The Role of Sustainability in Telemedicine Services: The Case of the Greek National Telemedicine Network
Abstract
1. Introduction
- What is the current theoretical background that arises from the literature review regarding telemedicine and sustainability?
- What are the potential challenges?
- Can a mutual conceptual framework be created with respect to the characteristics of the current governance model of telemedicine?
2. Theoretical Background
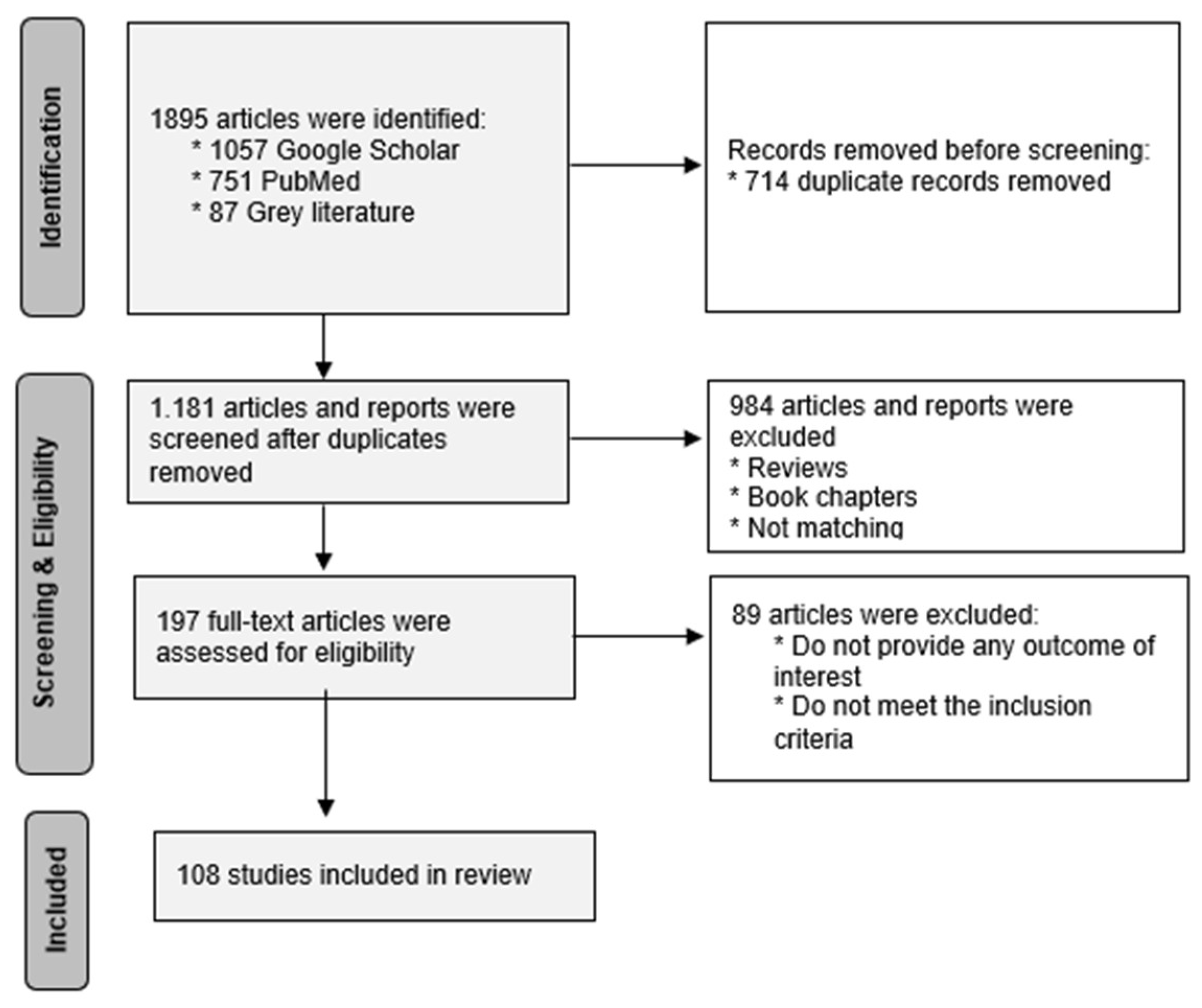
2.1. Methodology of Our Research
2.2. Challenges and Expected Positive Outcomes of Telemedicine
2.3. The National Telemedicine Network in Greece (EDIT)
- Sixty-six Patient-Doctor Telemedicine Stations (PDTS), situated in hospitals, health centers, and multipurpose regional clinics.
- Twenty-one Consultant Telemedicine Stations (CTS), located across 12 regional and tertiary hospitals in the 2nd Greek Health Region (HR), as well as in the National Emergency Centre (NEC).
- Over 170 Home Care Stations (HCS) installed in patient homes or social care facilities within the 2nd Greek HR’s jurisdiction.
- Three hundred and fifty-five new Patient–Doctor Telemedicine Stations (PDTS) to be deployed in selected healthcare facilities across the country.
- Thirty-five additional Consultant Telemedicine Stations (CTS), strategically placed based on healthcare facility capacity and operational needs.
- Five Telemedicine Training Centers, equipped with both CTS and PDTS technology, to train healthcare professionals in university hospitals nationwide.
- Three thousand Home Monitoring Systems (HCS), integrated with EDIT and its supporting software, to improve remote patient monitoring.
- Three new regional Control Centers and a centralized Command and Control Center at the Ministry of Health to oversee telemedicine operations.
3. Results
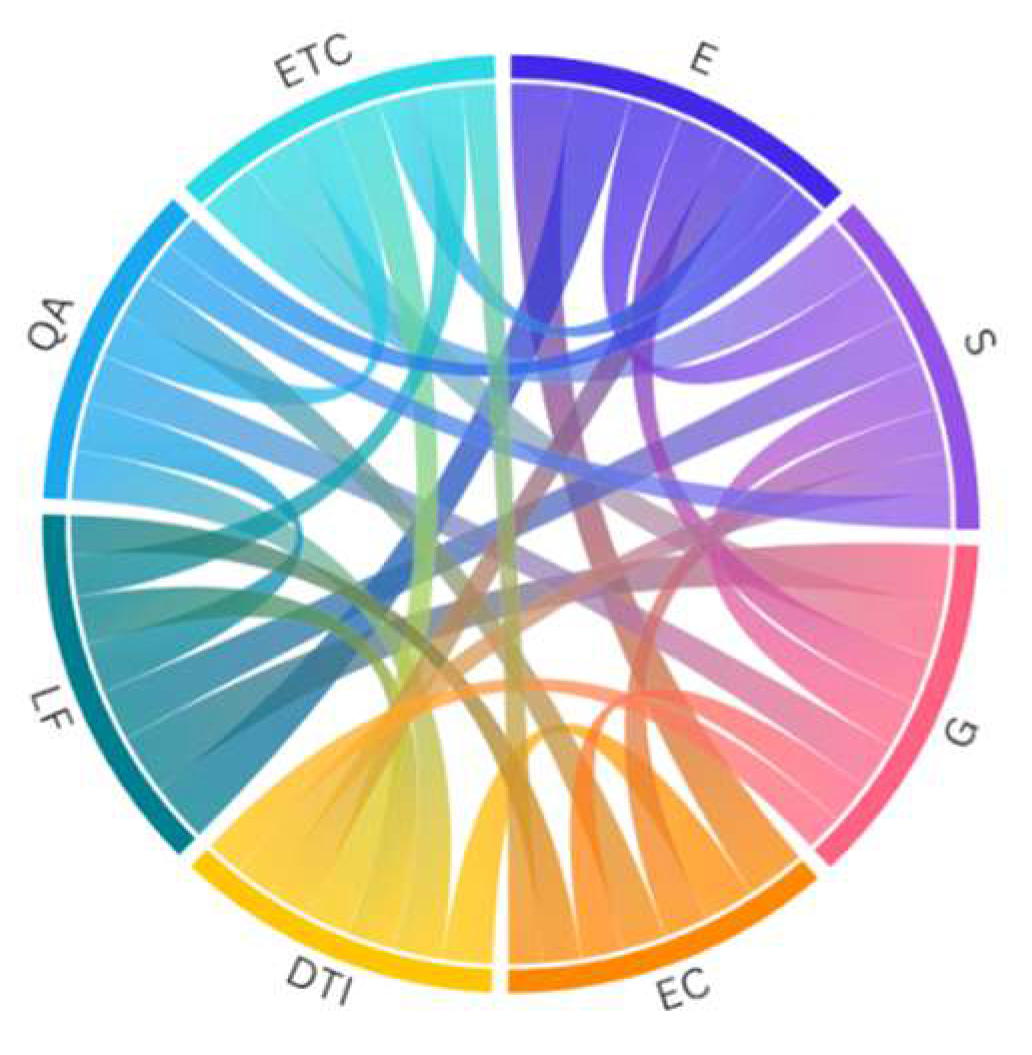
3.1. Fundamental Pillars of a Proper Sustainable Telemedicine Framework
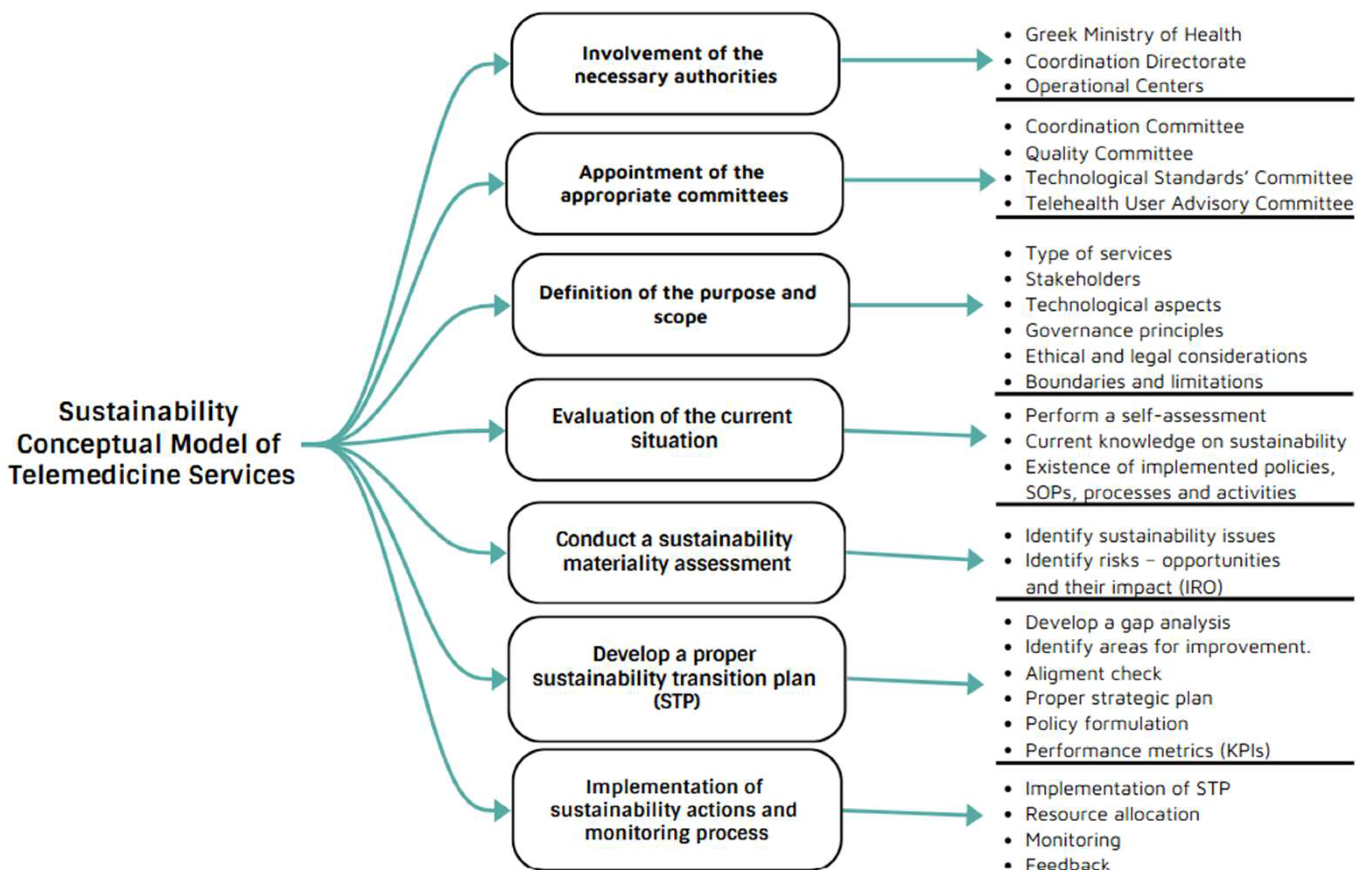
3.2. The Proposed Methodology for Developing a Sustainability Plan in Telemedicine Services in Greece
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| EDIT | National Telemedicine Network in Greece |
| HCOs | Healthcare organizations |
| SDGs | Sustainable Development Goals |
| ICT | information and communication technology |
| PDTS | Patient-Doctor Telemedicine Stations |
| CTS | Consultant Telemedicine Stations |
| HR | Health Region |
| DTI | Digital Transformation and Innovation |
| QA | Quality assurance |
| SOP | Standard operating procedure |
| IRO | Impact—risk and opportunities |
| KPIs | Key performance indicators |
| ESG | Environmental, Social, and Governance |
Appendix A
| Environment (E) Aspect | ||
| Code | Factor | Proposed KPI |
| EC001 | Energy Efficiency and Renewable Energy | Percentage of total energy from renewable sources. |
| EC002 | Waste Management and Reduction | Percentage of medical waste recycled or safely treated. |
| EC003 | Water Conservation and Management | Volume of water used per patient per day. |
| EC004 | Transportation and Mobility | Percentage reduction in fuel-based transportation emissions. |
| EC005 | Reduction in Hazardous Chemicals | Percentage of non-toxic, biodegradable cleaning products used. |
| Social (S) Aspect | ||
| Code | Factor | Proposed KPI |
| SC001 | Patient Safety and Quality of Care | Number of adverse events per 1000 patients. |
| SC002 | Health Equity and Accessibility | Percentage of underserved patients receiving care. |
| SC003 | Community Engagement and Public Health Programs | Number of community health initiatives per year. |
| SC004 | Ethical Patient Treatment and Informed Consent | Percentage of patients receiving informed consent before procedures. |
| SC005 | Patient Rights and Complaint Handling | Average resolution time for patient complaints. |
| Governance (G) Aspect | ||
| Code | Factor | Proposed KPI |
| GC001 | Regulatory Compliance | Number of compliance violations per year. |
| GC002 | Patient Safety and Quality Care | Hospital-acquired infection rate (HAI) per 1000 patient days. |
| GC003 | Data Governance and Security | Percentage of staff trained on data security protocols annually. |
| GC004 | Stakeholder Engagement and Transparency | Patient satisfaction score (measured via surveys). |
| GC005 | Patient Experience and Engagement | Patient engagement index or satisfaction scores. |
| Economic (EC) Aspect | ||
| Code | Factor | Proposed KPI |
| EcC001 | Cost Efficiency and Resource Allocation | Cost per patient treated (cost per session). |
| EcC002 | Operational Budget Management | Percentage of budget variance (actual vs. planned). |
| EcC003 | Cost-Effectiveness of Interventions | Amount of money that was saved due to the intervention |
| EcC004 | Financial Risk Management | Percentage of revenue protected through risk management strategies |
| EcC005 | Return on Investment (ROI) for Healthcare Services | ROI of preventive health programs. |
| Digital Transformation and Innovation (DTI) Aspect | ||
| Code | Factor | Proposed KPI |
| DTI001 | Return on digital investments | RODI = Net Benefits from Digital Investments/Total Digital Investment Cost × 100 |
| DTI002 | Revenue from new digital channels | Revenue from New Digital Channels = ∑Sales/Revenue from New Digital Platforms |
| DTI003 | Adoption and performance metrics | User Adoption Rate = Active Users/Total Target Users × 100 |
| DTI004 | Revenue from digital technology | Revenue from Digital Technology = ∑Revenue from Digital Products, Services, and Platforms |
| DTI005 | Actions performed to address digital illiteracy of patients | Patients Trained = ∑ Patients Who Completed Digital Literacy Programs |
| Legal Framework (LF) Aspect | ||
| Code | Factor | Proposed KPI |
| LF001 | Regulatory Compliance | Compliance Rate = (Telemedicine Services Compliant with Regulations/Total Telemedicine Services) × 100 |
| LF002 | Licensing and Credentialing | Licensing Compliance Rate = (Licensed Providers/Total Providers) × 100 |
| LF003 | Reimbursement and Payment Compliance | Reimbursement Rate = (Reimbursed Claims/Total Claims Submitted) × 100 |
| Quality Assurance (QA) Aspect | ||
| Code | Factor | Proposed KPI |
| QA001 | Clinical Quality and Effectiveness | Diagnosis Accuracy = (Correct Diagnoses/Total Diagnoses) × 100 |
| QA002 | Patient Satisfaction and Experience | PS = (Positive Responses from Patients/Total Responses) × 100 |
| QA003 | Patient Outcomes and Follow-Up Care | Follow-up Rate = (Scheduled Follow-up Appointments/Total Consultations) × 100 |
| Ethical Considerations (ETC) Aspect | ||
| Code | Factor | Proposed KPI |
| ECN001 | Patient Privacy and Confidentiality | Privacy Compliance Rate = (Compliant Systems/Total Systems) × 100 |
| ECN002 | Informed Consent | Informed Consent Rate = (Patients Who Signed Consent/Total Patients) × 100 |
| ECN003 | Accountability and Transparency | Documentation Transparency Rate = (Consultations Documented Clearly and Accurately/Total Consultations) × 100 |
| ECN004 | Cultural Sensitivity and Respect for Diversity | Training Rate = (Providers Who Received Cultural Sensitivity Training/Total Providers) × 100 |
References
- Atia, N.G.; Bassily, M.A.; Elamer, A.A. Do life-cycle costing and assessment integration support decision-making towards sustainable development? J. Clean. Prod. 2020, 267, 122056. [Google Scholar] [CrossRef]
- Turner, D.A.; Williams, I.D.; Kemp, S. Combined material flow analysis and life cycle assessment as a support tool for solid waste management decision making. J. Clean. Prod. 2016, 129, 234e248. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, M.; Zhang, H.; Jiang, Z.; Liu, C.; Cai, W. A review on energy, environment and economic assessment in remanufacturing based on life cycl assessment method. J. Clean. Prod. 2020, 255, 120160. [Google Scholar] [CrossRef]
- Garzoni, A.; L’Abate, V.; Raimo, N.; Vitolla, F. Exploring online sustainability disclosure in the healthcare industry: Evidence from best international hospitals. Bus. Strategy Environ. Wiley Blackwell 2024, 33, 2669–2682. [Google Scholar] [CrossRef]
- Rodriguez, R.; Svensson, G.; Wood, G. Sustainability trends in public hospitals: Efforts and priorities. Eval. Program. Plan. 2020, 78, 101742. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.K.; Murty, H.R.; Gupta, S.K.; Dikshit, A.K. An overview of sustainability assessment methodologies. Ecol. Indic. 2012, 15, 281–299. [Google Scholar] [CrossRef]
- Andrades, J.; Martinez-Martinez, D.; Larrán Jorge, M. Corporate governance disclosures by Spanish universities: How different variables can affect the level of such disclosures? Meditari Account. Res. 2021, 29, 86–109. [Google Scholar] [CrossRef]
- Creixans-Tenas, J.; Coenders, G.; Arimany-Serrat, N. Corporate social responsibility and financial profile of Spanish private hospitals. Heliyon 2019, 5, e02623. [Google Scholar] [CrossRef]
- Brandao, C.; Rego, G.; Duarte, I.; Nunes, R. Social responsibility: A new paradigm of hospital governance? Health Care Anal. 2013, 21, 390–402. [Google Scholar] [CrossRef]
- Jones, K.R.; Mucha, L. Sustainability assessment and reporting for nonprofit organizations: Accountability “for the public good”. Volunt. Int. J. Volunt. Nonprofit Organ. 2014, 25, 1465–1482. [Google Scholar] [CrossRef]
- Rahat, N.; Sahni, S.; Nasim, S. Mapping sustainability practices in the healthcare sector: A systematic literature review and future research agenda. Int. J. Consum. Stud. 2023, 48, e12997. [Google Scholar] [CrossRef]
- Hensher, B.M.; Mcgain, F. Health care sustainability metrics: Building a safer. Low-Carbon. Health Syst. 2020, 12, 2080–2087. [Google Scholar]
- Olawumi, T.O.; Chan, D.W.M. Critical success factors for implementing building information modeling and sustainability practices in construction projects: A Delphi survey. Sustain. Dev. 2019, 27, 587–602. [Google Scholar] [CrossRef]
- Wang, S.H.; Song, M.L. Review of hidden carbon emissions, trade, and labor income share in China, 2001–2011. Energy Policy 2014, 74, 395–405. [Google Scholar] [CrossRef]
- Salemi, J.L.; Salinas-Miranda, A.A.; Wilson, R.E.; Salihu, H.M. Transformative use of an improved all-payer hospital discharge data infrastructure for community-based participatory research: A sustainability pathway. Health Serv. Res. 2015, 50, 1322–1338. [Google Scholar] [CrossRef] [PubMed]
- Sepetis, A.; Rizos, F.; Pierrakos, G.; Karanikas, H.; Schallmo, D. A Sustainable Model for Healthcare Systems: The Innovative Approach of ESG and Digital Transformation. Healthcare 2024, 12, 156. [Google Scholar] [CrossRef]
- Mostepaniuk, A.; Akalin, T.; Parish, M.R. Practices Pursuing the Sustainability of A Healthcare Organization: A Systematic Review. Sustainability 2023, 15, 2353. [Google Scholar] [CrossRef]
- European Parliament; Council of the EU. Regulation (EU) 2020/852 of the European Parliament and of the Council of 18 June 2020 on the Establishment of a Framework to Facilitate Sustainable Investment, and Amending Regulation (EU) 2019/2088. 2020. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A32020R0852 (accessed on 12 December 2024).
- European Commission. The European Green Deal. COM (2019) 640 Final. 2019. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=celex:52019DC0640 (accessed on 12 December 2024).
- Cheba, K.; Bąk, I.; Szopik-Depczyńska, K.; Ioppolo, G. Directions of green transformation of the European Union countries. Ecol. Indic. 2022, 136, 108601. [Google Scholar] [CrossRef]
- Jameton, A.; Pierce, J. Environment and health: 8. Sustainable health care and emerging ethical responsibilities. Can. Med. Assoc. J. 2001, 164, 365–369. [Google Scholar]
- Marimuthu, M.; Paulose, H. Emergence of sustainability based approaches in healthcare: Expanding research and practice. Procedia Soc. Behav. Sci. 2016, 224, 554–561. [Google Scholar] [CrossRef]
- Manisalidis, I.; Stavropoulou, E.; Stavropoulos, A.; Bezirtzoglou, E. Environmental and health impacts of air pollution: A review. Front. Public Health 2020, 8, 14. [Google Scholar] [CrossRef] [PubMed]
- Rodler, S.; Ramacciotti, L.S.; Maas, M.; Mokhtar, D.; Hershenhouse, J.; De Castro Abreu, A.L.; Fuchs, G.; Stief, C.G.; Gill, I.S.; Cacciamani, G.E. The Impact of Telemedicine in Reducing the Carbon Footprint in Health Care: A Systematic Review and Cumulative Analysis of 68 Million Clinical Consultations. Eur. Urol. Focus 2023, 9, 873–887. [Google Scholar] [CrossRef]
- Babar, M.; Zhu, D.; Loloi, J.; Laudano, M.; Ohmann, E.; Abraham, N.; Small, A.C.; Watts, K.L. comparison of patient satisfaction and safety outcomes for postoperative telemedicine vs face-to-face visits in urology: Results of the Randomized Evaluation and Metrics Observing Telemedicine Efficacy (REMOTE) trial. Urol. Pract. 2022, 9, 371–378. [Google Scholar] [CrossRef]
- Klee, D.; Pyne, D.; Kroll, J.; James, W.; Hirko, K.A. Rural patient and provider perceptions of telehealth implemented during the COVID- 19 pandemic. BMC Health Serv. Res. 2023, 23, 981. [Google Scholar] [CrossRef] [PubMed]
- Hoff, T.; Lee, D.R. Physician satisfaction with telehealth: A systematic review and agenda for future research. Qual. Manag. Health Care 2022, 31, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Lu, W.; Wei, D.; Li, C.; Gao, P.; Ma, R.; Zhai, Y.; Wang, C. How to promote telemedicine patient adoption behavior for greener healthcare? J. Clean. Prod. 2024, 434, 139884. [Google Scholar] [CrossRef]
- Holmner, A.; Ebi, K.L.; Lazuardi, L.; Nilsson, M. Carbon footprint of telemedicine solutions-unexplored opportunity for reducing carbon emissions in the health sector. PLoS ONE 2014, 9, e105040. [Google Scholar] [CrossRef]
- Holmner, A.; Rocklov, J.; Ng, N.; Nilsson, M. Climate change and eHealth: A promising strategy for health sector mitigation and adaptation. Glob. Health Action. 2012, 5, 18428. [Google Scholar] [CrossRef]
- Maciel, P.K.; Peters, C.W.; Lange, C.; Castro, D.S.P.; Braga, J.N.D.; Stolz, P.V. Accessibility and satisfaction of the elderly living in rural areas in relation to the health services. Acta Sci. Health Sci. 2020, 42, 48896. [Google Scholar]
- National Institute for Health and Care Research Global Health Research Unit on Global Surgery. Reducing the environmental impact of surgery on a global scale: Systematic review and co prioritization with healthcare workers in 132 countries. Br. J. Surg. 2023, 110, 804–817. [Google Scholar] [CrossRef]
- Pradere, B.; Mallet, R.; de La Taille, A.; Bladou, F.; Prunet, D.; Beurrier, S.; Bardet, F.; Game, X.; Fournier, G.; Lechevallier, E.; et al. Climate-smart actions in the operating theatre for improving sustainability practices: A systematic review. Eur. Urol. 2023, 83, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Tafuri, A.; Ashrafi, A.N.; Palmer, S.; Shakir, A.; Cacciamani, G.E.; Iwata, A.; Iwata, T.; Cai, J.; Sali, A.; Gupta, C.; et al. One-Stop MRI and MRI/transrectal ultrasound fusion-guided biopsy: An expedited pathway for prostate cancer diagnosis. World J. Urol. 2020, 38, 949–956. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Watson, M. Guidance on Conducting a Systematic Literature Review. J. Plan. Educ. Res. 2019, 39, 93–112. [Google Scholar]
- Tranfield, D.; Denyer, D.; Smart, P. Towards a methodology for developing evidence-informed management knowledge by means of systematic review. Br. J. Manag. 2003, 14, 207–222. [Google Scholar] [CrossRef]
- Chauhan, A.; Jakhar, S.K.; Jabbour, C.J.C. Implications for sustainable healthcare operations in embracing telemedicine services during a pandemic. Technol. Forecast. Soc. Change 2022, 176, 121462. [Google Scholar] [CrossRef]
- Pan, J.; Ding, S.; Wu, D.; Yang, S.; Yang, J. Exploring behavioural intentions toward smart healthcare services among medical practitioners: A technology transfer perspective. Int. J. Prod. Res. 2019, 57, 5801–5820. [Google Scholar] [CrossRef]
- Adenuga, K.I.; Iahad, N.A.; Miskon, S. Towards reinforcing telemedicine adoption amongst clinicians in Nigeria. Int. J. Med. Inform. 2017, 104, 84–96. [Google Scholar] [CrossRef]
- Rubbio, I.; Bruccoleri, M.; Pietrosi, A.; Ragonese, B. Digital health technology enhances resilient behaviour: Evidence from the ward. Int. J. Oper. Prod. Manag. 2020, 40, 34–67. [Google Scholar] [CrossRef]
- Martínez-Caro, E.; Cegarra-Navarro, J.G.; García-P´erez, A.; Fait, M. Healthcare service evolution towards the Internet of Things: An end-user perspective. Technol. Forecast. Soc. Change 2018, 136, 268–276. [Google Scholar] [CrossRef]
- Cobelli, N.; Cassia, F.; Burro, R. Factors affecting the choices of adoption/non-adoption of future technologies during coronavirus pandemic. Technol. Forecast. Soc. Change 2021, 169, 120814. [Google Scholar] [CrossRef]
- Parimbelli, E.; Bottalico, B.; Losiouk, E.; Tomasi, M.; Santosuosso, A.; Lanzola, G.; Quaglini, S.; Bellazzi, R. Trusting telemedicine: A discussion on risks, safety, legal implications and liability of involved stakeholders. Int. J. Med. Inform. 2018, 112, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Xue, Y.; Liang, H.; Mbarika, V.; Hauser, R.; Schwager, P.; Getahun, M.K. Investigating the resistance to telemedicine in Ethiopia. Int. J. Med. Inform. 2015, 84, 537–547. [Google Scholar] [CrossRef] [PubMed]
- Scott Kruse, C.; Karem, P.; Shifflett, K.; Vegi, L.; Ravi, K.; Brooks, M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J. Telemed. Telecare 2018, 24, 4–12. [Google Scholar] [CrossRef]
- Peine, A.; Paffenholz, P.; Martin, L.; Dohmen, S.; Marx, G.; Loosen, S. Telemedicine in Germany during the COVID-19 pandemic: Multi-professional national survey. J. Med. Internet Res. 2020, 22, e19745. [Google Scholar] [CrossRef] [PubMed]
- Kamal, S.A.; Shafiq, M.; Kakria, P. Investigating acceptance of telemedicine services through an extended technology acceptance model (TAM). Technol. Soc. 2020, 60, 101212–101215. [Google Scholar] [CrossRef]
- Jerjes, W.; Harding, D. Telemedicine in the post-COVID era: Balancing accessibility, equity, and sustainability in primary healthcare. Front. Digit. Health 2024, 6, 1432871. [Google Scholar] [CrossRef]
- van Velsen, L.; Tabak, M.; Hermens, H. Measuring patient trust in telemedicine services: Development of a survey instrument and its validation for an anticoagulation web-service. Int. J. Med. Inform. 2017, 97, 52–58. [Google Scholar] [CrossRef]
- Serper, M.; Nunes, F.; Ahmad, N.; Roberts, D.; Metz, D.C.; Mehta, S.J. Positive early patient and clinician experience with telemedicine in an academic gastroenterology practice during the COVID-19 pandemic. Gastroenterology 2020, 159, 1589–1591.e4. [Google Scholar] [CrossRef]
- Rush, K.L.; Howlett, L.; Munro, A.; Burton, L. Videoconference compared to telephone in healthcare delivery: A systematic review. Int. J. Med. Inform. 2018, 118, 44–53. [Google Scholar] [CrossRef]
- Thomas, E.E.; Haydon, H.M.; Mehrotra, A.; Caffery, L.J.; Snoswell, C.L.; Banbury, A.; Smith, A.C. Building on the momentum: Sustaining telehealth beyond COVID-19. J. Telemed. Telecare. 2022, 28, 301–308. [Google Scholar] [CrossRef]
- Samal, P.; Samantaray, S. Balancing Technology and Environmental Responsibility: Leveraging Telemedicine for Sustainable Healthcare Solutions. In Proceedings of the 2024 International Conference on Advancements in Smart, Secure and Intelligent Computing (ASSIC), Bhubaneswar, India, 27–29 January 2024; pp. 1–5. [Google Scholar] [CrossRef]
- Schmidt, L.; Bohnet-Joschko, S. Planetary Health and Hospitals’ Contribution—A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 13536. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Hu, M.; Helm, J.E.; Lavieri, M.S.; Skolarus, T.A. Missed opportunities in preventing hospital readmissions: Redesigning post-discharge checkup policies. Prod. Oper. Manag. 2018, 27, 2226–2250. [Google Scholar] [CrossRef]
- Senot, C.; Chandrasekaran, A.; Ward, P.T. Collaboration between service professionals during the delivery of health care: Evidence from a multiple-case study in US hospitals. J. Oper. Manag. 2016, 42, 67–79. [Google Scholar] [CrossRef]
- Miao, R.; Wu, Q.; Wang, Z.; Zhang, X.; Song, Y.; Zhang, H.; Sun, Q.; Jiang, Z. Factors that influence users’ adoption intention of mobile health: A structural equation modeling approach. Int. J. Prod. Res. 2017, 55, 5801–5815. [Google Scholar] [CrossRef]
- Lu, W.; Hou, H.L.; Ma, R.; Chen, H.T.; Cui, F.F.; Zhang, R.; Cui, F.F.; Zhang, Q.; Gao, Y.C.; Wang, X.P.; et al. Influencing factors of patient satisfaction in teleconsultation: A cross-sectional study. Technol. Forecast. Soc. Change 2021, 168, 120775. [Google Scholar] [CrossRef]
- Patel, K.B.; Gonzalez, B.D.; Turner, K.; Alishahi, T.A.; Rollison, D.E.; Robinson, E.; Naso, C.; Wang, X.; Spiess, P.E. Estimated carbon emissions savings with shifts from in-person visits to telemedicine for patients with cancer. JAMA Netw. Open 2023, 6, e2253788. [Google Scholar] [CrossRef]
- Zhang, X.; Zaman, B.U. Adoption mechanism of telemedicine in underdeveloped country. Health Inf. J. 2020, 26, 1088–1103. [Google Scholar] [CrossRef] [PubMed]
- Bergmo, T.S. Can economic evaluation in telemedicine be trusted? A Systematic Review of the Literature. Cost Eff. Resour. Alloc. 2009, 7, 18. [Google Scholar] [CrossRef]
- Sagaro, G.G.; Battineni, G.; Amenta, F. Barriers to sustainable telemedicine implementation in Ethiopia: A systematic review. Telemed. Rep. 2020, 1, 8–15. [Google Scholar] [CrossRef]
- Sims, J.M. Communities of practice: Telemedicine and online medical communities. Technol. Forecast. Soc. Change 2018, 126, 53–63. [Google Scholar] [CrossRef]
- Liu, J.; Zhang, X.; Meng, F.; Lai, K.H. Deploying gamification to engage physicians in an online health community: An operational paradox. Int. J. Prod. Econ. 2020, 228, 107847. [Google Scholar] [CrossRef]
- Karanikas, H.; Tsoukas, V.; Drakopoulos, D.; Koukoulas, G.; Katsapi, A.; Rizos, F. Assessing Greek National Telemedicine Network. In Proceedings of the eTELEMED 2024: The Sixteenth International Conference on eHealth, Telemedicine, and Social Medicine, Barcelona, Spain, 26–30 May 2024. [Google Scholar]
- Katsapi, A.; Tsana, H.K.M.; Rizos, F.; Tsoukas, V.; Koukoulas, G. Quality and Governance Framework for the National Telemedicine Network in Greece. Int. J. Adv. Life Sci. 2024, 16, 188–195. [Google Scholar]
- Armfield, N.R.; Bradford, M.; Bradford, N.K. The clinical use of Skype—For which patients with which problems in which settings? A snapshot review of the literature. Int. J. Med. Inform. 2015, 84, 737–742. [Google Scholar] [CrossRef] [PubMed]
- Lolich, L.; Ricco, I.; Deusdad, B.; Timonen, V. Embracing technology? Health and social care professionals’ attitudes to the deployment of e-Health initiatives in elder care services in Catalonia and Ireland. Technol. Forecast. Soc. Change 2019, 147, 63–71. [Google Scholar] [CrossRef]
- Portnoy, J.; Waller, M.; Elliott, T. Telemedicine in the Era of COVID-19. J. Allergy Clin. Immunol. Pract. 2020, 8, 1489–1491. [Google Scholar] [CrossRef]
- Mayoka, K.G.; Rwashana, A.S.; Mbarika, V.W.; Isabalija, S. A framework for designing sustainable telemedicine information systems in developing countries. J. Syst. Inf. Technol. 2012, 14, 200–219. [Google Scholar] [CrossRef]
- Oladosu, J.B.; Ajala, A.F.; Popoola, O.O. On the use of web services technology in e-health applications. J. Theor. Appl. Inf. Technol. 2009, 12, 94–103. [Google Scholar]
- Adesina, I. Mobile/wireless eHealth for health system/workers development in Africa: Opportunities for eMobility ETP. In A Research Paper Presented at eMobility Mobile Communications & Technology Platform Staying Ahead! 2nd Workshop on Shaping the Future of Mobile and Wireless Communications: Rome, Italy, 2007. [Google Scholar]
- Rowena, L.L.; Ho, M.; Aoki, P. A Framework for Designing Teleconsultation Systems in Africa; University of California: Berkeley, CA, USA, 2009. [Google Scholar]
- Zlatko, S.; Vrček, N.; Hajdin, G. Legislative Framework for Telemedicine; Faculty of Organization and Informatics, University of Zagreb: Varaždin, Croatia, 2007. [Google Scholar]
- Oll, J.; Spandel, T.; Schiemann, F.; Akkermann, J. The Concept of Materiality in Sustainability Reporting: From Essential Contestation to Research Opportunities. Sustain. Account. Manag. Policy J. 2025, 16, 321–350. [Google Scholar] [CrossRef]
- Gerwanski, J.; Kordsachia, O.; Velte, P. Determinants of materiality disclosure quality in integrated reporting: Empirical evidence froman international setting. Bus. Strategy Environ. 2019, 28, 750–770. [Google Scholar] [CrossRef]
- Karagiannis, I.; Vouros, P.; Skouloudis, A.; Evangelinos, K. Sustainability reporting, materiality, and accountability assessment in the airport industry. Bus. Strategy Environ. 2019, 28, 1370–1405. [Google Scholar] [CrossRef]
- Saenz, C. Creating shared value using materiality analysis: Strategies from themining industry. Corp. Soc. Responsib. Environ. 2019, 26, 1351–1360. [Google Scholar] [CrossRef]
- Abhayawansa, S. Swimming against the tide: Back to single materiality for sustainability reporting. Sustain. Account. Manag. Policy J. 2022, 13, 1361–1385. [Google Scholar] [CrossRef]
- Hahn, R.; Reimsbach, D.; Wickert, C. Nonfinancial reporting and real sustainable change: Relationship status—It’s complicated. Organ. Environ. 2023, 36, 3–16. [Google Scholar] [CrossRef]
- Clark Clark, C.E. How do standard setters define materiality and why does itmatter? Bus. Ethics Environ. Responsib. 2021, 30, 378–391. [Google Scholar] [CrossRef]
- Edgley, C.; Jones, M.J.; Atkins, J. The adoption of the materiality concept in social and environmental reporting assurance: A field study approach. Br. Account. Rev. 2015, 47, 1–18. [Google Scholar] [CrossRef]
- Adams, C.A.; Abhayawansa, S. Connecting the COVID-19 pandemic, environmental, social and governance (ESG) investing and calls for ‘harmonisation’ of sustainability reporting. Crit. Perspect. Account. 2022, 82, 102309. [Google Scholar] [CrossRef]
- Christensen, H.B.; Hail, L.; Leuz, C. Mandatory CSR and sustainability reporting: Economic analysis and literature review. Rev. Account. Stud. 2021, 26, 1176–1248. [Google Scholar] [CrossRef]
- Fasan, M.; Mio, C. Fostering stakeholder engagement: The role of materiality disclosure in integrated reporting. Bus. Strategy Environ. 2017, 26, 288–305. [Google Scholar] [CrossRef]
- Gibbons, B. The financially material effects of mandatory nonfinancial disclosure. J. Account. Res. 2023, 62, 12499. [Google Scholar] [CrossRef]
- Grewal, J.; Hauptmann, C.; Serafeim, G. Material sustainability information and stock price informativeness. J. Bus. Ethics 2021, 171, 513–544. [Google Scholar] [CrossRef]
- Khan, M.; Serafeim, G.; Yoon, A. Corporate sustainability: First evidence on materiality. Account. Rev. 2016, 91, 1697–1724. [Google Scholar] [CrossRef]
- Puroila, J.; Mäkelä, H. Matter of opinion: Exploring the socio-political nature of materiality disclosures in sustainability reporting. Account. Audit. Account. J. 2019, 32, 1043–1072. [Google Scholar] [CrossRef]
- Schiehll, E.; Kolahgar, S. Financial materiality in the informativeness of sustainability reporting. Bus. Strategy Environ. 2021, 30, 840–855. [Google Scholar] [CrossRef]
- Hevner, A.R. A three cycle view of design science. Scand. J. Inf. Syst. 2007, 19, 87–92. [Google Scholar]
- Hevner, A.R.; March, S.T.; Park, J.; Ram, S. Design science in information systems research. MIS Q. 2004, 24, 75–105. [Google Scholar] [CrossRef]
- Government of Netherlands: E-health. Available online: https://www.government.nl/topics/ehealth (accessed on 18 April 2025).
- World Health Organization. The Rise of Telehealth in the European Region: Insights from Norway. Available online: https://www.who.int/europe/news/item/10-10-2024-the-rise-of-telehealth-in-the-european-region--insights-from-norway (accessed on 18 April 2025).
- Swedish eHealth Agency. Available online: https://www.ehalsomyndigheten.se/languages/english/welcome-to-the-swedish-ehealth-agency/ (accessed on 18 April 2025).
- Telemedicine in Estonia. Available online: http://telemedicine-momentum.eu/estonia/ (accessed on 18 April 2025).
- TIC Salut Social Foundation. Available online: https://ticsalutsocial.cat/en/ (accessed on 18 April 2025).
- Conseil National de l’Ordre des Médecins (CNOM). Available online: https://www.conseil-national.medecin.fr/lordre-medecins/conseil-national-lordre/lorganisation-conseil-national (accessed on 18 April 2025).
- Adekoya, O.O.; Daudu, C.D.; Okoli, C.E.; Isong, D.; Adefemi, A.; Tula, O.A. The role of environmental policies in shaping oil and gas operations: A comparative review of Africa and the USA. Int. J. Sci. Res. Arch. 2024, 11, 798–806. [Google Scholar] [CrossRef]
- Adekoya, O.O.; Isong, D.; Daudu, C.D.; Adefemi, A.; Okoli, C.E.; Tula, O.A. Reviewing the advancements in offshore drilling technologies in the USA and their global impact. World J. Adv. Res. Rev. 2024, 21, 2242–2249. [Google Scholar] [CrossRef]
- Babalola, O.; Nwatu, C.E.; Folorunso, A.; Adewa, A. A governance framework model for cloud computing: Role of AI, security, compliance, and management. World J. Adv. Res. Rev. 2024, 24, 1969–1982. [Google Scholar]
- Onyekwelu, P.N.; Patrick, O.A.; Nwabuike, C. Emotional resilience and employee performance of commercial banks in South-East Nigeria. Ann. Hum. Resour. Manag. Res. 2022, 2, 105–115. [Google Scholar]
- Ajiga, D.; Okeleke, P.A.; Folorunsho, S.O.; Ezeigweneme, C. Navigating ethical considerations in software development and deployment in technological giants. Int. J. Eng. Res. Updates 2024, 7, 50–63. [Google Scholar] [CrossRef]
- Bello, O.A.; Folorunso, A.; Ejiofor, O.E.; Budale, F.Z.; Adebayo, K.; Babatunde, O.A. Machine learning approaches for enhancing fraud prevention in financial transactions. Int. J. Manag. Technol. 2023, 10, 85–108. [Google Scholar]
- Oso, O.B.; Alli, O.I.; Babarinde, A.O.; Ibeh, A.I. Advanced financial modeling in healthcare investments: A framework for optimizing sustainability and impact. Gulf J. Adv. Bus. Res. 2025, 3, 561–589. [Google Scholar]
- Ayanponle, L.O.; Awonuga, K.F.; Asuzu, O.F.; Daraojimba, R.E.; Elufioye, O.A.; Daraojimba, O.D. A review of innovative HR strategies in enhancing workforce efficiency in the US. Int. J. Sci. Res. Arch. 2024, 11, 817–827. [Google Scholar] [CrossRef]
- Ayanponle, L.O.; Elufioye, O.A.; Asuzu, O.F.; Ndubuisi, N.L.; Awonuga, K.F.; Daraojimba, R.E. The future of work and Human Resources: A review of emerging trends and HR’s evolving role. Int. J. Sci. Res. Arch. 2024, 11, 113–124. [Google Scholar] [CrossRef]
- Soremekun, Y.M.; Udeh, C.A.; Oyegbade, I.K.; Igwe, A.N.; Ofodile, O.C. Conceptual framework for assessing the impact of financial access on SME growth and economic equity in the U.S. Int. J. Multidiscip. Res. Growth Eval. 2024, 5, 1049–1055. [Google Scholar] [CrossRef]
- Van Leeuwen, L.V.; Mesman, R.; Berden, H.J.; Jeurissen, P.P. Reimbursement of care does not equal the distribution of hospital resources: An explorative case study on a missing link among Dutch hospitals. BMC Health Serv. Res. 2023, 23, 1007. [Google Scholar] [CrossRef]
- Arinze, C.A.; Izionworu, V.O.; Isong, D.; Daudu, C.D.; Adefemi, A. Integrating artificial intelligence into engineering processes for improved efficiency and safety in oil and gas operations. Open Access Res. J. Eng. Technol. 2024, 6, 39–51. [Google Scholar] [CrossRef]
- Ibeto, M.; Onyekwelu, N. Teachers’ perception on family life education in public secondary schools in Anambra State. Int. J. Trend Sci. Res. Dev. 2020, 4, 823–829. [Google Scholar]
- Okeke, M.; Onyekwelu, N.; Akpua, J.; Dunkwu, C. Performance management and employee productivity in selected large organizations in south-East, Nigeria. J. Bus. Manag. 2019, 5, 57–70. [Google Scholar]
- Okeke, N.I.; Alabi, O.A.; Igwe, A.N.; Ofodile, O.C.; Ewim, C.P.-M. AI-powered customer experience optimization: Enhancing financial inclusion in underserved communities. Int. J. Appl. Res. Soc. Sci. 2024, 6, 2487–2511. [Google Scholar] [CrossRef]
- Gray, T.C.-H. A Participatory Design Approach in the Engineering of Ubiquitous Computing Systems. Ph.D. Thesis, The University of Queensland, St Lucia, Australia, 2009. [Google Scholar]
- Oliveira, T.C.; Barlow, J.; Gonçalves, L.; Bayer, S. Teleconsultations reduce greenhouse gas emissions. J. Health Serv. Res. Policy 2013, 18, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Chetty, M.; Blake, E.; Tucker, W. Developing Logically Relevant Applications for Rural South Africa: A Telemedicine Example; University of Cape Town: Cape Town, South Africa, 2005. [Google Scholar]
- Carcary, M. The Evaluation of ICT Investment Performance in Terms of Its Functional Deployment: A Study of Organizational Ability to Leverage Advantage from the Banner MIS in Institutes of Technology in Ireland; Limerick Institute of Technology: Limerick, Ireland, 2008. [Google Scholar]
- Elisa, S.A.; Brogonzoli, L.; De Benedictis, M.; Tomassi, M.F.; Paoli, G.; Giacomini, M. The Case for Telemedicine from a Sustainability Perspective. Appl. Med. Inform. 2024, 46, 49–52. [Google Scholar]
- Turnbull, S.; Cabral, C. Inequalities in the ability for people with type 2 diabetes and prediabetes to adapt to the reduction in in-person health support and increased use of digital support during the COVID-19 pandemic and beyond: Qualitative study. JMIR Diabetes 2024, 9, e55201. [Google Scholar] [CrossRef] [PubMed]
- Greenhalgh, T.; Ladds, E.; Hughes, G.; Moore, L.; Wherton, J.; E Shaw, S.; Papoutsi, C.; Wieringa, S.; Rosen, R.; Rushforth, A.; et al. Why do mGPs rarely do video consultations? Qualitative study in UK general practice. Br. J. GenmPract. 2022, 72, e351–e360. [Google Scholar] [CrossRef]
- Snoswell, C.L.; Caffery, L.J.; Haydon, H.M.; Thomas, E.E.; Smith, A.C. Telehealth uptake in general practice as a result of the coronavirus (COVID-19) pandemic. Aust. Health Rev. 2020, 44, 737–740. [Google Scholar] [CrossRef]
- Davidescu, A.A.; Manta, E.M.; Birlan, I. Economic Policies for Sustainable Healthcare: A Comparative Analysis of Telemedicine in Europe. In Sustainability Development Through Green Economics; Emerald Publishing Limited: Bingley, UK, 2024; pp. 191–217. [Google Scholar]
- Dvoryadkina, E.; Fechina, A. Defining “telemedicine services” in the context of large-scale digitalization. In Proceedings of the E3S Web of Conferences, Novosibirsk, Russia, 30 June–2 July 2021; Volume 296, p. 08021. [Google Scholar] [CrossRef]
- Vo, J. UN Sustainable Development Goal 3: Achieving Universal Health Coverage Through Digital Transformation. Public Health Insight. Available online: https://thepublichealthinsight.com/un-sustainable-development-goal-3-achieving-universal-health-coverage-through-digital-transformation/ (accessed on 11 December 2023).
- World Health Organization (WHO). Global Strategy on Digital Health 2020–2025. 2021. Available online: https://www.who.int/docs/default-source/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf (accessed on 11 December 2023).

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rizos, F.; Karanikas, H.; Katsapi, A.; Tsana, M.; Tsoukas, V.; Koukoulas, G.; Drakopoulos, D.; Katsiroumpa, A.; Galanis, P. The Role of Sustainability in Telemedicine Services: The Case of the Greek National Telemedicine Network. Healthcare 2025, 13, 1046. https://doi.org/10.3390/healthcare13091046
Rizos F, Karanikas H, Katsapi A, Tsana M, Tsoukas V, Koukoulas G, Drakopoulos D, Katsiroumpa A, Galanis P. The Role of Sustainability in Telemedicine Services: The Case of the Greek National Telemedicine Network. Healthcare. 2025; 13(9):1046. https://doi.org/10.3390/healthcare13091046
Chicago/Turabian StyleRizos, Fotios, Haralampos Karanikas, Angeliki Katsapi, Mariana Tsana, Vasileios Tsoukas, George Koukoulas, Dimitrios Drakopoulos, Aglaia Katsiroumpa, and Petros Galanis. 2025. "The Role of Sustainability in Telemedicine Services: The Case of the Greek National Telemedicine Network" Healthcare 13, no. 9: 1046. https://doi.org/10.3390/healthcare13091046
APA StyleRizos, F., Karanikas, H., Katsapi, A., Tsana, M., Tsoukas, V., Koukoulas, G., Drakopoulos, D., Katsiroumpa, A., & Galanis, P. (2025). The Role of Sustainability in Telemedicine Services: The Case of the Greek National Telemedicine Network. Healthcare, 13(9), 1046. https://doi.org/10.3390/healthcare13091046








