Effects of Multicomponent Exercise on Pain and Biopsychosocial Outcomes in Adults with Cancer: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Information Sources and Search Strategy
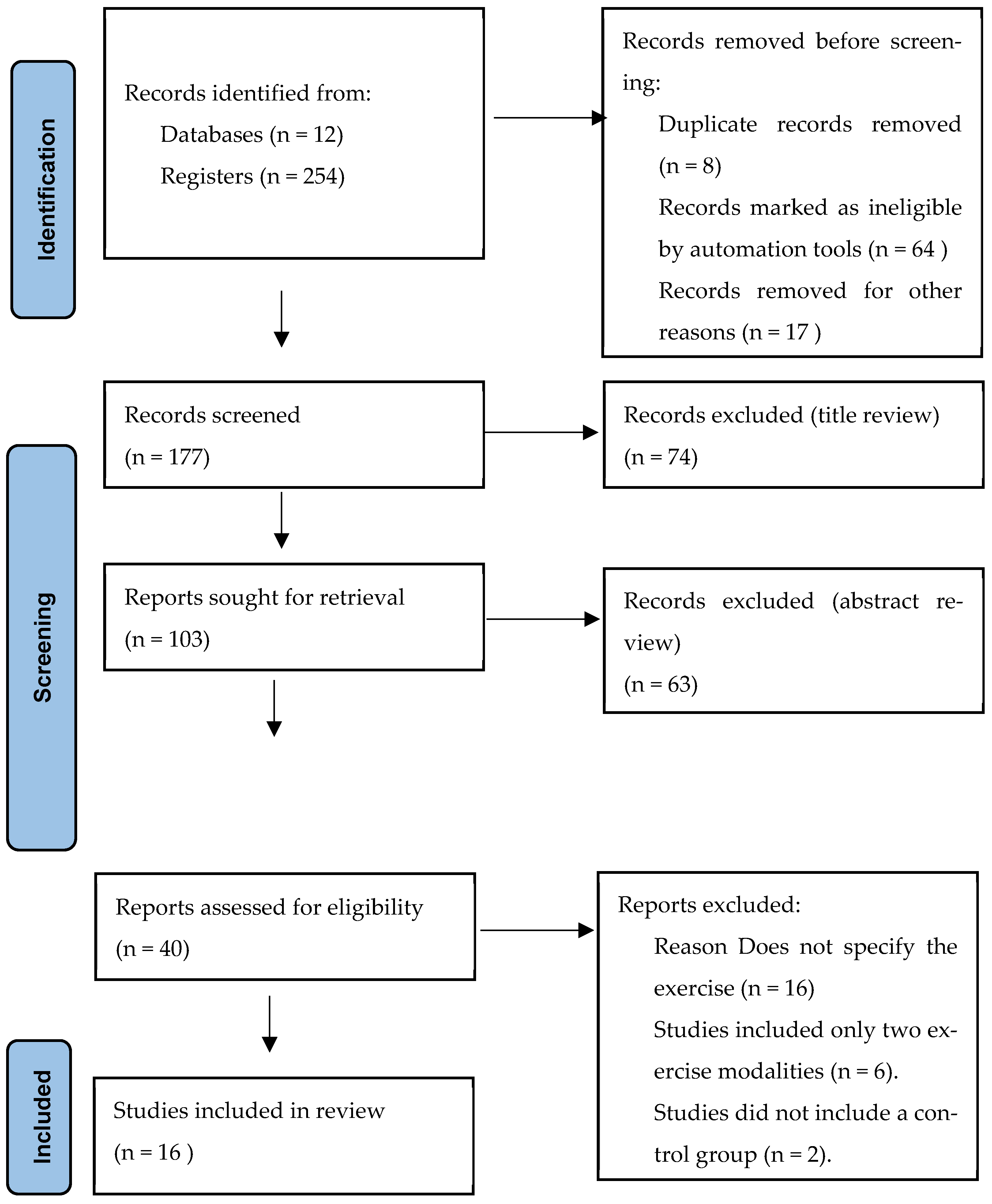
2.3. Study Selection
2.4. Data Collection Process
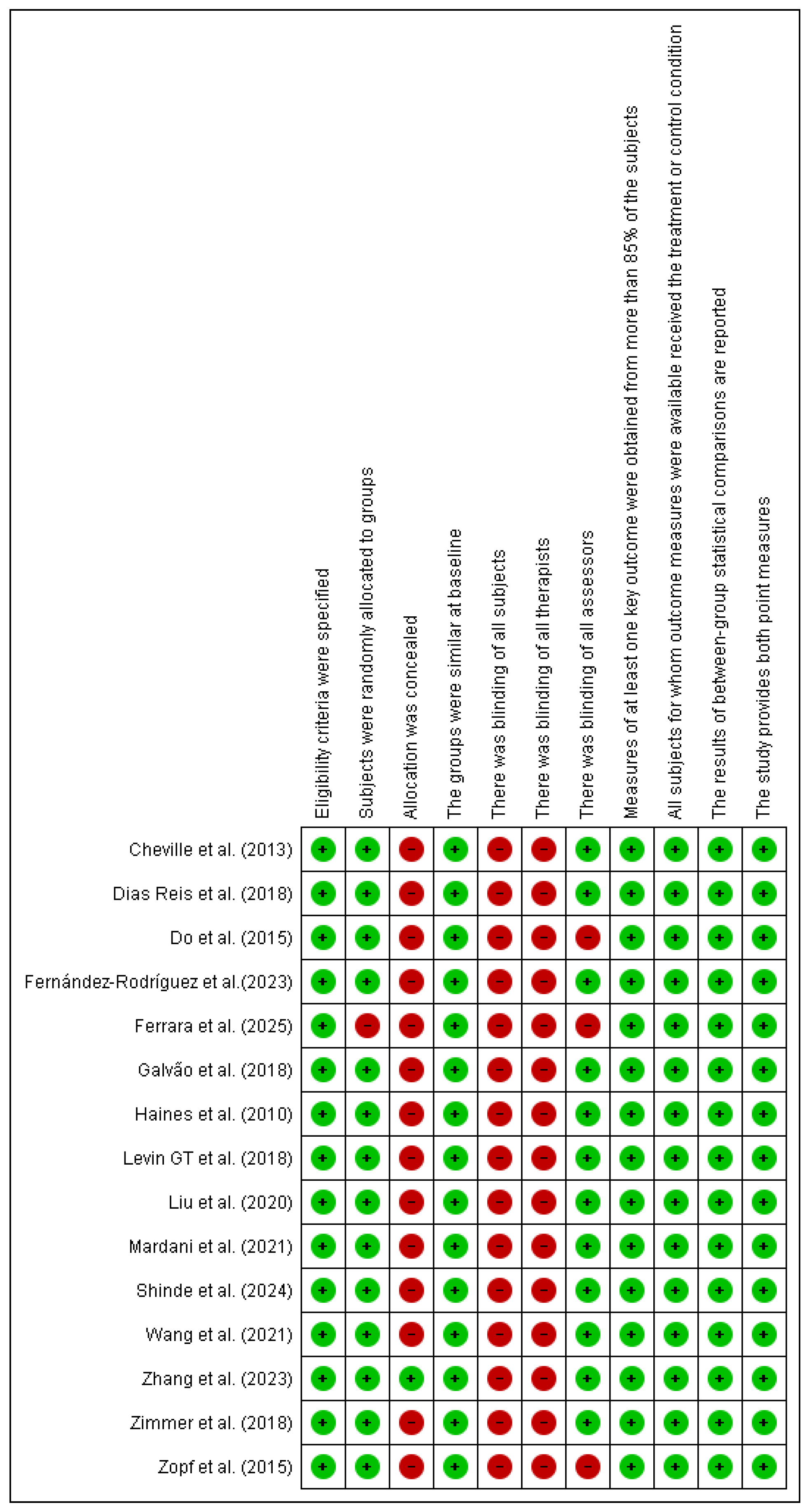
2.5. Quality Assessment and Risk of Bias
3. Results
3.1. Description of the Intervention
3.2. Description of Cancer Patient Characteristics
3.3. Description of the Main Results of the Study
3.3.1. Pain Outcomes
3.3.2. Disability Outcomes
3.3.3. Depression Outcomes
3.3.4. Quality of Life Outcomes
3.3.5. Physical Function Outcomes
3.3.6. Additional Findings
3.4. Risk of Bias Assessment
4. Discussion
4.1. Clinical Practice Implications
4.2. Research Implications
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Search Terms
| Search Combination Terms |
| Exercise therapy AND Cancer |
| Exercise multicomponent AND Cancer pain |
| Exercise multicomponent AND neoplasm |
| Exercise therapy AND Cancer pain |
| physical training AND Cancer Pain |
| Exercise therapy AND neoplasm |
| Exercise multicomponent AND Chemotherapy |
| Exercise multicomponent AND Radiation therapy |
| Exercise multicomponent AND Palliative therapy |
References
- PAHO/WHO Pan American Health Organization. World Cancer Day 2023: Close the Care Gap. Available online: https://www.paho.org/en/campaigns/world-cancer-day-2023-close-care-gap (accessed on 10 June 2025).
- Cancer. Available online: https://www.who.int/es/news-room/fact-sheets/detail/cancer (accessed on 10 June 2025).
- Cancer Today. Available online: https://gco.iarc.fr/today/en (accessed on 10 June 2025).
- American Cancer Society. Available online: https://www.cancer.org/es/cancer/diagnostico-y-etapa-del-cancer/senales-y-sintomas-del-cancer.html (accessed on 10 June 2025).
- VanHoose, L.; Black, L.L.; Doty, K.; Sabata, D.; Twumasi-Ankrah, P.; Taylor, S.; Johnson, R. An analysis of the distress thermometer problem list and distress in patients with cancer. Support. Care Cancer 2015, 23, 1225–1232. [Google Scholar] [CrossRef]
- Expósito Vizcaíno, S. Chronic Pain Associated with Cancer in Adults. Ph.D. Thesis, Universitat Rovira i Virgili, Tarragona, Spain, 26 November 2019. Available online: http://hdl.handle.net/10803/668978 (accessed on 10 March 2025).
- American Cancer Society. Available online: https://www.cancer.org/es/cancer/supervivencia/bienestar-tras-el-tratamiento/actividad-fisica-y-el-paciente-de-cancer.html (accessed on 10 June 2025).
- Traa, M.J.; De Vries, J.; Roukema, J.A.; Rutten, H.J.T.; Den Oudsten, B.L. The sexual health care needs after colorectal cancer: The view of patients, partners, and health care professionals. Support. Care Cancer 2014, 22, 763–772. [Google Scholar] [CrossRef]
- Paraskevi, T. Quality of life outcomes in patients with breast cancer. Oncol. Rev. 2012, 6, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Jansen, L.; Koch, L.; Brenner, H.; Arndt, V. Quality of life among long-term (≥5 years) colorectal cancer survivors—Systematic review. Eur. J. Cancer 2010, 46, 2879–2888. [Google Scholar] [CrossRef]
- Thewes, B.; Butow, P.; Zachariae, R.; Christensen, S.; Simard, S.; Gotay, C. Fear of cancer recurrence: A systematic literature review of self-report measures. Psychooncology 2012, 21, 571–587. [Google Scholar] [CrossRef]
- Kale, H.P.; Carroll, N.V. Self-reported financial burden of cancer care and its effect on physical and mental health-related quality of life among US cancer survivors. Cancer 2016, 122, 1283–1289. [Google Scholar] [CrossRef]
- Keesing, S.; Rosenwax, L.; McNamara, B. The implications of women’s activity limitations and role disruptions during breast cancer survivorship. Womens Health 2018, 14, 1745505718756381. [Google Scholar] [CrossRef]
- Bartley, E.J.; Fillingim, R.B. Sex differences in pain: A brief review of clinical and experimental findings. Br. J. Anaesth. 2013, 111, 52–58. [Google Scholar] [CrossRef]
- Miró, J.; de la Vega, R.; Gertz, K.J.; Jensen, M.P.; Engel, J.M. The Role of Perceived Family Social Support and Parental Solicitous Responses in Adjustment to Bothersome Pain in Young People with Physical Disabilities. Disabil. Rehabil. 2017, 41, 641. [Google Scholar] [CrossRef]
- Kuo, J.C.; Graham, D.M.; Salvarrey, A.; Kassam, F.; Le, L.W.; Shepherd, F.A.; Burkes, R.; Hollen, P.J.; Gralla, R.J.; Leighl, N.B. A Randomized Trial of the Electronic Lung Cancer Symptom Scale for Quality-of-Life Assessment in Patients with Advanced Non-small-Cell Lung Cancer. Curr. Oncol. 2020, 27, 156–162. [Google Scholar] [CrossRef]
- Hojman, P.; Gehl, J.; Christensen, J.F.; Pedersen, B.K. Molecular Mechanisms Linking Exercise to Cancer Prevention and Treatment. Cell Metab. 2018, 27, 10–21. [Google Scholar] [CrossRef]
- Courneya, K.S.; Vardy, J.L.; O’Callaghan, C.J.; Gill, S.; Friedenreich, C.M.; Wong, R.K.S.; Dhillon, H.M.; Coyle, V.; Chua, N.S.; Jonker, D.J.; et al. Structured Exercise after Adjuvant Chemotherapy for Colon Cancer. N. Engl. J. Med. 2025, 393, 13–25. [Google Scholar] [CrossRef]
- Miyamoto, T.; Nagao, A.; Okumura, N.; Hosaka, M. Effect of Post-diagnosis Physical Activity on Breast Cancer Recurrence: A Systematic Review and Meta-analysis. Curr. Oncol. Rep. 2022, 24, 1645–1659. [Google Scholar] [CrossRef]
- Cavalheri, V.; Burtin, C.; Formico, V.R.; Nonoyama, M.L.; Jenkins, S.; Spruit, M.A.; Hill, K. Exercise training undertaken by people within 12 months of lung resection for non-small cell lung cancer. Cochrane Database Syst. Rev. 2019, 6, CD009955. [Google Scholar] [CrossRef]
- Rosero, I.D.; Ramírez-Vélez, R.; Martínez-Velilla, N.; Cedeño-Veloz, B.A.; Morilla, I.; Izquierdo, M. Effects of a multicomponent exercise program in older adults with non-small-cell lung cancer during adjuvant/palliative treatment: An intervention study. J. Clin. Med. 2020, 9, 862. [Google Scholar] [CrossRef] [PubMed]
- Peddle-McIntyre, C.J.; Singh, F.; Thomas, R.; Newton, R.U.; Galvao, D.A.; Cavalheri, V. Exercise training for advanced lung cancer. Cochrane Database Syst. Rev. 2019, 2, CD012685. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T. Cochrane Handbook for Systematic Reviews of Interventions; Cochrane: London, UK, 2011. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 372, n71. [Google Scholar] [CrossRef]
- Nelson, M.E.; Rejeski, W.J.; Blair, S.N.; Duncan, P.W.; Judge, J.O.; King, A.C.; Macera, C.A.; Castaneda-Sceppa, C. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Med. Sci. Sports Exerc. 2007, 39, 1435–1445. [Google Scholar] [CrossRef]
- Izquierdo, M.; Merchant, R.A.; Morley, J.E.; Anker, S.D.; Aprahamian, I.; Arai, H.; Aubertin-Leheudre, M.; Bernabei, R.; Cadore, E.L.; Cesari, M.; et al. International Exercise Recommendations in Older Adults (ICFSR): Expert Consensus Guidelines. J. Nutr. Health Aging 2021, 25, 824–853. [Google Scholar] [CrossRef]
- Casas Herrero, Á.; Cadore, E.L.; Martínez Velilla, N.; Izquierdo Redin, M. El ejercicio físico en el anciano frágil: Una actualización [Physical exercise in the frail elderly: An update]. Rev. Esp. Geriatr. Gerontol. 2015, 50, 74–81. (In Spanish) [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef] [PubMed]
- Cheville, A.L.; Kollasch, J.; Vandenberg, J.; Shen, T.; Grothey, A.; Gamble, G.; Basford, J.R. A home-based exercise program to improve function, fatigue, and sleep quality in patients with Stage IV lung and colorectal cancer: A randomized controlled trial. J. Pain Symptom Manag. 2013, 45, 811–821. [Google Scholar] [CrossRef] [PubMed]
- Reis, A.D.; Pereira, P.T.V.T.; Diniz, R.R.; de Castro Filha, J.G.L.; dos Santos, A.M.; Ramallo, B.T.; Filho, F.A.A.; Navarro, F.; Garcia, J.B.S. Effect of exercise on pain and functional capacity in breast cancer patients. Health Qual. Life Outcomes 2018, 16, 58. [Google Scholar] [CrossRef]
- Mardani, A.; Pedram Razi, S.; Mazaheri, R.; Haghani, S.; Vaismoradi, M. Effect of the exercise programme on the quality of life of prostate cancer survivors: A randomized controlled trial. Int. J. Nurs. Pract. 2021, 27, e12883. [Google Scholar] [CrossRef]
- Wang, L.F.; Eaglehouse, Y.L.; Poppenberg, J.T.; Brufsky, J.W.; Geramita, E.M.; Zhai, S.; Davis, K.K.; Gibbs, B.B.; Metz, J.; van Londen, G.J. Effects of a personal trainer-led exercise intervention on physical activity, physical function, and quality of life of breast cancer survivors. Breast Cancer 2021, 28, 737–745. [Google Scholar] [CrossRef]
- Zimmer, P.; Trebing, S.; Timmers-Trebing, U.; Schenk, A.; Paust, R.; Bloch, W.; Rudolph, R.; Streckmann, F.; Baumann, F.T. Eight-week, multimodal exercise counteracts a progress of chemotherapy-induced peripheral neuropathy and improves balance and strength in metastasized colorectal cancer patients: A randomized controlled trial. Support. Care Cancer 2018, 26, 615–624. [Google Scholar] [CrossRef]
- Levin, G.T.; Greenwood, K.M.; Singh, F.; Newton, R.U. Modality of exercise influences rate of decrease in depression for cancer survivors with elevated depressive symptomatology. Support. Care Cancer 2018, 26, 1597–1606. [Google Scholar] [CrossRef]
- Liu, Z.; Qiu, T.; Pei, L.; Zhang, Y.; Xu, L.; Cui, Y.; Liang, N.; Li, S.; Chen, W.; Huang, Y. Two-week multimodal prehabilitation program improves perioperative functional capability in patients undergoing thoracoscopic lobectomy for lung cancer: A randomized controlled trial. Anesth. Analg. 2020, 131, 840–849. [Google Scholar] [CrossRef]
- Zopf, E.M.; Bloch, W.; Machtens, S.; Zumbé, J.; Rübben, H.; Marschner, S.; Kleinhorst, C.; Schulte-Frei, B.; Herich, L.; Felsch, M.; et al. Effects of a 15-Month Supervised Exercise Program on Physical and Psychological Outcomes in Prostate Cancer Patients Following Prostatectomy: The ProRehab Study. Integr. Cancer Ther. 2015, 14, 409–418. [Google Scholar] [CrossRef]
- Do, J.; Cho, Y.; Jeon, J. Effects of a 4-week multimodal rehabilitation program on quality of life, cardiopulmonary function, and fatigue in breast cancer patients. J. Breast Cancer 2015, 18, 87–96. [Google Scholar] [CrossRef]
- Shinde, S.B.; Jain, P.P.; Gudur, A.; Patil, S.K.; Shinde, R.V. Effect of Multi-component Exercise Program on Body Composition and Physical, Emotional and Social well being in Breast Cancer Survivors. Asian Pac. J. Cancer Prev. 2024, 25, 4397. [Google Scholar] [CrossRef]
- Shinde, S.B.; Jain, P.P.; Gudur, A.; Patil, S.K.; Shinde, R.V. Effect of Multi-component Exercise Program on Functional Performance in Breast Cancer Survivors. Asian Pac. J. Cancer Prev. 2024, 25, 4323–4331. [Google Scholar] [CrossRef]
- Ferrara, M.C.; Zambom-Ferraresi, F.; Castillo, A.; Delgado, M.; Galbete, A.; Arrazubi, V.; Morilla, I.; Zambom-Ferraresi, F.; Fernández González de la Riva, M.L.; Vera Garcìa, R.; et al. Effects of an individualised exercise program in hospitalised older adults with cancer: A randomised clinical trial. J. Nutr. Health Aging 2025, 29, 100424. [Google Scholar] [CrossRef]
- Fernandez-Rodriguez, E.J.; Sanchez-Gomez, C.; Mendez-Sanchez, R.; Recio-Rodriguez, J.I.; Puente-Gonzalez, A.S.; Gonzalez-Sanchez, J.; Cruz-Hernandez, J.J.; Rihuete-Galve, M.I. Multimodal Physical Exercise and Functional Rehabilitation Program in Oncological Patients with Cancer-Related Fatigue—A Randomized Clinical Trial. Int. J. Environ. Res. Public Health 2023, 20, 4938. [Google Scholar] [CrossRef] [PubMed]
- Haines, T.P.; Sinnamon, P.; Wetzig, N.G.; Lehman, M.; Walpole, E.; Pratt, T.; Smith, A. Multimodal exercise improves quality of life of women being treated for breast cancer, but at what cost? Randomized trial with economic evaluation. Breast Cancer Res. Treat. 2010, 124, 163–175. [Google Scholar] [CrossRef]
- Galvão, D.A.; Taaffe, D.R.; Spry, N.; Cormie, P.; Joseph, D.; Chambers, S.K.; Chee, R.; Peddle-McIntyre, C.J.; Hart, N.H.; Baumann, F.T.; et al. Exercise Preserves Physical Function in Prostate Cancer Patients with Bone Metastases. Med. Sci. Sports Exerc. 2018, 50, 393–399. [Google Scholar] [CrossRef]
- Zhang, H.; Meng, Y.; Jiang, R.; Ge, S.; Song, M. Effect of Multimodal Exercise on Cancer-Related Fatigue in Patients Undergoing Simultaneous Radiotherapy and Chemotherapy: A Randomized Trial in Patients with Breast Cancer. Altern. Ther. Health Med. 2023, 29, 233–237. [Google Scholar] [PubMed]
- Zhang, Y.; Li, G.; Zhang, S.; Zhou, Y.; Lv, Y.; Feng, L.; Yu, L. Effects of Exercise on Depression and Anxiety in Breast Cancer Survivors: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Cancer Med. 2025, 14, e70671. [Google Scholar] [CrossRef]
- Correia, I.R.; Cardoso, V.; Cargaleiro, C.; Magalhães, J.P.; Hetherington-Rauth, M.; Rosa, G.B.; Malveiro, C.; de Matos, L.V.; Cardoso, M.J.; Sardinha, L.B. Effects of home-based exercise programs on physical fitness in cancer patients undergoing active treatment: A systematic review and meta-analysis of randomized controlled trials. J. Sci. Med. Sport 2023, 26, 222–231. [Google Scholar] [CrossRef]
- Bowers, M.; Petrasso, C.; McLuskie, A.; Bayly, J.; Laird, B.J.A.; Higginson, I.J.; Maddocks, M. Multicomponent Interventions for Adults With Cancer Cachexia: A Systematic Review. J. Cachexia Sarcopenia Muscle 2025, 16, e13716. [Google Scholar] [CrossRef]
- Murnaghan, S.; Scruton, S.; Urquhart, R. Psychosocial interventions that target adult cancer survivors’ reintegration into daily life after active cancer treatment: A scoping review. JBI Evid. Synth. 2024, 22, 607–656. [Google Scholar] [CrossRef]
- González-Santos, Á.; Lopez-Garzon, M.; Gil-Gutiérrez, R.; del Mar Salinas-Asensio, M.; Postigo-Martin, P.; Cantarero-Villanueva, I. Nonlinear, Multicomponent Physical Exercise With Heart Rate Variability-Guided Prescription in Women With Breast Cancer During Treatment: Feasibility and Preliminary Results (ATOPE Study). Phys. Ther. 2023, 103, pzad070. [Google Scholar] [CrossRef]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014, 348, g1687. [Google Scholar] [CrossRef]
| Author | Population/Mean Age | Type of Cancer | Stage | Intervention | Control | Pharmacological Treatment | Scales Used |
|---|---|---|---|---|---|---|---|
| Cheville et al. (2013) [29] | IG: N = 33, mean 63; CG: N = 33, mean 65 | Colorectal, lung | IV | Program: aerobic, resistance with bands, flexibility | No prescribed exercise; booklet after study | NM | NRS, FACT-G |
| Reis et al. (2018) [30] | IG: N = 14, mean 47; CG: N = 14, mean 45 | Breast | NM | 12-week aerobic, resistance, flexibility training | Standard hospital care | NM | BPI |
| Mardani et al. (2021) [31] | IG: N = 35, mean 69; CG: N = 36, mean 70 | Prostate | NM | Aerobic, resistance, flexibility, pelvic floor muscle exercises | Routine medical care; maintain usual physical activity/diet | NM | EORTC QLQ-C30 |
| Wang et al. (2021) [32] | G: N = 23, mean 55; CG: N = 26, mean 56 | Breast | NM | Personalized program: flexibility, wall push-ups, upper body resistance, warm-up/cooldown | Waitlist control with initial evaluation | NM | QoL instrument |
| Zimmer et al. (2018) [33] | IG: N = 17, mean 68; CG: N = 13, mean 70 | Colorectal | IV | 8-week supervised, endurance, Strength training, balance, coordination (2 week, 60 min) | Standard written recommendations | Chemotherapy (FOLFIRI, FOLFOX, oxaliplatin), Capecitabine, Bevacizumab, Regorafenib, Trastuzumab | FACT; GOG; h1RM; GGT-Reha; 6MWT |
| Levin GT et al. (2018) [34] | IG: EX: N = 10; SMHB: N = 8; CG: N = 14 | Breast, Brain, Prostate, Kidney, Bladder | NM | EX: supervised resistance/aerobic, flexibility training 2/week; SMHB: self -managed ≥ 150 min/week aerobics. SMHB: received an exercise information booklet. Complete at least 150 min of aerobic exercise per week in sessions of 10 min or more | Only completing the questionnaire component of the study. | Chemotherapy and radiotherapy | HADS-D; HADS-A; GLTEQ; SF-36 (PHC and MHC); 400-m test |
| Liu et al. (2020) [35] | IG: N = 37; CG: N = 36 | Lung: non-small cell lung carcinoma (NSCLC) | I–III: 89% in stages I–II, 11% in stage III | Aerobic exercise comprised the core activity of the intervention program. A 30-min home-based exercise of aerobic endurance exercise (jogging, walking, cycling, at discretion) was required for at least 3 days per week. Resistance exercise involving the major muscle groups (upper and lower limbs, chest and core muscles) was performed twice a week. | Usual clinical care | NM | WHODAS 2.0; 6MWD |
| Zopf et al. (2015) [36] | IG: N = 56; CG: N = 29 | Prostate | II | 15-month program: weekly 1-h sessions of aerobic, resistance, flexibility, coordination and pelvic floor exercises | No intervention | NM | EORTC-QLQ-C30; PCa (EORTC QLQ-PR25), Freiburger Questionnaire of Physical Activity. |
| Do et al. (2015) [37] | IG: N = 32; CG: N = 30 | Breast | NM | Early/late groups: 4 weeks, 5/week, 80 min/day exercise (aerobic, strength, flexibility and core stability exercise) | Delayed exercise group receiving the same program starting after 4 weeks | NM | EORTC QLQ-C30; EORTC QLQ-BR23; FSS |
| Shinde et al. (2024) [38,39] | IG: N = 64, mean 50.9 ± 8.4; CG: N = 60, mean 49.7 ± 8.0 | Breast | I–III | Phases 1–3 (12 months): progressive aerobic, strength (manual, isometric, resistance), flexibility, mobility, energy conservation strategies, and recreational therapy; home-based and supervised | Supportive therapy: health education, nutrition counseling, psychological counseling | Chemotherapy, radiotherapy, hormonal therapy (unspecified) | FACT-B |
| Ferrara et al. (2025) [40] | IG: N = 28, mean 74.4 ± 5.3; CG: N = 30, mean 74.4 ± 5.2 | Colorectal, Upper digestive, Lung, Breast, Genitourinary, Head/Neck | III–IV | Supervised progressive resistance, balance training, walking (4 consecutive days, 2 sessions/day, 20 min each) | Usual care | NM | SPPB; Yesavage Geriatric Depression Scale; EORTC QLQ-C30; 1RM; Handgrip dynamometry |
| Fernández-Rodríguez et al. (2023) [41] | IG: N = 24; CG: N = 24, mean 63.5 ± 12.5 | Lung, Digestive, Prostate, Breast, Others | II–IV | Aerobic, resistance, balance, moderate-load strength, flexibility; 2 sessions/day (15–20 min/session) | Standard care + educational lifestyle program | NM | VAS; Barthel Index; FACT; EuroQoL; SPPB |
| Haines et al. (2010) [42] | IG: N = 46, mean 55.9; CG: N = 43, mean 54.2 | Breast | NM | Strength, balance, shoulder mobility, aerobic training | Flexibility and relaxation program | NM | EQ-5D; EORTC QLQ-C30; BR23 |
| Galvão et al. (2018) [43] | IG: N = 28; CG: N = 29, mean 70 | Prostate | IV | Supervised resistance, aerobic, flexibility (3x/week, 3 months) | Usual medical treatment | ADT: 95%; Chemotherapy: 16% | FACT-BP; SF-36; Self-reported physical function; 6MW; TUG |
| Zhang et al. (2023) [44] | IG: N = 92, mean 48.6; CG: N = 42, mean 49.3 | Breast | NM | 5-week hospital + home aerobic, strength, flexibility training | Usual care | NM | HADS; EORTC QLQ-C30 |
| Author | Pain (Instrument & Outcome) | Disability (Instrument & Result) | QoL (Instrument & Result) | Physical Function (PF) (Instrument & Result) | Key Notes |
|---|---|---|---|---|---|
| Cheville et al. (2013) [29] | NRS: IG −0.62 ± 2.59 CG −0.50 ± 2.01 (p = 0.87) | NM | Mobility: IG 4.88 ± 4.66 CG 0.23 ± 5.22 (p = 0.002); Activity: IG 1.56 ± 5.53, CG 0.94 ± 5.91 (p = 0.74) FACT-G: IG 1.07 ± 11.60 CG 0.12 ± 10.22 (p = 0.54) | NM | Pain unchanged; active mobility (QOL) improved in IG. |
| Reis et al. (2018) [30] | BPI: IG 2.43 ± 3.76 CG 3.93 ± 4.41 Total pain ↓ (p = 0.0047); general intensity (p = 0.0082); greater (p = 0.0284); lesser (p = 0.0365); interference in daily life (p = 0.0201) | NM | NM | VO2 max: IG 20.68 ± 2.50 CG 14.80 ± 2.46 (p = 0.0001) Handgrip right: IG 24.79 ± 6.77 CG 21.71 ± 7.44 (p = 0.0001) | ↓ Pain; ↑ VO2max and handgrip strength in IG. |
| Mardani et al. (2021) [31] | EORTC QLQ-C30 Pain: IG 40.47 ± 16.31 p = 0.002, CG 28.24 ± 15.84 | NM | EORTC QLQ-C30: IG Pre 60.19 ± 13.95 Post 72.57 ± 11.63 CG Pre 61.12 ± 14.10 CG Post 63.40 ± 12.80 p < 0.001 | ↓ Pain; ↑ Global QOL in IG. | |
| Wang et al. (2021) [32] | NM | NM | FACT-ES IG: 151 ± 14 change +1 [−2, 4] CG: 142 ± 26 change −1 [−5, 3] p = 0.023 | Steps/2 min IG 101 ± 23 change +18 [8, 28] CG 106 ± 23 change 9 [5, 13] p = 0.036 | ↑ QOL; ↑ Physical function in IG. |
| Zimmer et al. (2018) [33] | NM | NM | FACT-G: IG Pre 75.05 ± 14.82 IG Post 77.35 ± 11.83. CG Pre 76.42 ± 15.21 CG post 75.10 ± 14.95 p = 0.028 | 6 MWT distance: IG Pre 477.735 ± 91.911 IG Post 519.059 ± 68.958 CG Pre 459.654 ± 74.061 CG Post 482.154 ± 82.641 p = 0.432 h1RM [kg] leg press IG Pre 142.156 ± 44.125 Post 179.664 ± 68.196 p = 0.011 CG Pre 166.717 ± 56.304 159.991 ± 62.154 | ↑ QOL; ↑ Physical function in IG. |
| Levin GT et al. (2018) [34] | NM | NM | SF36 MHC Baseline: IG: 40.86 (9.82), SMHB: 43.84 (13.13), CG:44.09 (6.46) Week 6: IG: 44.23 (10.34), SMHB: 53.16 (5.75), CG: 41.94 (11.53) Week 12: IG: 51.63 (8.07), SMHB: 50.78 (9.87), CG: 40.85 (10.04) p: 0.005 | 400-m walk: Baseline: IG: 236.65 (40.43), SMHB: 251.39 (20.63) Week 6: IG: 226.48 (35.65), SMHB: 239.55 (22.77) Week 12: EX: 218.57 (32.75), SMHB: 231.01 (22.88) p = 0.466 | ↑ QOL (MHC) in IG. |
| Liu et al. (2020) [35] | NM | WHODAS 2.0a: Mean Difference Between Prehabilitation and Control Groups (95% CI): −1.0 (−2.4 to 0.4) p: 0.152 | NM | 6MWD (m): Mean Difference Between Prehabilitation and Control Groups (95% CI): 60.9 (32.4 to 89.5) p: < 0.001 | ↑ 6MWD in IG |
| Zopf et al. (2015) [36] | EORTC QLQ-C30 Pain IG: −2.37 points p = 0.679 CG: +3.33 points: p = 0.704 | NM | EORTC QLQ-30: Change from Baseline to posttest IG: Mean 6.83 p: 0.064 CG: Mean 1.75 p: 0.717 | EORTC QLQ-30: Change from Baseline to posttest IG: Mean 9.67 p: < 0.001 CG: Mean 4.20 p: 0.303 | ↑ Physical function in IG. |
| Do et al. (2015) [37] | EORTC QLQ-C30 Pain: IG pre 40.9 ± 28.1, IG post 19.4 ± 13.6, p < 0.001; CG no significant change | NM | EORTC QLQ-C30 IG pre 58.0 ± 18.6 IG post 87.3 ± 13.7 CG pre 59.5 ± 17.9 CG Post 61.0 ± 17.5 p = < 0.001 | EORTC QLQ-C30 Physical function: IG pre 74.1 ± 17.3, IG post 89.4 ± 8.4, p < 0.001; CG similar later improvement | ↑ QOL in IG. |
| Shinde et al. (2024) [38] | NM | NM | FACT-B: IG Pre 99.12 ± 10.24 IG Post 111.07 ± 11.61 CG Pre 100.05 ± 11.02 CG Post 102.15 ± 10.85 p = 0.001 | NM | ↑ QOL in IG. |
| Shinde et al. (2024) [39] | NM | NM | NM | STS: IG Pre 12.96 ± 4.24 IG Post 17.12 ± 7.39 p = 0.0002 CG Pre 13.86 ± 4.78 CG Post 14.2 ± 4.59 p = 0.92 12MWT IG Pre 1242.73 ± 205.68 IG post 1309.37 ± 167.35 p = 0.008 CG Pre 1249.91 ± 213.18 CG Post 1254 ± 186.59 p = 0.93 | ↑ PF in IG |
| Ferrara et al. (2025) [40] | NM | NM | EORTC QLQ-C30: IG 6.59, CG 4.93; Diff 1.65 (p = NS) | Leg press 1RM IG +9.54 (2.14–16.8) p = 0.153 Knee extension 1RM IG +9.77 (5.33 51.5) p = 0.018 SPPB IG 2.30 (1.43, 3.18) CG 0.38 (−0.34, 1.09) p = 0.002 | No changes QOL; ↑ Knee extensor strength & balance in IG. |
| Fernández-Rodríguez et al. (2023) [41] | VAS: IG Pre 4.29 ± 2.21 IG Post 3.58 ± 2.78; EQ-5D Pain IG Pre: 1.96 ± 0.69 IG Post 1.71 ± 0.62 (p = 0.334) | NM | FACT: IG Pre 94.96 ± 11.91 IG Post 102.75 ± 13.00 CG Pre 95.10 ± 11.70 CG Post 96.00 ± 11.50 p = 0.036 | SPPB total IG 6.21 ± 2.99 CG 4.42 ± 3.03 p = 0.045 SPPB gait IG 1.75 ± 0.94 CG 1.17 ± 0.91 p = 0.035 | ↑ QOL (follow-up IG); ↑ PF. |
| Haines et al. (2010) [42] | EQ-5D VAS: IG 80.6, CG 74.1 comparison 10.08 (2.84, 17.32) (p = 0.006) | NM | EORTC QLQ-C30 IG Pre 69.4 ± 15.1 IG Post 76.6 ± 15.0 CG Pre 70.0 ± 14.9 CG Post 71.2 ± 15.1 p = 0.04 | 6MWT (m) IG 535 ±110, CG 532 ± 82 comparison 22.52 (−23.24, 68.28), p = 0.34 Grip strength (kg) IG 25.4 ± 7.7 CG 24.2 ± 5.4, comparison −1.24 (−4.65, 2.17) p = 0.48 | ↑ QOL in IG; no change in PF. |
| Galvão et al. (2018) [43] | FACT-BP: p = 0.507 | NM | NM | Leg extension 1RM IG +6.6 kg (95% CI 0.6 12.7) p = 0.033 | No change in pain; ↑ PF. |
| Zhang et al. (2023) [44] | NM | NM | EORTC QLQ-C30 FF, FE, SG, Fatigue, Insomnia (all p < 0.05) | ↑ QOL in IG |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ordoñez-Mora, L.T.; Gómez-Gómez, J.F.; Marquez-Bustamante, M.; Rosero, I.D.; Rivas-Tafurt, G.P.; Estela-Zape, J.L. Effects of Multicomponent Exercise on Pain and Biopsychosocial Outcomes in Adults with Cancer: A Systematic Review. Healthcare 2025, 13, 2842. https://doi.org/10.3390/healthcare13222842
Ordoñez-Mora LT, Gómez-Gómez JF, Marquez-Bustamante M, Rosero ID, Rivas-Tafurt GP, Estela-Zape JL. Effects of Multicomponent Exercise on Pain and Biopsychosocial Outcomes in Adults with Cancer: A Systematic Review. Healthcare. 2025; 13(22):2842. https://doi.org/10.3390/healthcare13222842
Chicago/Turabian StyleOrdoñez-Mora, Leidy Tatiana, Juan Fernando Gómez-Gómez, Mateo Marquez-Bustamante, Ilem D. Rosero, Giovanna Patricia Rivas-Tafurt, and Jose Luis Estela-Zape. 2025. "Effects of Multicomponent Exercise on Pain and Biopsychosocial Outcomes in Adults with Cancer: A Systematic Review" Healthcare 13, no. 22: 2842. https://doi.org/10.3390/healthcare13222842
APA StyleOrdoñez-Mora, L. T., Gómez-Gómez, J. F., Marquez-Bustamante, M., Rosero, I. D., Rivas-Tafurt, G. P., & Estela-Zape, J. L. (2025). Effects of Multicomponent Exercise on Pain and Biopsychosocial Outcomes in Adults with Cancer: A Systematic Review. Healthcare, 13(22), 2842. https://doi.org/10.3390/healthcare13222842








