1. Introduction
The Center for Disease Control (CDC) reported that 38% of all adults in the United States had prediabetes between 2017 and 2020 [
1]. Prediabetes, also called impaired glucose tolerance, impaired fasting glucose, or intermediate hyperglycemia, progresses to type 2 diabetes at an annualized rate of 5–10% [
2]. The Veteran population displays a higher diabetes prevalence compared to the general population with nearly 25% of Veterans in the health care system with a diabetes diagnosis. National VA data demonstrates that there may also be a higher prevalence of prediabetes in Veterans. There are over 1.7 million Veterans within VHA, nearly 119,000 in the VA Mid-Atlantic Health Care Network alone (VISN 6), who potentially have prediabetes, based on their HbA1c result [
3].
It is important to identify and characterize the current Veteran population with prediabetes, not only because of the existing high prevalence of type 2 diabetes, but because the Veteran population holds unique risk factors for developing prediabetes and type 2 diabetes. Obesity is a known risk factor for diabetes and prediabetes [
4]. According to Breland et al., obesity rates range from 28% to 49% among VHA facilities, in comparison to the nearly 42% of US adults who are obese [
5,
6]. Veterans also experience a higher prevalence of serious mental illness. Liu et al. found that 9.6% Veterans were diagnosed with depression, higher than the 6.7% reported by adults in the United States [
7]. Serious mental illness, such as major depressive disorder and schizophrenia, is associated with a greater risk of type 2 diabetes in Veterans compared to Veterans without serious mental illness [
8]. Not only can serious mental illness increase the risk of diabetes, but so can the medications often prescribed to treat these conditions. There is well-documented evidence of these medications, such as atypical antipsychotics, contributing to metabolic syndrome, including hyperglycemia, weight gain, and hypertension [
9].
Identifying Veterans with prediabetes is crucial to type 2 diabetes prevention and its complications. A relationship exists between prediabetes and the micro- and macrovascular complications often associated with diabetes [
10]. A meta-analysis from 2021 found that prediabetes is associated with a risk of all-cause mortality [
11]. A cross-sectional study from Ishikawa et al. reported an over 39% prevalence of prediabetes in people with heart failure [
12]. With these costly potential complications, investigating prediabetes diagnosis patterns in VISN 6 Veterans with cardiovascular risk factors is critical. Dyslipidemia, a condition associated with cardiovascular disease, is a known risk factor for type 2 diabetes (Von Eckardstein and Sibler 2011; Davis et al. 2018 [
13,
14]). A retrospective study including six VA medical facilities identified that over 36% of Veterans had dyslipidemia [
15]. Hypertension, another risk factor for type 2 diabetes and cardiovascular disease, affects nearly 45% of Veterans in the VHA [
15,
16]. Heart failure and prediabetes have a bidirectional relationship, which demonstrates the importance of assessing prediabetes status for the prevention and management of heart failure [
17,
18,
19]. With such a prevalence of these risk factors among Veterans, routine screening and documentation of prediabetes is indicated and necessary for the prevention of diabetes and cardiovascular disease.
Veterans are more likely reside in rural areas than the general population. Living in rural areas brings its own challenges for health care and disease management [
20,
21]. Rural populations tend to have a higher prevalence of diabetes and risk factors for diabetes, as well as a higher diabetes-related mortality [
22]. While there is limited data regarding prediabetes prevalence among Veterans in rural areas, based on diabetes prevalence it is likely greater than in urban areas, making this a key at-risk population for prediabetes.
The purpose of this retrospective analysis is to characterize the Veteran population within the VISN 6 network with and without a documented prediabetes diagnosis. We assess various known risk factors for prediabetes and diabetes to guide better population screening and education for prediabetes. This study provides insight into the prediabetes population across VISN 6, including diagnosis patterns, and provides directions for improvements in addressing prediabetes in Veterans.
2. Materials and Methods
2.1. Study Design and Patient Population
This analysis is a cross-sectional, observational, retrospective review of patient data available from North Carolina and Virginia VA Medical Centers (VAMCs) included in the Mid-Atlantic Health Care Network (VISN 6) to understand factors that may influence a formal diagnosis of prediabetes within the system.
Data was retrieved from the on-premises cloud server farm, the Corporate Data Warehouse (CDW; Austin, TX, USA), using T-SQL (SQL Server Management Studio 0.2.37.0, Redmond, WA, USA) for living Veterans aged 35–89 with at least one outpatient encounter at a VISN 6 VA Medical Center (VAMC) within the previous 24 months (24 June 2023 through 23 June 2025). VISN 6, also known as the Mid-Atlantic Health Care Network, encompasses VAMCs in North Carolina and Virginia. Duplicate encounters were excluded from the initial query. Patients were included in the analysis if they had a qualifying lab for prediabetes from 24 June 2023 to 23 June 2025. Prediabetes was defined as an HbA1c result equal to or greater than 5.7% and less than 6.5% in the 24-month analysis window from both inpatient and outpatient labs. Because it is VHA policy that patients do not fast for blood work, this analysis did not include fasting plasma glucose in inclusion criteria. Patients were excluded if they were previously diagnosed with diabetes with ICD-10 codes E10.xx, E11.xx, or E13.xx.
2.2. Outcome Variable
The outcome variable was defined as the presence of a diagnosis of prediabetes through at least one documented instance of ICD-10 code R73.xx, which encompasses impaired fasting glucose, impaired glucose tolerance, and prediabetes.
2.3. Exposure Variables
Patient race, age, and sex were included in the analysis to observe differences in sociodemographic characteristics between patients with and without a documented diagnosis of prediabetes. Within each group, we used ICD-10 codes to identify patients with medical conditions associated with prediabetes and diabetes risk, including hypertension (I10), dyslipidemia (E78), and heart failure (I50). Because Veterans have a higher prevalence of serious mental health conditions associated with diabetes risk, we included ICD-10 codes for depression and major depression (F32, F33), anxiety disorders including PTSD (F41, F43), and schizophrenia (F20). Common medication classes with a known risk for diabetes or risk factors were included in the analysis. Prescriptions were flagged as yes/no if a patient had an active or suspended prescription for the following medication classes: antipsychotics (CN701, CN709), prednisone (HS051) with a written quantity of 90 or greater, immunosuppressants (IM599, IM600), GLP1 agonists (HS509), weight loss medications (GA751, GA900), and metformin (HS502).
To assess rurality, addresses were coded as Urban, Rural, Highly Rural, and Insular (U, R, H, I) based on VHA designation determined by the census tract in which the Veteran resided. To understand differences in the size and capabilities of different VAMCs on diagnosis patterns of prediabetes, we included VA facility complexity in the analysis. Complexity level reflects the volume, patient risk level, clinical programs, and size of clinical and teaching programs of the VA facility. All VISN 6 Medical Centers are designated as complexity 1, further designated as 1a, 1b, or 1c, with ‘1a’ being the most complex.
2.4. Statistical Analysis
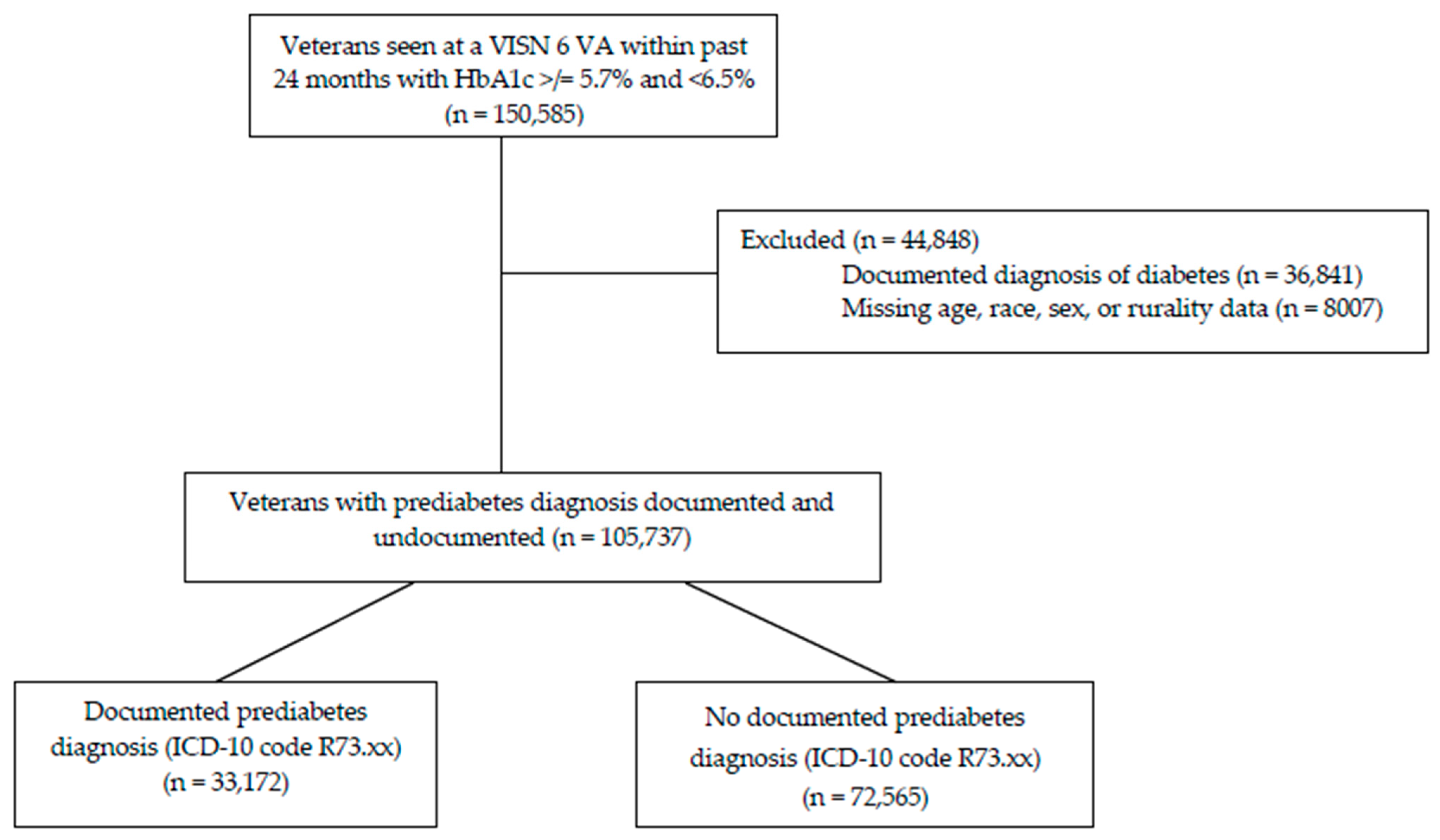
Data cleaning and analysis was performed in SAS 9.4 (SAS Institute, Cary, NC, USA). Patients with a diagnosis of diabetes or missing information on age, sex, or race were removed from the analysis by listwise deletion (
Figure 1). After removal of those with an ICD-10 code for diabetes in the last two years (n = 36,841) or with missing demographic data (n = 8007), remaining patients with a qualifying HbA1c for prediabetes (n = 105,737) were categorized by presence of a documented diagnosis of prediabetes (R73.xx). Descriptive statistics were reported for demographics (
Table 1), active medication prescriptions identified for analysis (
Table 2), and the conditions associated with diabetes risk and prediabetes (
Table 3). Bivariate analysis was performed on patients with a documented prediabetes diagnosis code versus patients without a documented code. Bivariate analysis was performed by using the Kruskal–Wallis test for continuous variables (age) and the Chi-Square test of independence for categorical variables (gender, race, prescriptions, and risk factor ICD-10 codes). Statistical significance was set at α = 0.05, and no corrections for multiple comparisons were applied.
Table 4 shows prediabetes documentation by facility complexity (1a, 1b, or 1c).
2.5. Ethical Considerations
This study was reviewed by the WNCVAHCS Institutional Review Board and deemed not to be research.
3. Results
3.1. Diagnosis and Demographics
Baseline demographics are displayed in
Table 1. The average age (median 62 years) for those with a prediabetes diagnosis and those without a diagnosis was similar. Both groups were predominantly male (84%), mirroring VHA enrollees nationally. Within VISN 6, female patients were shown to have a higher proportion of documented prediabetes than undocumented prediabetes (18.7% versus 15.2%), unlike male patients. Black patients had a higher proportion of documented prediabetes versus non-documented prediabetes (45.5% vs. 38.4%), while white patients had a lower proportion of coded diagnosis (47.7% vs. 54.3%) within the study sample.
3.2. Medications
Table 2 summarizes the findings among the cohorts prescribed specific medication classes. While only a small percentage of Veterans were prescribed an antipsychotic, there is an established association between hyperglycemia and antipsychotic medications. Despite this knowledge, over 71% of Veterans with prediabetes prescribed an antipsychotic displayed no documented prediabetes diagnosis. This was similar among Veterans prescribed immunosuppressants and chronic prednisone.
Obesity is a well-recognized risk factor for prediabetes, yet only 32.4% of Veterans prescribed a weight loss medication had a documented prediabetes diagnosis. Metformin demonstrated potential benefit in prediabetes through the Diabetes Prevention Program study yet just 54% of Veterans prescribed metformin had a documented diagnosis.
3.3. Concurrent Medical Conditions
Table 3 captures the incidence of concurrent medical conditions in each prediabetes group. Cardiovascular conditions associated with hyperglycemia were evaluated. Veterans with a lipid disorder or hypertension were less likely to have a documented prediabetes diagnosis. The lack of documentation was even higher, at over 30%, for those with heart failure.
Mental illness comorbidities, including schizophrenia, depressive and major depressive disorders, anxiety disorders, and stress and adjustment disorders, were included in our evaluation. Schizophrenia represented a very small percentage of the population (<1%), but the majority with prediabetes did not have a documented diagnosis. The lack of documented diagnosis was similar, around 67%, in Veterans with depressive, anxiety, and stress and adjustment disorder diagnoses.
3.4. Comparison of VISN Facilities
The percentage of Veterans with a documented diagnosis was similar across the seven facilities. Documentation ranged from 27.9% to 36.3% between facilities, with an average of 31.4%. When facility complexity was considered, the percentage of Veterans without a diagnosis was similar, apart from level 1b facilities. This complexity level, which also had the smallest prediabetes population, demonstrated a lower documentation rate (
Table 4). When assessing rurality, interestingly, urban and highly rural Veterans had similar rates of diagnosis, while rural Veterans experienced a lower rate of documented diagnosis (
Table 5).
4. Discussion
Almost 69% of Veterans meeting the criteria did not have a documented diagnosis of prediabetes. A study in 2022 found a similar gap in prediabetes diagnosis within the active military population. They found that less than half of those meeting the criteria for prediabetes actually had a documented diagnosis [
23].
Much of the analyzed population were white males. This is reflective of the general VHA population and may not be applicable to the general population. Though the population numbers of Black Veterans and female Veterans were small, they were more likely to have a documented prediabetes diagnosis, and this should be further explored.
We analyzed certain concurrent health conditions associated with prediabetes and type 2 diabetes. We found that Veterans with cardiovascular conditions including dyslipidemia, hypertension, and heart failure were less likely to have a documented diagnosis. These are known risk factors for type 2 diabetes, and therefore we would anticipate a higher rate of prediabetes recognition through documentation. There were similar rates of diagnosis documentation among Veterans with depressive, anxiety, and stress and adjustment disorder diagnoses, but this rate was low. These conditions can increase the risk of diabetes due to their association with obesity and medications that may lead to hyperglycemia.
The assessment of medications that may impact glucose found a higher rate of diagnosis documentation in those prescribed metformin or a GLP1 agonist. This was expected based on evidence that these medication classes positively impact glucose and weight. Despite the known hyperglycemia risk, over 71% of Veterans with prediabetes prescribed an antipsychotic displayed no documented diagnosis. There was a small volume of prescriptions for immunosuppressants and chronic prednisone, but the lack of a documented diagnosis was similar to those prescribed antipsychotics.
Documentation rates among VISN 6 facilities based on facility complexity indicated that a lack of documentation occurred at a range of VAs. More detailed assessment may reveal potential contributors to the lower documentation rate among 1b facilities. Regarding rurality, the lack of an ordered trend from highly rural, to rural, to urban needs further investigation, including a multivariate analysis to account for variables such as those gathered in this study.
Limitations exist with this retrospective analysis. It is possible that a Veteran may be informed of a prediabetes diagnosis, but documentation was not completed by the provider. Documentation of ICD-10 codes may differ based on the provider or facility, or may be documented externally for Veterans seeking care outside of the VA system. These findings are limited to the facilities within this geographic area and may not reflect the VA as a whole or non-VA facilities. Because the focus of this evaluation was an exploratory evaluation of the VISN 6 geographic region, this study is primarily descriptive. Because this study observes clinical characteristics, demographic data, and a diagnosis of prediabetes over at any time over a two-year cross-sectional period, multivariate regression cannot be used for causal analysis, as comorbid diagnoses and related prescriptions are not specified to occur prior to a diagnosis of prediabetes. Moreover, prescriptions for prediabetes treatment, such as metformin, are often associated with a formal diagnosis, indicating that perhaps documentation of the diagnosis is overlooked. Providers may have varying experience and understanding about prediabetes, contributing to the low frequency of diagnosis documentation. Additionally, we acknowledge HbA1c testing limitations in terms of the screening and diagnosis of prediabetes. Various medical conditions impacting hemoglobin concentrations or red blood cell turnover could potentially lead to unreliable HbA1c measurements. Some evidence indicates that certain racial groups may experience higher baseline HbA1c levels, which could lead to the misdiagnosis of some patient populations. VHA clinical guidance for prediabetes diagnosis criteria includes HbA1c ≥ 5.7–6.4% and fasting plasma glucose (FPG) ≥ 100 mg/dL (5.5 mmol/L) [
24]. We did not include FPG in our review, as no retrospective method was available to confirm a Veteran’s fasting state when the blood was collected. VHA policy states that labs do not require fasting unless specifically stated or requested by the ordering provider [
25].
While this was an exploratory analysis, future research could include multivariate analysis to assess the impact of these diabetes risk factors that are more common among the Veteran population. Our findings may also guide qualitative research assessing provider education and understanding of prediabetes, including the clinical impact of the condition and evidenced-based interventions that can prevent progression to type 2 diabetes.
5. Conclusions
The risks associated with prediabetes are well documented, including not only potential progression to type 2 diabetes but also complications such as cardiovascular disease. Despite the known risks, there is an apparent gap in diagnosis documentation. This missing documentation could reflect a lack of recognition by a provider. If a provider does not recognize a prediabetes diagnosis, then an opportunity to educate the Veteran about type 2 diabetes risk may also be missed.
This data provides the opportunity to bring the attention of health care providers towards prediabetes diagnosis and its documentation for at-risk Veterans. Completing diagnosis documentation is a positive step toward confirming that Veterans are aware of the condition. Recognizing the condition can help health care providers to inform Veterans of opportunities for education and lifestyle intervention to reduce the risk of progression to type 2 diabetes.
Author Contributions
Conceptualization, B.D.G. and P.R.G.; methodology, B.D.G., P.R.G., R.S.C., and A.T.P.-J.; formal analysis, A.T.P.-J.; resources, B.D.G., R.S.C., and A.T.P.-J.; data curation, R.S.C.; writing—original draft preparation, B.D.G.; writing—review and editing, B.D.G. and P.R.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was reviewed by the WNCVAHCS Institutional Review Board and deemed not to be research.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data sets presented in this article are not readily available because they are restricted to the Veterans Health Administration.
Conflicts of Interest
Authors of this information and publication have no conflicts of interest to disclose. This material is the result of work supported with resources of the Western North Carolina VA Health Care system. It does not represent the official stance or viewpoint of the U.S. Department of Veteran Affairs or any affiliates.
Abbreviations
The following abbreviations are used in this manuscript:
| VHA | Veterans Health Administration |
| VISN | Veterans Integrated Service Network |
| HbA1c | Hemoglobin A1c |
References
- Prediabetes|CDC. 23 February 2023. Available online: https://www.cdc.gov/diabetes/php/data-research/index.html (accessed on 9 May 2025).
- Gerstein, H.C.; Santaguida, P.; Raina, P.; Morrison, K.M.; Balion, C.; Hunt, D.; Yazdi, H.; Booker, L. Annual Incidence and Relative Risk of Diabetes in People with Various Categories of Dysglycemia: A Systematic Overview and Meta-Analysis of Prospective Studies. Diabetes Res. Clin. Pract. 2007, 78, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Power BI VSSC Diabetes. Available online: https://app.powerbigov.us/groups/me/apps/0a274e14-d0ba-47c9-b2cf-3603afc5a6f6/reports/2a03f818-aaa2-44fa-82ff-1049ebecebca/ReportSection (accessed on 9 May 2025).
- American Diabetes Association Professional Practice Committee; ElSayed, N.A.; McCoy, R.G.; Aleppo, G.; Balapattabi, K.; Beverly, E.A.; Early, K.B.; Bruemmer, D.; Ebekozien, O.; Echouffo-Tcheugui, J.B.; et al. 2. Diagnosis and Classification of Diabetes: Standards of Care in Diabetes—2025. Diabetes Care 2025, 48 (Suppl. 1), S27–S49. [Google Scholar] [CrossRef]
- Adult Obesity Facts. Available online: https://www.cdc.gov/obesity/adult-obesity-facts/?CDC_AAref_Val=https://www.cdc.gov/obesity/data/adult.html (accessed on 24 July 2025).
- Breland, J.Y.; Phibbs, C.S.; Hoggatt, K.J.; Washington, D.L.; Lee, J.; Haskell, S.; Uchendu, U.S.; Saechao, F.S.; Zephyrin, L.C.; Frayne, S.M. The Obesity Epidemic in the Veterans Health Administration: Prevalence Among Key Populations of Women and Men Veterans. J. Gen. Intern. Med. 2017, 32 (Suppl. 1), 11–17. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Collins, C.; Wang, K.; Xie, X.; Bie, R. The Prevalence and Trend of Depression among Veterans in the United States. J. Affect. Disord. 2019, 245, 724–727. [Google Scholar] [CrossRef] [PubMed]
- Pless, L.L.; Mitchell-Miland, C.; Seo, Y.-J.; Bennett, C.B.; Freyberg, Z.; Haas, G.L. Psychiatric Factors Predict Type 2 Diabetes Mellitus in US Veterans. Schizophrenia 2025, 11, 63. [Google Scholar] [CrossRef] [PubMed]
- Carli, M.; Kolachalam, S.; Longoni, B.; Pintaudi, A.; Baldini, M.; Aringhieri, S.; Fasciani, I.; Annibale, P.; Maggio, R.; Scarselli, M. Atypical Antipsychotics and Metabolic Syndrome: From Molecular Mechanisms to Clinical Differences. Pharmaceuticals 2021, 14, 238. [Google Scholar] [CrossRef] [PubMed]
- Knowler, W.C.; Barrett-Connor, E.; Fowler, S.E.; Hamman, R.F.; Lachin, J.M.; Walker, E.A.; Nathan, D.M.; Diabetes Prevention Program Research Group. Reduction in the Incidence of Type 2 Diabetes with Lifestyle Intervention or Metformin. N. Engl. J. Med. 2002, 346, 393–403. [Google Scholar] [CrossRef] [PubMed]
- Schlesinger, S.; Neuenschwander, M.; Barbaresko, J.; Lang, A.; Maalmi, H.; Rathmann, W.; Roden, M.; Herder, C. Prediabetes and Risk of Mortality, Diabetes-Related Complications and Comorbidities: Umbrella Review of Meta-Analyses of Prospective Studies. Diabetologia 2022, 65, 275–285. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, Y.; Lewis, R.D.; Laing, E.M.; Anderson, A.K.; Zhang, D.; Quyyumi, A.A.; Dunbar, S.B.; Trivedi-Kapoor, R.; Sattler, E.L.P. Prevalence and Trends of Type 2 Diabetes Mellitus and Prediabetes among Community-Dwelling Heart Failure Patients in the United States. Diabetes Res. Clin. Pract. 2022, 184, 109191. [Google Scholar] [CrossRef] [PubMed]
- von Eckardstein, A.; Sibler, R.A. Possible contributions of lipoproteins and cholesterol to the pathogenesis of diabetes mellitus type 2. Curr. Opin. Lipidol. 2011, 22, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Davis, P.J.; Liu, M.; Sherman, S.; Natarajan, S.; Alemi, F.; Jensen, A.; Avramovic, S.; Schwartz, M.D.; Richard, B. HayesHbA1c, lipid profiles and risk of incident type 2 Diabetes in United States Veterans. PLoS ONE 2018, 13, e0203484. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M.L.; Pietz, K.; Battleman, D.S.; Beyth, R.J. Prevalence of Comorbid Hypertension and Dyslipidemia and Associated Cardiovascular Disease. Am. J. Manag. Care 2004, 10, 926–932. [Google Scholar] [PubMed]
- Carrico, M.; Frosch, C.; Craig, K.; Carter, M.; Falk, J.; Guerrero, S.; Huang, L.; Kossoudji, A.; Michelson, T.R.; Miller, P.; et al. Implementation of Video Blood Pressure Visits in the Veterans Health Administration. Telemed. E-Health 2024, 30, 1006–1012. [Google Scholar] [CrossRef] [PubMed]
- Gerstein, H.C.; Swedberg, K.; Carlsson, J.; McMurray, J.J.V.; Michelson, E.L.; Olofsson, B.; Pfeffer, M.A.; Yusuf, S. The Hemoglobin A1c Level as a Progressive Risk Factor for Cardiovascular Death, Hospitalization for Heart Failure, or Death in Patients With Chronic Heart Failure: An Analysis of the Candesartan in Heart Failure: Assessment of Reduction in Mortality and Morbidity (CHARM) Program. Arch. Intern. Med. 2008, 68, 1699. [Google Scholar] [CrossRef]
- Kristensen, S.L.; Jhund, P.S.; Lee, M.M.Y.; Køber, L.; Solomon, S.D.; Granger, C.B.; Yusuf, S.; Pfeffer, M.A.; Swedberg, K.; McMurray, J.J.V.; et al. Prevalence of Prediabetes and Undiagnosed Diabetes in Patients with HFpEF and HFrEF and Associated Clinical Outcomes. Cardiovasc. Drugs Ther. 2017, 31, 545–549. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.-D.; Liang, D.-L.; Xie, Y. Prediabetes and Risk of Heart Failure: The Link Grows Stronger. Cardiovasc. Diabetol. 2021, 20, 112. [Google Scholar] [CrossRef] [PubMed]
- Cusack, M.; Montgomery, A.E.; Harris, T.; Roncarati, J.; Brecht, T.; Antonellis, C.; Byrne, T.; Tsai, J.; True, G. Providers’ Reflections on Infrastructure and Improvements to Promote Access to Care for Veterans Experiencing Housing Instability in Rural Areas of the United States: A Qualitative Study. Health Soc. Care Community 2022, 30, e6356–e6365. [Google Scholar] [CrossRef] [PubMed]
- Ohl, M.E.; Carrell, M.; Thurman, A.; Weg, M.V.; Hudson, T.; Mengeling, M.; Vaughan-Sarrazin, M. “Availability of Healthcare Providers for Rural Veterans Eligible for Purchased Care under the Veterans Choice Act”. BMC Health Serv. Res. 2018, 18, 315. [Google Scholar] [CrossRef] [PubMed]
- Dugani, S.B.; Mielke, M.M.; Vella, A. Burden and Management of Type 2 Diabetes in Rural United States. Diabetes/Metab. Res. Rev. 2021, 37, e3410. [Google Scholar] [CrossRef] [PubMed]
- Clutter, C.A.; Beckman, D.J.; Wardian, J.L.; Rittel, A.G.; True, M.W. Are We Missing an Opportunity? Prediabetes in the U.S. Military. Mil. Med. 2024, 189, 326–331. [Google Scholar] [CrossRef] [PubMed]
- VA.Gov|Veterans Affairs. General Information. Available online: https://www.healthquality.va.gov/guidelines/CD/diabetes/index.asp (accessed on 9 November 2023).
- Quinlan, J. Overnight Fasting No Longer Required for Most VA Blood Testing. Available online: https://news.va.gov/117068/fasting-not-required-blood-testing/ (accessed on 7 August 2025).
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).