Lost Futures: The Human and Economic Cost of Suicide in Türkiye, 2012–2023
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. Statistical Analysis
2.2.1. Calculation of Crude and Standardized Rates
2.2.2. Joinpoint Regression
2.2.3. Calculation of YLL and YPLL
2.2.4. Human Capital Approach
3. Results
3.1. Crude and Standardized Suicidal Rate
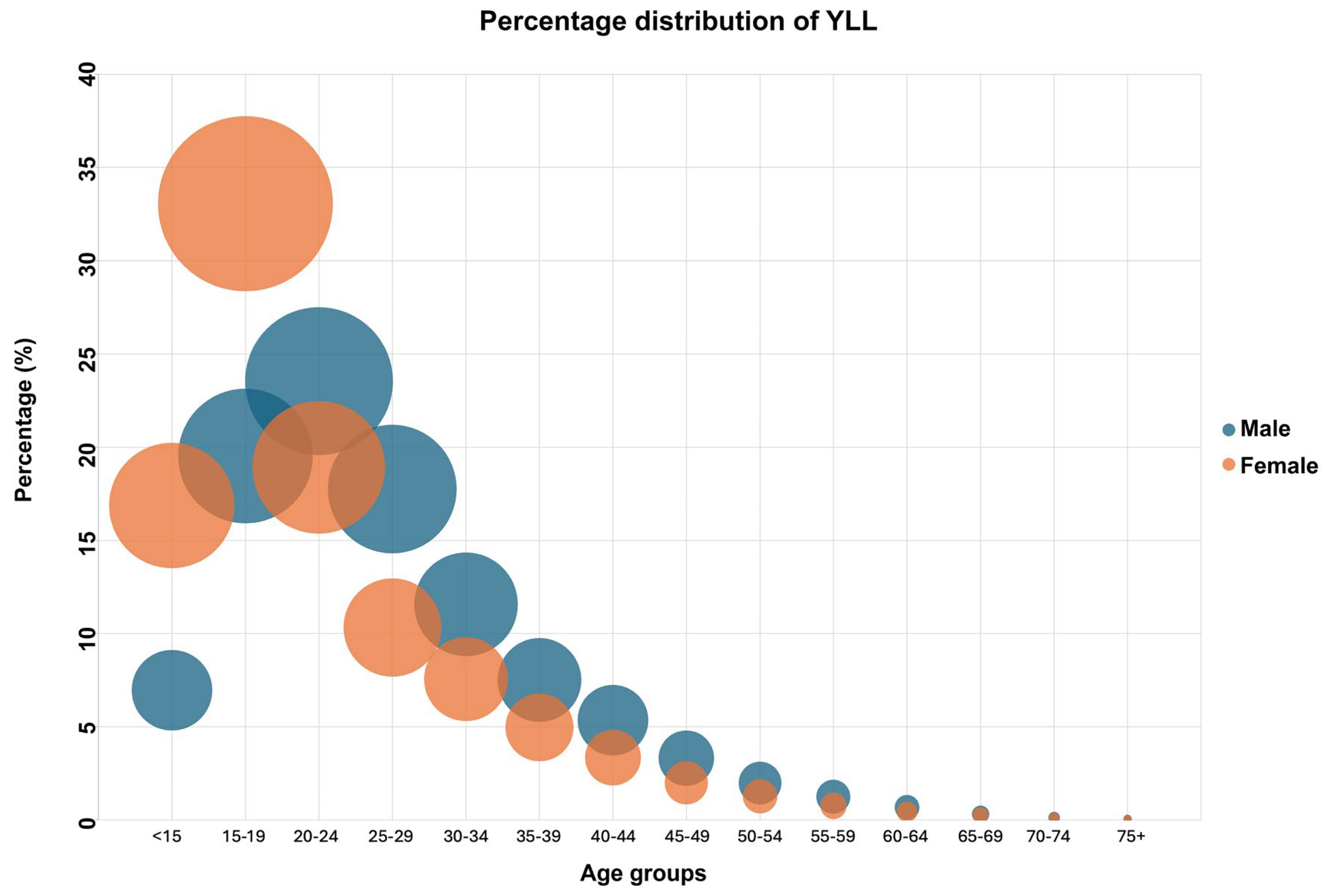
3.2. YLL Due to Suicide
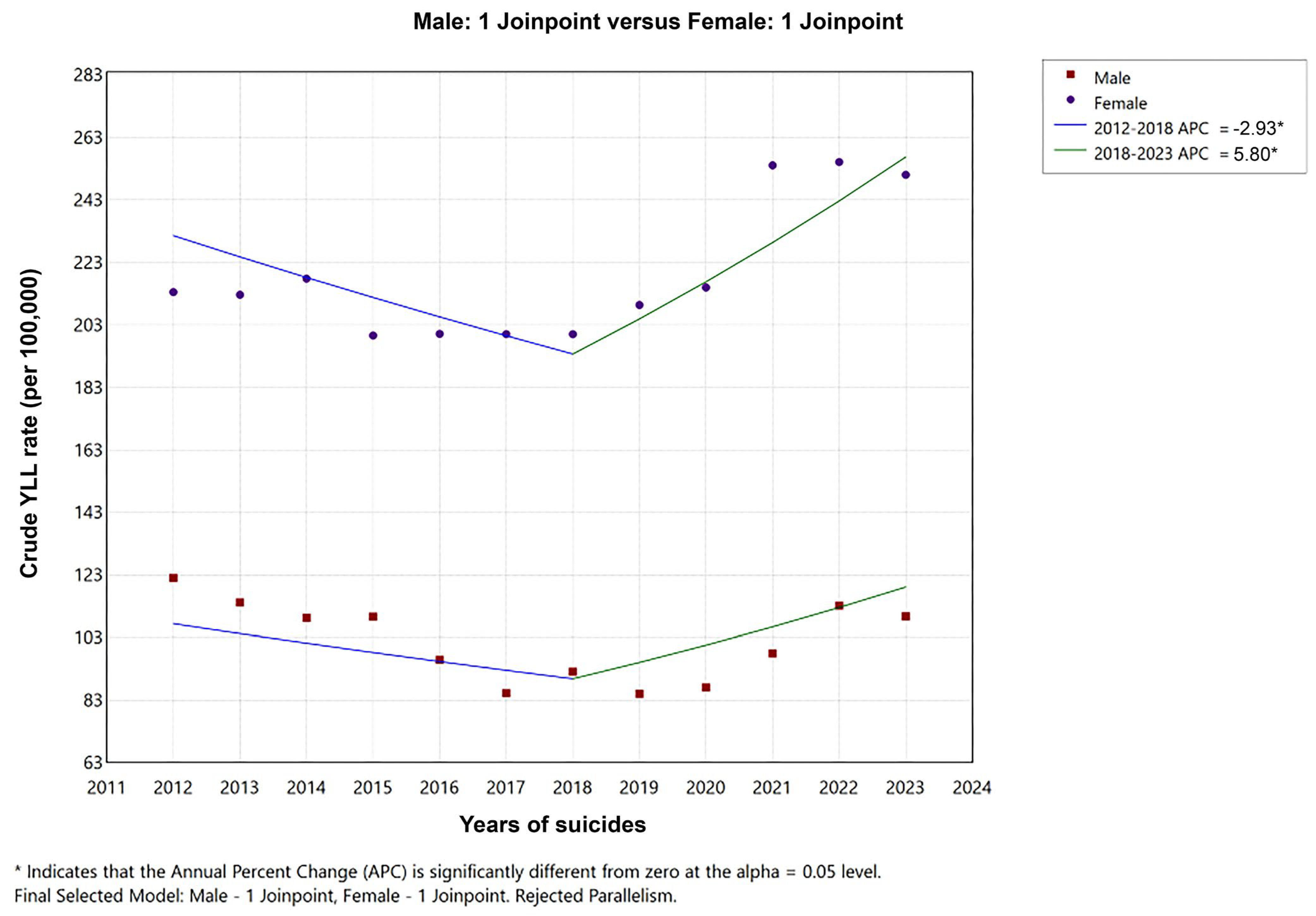
3.3. Time Trend of Suicides
3.4. YPLL Due to Suicide
3.5. Cost of Suicides Based on the Human Capital Method
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Suicide. Available online: https://www.who.int/news-room/fact-sheets/detail/suicide (accessed on 2 July 2025).
- Safarpour, H.; Sohrabizadeh, S.; Malekyan, L.; Safi-Keykaleh, M.; Pirani, D.; Daliri, S. Suicide death rate after disasters: A meta-analysis study. Arch. Suicide Res. 2022, 26, 14–27. [Google Scholar] [CrossRef]
- Zalsman, G.; Stanley, B.; Szanto, K.; Clarke, D.E.; Carli, V.; Mehlum, L.; Wasserman, D. Suicide in the time of COVID-19: Review and recommendations. Arch. Suicide Res. 2020, 24, 477–482. [Google Scholar] [CrossRef]
- Baeza, F.; González, F.; Benmarhnia, T.; Vives Vergara, A. Effects of the Great Recession on suicide mortality in Chile and contributing factors. SSM Ment. Health 2022, 2, 100104. [Google Scholar] [CrossRef]
- Vijayakumar, L.; John, S.; Pirkis, J.; Whiteford, H. Suicide prevention in developing countries (2): The WHO workshop in Chennai, India. Crisis 2005, 26, 120–124. [Google Scholar] [CrossRef] [PubMed]
- Owen, D.W.; Korkut-Owen, F.; Kurter, M.F. Career development in Turkey: An evolving profession. Career Plan. Adult Dev. J. 2011, 27, 39–52. [Google Scholar]
- Ozdinc, F. Examining the Status Quo Bias for the Recent Global Economic Crisis: The Case of Türkiye. Iğdır Univ. J. Soc. Sci. 2023, 37, 431–444. [Google Scholar] [CrossRef]
- Goktas, S.; Metintas, S. Suicide mortality trends by age, gender and method in Turkey. Turk. J. Public Health 2019, 17, 195–206. [Google Scholar]
- Turkish Statistical Institute (TurkStat). Suicide Statistics. Available online: https://data.tuik.gov.tr/Kategori/GetKategori?p=Nufus-ve-Demografi-109 (accessed on 23 July 2025).
- Lee, D.J.; Park, K.S. Association Between Physical Activity and Suicidal Ideation: The Moderating Effect of Self-Rated Health Status. Healthcare 2025, 13, 1506. [Google Scholar] [CrossRef] [PubMed]
- Casant, J.; Helbich, M. Inequalities of Suicide Mortality across Urban and Rural Areas: A Literature Review. Int. J. Environ. Res. Public Health 2022, 19, 2669. [Google Scholar] [CrossRef]
- Jia, P.; Zhuang, J.; Vaca Lucero, A.M.; Osei, C.D.; Li, J. Does Participation in Local Non-Agricultural Employment Improve the Mental Health of Elderly Adults in Rural Areas? Evidence from China. Front. Public Health 2021, 9, 746580. [Google Scholar] [CrossRef]
- Casas, L.; Cox, B.; Bauwelinck, M.; Nemery, B.; Deboosere, P.; Nawrot, T.S. Does Air Pollution Trigger Suicide? A Case-Crossover Analysis of Suicide Deaths over the Life Span. Eur. J. Epidemiol. 2017, 32, 973–981. [Google Scholar] [CrossRef]
- World Health Organization. Preventing Suicide: A Global Imperative; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- World Health Organization. Suicide Worldwide in 2021: Global Health Estimates; World Health Organization: Geneva, Switzerland, 2025. [Google Scholar]
- Kim, J.L.; Cho, K.H.; Park, E.C.; Cho, W.H. A single measure of cancer burden combining incidence with mortality rates for worldwide application. Asian Pac. J. Cancer Prev. 2014, 15, 433–439. [Google Scholar] [CrossRef]
- Ledesma-Cuenca, A.; Montañés, A.; Simón-Fernández, M.B. Disparities in premature mortality: Evidence for the OECD countries. Soc. Sci. Med. 2022, 307, 115198. [Google Scholar] [CrossRef] [PubMed]
- Lucas, R.E., Jr. On the Mechanics of Economic Development. J. Monet. Econ. 1988, 22, 3–42. [Google Scholar] [CrossRef]
- Łyszczarz, B. Production losses attributable to suicide deaths in European Union. BMC Public Health 2021, 21, 950. [Google Scholar] [CrossRef]
- Khorasani, S.; Rezaei, S.; Rashidian, H.; Daroudi, R. Years of potential life lost and productivity costs due to premature cancer-related mortality in Iran. Asian Pac. J. Cancer Prev. 2015, 16, 1845–1850. [Google Scholar] [CrossRef]
- Hanly, P.A.; Sharp, L. The cost of lost productivity due to premature cancer-related mortality: An economic measure of the cancer burden. BMC Cancer 2014, 14, 224. [Google Scholar] [CrossRef] [PubMed]
- Nigam, A.; Vuddemarry, M.; Zadey, S. Economic burden of suicide deaths in India (2019): A retrospective, cross-sectional study. Lancet Reg. Health Southeast Asia 2024, 29, 100477. [Google Scholar] [CrossRef]
- Organisation for Economic Co-operation and Development (OECD). OECD Economic Surveys: Türkiye 2025; OECD Publishing: Paris, France, 2025. [Google Scholar] [CrossRef]
- Turkish Statistical Institute (TurkStat). Death and Cause of Death Statistics. 2024. Available online: https://data.tuik.gov.tr/Bulten/Index?p=Olum-ve-Olum-Nedeni-Istatistikleri-2024-54195 (accessed on 23 August 2025).
- Organisation for Economic Co-operation and Development (OECD). Global Economy and Turkey: An OECD Perspective. Available online: https://www.oecd.org/turkey/theglobaleconomyandturkeyanoecdperspective.htm (accessed on 22 March 2024).
- International Labour Organization (ILO). Unemployment and Labour Underutilization. Available online: https://ilostat.ilo.org/topics/unemployment-and-labour-underutilization (accessed on 22 March 2024).
- Ahmad, O.B.; Boschi-Pinto, C.; Lopez, A.D.; Murray, C.J.; Lozano, R.; Inoue, M. Age Standardization of Rates: A New WHO Standard; World Health Organization: Geneva, Switzerland, 2001; Volume 9, pp. 1–14. [Google Scholar]
- Yoshioka, E.; Hanley, S.; Kawanishi, Y.; Saijo, Y. Time trends in method-specific suicide rates in Japan, 1990–2011. Epidemiol. Psychiatr. Sci. 2016, 25, 58–68. [Google Scholar] [CrossRef]
- National Cancer Institute. Joinpoint Trend Analysis Software; National Cancer Institute: Bethesda, MD, USA, 2023. Available online: https://surveillance.cancer.gov/joinpoint/ (accessed on 22 March 2024).
- Murray, C. Quantifying the burden of disease: The technical basis for disability-adjusted life years. Bull. World Health Organ. 1994, 72, 429–445. [Google Scholar]
- Devleesschauwer, B.; Havelaar, A.H.; Maertens de Noordhout, C.; Haagsma, J.A.; Praet, N.; Dorny, P.; Duchateau, L.; Torgerson, P.R.; Van Oyen, H.; Speybroeck, N. Calculating disability-adjusted life years to quantify burden of disease. Int. J. Public Health 2014, 59, 565–569. [Google Scholar] [CrossRef] [PubMed]
- Hanly, P.; Soerjomataram, I.; Sharp, L. Measuring the societal burden of cancer: The cost of lost productivity due to premature cancer-related mortality in Europe. Int. J. Cancer 2015, 136, E136–E145. [Google Scholar] [CrossRef]
- Turkish Statistical Institute (TurkStat). Adrese Dayalı Nüfus Kayıt Sistemi Sonuçları–2024. Available online: https://data.tuik.gov.tr/Bulten/Index?p=Adrese-Dayali-Nufus-Kayit-Sistemi-Sonuclari-2024-53783 (accessed on 23 July 2025).
- Organisation for Economic Co-operation and Development (OECD). Working-Age Population (Indicator). 2023. Available online: https://www.oecd.org/en/data/indicators/working-age-population.html (accessed on 23 July 2025).
- Metintas, S.; Ak, G.; Metintas, M. Potential Years of Life and Productivity Loss Due to Malignant Mesothelioma in Turkey. Arch. Environ. Occup. Health 2020, 75, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Najafi, F.; Karami-Matin, B.; Rezaei, S.; Khosravi, A.; Soofi, M. Productivity costs and years of potential life lost associated with five leading causes of death: Evidence from Iran (2006–2010). Med. J. Islam. Repub. Iran 2016, 30, 412. [Google Scholar]
- Mosegui, G.B.; Antoñanzas, F.; de Mello Vianna, C.M. Cost of Lost Productivity from Acute Respiratory Infections in South America. Rev. Panam. Salud Pública 2023, 47, e65. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Making Choices in Health: WHO Guide to Cost-Effectiveness Analysis; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Organisation for Economic Co-operation and Development (OECD). Cost-Benefit Analysis and the Environment: Further Developments and Policy Use; OECD Publishing: Paris, France, 2018. [Google Scholar]
- Freeman, M.C.; Groom, B.; Turk, Z. Social Discount Rates for Cost-Benefit Analysis: A Review; International Seabed Authority: Kingston, Jamaica, 2020. [Google Scholar]
- T.C. Sağlık Bakanlığı. Sağlık Teknolojilerinin Değerlendirilmesi (HTA) Rehberi; Sağlık Bakanlığı Yayınları: Ankara, Türkiye, 2010. [Google Scholar]
- Ortiz-Ortiz, K.J.; Pérez-Irizarry, J.; Marín-Centeno, H.; Ortiz, A.P.; Torres-Berrios, N.; Torres-Cintron, M.; de la Torre-Feliciano, T.; Laborde-Rivera, J.; Calo, W.A.; Figueroa-Valles, N.R. Productivity loss in Puerto Rico’s labor market due to cancer mortality. Puerto Rico Health Sci. J. 2010, 29, 241–249. [Google Scholar]
- Bang, K.M.; Mazurek, J.M.; Wood, J.M.; Hendricks, S.A. Diseases attributable to asbestos exposure: Years of potential life lost, United States, 1999–2010. Am. J. Ind. Med. 2014, 57, 38–48. [Google Scholar] [CrossRef]
- World Bank. Country and Lending Groups. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed on 23 August 2025).
- World Health Organization. Suicide Mortality Rate (Per 100,000 Population). Available online: https://data.who.int/indicators/i/F08B4FD/16BBF41 (accessed on 23 August 2025).
- Eskin, M.; Baydar, N.; El-Nayal, M.; Asad, N.; Noor, I.M.; Rezaeian, M.; Abdel-Khalek, A.M.; Al Buhairan, F.; Harlak, H.; Hamdan, M.; et al. Associations of religiosity, attitudes towards suicide and religious coping with suicidal ideation and suicide attempts in 11 Muslim countries. Soc. Sci. Med. 2020, 265, 113390. [Google Scholar] [CrossRef]
- Eskin, M.; Köskün, T.; Harlak, H. Beliefs about suicide prevention by excluding the phenomenon versus the person: The role of cultural orientation, attitudes towards suicide, and social reactions to suicidal persons in Turkish university students. Scand. J. Psychol. 2022, 63, 83–90. [Google Scholar] [CrossRef]
- Coskun, M.; Zoroglu, S.; Ghaziuddin, N. Suicide rates among Turkish and American youth: A cross-cultural comparison. Arch. Suicide Res. 2012, 16, 59–72. [Google Scholar] [CrossRef]
- Sher, L. Suicide in men: An underappreciated public health challenge. Eur. Arch. Psychiatry Clin. Neurosci. 2020, 270, 277–278. [Google Scholar] [CrossRef]
- Möller-Leimkühler, A.M. The gender gap in suicide and premature death or: Why are men so vulnerable? Eur. Arch. Psychiatry Clin. Neurosci. 2003, 253, 1–8. [Google Scholar] [CrossRef]
- Värnik, P. Suicide in the world. Int. J. Environ. Res. Public Health 2012, 9, 760–771. [Google Scholar] [CrossRef] [PubMed]
- Angst, J.; Hengartner, M.P.; Rogers, J.; Schnyder, U.; Steinhausen, H.C.; Ajdacic-Gross, V.; Rössler, W. Suicidality in the prospective Zurich study: Prevalence, risk factors and gender. Eur. Arch. Psychiatry Clin. Neurosci. 2014, 264, 557–565. [Google Scholar] [CrossRef]
- Singer, M.; Bulled, N.; Ostrach, B.; Mendenhall, E. Syndemics and the biosocial conception of health. Lancet 2017, 389, 941–950. [Google Scholar] [CrossRef]
- Scheer, J.R.; Helminen, E.C.; Felver, J.C.; Coolhart, D. Nonmedical social determinants, syndemic conditions, and suicidal thoughts and behaviors in a treatment-seeking community sample: A latent class analysis. Arch. Suicide Res. 2023, 27, 1063–1082. [Google Scholar] [CrossRef]
- Edirne, T.; Can, M.; Kolusari, A.; Yildizhan, R.; Adali, E.; Akdag, B. Trends, characteristics, and outcomes of adolescent pregnancy in eastern Turkey. Int. J. Gynaecol. Obstet. 2010, 110, 105–108. [Google Scholar] [CrossRef]
- Freitas, G.V.S.; Cais, C.F.S.; Stefanello, S.; Botega, N.J. Psychosocial conditions and suicidal behavior in pregnant teenagers. Eur. Child Adolesc. Psychiatry 2008, 17, 336–342. [Google Scholar] [CrossRef]
- Van Bergen, D.; Eylem-Van Bergeijk, O.; Montesinos, A.H. Attempted suicide and suicide of young Turkish women in Europe and Turkey: A systematic literature review of characteristics and precipitating factors. PLoS ONE 2021, 16, e0253274. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Health Estimates 2021: Disease Burden by Cause, Age, Sex, by Country and by Region, 2000–2021; World Health Organization: Geneva, Switzerland, 2024. [Google Scholar]
- Godinić, D.; Obrenovic, B. Effects of economic uncertainty on mental health in the COVID-19 pandemic context: Social identity disturbance, job uncertainty and psychological well-being model. Int. J. Innov. Econ. Dev. 2020, 6, 61–74. [Google Scholar] [CrossRef]
- Turkmen, L.; Tekedere, H. SARS-CoV-2 pandemic and beyond: The impact of the SARS-CoV-2 pandemic on Turkish youth and their attitude toward future prospects. J. Infect. Dev. Ctries. 2023, 17, 911–921. [Google Scholar] [CrossRef] [PubMed]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Koda, M.; Harada, N.; Eguchi, A.; Nomura, S.; Ishida, Y. Reasons for suicide during the COVID-19 pandemic in Japan. JAMA Netw. Open 2022, 5, e2145870. [Google Scholar] [CrossRef]
- Khan, A.R.; Ratele, K.; Arendse, N. Men, suicide, and COVID-19: Critical masculinity analyses and interventions. Postdigit. Sci. Educ. 2020, 2, 651–656. [Google Scholar] [CrossRef] [PubMed]
- Grande, E.; Grippo, F.; Marchetti, S.; Frova, L. Suicide in Italy during the COVID-19 pandemic: Excess mortality in 2021 among men and adolescent girls. J. Psychiatr. Res. 2025, 181, 282–285. [Google Scholar] [CrossRef]
- Ogrodniczuk, J.S.; Rice, S.M.; Kealy, D.; Seidler, Z.E.; Delara, M.; Oliffe, J.L. Psychosocial impact of the COVID-19 pandemic: A cross-sectional study of online help-seeking Canadian men. Postgrad. Med. 2021, 133, 750–759. [Google Scholar] [CrossRef]
- Cerel, J.; Brown, M.M.; Maple, M.; Singleton, M.; van de Venne, J.; Moore, M.; Flaherty, C. How many people are exposed to suicide? Not six. Suicide Life-Threat. Behav. 2019, 49, 529–534. [Google Scholar] [CrossRef]


| Year | Male | Female | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Number | Crude Rate | Std. Rate * | Number | Crude Rate | Std. Rate * | Number | Crude Rate | Std. Rate * | |
| 2012 | 2341 | 6.17 | 6.19 | 907 | 2.41 | 2.38 | 3248 | 4.29 | 4.25 |
| 2013 | 2359 | 6.13 | 6.12 | 866 | 2.27 | 2.23 | 3225 | 4.21 | 4.14 |
| 2014 | 2325 | 5.96 | 5.91 | 811 | 2.09 | 2.07 | 3136 | 4.04 | 3.96 |
| 2015 | 2353 | 5.96 | 5.88 | 882 | 2.25 | 2.20 | 3235 | 4.11 | 4.02 |
| 2016 | 2424 | 6.05 | 5.96 | 767 | 1.93 | 1.90 | 3191 | 4.00 | 3.90 |
| 2017 | 2445 | 6.03 | 5.90 | 723 | 1.80 | 1.76 | 3168 | 3.92 | 3.81 |
| 2018 | 2529 | 6.15 | 6.00 | 813 | 1.99 | 1.96 | 3342 | 4.08 | 3.95 |
| 2019 | 2684 | 6.43 | 6.25 | 792 | 1.91 | 1.88 | 3476 | 4.18 | 4.05 |
| 2020 | 2845 | 6.79 | 6.58 | 865 | 2.07 | 2.01 | 3710 | 4.44 | 4.27 |
| 2021 | 3263 | 7.69 | 7.42 | 931 | 2.20 | 2.06 | 4194 | 4.95 | 4.77 |
| 2022 | 3111 | 7.29 | 7.05 | 1035 | 2.43 | 2.41 | 4146 | 4.86 | 4.72 |
| 2023 | 3062 | 7.17 | 6.92 | 999 | 2.34 | 2.32 | 4061 | 4.76 | 4.61 |
| Total | 31,741 | 6.50 | 6.19 | 10,391 | 2.14 | 2.38 | 42,132 | 4.32 | 4.20 |
| Suicide Rate | |||||||||
| Male | Female | Combined | |||||||
| Period | APC | p | Period | APC | p | Period | APC | p | |
| 2012–2018 | −0.3 (−1.4 to 0.5) | 0.458 | 2012–2017 | −5.3 * (−9.5 to −2.7) | 0.010 | 2012–2017 | −1.6 (−4.3 to 1.3) | 0.267 | |
| 2018–2021 | 7.8 * (5.9 to 9.3) | 0.011 | 2017–2023 | 4.5 * (2.5 to 7.9) | 0.0014 | 2017–2023 | 4.0 * (2.0–6.2) | 0.001 | |
| 2021–2023 | −2.6 * (−5.0 to −0.3) | 0.012 | |||||||
| AAPC | 1.4 * (1.0 to 1.8) | 0.0 (−1.0 to 0.9) | 1.5 (−0.1 to 3.1) | ||||||
| YLL Rate | |||||||||
| Male | Female | Combined | |||||||
| Period | APC | p | Period | APC | p | Period | APC | p | |
| 2012–2019 | −5.2 * (−7.5 to −2.9) | 0.001 | 2012–2018 | −1.3 (−3.8 to 1.4) | 0.300 | 2012–2018 | −2.9 * (−5.6 to −0.1) | 0.040 | |
| 2019–2023 | 8.2 * (2.2 to 14.6) | 0.014 | 2018–2023 | 5.8 * (2.5 to 9.3) | 0.004 | 2018–2023 | 5.8 * (2.1 to 9.6) | 0.003 | |
| AAPC | −0.5 (−2.7 to 1.6) | 1.9 * (0.2 to 3.7) | 0.9 (−1.1 to 3.0) | ||||||
| Age Group | Male | Female | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| YPLL | YPLL per 100,000 Population | Distribution of Percentage | YPLL | YPLL per 100,000 Population | Distribution of Percentage | YPLL | YPLL per 100,000 Population | Distribution of Percentage | |
| 15–24 | 281,880.6 | 356.09 | 36.60 | 142,293.1 | 188.74 | 52.69 | 424,173.7 | 274.45 | 40.77 |
| 25–49 | 443,358.4 | 243.02 | 57.56 | 116,611.27 | 65.34 | 43.18 | 559,969.6 | 155.15 | 53.83 |
| 50–64 | 45,014.9 | 62.29 | 5.84 | 11,167.13 | 15.32 | 4.13 | 56,182.1 | 38.70 | 5.40 |
| Total | 770,253.9 | 230.71 | 100.00 | 270,071.5 | 82.65 | 100.00 | 1,040,325.4 | 157.47 | 100.00 |
| Male | Female | Total | |
|---|---|---|---|
| Total premature mortality cost (USD) (12 years period) | 8,836,721,182 | 1,939,222,015 | 10,775,943,197 |
| Total premature mortality cost (USD)/annual | 736,393,432 | 161,601,835 | 897,995,266 |
| Premature mortality cost per death (USD) | 278,400.84 | 186,625.16 | 255,766.24 |
| Premature mortality cost per YLL (USD) | 8292.23 | 3910.36 | 6900.66 |
| Premature mortality cost per YPLL (USD) | 11,472.48 | 7180.40 | 10,358.24 |
| Gender | YLL Annual Average Value (Year) | % Change | YPLL Annual Average Value (Year) | % Change | Cost Annual Average Value (USD) | % Change | |
|---|---|---|---|---|---|---|---|
| Segment | Male | ||||||
| 1 | 2012–2018 | 80,889.40 | 57,160.01 | 653,758,685.3 | |||
| 2 | 2018–2021 | 99,887.35 | 1–2 +23.49% | 72,662.14 | 1–2 +22.36% | 852,082,077.6 | 1–2 +25.56% |
| 3 | 2021–2023 * | - | - | - | |||
| Segment | Female | ||||||
| 1 | 2012–2017 | 41,014.29 | 21,633.46 | 150,358,046.50 | |||
| 2 | 2017–2023 | 41,763.76 | 1–2 +1.83% | 23,727.46 | 1–2 +9.68% | 177,343,137.90 | 1–2 +17.95% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akbulut Zencirci, S.; Atay, E.; Önsüz, M.F.; Metintaş, S. Lost Futures: The Human and Economic Cost of Suicide in Türkiye, 2012–2023. Healthcare 2025, 13, 2841. https://doi.org/10.3390/healthcare13222841
Akbulut Zencirci S, Atay E, Önsüz MF, Metintaş S. Lost Futures: The Human and Economic Cost of Suicide in Türkiye, 2012–2023. Healthcare. 2025; 13(22):2841. https://doi.org/10.3390/healthcare13222841
Chicago/Turabian StyleAkbulut Zencirci, Sevil, Emrah Atay, Muhammed Fatih Önsüz, and Selma Metintaş. 2025. "Lost Futures: The Human and Economic Cost of Suicide in Türkiye, 2012–2023" Healthcare 13, no. 22: 2841. https://doi.org/10.3390/healthcare13222841
APA StyleAkbulut Zencirci, S., Atay, E., Önsüz, M. F., & Metintaş, S. (2025). Lost Futures: The Human and Economic Cost of Suicide in Türkiye, 2012–2023. Healthcare, 13(22), 2841. https://doi.org/10.3390/healthcare13222841






