˃9 h). | Statistical: Depression, age, education, medical comorbidities, physical morbidity, hypnotic use |
| St. Martin et al., (2012) [18] France | Cross-Sectional | N—272 Mean Age—74.8 % Female—71 | SL: SL was not associated with any of the 7 cognitive function measures. TST: TST was not associated with any of the 7 cognitive function measures. General Sleep Problems: Higher PSQI total scores were correlated with a poorer global cognitive function, shorter working memory, and worse attention span. Poorer sleep quality associated with shorter working memory and poorer delayed episodic memory. | Exclusion Criteria: MI, heart failure, stroke, previous dementia, neurological D/O, initiation of CPAP for OSA, diagnosis of a new neurological D/O Statistical: Gender, AHI, anxiety, depression, use of sleep meds |
| Nebes et al., (2009) [19] USA | Cross-sectional | N—157 Mean Age—72.2 % Female—Not provided | SL: Longer SL was associated with poorer global cognitive function but not associated with measures of attention, working memory, processing speed, executive function, and episodic memory. SE: Lower SE was associated with poorer global cognitive function and working memory (N-Back) but not associated with other measures of working memory, processing speed, executive function, and episodic memory. TST: Sleep duration was not associated with any of the cognitive function measures. General Sleep Problems: Higher PSQI scores were associated with poorer global cognitive function, a test of executive function(TMT-B), attention (TMT-B), and working memory (N-Back) but not other tests of executive function, processing speed, episodic memory, and working memory. | Exclusion Criteria: No CNS pathology, substance abuse, taking prescription psychoactive medication, no diagnosis of major depression in last five years or GDS score >15 Statistical: Total depressive score, risk of cerebrovascular disease, use of sleeping pills and anticholinergic meds |
| Miyata et al., (2013) [20] Japan | Cross-Sectional | N—78 Mean Age—72.2 % Female—79.5 | SL: SL not associated with working memory or attention. WASO: WASO not associated with working memory or attention. SE: Lower SE was significantly associated with worse working memory but not attention. TST: Accuracy of 0-back was different for those with ˂5 h than those with ˃7 h. No difference was seen between the participants with short and long sleep duration with accuracy on the 1-back test and the attention measure. General Sleep Problems: Global sleep quality was not associated with working memory and attention. | None provided |
| Chang-Quan, Bi-Rong & Yan, (2012) [21] China | Cross-Sectional | N—660 Mean Age—93.5 % Female—67.3 | SL: Longer SL was correlated with cognitive impairment. SE: Lower SE was correlated with cognitive impairment. General Sleep Problems: Poor sleep quality increased the risk for cognitive impairment. | Statistical: Age, gender, education level, serum lipid/lipoprotein, BMI, blood pressure, blood glucose level, smoking habit, alcohol consumption, tea consumption, exercise |
| Auyeung et al., (2011) [22] China | Cross-Sectional | N—2945 Age—73.9 (±5.0) % Female—40.8 | SL: A higher MMSE score was significantly associated with fewer reports of prolonged SL before and after statistical adjustment. TST: Longer nocturnal TST (>7 h) was significantly associated with lower general cognition. No association between global CF and short sleep duration (4 h to 7.9 h). General Sleep Problems: A higher MMSE score was significantly associated with less chronic sleep complaints in the univariate but not multivariate analyses. | Exclusion Criteria: Cognitively incompetent to give informed consent, medical conditions that made them unlikely to complete the study Statistical: Age, gender, MMSE score, education, smoking, alcohol, tea and coffee consumption, habitual smoking, depression (GDS ≥8), use of psychotropic meds, dx of HTN, diabetes, stroke, CHD, COPD |
| Keage et al., (2012) [23] UK | Cross-Sectional Longitudinal (2 and 10 years) | N-Baseline—2041 2 years—1658 10 years—663 Median age—75 % Female—53 | SL: SL was not cross-sectionally associated with cognitive impairment or predicted cognitive decline after 2 or 10 years. WASO: WASO was not cross-sectionally or longitudinally associated with cognitive impairment. TST: Both short (≤6.5 h) and long (≥9 h) sleep duration were not cross-sectionally associated with global cognitive impairment. Short sleep duration was associated with incident cognitive impairment over 10 years. Long sleep duration did not predict risk for cognitive impairment at years two and 10. General Sleep Problems: General sleep problems were not cross-sectionally or longitudinally associated with cognitive impairment. | Statistical: MMSE ≤21 at baseline, sex, age at baseline, BMI classification, education |
| Potvin et al., (2012) [24] Canada | Longitudinal (1 year) | N—1664 Mean Age Male—72.7 Female—73.9 % Female—69.7 | SL: SL was not associated with incident cognitive decline. SE: In women, SE was not associated with incident cognitive decline. In men, sleep efficiency predicted incident cognitive decline after one year. TST: Short sleep duration (≤5 h) was associated with incident cognitive decline in men and not women. In women and not men, long sleep duration (≥9 h) was associated with incident cognitive impairment over one year. General Sleep Problems: In women but not men, PSQI sleep disturbance score was associated with general cognitive decline one year later. In men but not women, global sleep quality score was associated with incident cognitive decline after one year. | Exclusion Criteria: Dementia, Cerebrovascular disease, Brain trauma/tumor/infections, Parkinson’s disease, Epilepsy, Schizophrenia and other forms of psychosis, Baseline MMSE score below the 15th percentile Statistical: Age, education, baseline MMSE score, anxiety, depressive episode psychotropic drug use, cardiovascular conditions score, chronic diseases |
| Jaussent et al., (2012) [25] France | Longitudinal (8 years) | N—4894 Mean Age—Not provided % Female—57 | SOL: SOL not associated with cognitive decline. WASO: As WASO increased, the risk of experiencing cognitive decline increased. General Sleep Problems: Sleep quality not associated with cognitive decline. | Statistical: Study center, sex, age, educational level, MMSE score at baseline, prescribed sleep meds, insomnia severity |
| Wilckens et al., (2014) [26] USA | Cross-Sectional | N—53 Mean Age—62.68 % Female—Not provided | WASO: Lower WASO was associated with better executive function, verbal fluency, and episodic memory, but not working memory or processing speed. TST: Neither total, long, nor shoet sleep duration were associated with executive function, episodic memory, working memory, verbal fluency or processing speed. | Exclusion Criteria: Self-reported diagnosis of depression, current psychiatric medication use, dependence on drugs or alcohol, diagnosis of a neurodegenerative disease Statistical: Sex, education |
| McCrae et al., (2012) [27] USA | Cross-Sectional | N—72 Mean Age—70.2 % Female—Not provided | TST: TST did not predict executive functioning or processing speed. General Sleep Problems: Total wake time did not predict executive functioning but significantly predicted processing speed. | Exclusion Criteria: Medical and neurological disorder, psychopathology, sleep disorders (OSA, RLS), MMSE lower than 23, severe depressive symptoms, suspected SDB, missing more than seven days of sleep data |
| Benito-Leon, Louis & Bermejo-Pareja, (2013) [28] Spain | Longitudinal (3 years) | N—2715 Age—72.9 (±6.1) % Female—56.9 | TST: At baseline, short sleep (≤5 h) global CF score was significantly different than reference (6–8 h) group but long sleep (≥9 h) global CF score not significantly different. Longitudinally, change in global CF associated with long sleep but not short sleep. Rate of cognitive decline not significantly different between short sleep and reference but significantly different between long sleep and reference groups. Long sleepers were 1.3 times more likely to have cognitive decline than reference group. Short sleepers’ odds of having cognitive decline similar to reference group. | Exclusion Criteria: Age, gender, geographical area, educational level, diabetes mellitus, chronic obstructive pulmonary disease, depressive symptoms, antidepressant use, medications with central nervous system effects |
| Virta et al., (2013) [29] Finland | Longitudinal (22.5 years) | N—2336 Mean Age—74.4 % Female—47.9 | TST: Short sleep duration (<7 h) and long sleep duration (>8 h) associated with poorer cognition. General Sleep Complaints: Poor sleep quality associated with poorer cognition. | Statistical: Snoring, use of hypnotics and tranquilizers, age, educational level, life satisfaction, obesity, hypertension, leisure time physical activity, alcohol consumption, binge drinking, APOE genotype |
| Loerbroks et al., (2010) [30] Germany | Cross-Sectional Longitudinal (8.5 years) | N—695 Mean Age—72.1 % Female—59 | TST: Short (≤6 h) and long (≥9 h) sleep duration were not cross-sectionally or longitudinally associated with global cognitive function. After statistical adjustment, a decline in sleep duration did not predict global cognitive impairment but an increase in sleep duration was associated with a two-fold increase in global cognitive impairment after 8.5 years. | Exclusion Criteria: Depression, taking mood enhancing drugs Statistical: Age, gender, educational level, physical activity, alcohol consumption, body mass index, smoking status, use of sleep medication, depressive symptoms at the time of testing |
| Xu et al., (2010) [31] China | Cross Sectional | N—28,670 Mean Age—62 % Female—72.5 | TST: Short TST(3–4 h and 5 h) and long TST (more than 10 h) were associated with worse episodic memory and global cognition. | Exclusion Criteria: self-reported mental illness or neurological disease, extremely short or long sleep duration Statistical: Age, sex, employment, occupation, education, smoking, drinking, physical activity, tea consumption, self-rated health, waist circumference, cholesterol, fasting plasma glucose, systolic blood pressure, sleeping duration, napping, insomnia, feeling tired in the morning |
| Ohayon & Vecchierini, (2002) [32] France | Cross-Sectional | N—1026 Mean age—Not provided % Female—59.8 | TST: Short sleep time (<7 h), but not long sleep duration (>8.5 h), was associated with attention-concentration deficits and difficulties in orientation for persons but not praxis, delayed recall, difficulties in temporal orientation, and prospective memory using the McNair Scale. Neither long nor short sleep duration was associated with MMSE. | Statistical: Age, sex, physical activity, occupation, organic diseases, use of sleep or anxiety medications, psychological well being |
| Faubel et al., (2009) [33] Spain | Cross-Sectional | N—3212 Age—71.6 % Female—52.6 | TST: Long sleep duration (>10 h) was associated with an increased risk for cognitive impairment. Short sleep duration (<7 h) was not associated with an increased risk of cognitive impairment. As TST increased from 7 h to 11 h, cognition progressively worsened. | Exclusion Criteria: Diagnosis of depression, extreme sleep duration <4 h or >17 h, dementia diagnosis Statistical: Age sex, physical activity, tobacco use, alcohol consumption, coffee consumption, educational level, SF-36 mental and physical summary scores, night time awakening, BMI, chronic diseases, anxiolytic and medical drug use, HTN, antihypertensive meds, number of social ties, head of family’s work status |
| Sampaio et al., (2012) [34] Japan | Cross-Sectional | N—145 Mean Age—73 % Female—53.1% | General Sleep Problems: Significant difference reported between good and poor sleepers on global cognition. | Exclusion Criteria: MMSE ≤21, uncontrolled cardiovascular, pulmonary, or metabolic diseases, surgery or forced bedrest in the past three months, current treatment for cancer, orthopedic condition that could restrict ADLs Statistical: Sex, education, living situation, work, financial satisfaction, smoking, alcohol, number of consultations in six months, number of medications, morbidities, comorbidities and regular physical activity categories. |
| Lim et al., (2013) [35] USA | Prospective Longitudinal (6 years) | N—737 Age—81.6 % Female—76 | General Sleep Problems: Increased sleep fragmentation associated with lower baseline global cognition and a more rapid rate of global cognitive decline. Persons with high sleep fragmentation had an increased risk of developing Alzheimer’s disease. | Statistical: Age, sex, education, time |
| Foley et al. (2001) [36] USA | Longitudinal (3 year) | N—2346 Mean Age—76.6 % Female—0 | General Sleep Problems: Having trouble falling asleep or waking up too early and being unable to fall asleep again at baseline was not predictive of global cognition 3 years later. | Exclusion Criteria: Diagnosis of dementia Statistical: Age, education, APOE, CASI score, depressive symptoms, hours of sleep, daytime napping, coronary heart disease, history of stroke |
| Gamaldo, Allaire & Whitfield, (2008) [37] USA | Cross-Sectional | N—174 Mean Age—72.7 % Female—70.7 | General Sleep Problems: There was a negative association between trouble falling asleep and working memory. There were no significant associations between trouble falling sleep and global cognition or episodic memory. Trouble falling asleep predicted working memory but not global cognition or episodic memory after statistical adjustment. | Statistical: Age, gender, education, depression, health, income |
| Zimmerman et al., (2012) [38] USA | Cross-Sectional | N—549 Mean Age—79.7 % Female—62.1 | General Sleep Problems: General sleep onset/maintenance difficulties were not associated with any of the cognition measures. | Exclusion Criteria: Visual and auditory impairment, active psychiatric symptoms, dementia, amnestic MCI Statistical: Age, gender, ethnicity, depression, cardiovascular history |
| Sutter et al., (2012) [39] Zurich | Cross-Sectional | N—96 Mean Age—72 % Female—57 | General Sleep Problems: Poor sleep quality was negatively associated with executive function, verbal fluency, and attention at higher levels of depression. Sleep quality was not associated with processing speed and episodic memory. | Exclusion Criteria: Parkinson’s disease, clinical significant depressive symptoms, use of antidepressants, Statistical: Age, sleep medications |
3. Results
| Subjective | Objective |
|---|---|
| Investigator-Developed Sleep Questionnaire | Actigraphy |
| Ramos et al., (2013) [11]; Devore et al., (2014) [14]; Tworoger et al., (2006) [15]; Schmutte et al., (2007) [17]; Auyeung et al., (2013) [22]; Keage et al., (2012) [23]; Jaussent et al., (2012) [25]; Virta et al., (2013) [29]; Loerbroks et al., (2010) [30]; Xu et al., (2010) [31]; Faubel et al., (2009) [33]; Sampaio et al., (2012) [34]; Lim et al., (2013) [35]; Foley et al., (2001) [36]; Gamaldo, Allaire & Whitfield, (2008) [37] | Blackwell et al., (2006) [12]; Blackwell et al., (2011) [13]; Lambaise et al., (2014) [16]; Miyata et al., (2013) [20]; Lim et al., (2013) [35] |
| Pittsburgh Sleep Quality Index | SensaWear |
| Blackwell et al., (2011) [13]; St. Martin et al., (2012) [18]; Nebes et al., (2009) [19]; Miyata et al., (2013) [20]; Chang-Quan, Bi-Rong & Yan, (2012) [21]; Potvin et al., (2012) [24]; Sutter et al. (2012) [39] | Wilckens et al., (2014) [26] |
| Sleep Diary | |
| Blackwell et al., (2011) [13]; Lambaise et al., (2014) [16]; McCrae et al., (2012) [27] | |
| Sleep-EVAL System | |
| Blackwell et al., (2011) [13]; Lambaise et al., (2014) [16]; McCrae et al., (2012) [27] | |
| Medical Outcomes Study Sleep Scale | |
| Zimmerman et al., (2012) [38] |
| Executive Function | Attention | Episodic Memory | Working Memory | Verbal Fluency | Processing Speed | Global Cognition |
|---|---|---|---|---|---|---|
| German Achievement Measure Test | Continuous Performance Test | Delayed Recall of the TICS 10 Word List | Alpha Span Task | Alphabetic/Word Fluency | Code Test | (Modified) Mini-Mental Status Exam |
| Sutter et al., (2012) [39] | Miyata et al., (2013) [20] | Devore et al., (2014) [14]; Tworoger et al., (2006) [15] | Gamaldo, Allaire & Whitfield, (2008) [37] | Lambaise et al., (2014) [16]; St. Martin et al., (2012) [18]; Wilckens et al., (2014) [26]; Zimmerman et al., (2012) [38]; Sutter et al., (2012) [39] | St. Martin et al., (2012) [18] | Ramos et al., (2013) [11]; Blackwell et al., (2011) [13]; Tworoger et al., (2006) [15]; St. Martin et al., (2012) [18]; Chang-Quan, Bi-Rong & Yan, (2012) [21]; Auyeung et al., (2013) [22]; Keage et al., (2012) [23]; Potvin et al., (2012) [24]; Jaussent et al., (2012) [25]; McCrae et al., (2012) [27]; Xu et al., (2010) [31]; Ohayon & Vecchierini, (2002) [32]; Faubel et al., (2009) [33]; Sampaio et al., (2012) [34]; Gamaldo, Allaire & Whitfield, (2008) [37] |
| Go/No-Go Task | Digit Vigilance Test | East Boston Memory Test | Benton Visual Retention Test | Category Fluency | Conceptual and Perceptual Comparison | Cognitive Abilities Screening Instrument |
| Sutter et al., (2012) [39] | Blackwell et al., (2011) [13] | Devore et al., (2014) [14]; Tworoger et al., (2006) [15] | Jaussent et al., (2012) [25]; St. Martin et al., (2012) [18] | Devore et al., (2014) [14]; Lambaise et al., (2014) [16]; St. Martin et al., (2012) [18]; Schmutte et al., (2007) [17]; Sutter et al., (2012) [39]; Tworoger et al., (2006) [15]; Zimmerman et al., (2012) [38]; Wilckens et al., (2014) [26] | Nebes et al., (2009) [19] | Foley et al., (2001) [36] |
| Hayling Test | Months Backward | Letter Series Task | Digit Span Backwards | Digit Symbol Substitution | Telephone Interview for Cognitive Status | |
| Nebes et al., (2009) [19] | Schmutte et al., (2007) [17] | McCrae et al., (2012) [27] | Devore et al., (2014) [14]; Tworoger et al., (2006) [15]; Schmutte et al., (2007) [17]; Loerbroks et al., (2010) [30]; Gamaldo, Allaire & Whitfield, (2008) [37]; Zimmerman et al., (2012) [38] | Lambaise et al., (2014) [16]; Schmutte et al., (2007) [17]; Wilckens et al., (2014) [26]; Sutter et al., (2012) [39] | Devore et al., (2014) [14]; Tworoger et al., (2006) [15]; Virta et al., (2013) [29]; Loerbroks et al., (2010) [30] | |
| Stroop Test | Trail Making Test Part A | Logical Memory Test | Forward Digit Span | Symbol Digit Modalities Test | Repeatable Battery for the Assessment of Neuropsychological Status | |
| St. Martin et al., (2012) [18]; Nebes et al., (2009) [19]; Wilckens et al., (2014) [26] | Lambaise et al., (2014) [16]; St. Martin et al., (2012) [18]; Zimmerman et al., (2012) [38]; Sutter et al., (2012) [39] | Nebes et al., (2009) [19] | Gamaldo, Allaire & Whitfield, (2008) [37] | McCrae et al., (2012) [27] | Nebes et al., (2009) [19] | |
| Trail Making Test Part B | Trail Making Test Part B | Selective Reminding Test | N-Back Test | Composite of Tests of Multiple Domains | ||
| Blackwell et al., (2006) [12]; Blackwell et al., (2011) [13]; Lambaise et al., (2014) [16]; St. Martin et al., (2012) [18]; Nebes et al., (2009) [19]; Zimmerman et al., (2012) [38]; Sutter et al., (2012) [39] | Blackwell et al., (2006) [12]; Blackwell et al., (2011) [13]; Lambaise et al., (2014) [16]; St. Martin et al., (2012) [18]; Nebes et al., (2009) [19]; Zimmerman et al., (2012) [38]; Sutter et al., (2012) [39] | Schmutte et al., (2007) [17]; St. Martin et al., (2012) [18]; Zimmerman et al., (2012) [38] | Miyata et al., (2013) [17]; Nebes et al., (2009) [19]; Wilckens et al., (2014) [26] | Lim et al., (2013) [35] | ||
| Verbal Learning Test | Stenberg Working Memory Task | Cognitive Difficulties Scale | ||||
| Gamaldo, Allaire & Whitfield, (2008) [37]; Sutter et al., (2012) [39] | Wilckens et al., (2014) [26] | St. Martin et al., (2012) [18]; Ohayon & Vecchierini, (2002) [32] | ||||
| Consortium to Establish a Registry for Alzheimer’s Disease List Memory Test | Blessed Information Memory Concentration Test | |||||
| Wilckens et al., (2014) [26]; Xu et al., (2010) [31] | Zimmerman et al., (2012) [38] | |||||
| TELE | ||||||
| Virta et al., (2013) [29] |
| Sleep Parameters | Executive Function | Attention | Episodic Memory | Working Memory | Verbal Fluency | Processing Speed | Global Cognition | |
|---|---|---|---|---|---|---|---|---|
| Long Sleep Latency | Sig | Schmutte et al., (2007) [17]* | Schmutte et al., (2007) [17]* | Schmutte et al., (2007) [17] | Schmutte et al., (2007) [17]* | Nebes et al., (2009) [19]; Chang-Quan et al., (2012) [21]; Auyeung et al., (2013) [22] | ||
| NS | St. Martin et al., (2012) [18]; Nebes et al., (2009) [19] | Schmutte et al., (2007) [17]; St. Martin et al., (2012) [18]; Nebes et al., (2009) [19] | Tworoger et al., (2006) [15]; Schmutte et al., (2007) [17]; St. Martin et al., (2012) [18] | Schmutte et al., (2007) [17]; St. Martin et al., (2012) [18]; Nebes et al., (2009) [19]; Miyata et al., (2013) [20] | St. Martin et al., (2012) [18] | Schmutte et al., (2007) [17]; St. Martin et al., (2012) [18]; Nebes et al., (2009) [19] | St. Martin et al., (2012) [18]; Keage et al., (2012) [23]; Potvin et al., (2012) [24]; Jaussent et al., (2012) [25] | |
| Long Wake After Sleep Onset | Sig | Chang-Quan et al., (2012) [21] | ||||||
| NS | Keage et al., (2012) [23] | |||||||
| Low Sleep Efficiency | Sig | Nebes et al., (2009) [19]; Chang-Quan et al., (2012) [21]; Potvin et al., (2012) [24]* | ||||||
| NS | Lambaise et al., (2014) [16]; Nebes et al., (2009) [19] | Lambaise et al., (2014) [16]; Nebes et al., (2009) [19] | Nebes et al., (2009) [19] | Nebes et al., (2009) [19] | Lambaise et al., (2014) [16] | Lambaise et al., (2014) [16]; Nebes et al., (2009) [19] | Tworoger et al., (2006) [15]; Potvin et al., (2012) [24] | |
| Short Sleep Duration | Sig | Loerbroks et al., (2010) [30] | Devore et al., (2014) [14]; Xu et al., (2011) [31] | Devore et al., (2014) [14] | Devore et al., (2014) [14]; Tworoger et al., (2006) [15]* | Blackwell et al., (2011) [13]; Devore et al., (2014) [14]; Tworoger et al., (2006) [15]*; Keage et al., (2012) [23]*; Potvin et al., (2012) [24]*; Benito-Leon et al., (2013) [28]*; Virta et al., (2013) [29]; Xu et al., (2011) [31] | ||
| NS | Blackwell et al., (2011) [13] | Blackwell et al., (2011) [13]; Schmutte et al., (2007) [17] | Tworoger et al., (2006) [15]; Schmutte et al., (2007) [17]; Loerbroks et al., (2010) [30] | Schmutte et al., (2007) [17] | Tworoger et al., (2006) [15]; Schmutte et al., (2007) [17] | Schmutte et al., (2007) [17] | Ramos et al., (2013) [11]; Tworoger et al., (2006) [15]; Auyeung et al., (2013) [22]; Keage et al., (2012) [23]; Potvin et al., (2012) [24]; McCrae et al., (2012) [27]; Loerbroks et al., (2010) [30]; Ohayon & Vecchierini, (2002) [32]; Faubel et al., (2009) [33] | |
| Long Sleep Duration | Sig | Blackwell et al., (2011) [13] | Blackwell et al., (2011) [13] | Schmutte et al., (2007) [17]*; Xu et al. (2011) [31] | Ramos et al., (2013) [11]; Blackwell et al., (2011) [13]; Auyeung et al., (2013) [22]; Potvin et al., (2012) [24]*; Benito-Leon et al. (2013) [28]*; Virta et al., (2013) [29]; Xu et al., (2011) [31]; Faubel et al., (2009) [33] | |||
| NS | Wilckens et al., (2014) [26]; Ohayon & Vecchierini, (2002) [32] | Schmutte et al., (2007) [17]; Loerbroks et al., (2010) [30] | Tworoger et al., (2006) [15]; Schmutte et al., (2007) [17]; Wilckens et al., (2014) [26]; Loerbroks et al., (2010) [30]; Ohayon & Vecchierini, (2002) [32] | Schmutte et al., (2007) [17]; Wilckens et al., (2014) [26]; Loerbroks et al., (2010) [30] | Tworoger et al., (2006) [15]; Schmutte et al., (2007) [17]; Wilckens et al., (2014) [26]; Loerbroks et al., (2010) [30] | Schmutte et al., (2007) [17]; Wilckens et al., (2014) [26] | Tworoger et al., (2006) [15]; Keage et al., (2012) [23]; Potvin et al., (2012) [24]; Benito-Leon et al., (2013) [28]; Loerbroks et al., (2010) [30] | |
| Total Sleep Duration | Sig | Lambaise et al., (2014) [16] | Lambaise et al., (2014) [16] | |||||
| NS | St. Martin et al., (2012) [18]; Nebes et al., (2009) [19]; McCrae et al., (2012) [27] | St. Martin et al., (2012) [18]; Nebes et al., (2009) [19] | St. Martin et al., (2012) [18]; Nebes et al., (2009) [19] | St. Martin et al., (2012) [18]; Nebes et al., (2009) [19] | Lambaise et al., (2014) [16]; St. Martin et al., (2012) [18] | St. Martin et al., (2012) [18]; Nebes et al., (2009) [19]; McCrae et al., (2012) [27] | St. Martin et al., (2012) [18]; Nebes et al., (2009) [19] | |
| General Sleep Problems | Sig | Nebes et al., (2009) [19]*; Sutter et al., (2012) [39] | St. Martin et al., (2012) [18]; Nebes et al., (2009) [19]; Sutter et al., (2012) [39] | St. Martin et al., (2012) [18]* | St. Martin et al., (2012) [18]; Nebes et al., (2009) [19]*; Gamaldo et al., (2008) [37] | Sutter et al., (2012) [39] | McCrae et al., (2012) [27] | Tworoger et al., (2006) [15]*; St. Martin et al., (2012) [18]*; Nebes et al., (2009) [19]; Chang-Quan et al., (2012) [21]; Auyeung et al., (2013) [22]*; Potvin et al., (2012) [24]*; Virta et al., (2013) [29]; Sampaio et al., (2012) [34] |
| NS | Blackwell et al., (2011) [13]; St. Martin et al., (2012) [18]; Nebes et al., (2009) [19]; McCrae et al., (2012) [27]; Zimmerman et al., (2012) [38] | Blackwell et al., (2011) [13]; Miyata et al., (2013) [20]; Zimmerman et al., (2012) [38] | Tworoger et al., (2006) [15]; St. Martin et al., (2012) [18]; Nebes et al., (2009) [19]; Gamaldo et al., (2008) [37]; Sutter et al., (2012) [39] | Zimmerman et al., (2012) [38] | Tworoger et al., (2006) [15]; St. Martin et al., (2012) [18]; Zimmerman et al., (2012) [38] | St. Martin et al., (2012) [18]; Nebes et al., (2009) [19]; Sutter et al., (2012) [39] | Blackwell et al., (2011) [13]; Tworoger et al., (2006) [15]; St. Martin et al., (2012) [18]; Auyeung et al., (2013) [22]; Keage et al., (2012) [23]; Potvin et al., (2012) [24]; Jaussent et al., (2012) [25]; Foley et al., (2001) [36]; Gamaldo et al., (2008) [37]; Zimmerman et al., (2012) [38] | |
| Sleep Parameters | Executive Function | Attention | Episodic Memory | Working Memory | Verbal Fluency | Processing Speed | Global Cognition | ||
|---|---|---|---|---|---|---|---|---|---|
| Long Sleep Latency | Sig | Blackwell et al., (2006) [12] | Blackwell et al., (2006) [12] | Blackwell et al., (2006) [12] | |||||
| NS | Miyata et al., (2013) [20] | Miyata et al., (2013) [20] | |||||||
| Long Wake After Sleep Onset | Sig | Blackwell et al., (2006) [12]; Blackwell et al., (2011) [13]; Wilckens et al., (2014) [26] | Blackwell et al., (2006) [12]; Blackwell et al., (2011) [13] | Wilckens et al., (2014) [26] | Wilckens et al., (2014) [26] | Blackwell et al., (2006) [12]; Blackwell et al., (2011) [13] | |||
| NS | Miyata et al., (2013) [20] | Miyata et al., (2013) [20]; Wilckens et al., (2014) [26] | Wilckens et al., (2014) [26] | ||||||
| Low Sleep Efficiency | Sig | Blackwell et al., (2006) [12]; Blackwell et al., (2011) [13]; Lambaise et al., (2014) [16] | Blackwell et al., (2006) [12]; Blackwell et al., (2011) [13]; Lambaise et al., (2014) [16] | Miyata et al., ( 2013) [20] | Lambaise et al., (2014) [16] | Blackwell et al., (2006) [12] | |||
| NS | Miyata et al., ( 2013) [20] | Lambaise et al., (2014) [16] | Blackwell et al., (2011) [13] | ||||||
| Sleep Dura-tion | Short | Sig | Miyata et al., (2013) [20] | ||||||
| NS | Blackwell et al., (2011) [13]; Wilckens et al., (2014) [26] | Blackwell et al., (2011) [13]; Miyata et al., (2013) [20] | Wilckens et al., (2014) [26] | Miyata et al., (2013) [20]; Wilckens et al., (2014) [26] | Wilckens et al., (2014) [26] | Wilckens et al., (2014) [26] | Blackwell et al., (2011) [13] | ||
| Long | Sig | Blackwell et al., (2011) [13] | |||||||
| NS | Blackwell et al., (2011) [13]; Wilckens et al., (2014) [26] | Blackwell et al., (2011) [13]; Miyata et al., (2013) [20] | Wilckens et al., (2014) [26] | Miyata et al., (2013) [20]; Wilckens et al., (2014) [26] | Wilckens et al., (2014) [26] | Wilckens et al., (2014) [26] | |||
| Total | Sig | Blackwell et al., (2006) [12] | |||||||
| NS | Blackwell et al., (2006) [12]; Lambaise et al., (2014) [16]; Wilckens et al., (2014) [26] | Blackwell et al., (2006) [12]; Lambaise et al., (2014) [16] | Wilckens et al., (2014) [26] | Wilckens et al., (2014) [26] | Lambaise et al., (2014) [16]; Wilckens et al., (2014) [26] | Lambaise et al., (2014) [16]; Wilckens et al., (2014) [26] | |||
| General Sleep Problems | Sig | Lim et al., (2013) [35] | |||||||
| NS | |||||||||
3.1. Sleep Latency
3.2. Wake after Sleep Onset
3.3. Sleep Efficiency
3.4. Sleep Duration
3.5. General Sleep Problems
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Salthouse, T. Consequences of age-related cognitive declines. Annu. Rev. Psychol. 2012, 63, 201–226. [Google Scholar] [CrossRef] [PubMed]
- Ohayon, M.M.; Carskadon, M.A.; Guilleminault, C.; Vitiello, M.V. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the human lifespan. Sleep 2004, 27, 1255–1273. [Google Scholar] [PubMed]
- Glisky, E.L. Changes in cognitive function in human aging. In Brain Aging: Models, Methods, and Mechanisms; Riddle, D.R., Ed.; CRC Press: Boca Raton, FL, USA, 2007. [Google Scholar]
- Vitiello, M.V. Sleep in normal aging. Sleep Med. Clin. 2006, 1, 171–176. [Google Scholar] [CrossRef]
- Shapiro, C.M.; Flanigan, M.J. ABC of sleep disorders. Function of sleep. BMJ 1993, 306, 383–385. [Google Scholar] [CrossRef] [PubMed]
- National Heart, Lung, and Blood Institute. Why is sleep important? Available online: http://www.nhlbi.nih.gov/health/health-topics/topics/sdd/why.html (accessed on 1 March 2015).
- Cricco, M.; Simonsick, E.M.; Foley, D.J. The impact of insomnia on cognitive functioning in older adults. J. Am. Geriatr. Soc. 2001, 49, 1185–1189. [Google Scholar] [CrossRef] [PubMed]
- Stickgold, R. Sleep-dependent memory consolidation. Nature 2005, 437, 1272–1278. [Google Scholar] [CrossRef] [PubMed]
- Scullin, M.K.; Bliwise, D.L. Sleep, cognition, and normal aging: Integrating a half century of multidisciplinary research. Perspect. Psychol. Sci. 2015, 10, 97–137. [Google Scholar] [CrossRef] [PubMed]
- Yaffe, K.; Falvey, C.M.; Hoang, T. Connections between sleep and cognition in older adults. Lancet Neurol. 2014, 13, 1017–1028. [Google Scholar] [CrossRef]
- Ramos, A.R.; Dong, C.; Elkind, M.S.; Boden-Albala, B.; Sacco, R.L.; Rundek, T.; Wright, C.B. Association between sleep duration and the mini-mental score: The northern manhattan study. J. Clin. Sleep Med. 2013, 9, 669–673. [Google Scholar] [CrossRef] [PubMed]
- Blackwell, T.; Yaffe, K.; Ancoli-Israel, S.; Scheider, J.L.; Cauley, J.A.; Hillier, T.A.; Fink, H.A.; Stone, K.L.; Grp, S.O.F. Poor sleep is associated with impaired cognitive function in older women: The study of osteoporotic fractures. J. Gerontol. Ser. A 2006, 61, 405–410. [Google Scholar] [CrossRef]
- Blackwell, T.; Yaffe, K.; Ancoli-Israel, S.; Redline, S.; Ensrud, K.E.; Stefanick, M.L.; Laffan, A.; Stone, K.L.; Osteoporotic Fractures in Men Study Group. Associations between sleep architecture and sleep-disordered breathing and cognition in older community-dwelling men: The osteoporotic fractures in men sleep study. J. Am. Geriatr. Soc. 2011, 59, 2217–2225. [Google Scholar] [CrossRef] [PubMed]
- Devore, E.E.; Grodstein, F.; Duffy, J.F.; Stampfer, M.J.; Czeisler, C.A.; Schernhammer, E.S. Sleep duration in midlife and later life in relation to cognition. J. Am. Geriatr. Soc. 2014, 62, 1073–1081. [Google Scholar] [CrossRef] [PubMed]
- Tworoger, S.S.; Lee, S.; Schernhammer, E.S.; Grodstein, F. The association of self-reported sleep duration, difficulty sleeping, and snoring with cognitive function in older women. Alzheimer Dis. Assoc. Disord. 2006, 20, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Lambiase, M.J.; Gabriel, K.P.; Kuller, L.H.; Matthews, K.A. Sleep and executive function in older women: The moderating effect of physical activity. J. Gerontol. A 2014, 69, 1170–1176. [Google Scholar] [CrossRef] [PubMed]
- Schmutte, T.; Harris, S.; Levin, R.; Zweig, R.; Katz, M.; Lipton, R. The relation between cognitive functioning and self-reported sleep complaints in nondemented older adults: Results from the bronx aging study. Behav. Sleep Med. 2007, 5, 39–56. [Google Scholar] [CrossRef] [PubMed]
- Saint Martin, M.; Sforza, E.; Barthelemy, J.C.; Thomas-Anterion, C.; Roche, F. Does subjective sleep affect cognitive function in healthy elderly subjects? The proof cohort. Sleep Med. 2012, 13, 1146–1152. [Google Scholar] [CrossRef] [PubMed]
- Nebes, R.D.; Buysse, D.J.; Halligan, E.M.; Houck, P.R.; Monk, T.H. Self-reported sleep quality predicts poor cognitive performance in healthy older adults. J. Gerontol. B 2009, 64, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Miyata, S.; Noda, A.; Iwamoto, K.; Kawano, N.; Okuda, M.; Ozaki, N. Poor sleep quality impairs cognitive performance in older adults. J. Sleep Res. 2013, 22, 535–541. [Google Scholar] [CrossRef] [PubMed]
- Chang-Quan, H.; Bi-Rong, D.; Yan, Z. Association between sleep quality and cognitive impairment among chinese nonagenarians/centenarians. J. Clin. Neurophysiol. 2012, 29, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Auyeung, T.W.; Lee, J.S.W.; Leung, J.; Kwok, T.; Leung, P.C.; Woo, J.; Wing, Y.K. Cognitive deficit is associated with phase advance of sleep-wake rhythm, daily napping, and prolonged sleep duration—A cross-sectional study in 2947 community-dwelling older adults. Age 2013, 35, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Keage, H.A.; Banks, S.; Yang, K.L.; Morgan, K.; Brayne, C.; Matthews, F.E. What sleep characteristics predict cognitive decline in the elderly? Sleep Med. 2012, 13, 886–892. [Google Scholar] [CrossRef] [PubMed]
- Potvin, O.; Lorrain, D.; Forget, H.; Dubé, M.; Grenier, S.; Préville, M.; Hudon, C. Sleep quality and 1-year incident cognitive impairment in community-dwelling older adults. Sleep 2012, 35, 491–499. [Google Scholar] [CrossRef] [PubMed]
- Jaussent, I.; Bouyer, J.; Ancelin, M.-L.; Berr, C.; Foubert-Samier, A.; Ritchie, K.; Ohayon, M.M.; Besset, A.; Dauvilliers, Y. Excessive sleepiness is predictive of cognitive decline in the elderly. Sleep 2012, 35, 1201–1207. [Google Scholar] [CrossRef] [PubMed]
- Wilckens, K.A.; Woo, S.G.; Kirk, A.R.; Erickson, K.I.; Wheeler, M.E. Role of sleep continuity and total sleep time in executive function across the adult lifespan. Psychol. Aging 2014, 29, 658–665. [Google Scholar] [CrossRef] [PubMed]
- McCrae, C.S.; Vatthauer, K.E.; Dzierzewski, J.M.; Marsiske, M. Habitual sleep, reasoning, and processing speed in older adults with sleep complaints. Cogn. Ther. Res. 2012, 36, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Benito-León, J.; Louis, E.D.; Bermejo-Pareja, F. Cognitive decline in short and long sleepers: A prospective population-based study (NEDICES). J. Psychiatr. Res. 2013. [Google Scholar] [CrossRef] [PubMed]
- Virta, J.J.; Heikkila, K.; Perola, M.; Koskenvuo, M.; Raiha, I.; Rinne, J.O.; Kaprio, J. Midlife sleep characteristics associated with late life cognitive function. Sleep 2013, 36, 1533–1541. [Google Scholar] [CrossRef] [PubMed]
- Loerbroks, A.; Debling, D.; Amelang, M.; Sturmer, T. Nocturnal sleep duration and cognitive impairment in a population-based study of older adults. Int. J. Geriatr. Psychiatry 2010, 25, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Jiang, C.Q.; Lam, T.H.; Zhang, W.S.; Cherny, S.S.; Thomas, G.N.; Cheng, K.K. Sleep duration and memory in the elderly chinese: Longitudinal analysis of the guangzhou biobank cohort study. Sleep 2014, 37, 1737–1744. [Google Scholar] [CrossRef] [PubMed]
- Ohayon, M.M.; Vecchierini, M.F. Daytime sleepiness and cognitive impairment in the elderly population. Arch. Intern. Med. 2002, 162, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Faubel, R.; López-García, E.; Guallar-Castillón, P.; Graciani, A.; Banegas, J.R.; Rodríguez-Artalejo, F. Usual sleep duration and cognitive function in older adults in spain. J. Sleep Res. 2009, 18, 427–435. [Google Scholar] [CrossRef] [PubMed]
- Sampaio, R.A.C.; Sewo Sampaio, P.Y.; Yamada, M.; Tsuboyama, T.; Arai, H. Self-reported quality of sleep is associated with bodily pain, vitality and cognitive impairment in japanese older adults. Geriatr. Gerontol. Int. 2014, 14, 628–635. [Google Scholar] [CrossRef] [PubMed]
- Lim, A.S.; Kowgier, M.; Yu, L.; Buchman, A.S.; Bennett, D.A. Sleep fragmentation and the risk of incident alzheimer’s disease and cognitive decline in older persons. Sleep 2013, 36, 1027–1032. [Google Scholar] [CrossRef] [PubMed]
- Foley, D.; Monjan, A.; Masaki, K.; Ross, W.; Havlik, R.; White, L.; Launer, L. Daytime sleepiness is associated with 3-year incident dementia and cognitive decline in older japanese-american men. J. Am. Geriatr. Soc. 2001, 49, 1628–1632. [Google Scholar] [CrossRef] [PubMed]
- Gamaldo, A.A.; Allaire, J.C.; Whitfield, K.E. Exploring the within-person coupling of sleep and cognition in older african americans. Psychol. Aging 2010, 25, 851–857. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, M.E.; Bigal, M.E.; Katz, M.J.; Brickman, A.M.; Lipton, R.B. Sleep onset/maintenance difficulties and cognitive function in nondemented older adults: The role of cognitive reserve. J. Int. Neuropsychol. Soc. 2012, 18, 461–470. [Google Scholar] [CrossRef] [PubMed]
- Sutter, C.; Zollig, J.; Allemand, M.; Martin, M. Sleep quality and cognitive function in healthy old age: The moderating role of subclinical depression. Neuropsychology 2012, 26, 768–775. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F., 3rd; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Clark, C.A.; Nelson, J.M.; Garza, J.; Sheffield, T.D.; Wiebe, S.A.; Espy, K.A. Gaining control: Changing relations between executive control and processing speed and their relevance for mathematics achievement over course of the preschool period. Front. Psychol. 2014. [Google Scholar] [CrossRef] [PubMed]
- Dickinson, D.; Coursey, R.D. Independence and overlap among neurocognitive correlates of community functioning in schizophrenia. Schizophr. Res. 2002, 56, 161–170. [Google Scholar] [CrossRef]
- Ayas, N.T.; White, D.P.; Manson, J.E.; Stampfer, M.J.; Speizer, F.E.; Malhotra, A.; Hu, F.B. A prospective study of sleep duration and coronary heart disease in women. Arch. Intern. Med. 2003, 163, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Sabanayagam, C.; Shankar, A. Sleep duration and cardiovascular disease: Results from the national health interview survey. Sleep 2010, 33, 1037–1042. [Google Scholar] [PubMed]
- Pace-Schott, E.F.; Spencer, R.M. Age-related changes in the cognitive function of sleep. Prog. Brain Res. 2011, 191, 75–89. [Google Scholar] [PubMed]
- Morgenthaler, T.; Alessi, C.; Friedman, L.; Owens, J.; Kapur, V.; Boehlecke, B.; Brown, T.; Chesson, A., Jr.; Coleman, J.; Lee-Chiong, T.; et al. Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: An update for 2007. Sleep 2007, 30, 519–529. [Google Scholar] [PubMed]
- Kushida, C.A.; Littner, M.R.; Morgenthaler, T.; Alessi, C.A.; Bailey, D.; Coleman, J., Jr.; Friedman, L.; Hirshkowitz, M.; Kapen, S.; Kramer, M.; et al. Practice parameters for the indications for polysomnography and related procedures: An update for 2005. Sleep 2005, 28, 499–521. [Google Scholar] [PubMed]
- National Sleep Foundation (NSF). 2003 Sleep in America Poll; NSF: Arlington, VA, 2003. [Google Scholar]
- Snowden, M.; Steinman, L.; Mochan, K.; Grodstein, F.; Prohaska, T.R.; Thurman, D.J.; Brown, D.R.; Laditka, J.N.; Soares, J.; Zweiback, D.J.; et al. Effect of exercise on cognitive performance in community-dwelling older adults: Review of intervention trials and recommendations for public health practice and research. J. Am. Geriatr. Soc. 2011, 59, 704–716. [Google Scholar] [CrossRef] [PubMed]
- Thomas, A.J.; O’Brien, J.T. Depression and cognition in older adults. Curr. Opin. Psychiatry 2008, 21, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Aloia, M.S.; Ilniczky, N.; di Dio, P.; Perlis, M.L.; Greenblatt, D.W.; Giles, D.E. Neuropsychological changes and treatment compliance in older adults with sleep apnea. J. Psychosom. Res. 2003, 54, 71–76. [Google Scholar] [CrossRef]
- Steffens, D.C.; Otey, E.; Alexopoulos, G.S.; Butters, M.A.; Cuthbert, B.; Ganguli, M.; Geda, Y.E.; Hendrie, H.C.; Krishnan, R.R.; Kumar, A.; et al. Perspectives on depression, mild cognitive impairment, and cognitive decline. Arch. Gen. Psychiatry 2006, 63, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Denton, F.T.; Spencer, B.G. Chronic health conditions: Changing prevalence in an aging population and some implications for the delivery of health care services. Can. J. Aging 2010, 29, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Wolff, J.L.; Starfield, B.; Anderson, G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch. Intern. Med. 2002, 162, 2269–2276. [Google Scholar] [CrossRef] [PubMed]
- Kronholm, E.; Sallinen, M.; Suutama, T.; Sulkava, R.; Era, P.; Partonen, T. Self-reported sleep duration and cognitive functioning in the general population. J. Sleep Res. 2009, 18, 436–446. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brewster, G.S.; Varrasse, M.; Rowe, M. Sleep and Cognition in Community-Dwelling Older Adults: A Review of Literature. Healthcare 2015, 3, 1243-1270. https://doi.org/10.3390/healthcare3041243
Brewster GS, Varrasse M, Rowe M. Sleep and Cognition in Community-Dwelling Older Adults: A Review of Literature. Healthcare. 2015; 3(4):1243-1270. https://doi.org/10.3390/healthcare3041243
Chicago/Turabian StyleBrewster, Glenna S., Miranda Varrasse, and Meredeth Rowe. 2015. "Sleep and Cognition in Community-Dwelling Older Adults: A Review of Literature" Healthcare 3, no. 4: 1243-1270. https://doi.org/10.3390/healthcare3041243
APA StyleBrewster, G. S., Varrasse, M., & Rowe, M. (2015). Sleep and Cognition in Community-Dwelling Older Adults: A Review of Literature. Healthcare, 3(4), 1243-1270. https://doi.org/10.3390/healthcare3041243






