1. Introduction
Hearing loss (HL) has emerged as a significant global public health challenge, affecting approximately 6.1% of the world’s population [
1,
2]. Its prevalence increases with age, making it one of the most common chronic health conditions among adults [
2]. Depending on severity, HL can profoundly impair quality of life by limiting communication, causing social isolation, hindering workplace performance, and contributing to psychosocial and economic burdens [
3,
4,
5].
Epidemiological studies highlight HL as an emerging problem among younger populations as well [
6,
7]. Although the etiology of HL varies with age, ranging from genetic and infectious causes in children to presbycusis and noise exposure in adults, noise-induced hearing loss (NIHL) has attracted growing attention as one of the most preventable forms of HL [
8,
9].
NIHL results from prolonged exposure to loud sounds, which irreversibly damage cochlear sensory hair cells [
10]. Safe listening guidelines suggest that sound levels above 60 dB for more than one hour can cause temporary threshold shifts, while sustained exposure to 85 dB or higher for at least 8 h daily can lead to permanent auditory damage [
11]. Traditionally, occupational noise exposure was considered the dominant risk factor; however, in recent decades, recreational noise exposure has become increasingly prevalent [
12,
13]. It is estimated that over 600 million individuals globally, representing more than 12% of the population, remain at risk of developing NIHL due to unsafe noise levels [
12,
14].
The rapid adoption of smartphones and portable listening devices (PLDs), including headphones and earphones, has amplified concerns regarding recreational noise exposure [
15]. These devices enable prolonged listening at unsafe volumes, often without the user’s awareness of the associated risks. Alarmingly, improper use of headsets is linked to tinnitus, dizziness, difficulty in speech comprehension, and irreversible hearing impairment [
16]. Despite these risks, public awareness about the safe use of PLD remains limited in many regions [
17,
18,
19,
20].
In Saudi Arabia, multiple studies across different regions (Southern, Makkah, Jazan, and Eastern Provinces) have identified high basic awareness of NIHL, but also revealed critical gaps in knowledge regarding harmful sound levels, exposure duration, symptoms, and safe listening habits [
19,
21,
22,
23]. Nationally, approximately 49–59% of surveyed groups demonstrate awareness of NIHL, but knowledge of safe listening limits and consistent protective behavior remains unsatisfactory [
24].
International research aligns with these findings, showing that, despite basic awareness, detailed knowledge, and preventive practices, these are lacking in many populations, especially where public health campaigns are limited and PLD use is culturally normalized as part of modern communication and social enjoyment [
15]. These international patterns underscore the importance of bridging knowledge gaps that are specific to each region’s population, age groups, and cultural practices [
25].
Behavioral science frameworks offer critical insight into why individuals adopt or neglect preventive measures [
26]. The Health Belief Model (HBM) systematically examines how perceived susceptibility, severity, benefits, and barriers influence health behaviors [
27], while the COM-B model (Capability, Opportunity, Motivation–Behavior) clarifies the interaction between knowledge, environmental factors, and personal motivation in determining behavioral outcomes [
28,
29]. Integrating these models provides a structured framework for assessing the psychological and contextual factors that underlie the safe or risky use of personal listening devices. In the present study, the HBM and COM-B frameworks were employed not only to guide data analysis but to improve translation of findings into actionable public health strategies.
Taken together, there is a clear need for targeted public health interventions and structured educational campaigns, both globally and in Saudi Arabia, to assess and raise awareness, identify risk factors, and motivate behavioral changes to reduce the burden of NIHL from headphone use. However, deeply contextualized data from the Northern Border Region remain limited, justifying the relevance and novelty of this study in fulfilling these objectives in this population.
2. Materials and Methods
2.1. Study Design
A cross-sectional analytical study was conducted to assess adults’ awareness of noise-induced hearing loss from headphone use in the Northern Border Region of Saudi Arabia.
2.2. Study Population and Sampling
Eligible participants were male and female adults aged 18 to 60 years residing in the Northern Border Region, irrespective of nationality. Individuals older than 60 years were excluded to minimize confounding from age-related hearing loss. Participants were recruited between 10 September 2024 and 15 November 2024 using a convenience sampling approach. The survey link was widely disseminated across multiple social media platforms (e.g., WhatsApp groups, Twitter, Facebook) and local community groups to maximize geographic and demographic reach within the Northern Border Region. The invitation included a brief study explanation and eligibility criteria (age 18–60, residence in the region, willingness to participate). To help ensure data integrity, each respondent could submit only one entry per device, and duplicate or incomplete responses were identified and excluded during data cleaning. No financial or material incentives were provided. All participation was voluntary and anonymous, with informed consent obtained electronically before survey access.
Sample size was calculated using the Raosoft sample size calculator (Raosoft Inc., Seattle, WA, USA). Assuming a 5% margin of error, 95% confidence interval, and population response distribution of 50%, a minimum of 384 respondents was required.
2.3. Ethical Statement
Ethical approval for this study was obtained from the Local Bioethics Committee (HAP-09-A-043) at Northern Border University (approval no. 101/24/H) dated 6 September 2024, and the work was conducted in accordance with the principles outlined in the Declaration of Helsinki.
2.4. Data Collection Tool
Data were collected using a previously validated structured questionnaire adapted from relevant literature and expert consensus [
30]. The survey was administered electronically via a Google Form. It consisted of 37 items (
Supplementary File) divided into six major domains:
Demographic and health status characteristics data (10 items): sex, age range, nationality, residence, education level, marital status, occupation, smoking status, chronic health conditions, and family history of hearing problems.
Risk factors related to NIHL (6 items): exposure to occupational noise, preferred type of audio device, frequency and duration of listening sessions, typical volume settings, and perceived impact on surroundings.
Signs and symptoms (5 items): tinnitus occurrence, increased speech volume, repeated requests for clarification, frequent increases of TV/radio volume, and time required for acclimatization to loud environments.
Knowledge and beliefs (10 items): perceptions of how noise and environment affect hearing, recognition of early warning signs, beliefs about NIHL preventability, and awareness of sound level and exposure duration risks.
Practices and attitudes (6 items): information sources about NIHL, personal listening practices, support for device-based volume limitations, readiness for behavioral change, endorsement of warning indicators, and willingness to use sound level control programs.
Prevention awareness: views and behaviors regarding preventive measures and family protection.
2.5. Pilot Study and Validation
Before distributing the primary survey, a pilot study was conducted with a subset of the sample (n = 40) to assess reliability and clarity. The internal consistency of the questionnaire domains was assessed using Cronbach’s alpha (α = 0.89 for the total scale), and necessary revisions were made to improve comprehensibility and data integrity.
2.6. Operational Definitions
NIHL awareness was defined as participants’ knowledge, attitudes, and preventive behaviors related to hearing loss from prolonged or high-volume headphone use. Overall awareness levels were categorized as low (<60%), moderate (60–79%), or high (≥80%) based on mean percentage domain and total scores.
2.7. Data Management and Statistical Analysis
Survey responses were downloaded, coded, and entered into Microsoft Excel for initial cleaning. Statistical analysis was performed using standard statistical software (e.g., SPSS v26, IBM, Armonk, NY, USA). Descriptive statistics (frequencies, percentages, means, SDs) were used to characterize participant demographics and summarize categorical variables.
Comparative analyses used the Chi-square or Fisher’s exact tests, where appropriate, to identify associations between categorical variables.
The knowledge score was constructed by assigning one point for each correct response to nine selected objective items within the knowledge domain (questions 22–28, 30–31). Item 29 (“Do I currently have enough information concerning the danger posed by exposure to loud noise(s) on hearing ability?”) was excluded from the final score because it assessed self-perceived sufficiency of information rather than factual knowledge. Thus, the maximum possible knowledge score was 9, with an observed range of 1–9. For each included item, correct answers were defined accordingly [
21,
30]. Total scores were used for statistical analysis and descriptive reporting.
Independent-sample t-tests and a one-way ANOVA were used to compare mean knowledge scores across demographic groups, including sex, education level, and occupation. The score was treated as a continuous variable after assessing normality. Odds ratios (ORs) and corresponding 95% confidence intervals (CIs) were calculated to investigate independent risk factors of NIHL. A significance level of p < 0.05 was employed. Due to the exploratory nature of the study, no formal multiple-testing adjustments were implemented. The results were meticulously analyzed to minimize the likelihood of a Type I error.
2.8. Theoretical Frameworks and Analytical Strategy
This study prospectively adopted the HBM and COM-B framework to guide questionnaire development, data interpretation, and the design of recommendations. Quantitative results were mapped onto the constructs of each model, allowing for a multidimensional understanding of the determinants and barriers to preventive behavior. The analytic approach allowed identification of both individual cognitive factors and social or contextual influences relevant to NIHL prevention.
4. Discussion
This cross-sectional study examined awareness, attitudes, and risk factors related to NIHL from headphone use in the Northern Border Region of Saudi Arabia, employing the HBM and COM-B framework to interpret behavioral determinants. The findings reveal substantial knowledge gaps and risky listening habits despite widespread recognition of noise exposure as a threat to hearing health.
The prevalence of hearing loss symptoms in this sample is high: 74.7% of participants reported at least one symptom, and 42.4% experienced tinnitus. These findings align with global trends indicating a rise in NIHL among young and middle-aged adults, which is associated with the increasing use of PLDs [
15]. Age, smoking, chronic disease, family history, workplace noise, and both frequency and duration of PLD use were significantly associated with greater risk, consistent with previous studies highlighting these exposures as principal risk factors [
22,
25,
31].
Knowledge assessment revealed that while 78.4% of participants recognized the harmfulness of high volume levels, a much lower proportion correctly identified specific thresholds for hazardous exposure, and only 58% believed NIHL to be preventable. This suggests that general awareness does not consistently translate into accurate risk perception or protective behavior, a pattern observed globally, especially in settings where health education on NIHL is limited [
32]. The predominance of social media as an information source raises questions about the quality and reach of health literacy interventions and underlines the need for structured campaigns using reliable platforms [
15,
24,
33,
34].
Interpreting these outcomes through the HBM demonstrates inconsistent perceived susceptibility and moderate perceived severity. While symptoms were common and most participants recognized noise as a danger, many struggled to accurately assess their own behaviors or the reversibility of the harm they caused. The desire to reduce volume and the readiness to change reported by most respondents underscore strong motivation when clear benefits and cues to action are established. However, barriers such as insufficient knowledge, social normalization of high-volume listening, and environmental factors (e.g., workplace noise) hinder protective action.
The COM-B analysis further elucidates that behavioral change is constrained by limited psychological capability (knowledge deficits) and by environmental and social opportunity (prevalence of workplace noise, lack of device controls, and permissive social attitudes regarding loud PLD use). Reflective motivation for change appears robust, with most participants open to interventions if supported by tangible evidence and effective cues. In contrast, automatic motivation (habit and enjoyment) may counter efforts unless addressed in campaigns and policy.
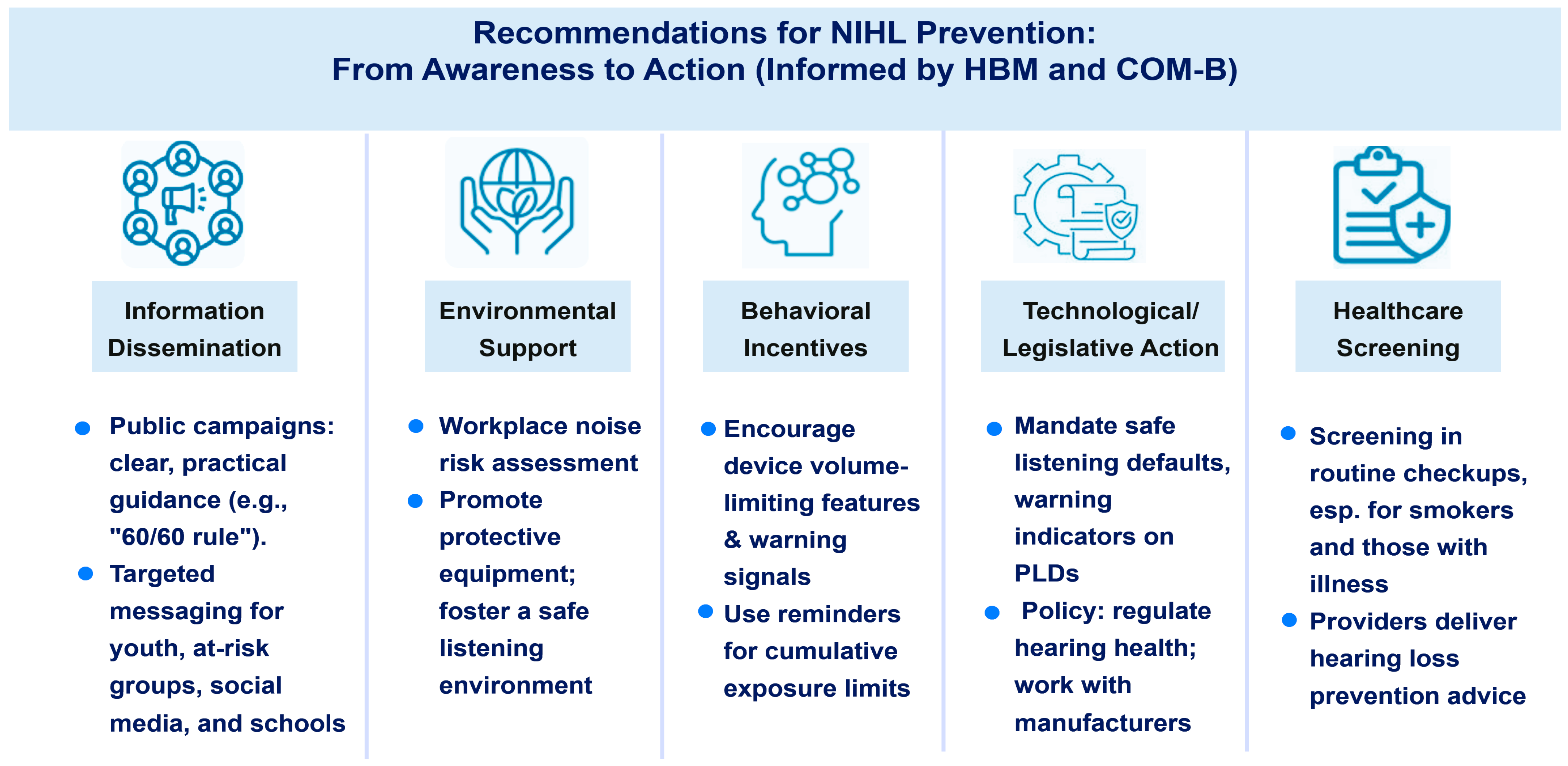
Collectively, these results highlight the urgent need for multifaceted public health strategies. Health promotion activities should incorporate behavior change theory, deliver evidence-based, tailored messaging via trusted channels, support environmental and policy changes (such as volume-limiting features on devices), and embed NIHL prevention within broader health literacy and chronic disease frameworks. Targeted interventions for high-risk groups (smokers, those with occupational exposure) and reinforcement of preventive attitudes among youth are especially warranted.
It is worth noting that Saudi Arabia is a vast and sociodemographically diverse country, with marked variations in geography, population density, occupational risk profiles, cultural practices, and health service accessibility across its regions. While several studies have explored NIHL and hearing health awareness in regions such as Riyadh, Makkah, Jazan, and the Eastern Province, often using similar instruments for comparability, this region-specific research is crucial for several reasons: First, the burden of hearing loss, exposure risks (e.g., industrialization, prevalence of consanguinity, rural isolation), and key determinants (education, socioeconomic status, cultural attitudes) can differ markedly between regions [
35]. For example, industrialized eastern regions report higher prevalence, in part due to occupational exposures. In contrast, southern and northern rural regions face unique challenges related to terrain, health literacy, and access to healthcare resources [
36,
37,
38]. Second, regionally tailored data enables local public health and policy interventions to be adjusted effectively, ensuring that needs and service gaps are addressed in alignment with Saudi Arabia’s Vision 2030 goals [
39,
40].
While national-level studies provide a broad epidemiological perspective, local or regional studies, using comparable tools, offer granular insights necessary for implementation science and targeted health promotion [
41]. Our study uniquely contributes data from the underrepresented Northern Border Region, supporting intra-national comparisons and province-level policy planning. The similarities in questionnaire structure across studies improve comparability. Still, our research adds specific value by documenting context-linked risk patterns, health literacy gaps, and opportunities for culturally and regionally adapted intervention in this part of Saudi Arabia [
35].
4.1. Study Strengths and Limitations
The integration of the HBM and COM-B frameworks is a key strength, enabling a comprehensive analysis of the cognitive, social, and contextual factors that contribute to NIHL risk. The study’s limitations include reliance on self-report, a cross-sectional design that precludes causal inference, and recruitment through online platforms, which may introduce potential selection bias.
Furthermore, recruiting participants via online platforms using a convenience sampling approach from a single region may introduce significant selection bias and limit the generalizability of these findings. Individuals without internet access, lower health engagement, or from underrepresented demographic groups are likely to be excluded, leading to a sample skewed toward those more familiar with technology, with higher education, or with greater health awareness. In addition, the single-region focus restricts the applicability of our results to other geographic or cultural contexts within Saudi Arabia, where occupational, educational, or healthcare access factors may vary considerably.
It is also important to note that this study assessed hearing loss solely through self-reported symptoms rather than objective audiometric testing. Evidence indicates that self-reported hearing status shows only moderate agreement with objectively measured hearing loss, and discrepancies may vary by age, gender, and cultural context [
42,
43]. Self-reports can miss milder degrees of impairment or be influenced by factors such as awareness, stigma, or comorbid symptoms [
44,
45]. Future studies should integrate both subjective and objective (audiometric) assessments to improve diagnostic validity and comparability with broader epidemiological data.
4.2. Implications and Future Directions
Future research should evaluate the impact of multifaceted educational interventions and policy measures on behavior and hearing health outcomes. Collaboration among healthcare providers, policymakers, and the media is essential for achieving adequate health literacy and preventing NIHL in vulnerable populations (
Figure 1).