Analyzing Global Research Trends on Medical Resident Burnout and Physical Activity: A Bibliometric Analysis (2005–2025)
Abstract
1. Introduction
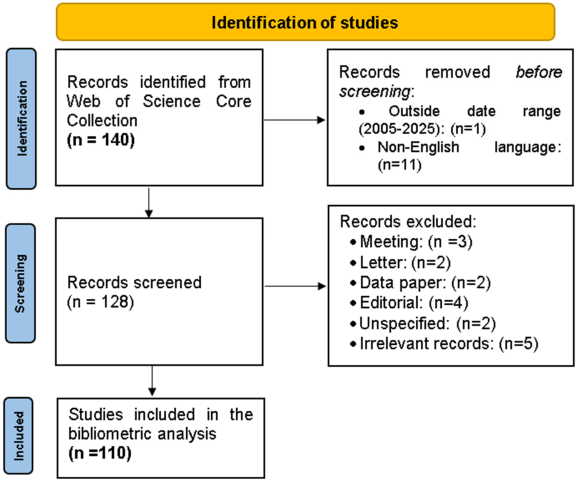
2. Materials and Methods
2.1. Study Design
2.2. Data Source and Search Strategy
2.3. Inclusion and Exclusion Criteria
2.4. Data Extraction and Processing
2.5. Analytical Approach
3. Results
3.1. Bibliometric Overview
3.2. Performance Analysis
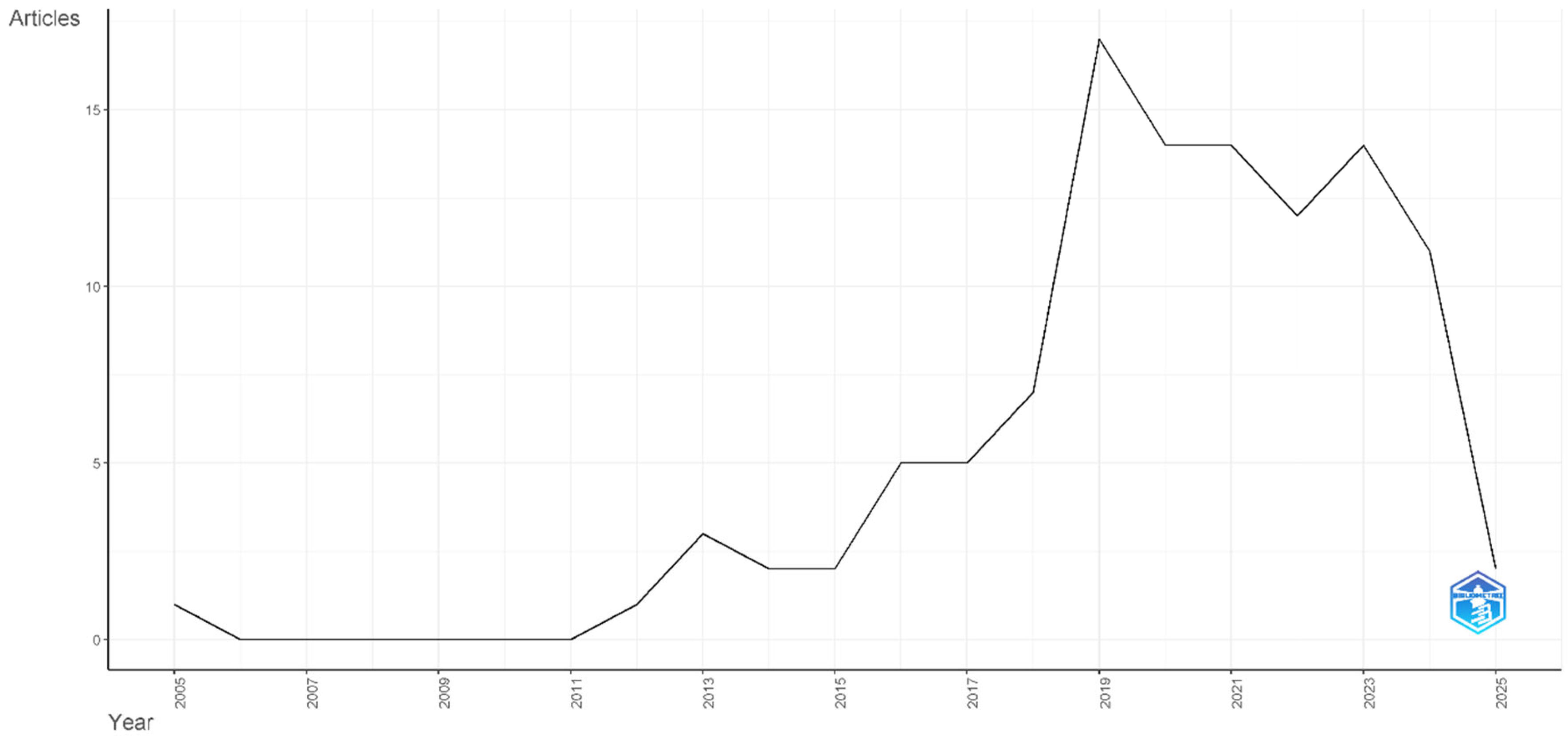
Annual Scientific Production
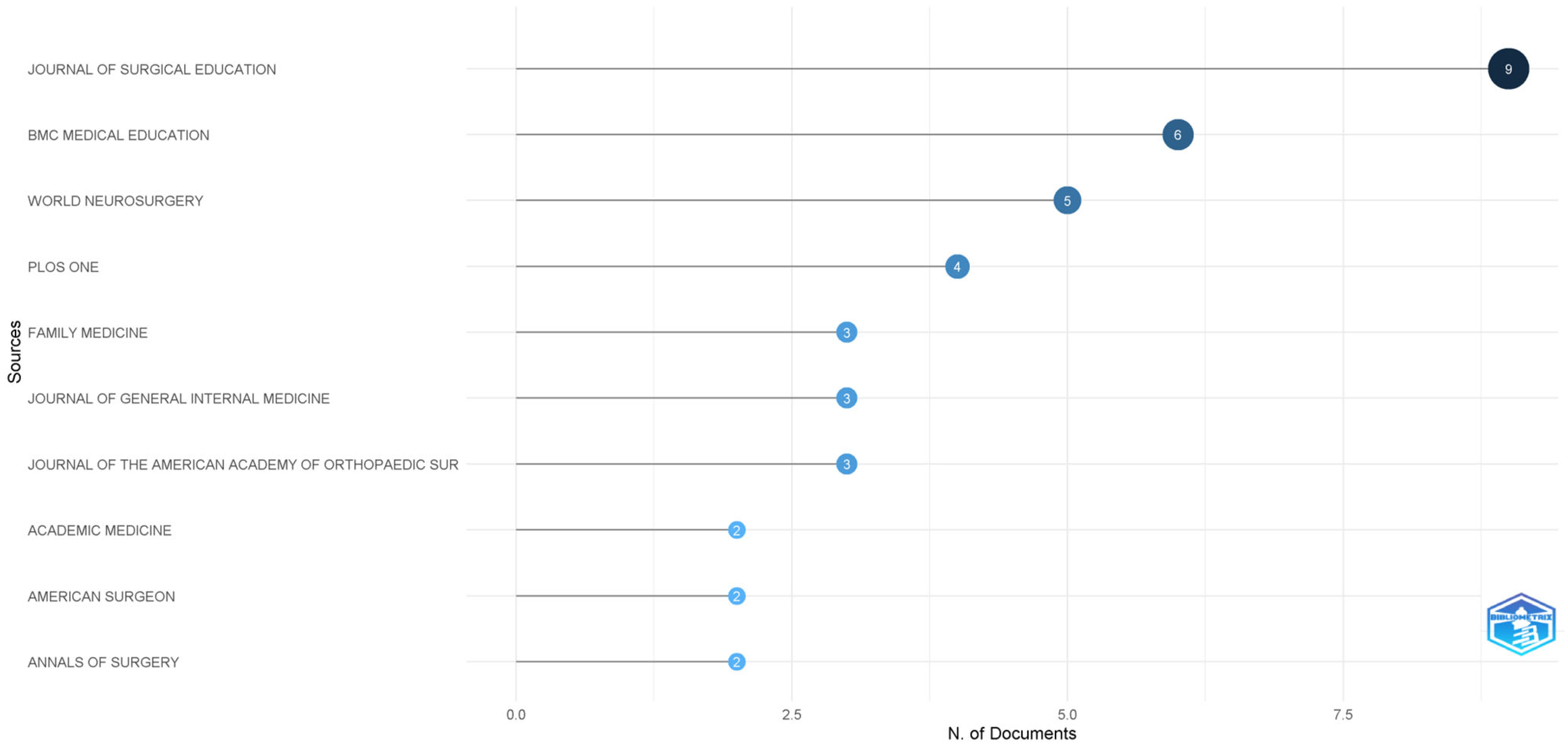
3.3. Most Productive Journals
3.4. Author Productivity and Impact
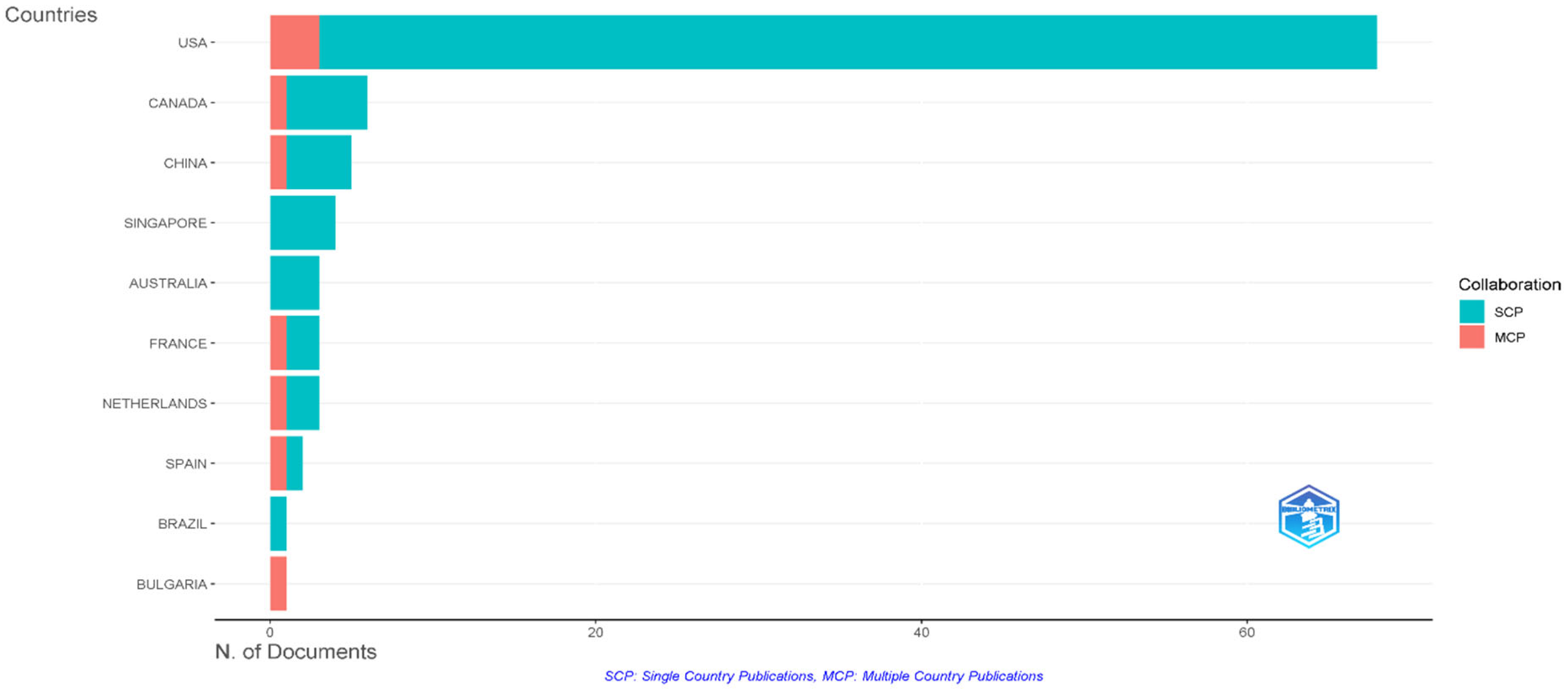
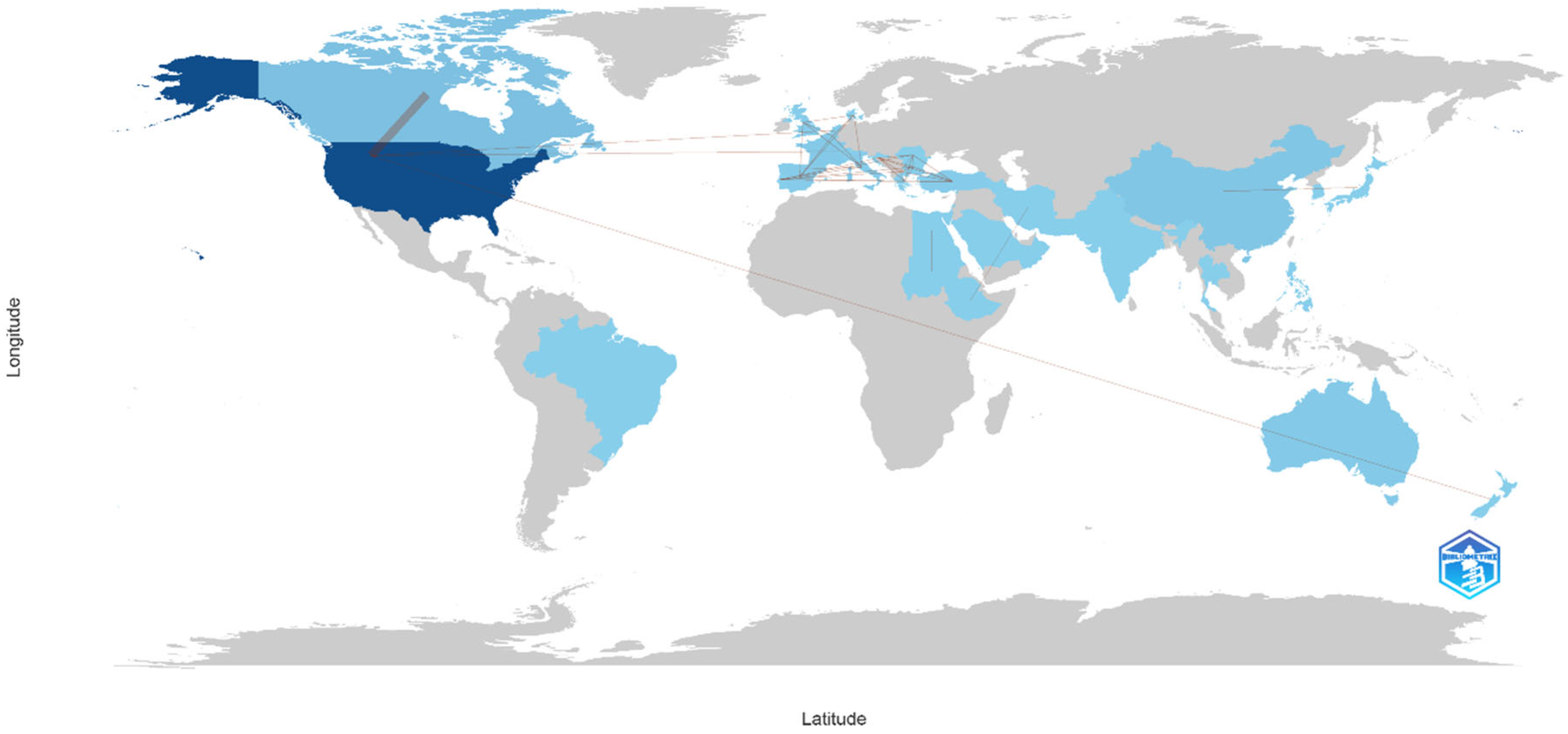
3.5. Geographic Distribution and International Collaboration
3.6. Institutional Contributions
3.7. Scientific Mapping
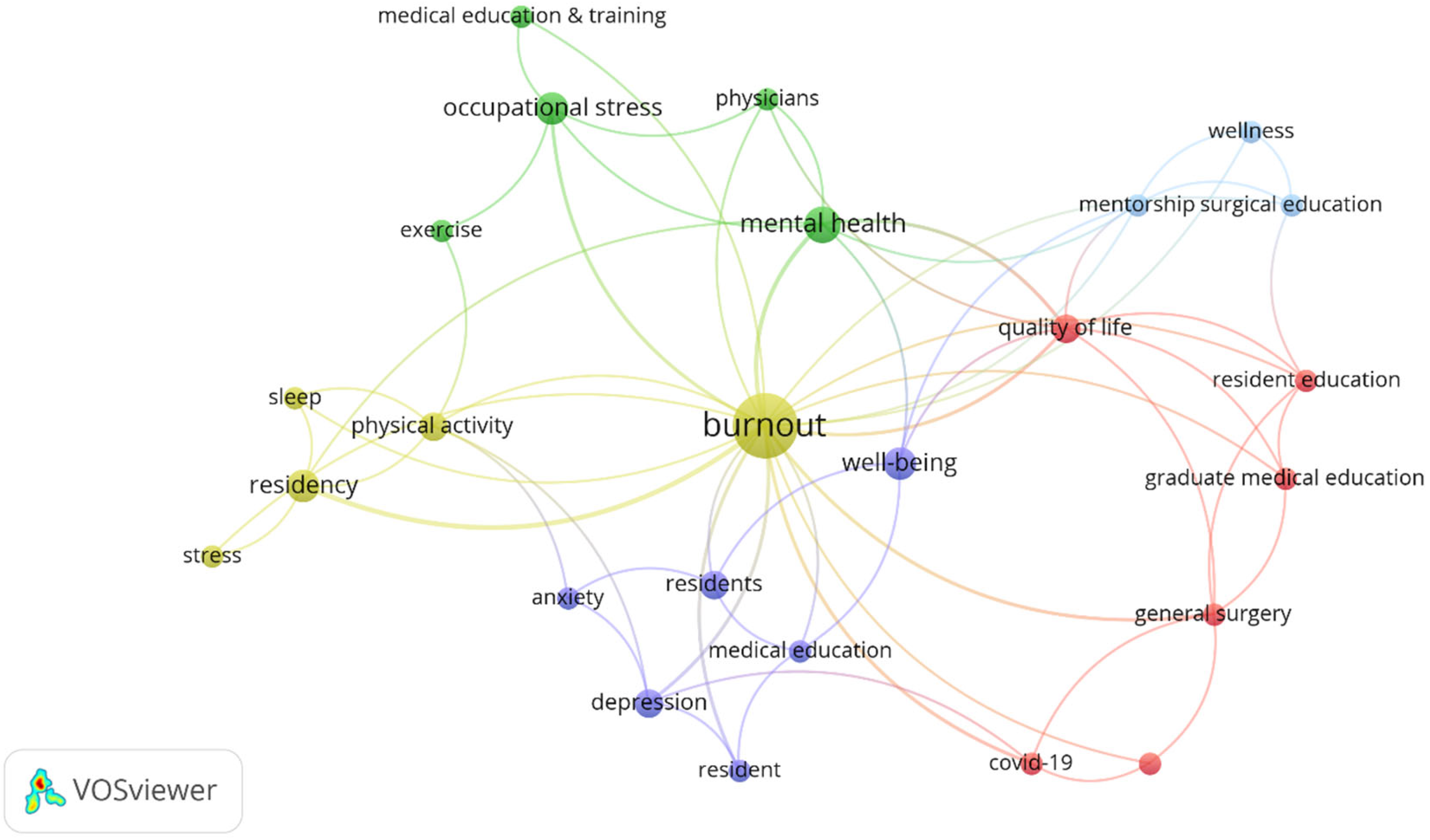
Keyword Co-Occurrence Analysis
3.8. Author Co-Citation Analysis
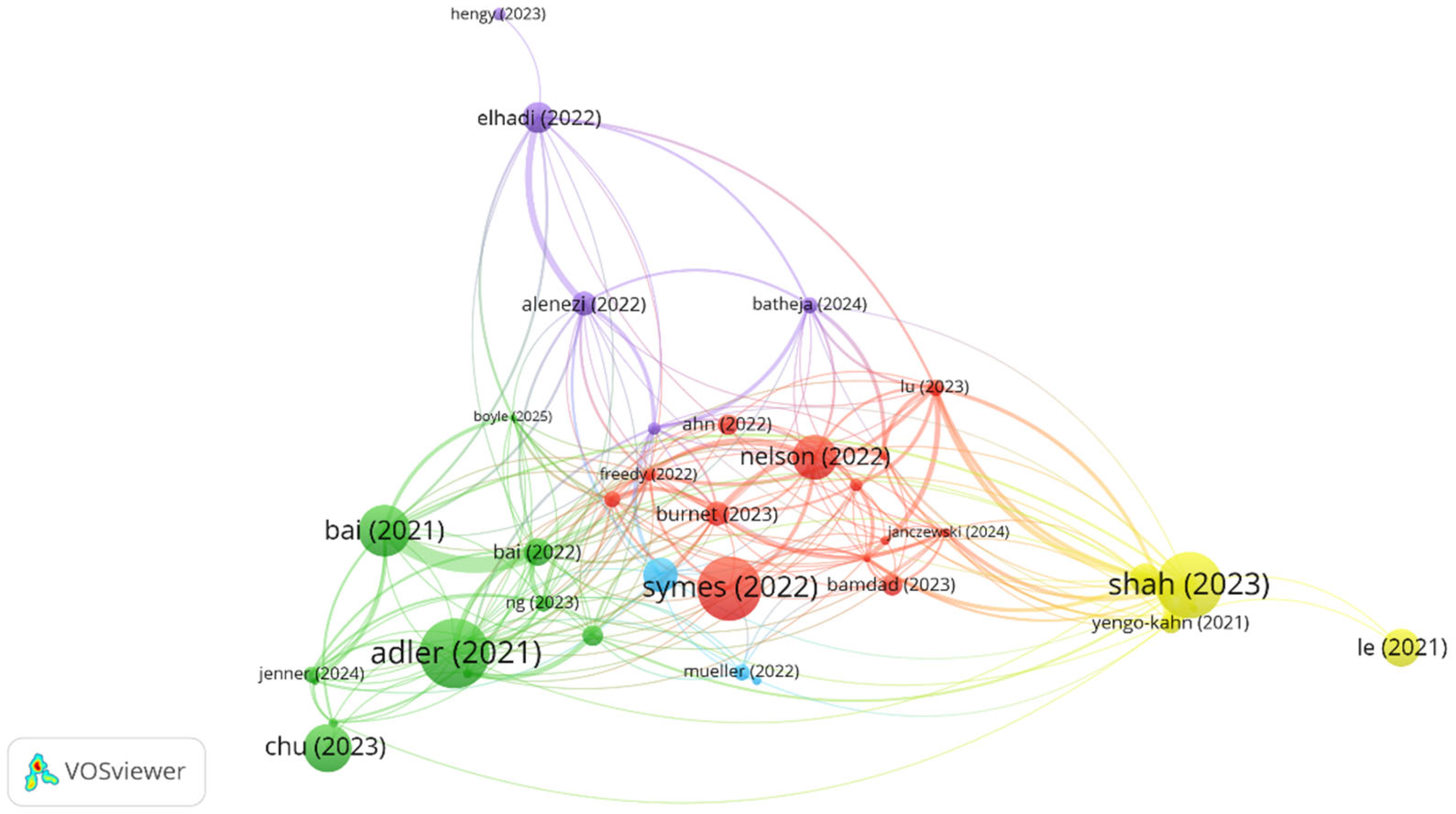
3.9. Bibliographic Coupling Analysis
4. Discussion
4.1. Global Research Trends and Knowledge Gaps
4.2. Policy and Medical Education Implications
4.3. Future Research Recommendations
4.3.1. Thematic Evolution and Research Priorities
4.3.2. Physical Activity as an Intervention Strategy
4.3.3. Institutional and Policy Implications
4.3.4. Future Research Directions and Innovation Opportunities
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Almutairi, H.; Alsubaiei, A.; Abduljawad, S.; Alshatti, A.; Fekih-Romdhane, F.; Husni, M.; Jahrami, H. Prevalence of Burnout in Medical Students: A Systematic Review and Meta-Analysis. Int. J. Soc. Psychiatry 2022, 68, 1157–1170. [Google Scholar] [CrossRef]
- Ashkar, K.; Romani, M.; Musharrafieh, U.; Chaaya, M. Prevalence of Burnout Syndrome among Medical Residents: Experience of a Developing Country. Postgrad. Med. J. 2010, 86, 266–271. [Google Scholar] [CrossRef]
- Dimitriu, M.C.T.; Pantea-Stoian, A.; Smaranda, A.C.; Nica, A.A.; Carap, A.C.; Constantin, V.D.; Davitoiu, A.M.; Cirstoveanu, C.; Bacalbasa, N.; Bratu, O.G.; et al. Burnout Syndrome in Romanian Medical Residents in Time of the COVID-19 Pandemic. Med. Hypotheses 2020, 144, 109972. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E. The Measurement of Experienced Burnout. J. Organ. Behav. 1981, 2, 99–113. [Google Scholar] [CrossRef]
- De Mélo Silva Júnior, M.L.; Valença, M.M.; Rocha-Filho, P.A.S. Individual and Residency Program Factors Related to Depression, Anxiety and Burnout in Physician Residents—A Brazilian Survey. BMC Psychiatry 2022, 22, 272. [Google Scholar] [CrossRef] [PubMed]
- Gopal, R.; Glasheen, J.J.; Miyoshi, T.J.; Prochazka, A.V. Burnout and Internal Medicine Resident Work-Hour Restrictions. Arch. Intern. Med. 2005, 165, 2595. [Google Scholar] [CrossRef] [PubMed]
- Maryam, M.; Saber, M.; MirSaeed, A. Occupational stress and influencing factors, in medical residents of one of the educational hospitals of Tehran University of Medical Sciences. Razi J. Med. Sci. 2011, 18, 24–35. [Google Scholar]
- Bakker, A.B.; Demerouti, E. The Job Demands-Resources Model: State of the Art. J. Manag. Psychol. 2007, 22, 309–328. [Google Scholar] [CrossRef]
- Hewitt, D.B.; Ellis, R.J.; Chung, J.W.; Cheung, E.O.; Moskowitz, J.T.; Huang, R.; Merkow, R.P.; Yang, A.D.; Hu, Y.-Y.; Cohen, M.E.; et al. Association of Surgical Resident Wellness With Medical Errors and Patient Outcomes. Ann. Surg. 2021, 274, 396–402. [Google Scholar] [CrossRef]
- Li, C.J.; Shah, Y.B.; Harness, E.D.; Goldberg, Z.N.; Nash, D.B. Physician Burnout and Medical Errors: Exploring the Relationship, Cost, and Solutions. Am. J. Med. Qual. 2023, 38, 196–202. [Google Scholar] [CrossRef]
- Saadat, S.; Nikpour, H.; Imannezhad, S.; Jafari, M. Burnout in Medical Residents: A Systematic Review of Literature. Med. Educ. Bull. 2024, 5, 907–920. [Google Scholar] [CrossRef]
- Wan, Z.; Tang, J.; Bai, X.; Cao, Y.; Zhang, D.; Su, T.; Zhou, Y.; Qiao, L.; Shen, K.; Wang, L.; et al. Burnout among Radiology Residents: A Systematic Review and Meta-Analysis. Eur. Radiol. 2023, 34, 1399–1407. [Google Scholar] [CrossRef]
- Alzahrani, A.; Althobaiti, N.; Althobaiti, A.; Althobaiti, L.; Alzhrani, L.; Althobaiti, G.; Alsufyani, N. The Prevalence of Burnout among Medical Students at Taif University, Saudi Arabia. Int. J. Med. Dev. Ctries. 2024, 8, 1736–1742. [Google Scholar] [CrossRef]
- Chahal, K.; Matwala, K. A Systematic Review of the Prevalence of Burnout in Orthopaedic Surgeons. Ann. R. Coll. Surg. Engl. 2025, 107, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Dyrbye, L.; Shanafelt, T. A Narrative Review on Burnout Experienced by Medical Students and Residents. Med. Educ. 2016, 50, 132–149. [Google Scholar] [CrossRef] [PubMed]
- Muteshi, C.; Ochola, E.; Kamya, D. Burnout among Medical Residents, Coping Mechanisms and the Perceived Impact on Patient Care in a Low/Middle Income Country. BMC Med. Educ. 2024, 24, 828. [Google Scholar] [CrossRef]
- Somerson, J.S.; Patton, A.; Ahmed, A.A.; Ramey, S.; Holliday, E.B. Burnout Among United States Orthopaedic Surgery Residents. J. Surg. Educ. 2020, 77, 961–968. [Google Scholar] [CrossRef]
- Barreto, T.M.; Tavares, M.R.; Azi, M.L.; Azi, L.M.T.A.; Sadgursky, D.; Alencar, D. Impacto da pandemia COVID-19 na prevalência de burnout entre residentes em ortopedia. Rev. Bras. Ortop. (Sao Paulo) 2022, 57, 159–166. [Google Scholar] [CrossRef]
- Gisselbaek, M.; Suppan, M.; Saxena, S.; Hudelson, P.; Savoldelli, G.L. Association of Impostor Phenomenon and Burnout among Swiss Residents and Junior Anaesthesiologists: Results of a Cross-Sectional Survey. BMC Anesth. 2025, 25, 98. [Google Scholar] [CrossRef]
- Yuan, J.H.; Huang, Y.; Rosgen, B.K.; Donnelly, S.; Lan, X.; Katz, S.J. Burnout and Fatigue amongst Internal Medicine Residents: A Cross-Sectional Study on the Impact of Alternative Scheduling Models on Resident Wellness. PLoS ONE 2023, 18, e0291457. [Google Scholar] [CrossRef]
- Balatoni, I.; Szépné, H.V.; Kiss, T.; Adamu, U.G.; Szulc, A.M.; Csernoch, L. The Importance of Physical Activity in Preventing Fatigue and Burnout in Healthcare Workers. Healthcare 2023, 11, 1915. [Google Scholar] [CrossRef]
- Appelqvist-Schmidlechner, K.; Heikkinen, R.; Vasankari, T.; Virtanen, T.; Pihlainen, K.; Honkanen, T.; Kyröläinen, H.; Vaara, J.P. Relationships between Psychosocial Well-Being and Leisure Time Physical Activity among 160.000 Young Finnish Men: A Cross-Sectional Study during 2015–2021. Arch. Public Health 2023, 81, 26. [Google Scholar] [CrossRef] [PubMed]
- Morgan, T.; McFadden, T.; Fortier, M.; Sweet, S.; Tomasone, J. Do Physical Activity Intensity and Sedentary Behaviour Relate to Burnout among Medical Students? Insight from Two Canadian Medical Schools. Can. Med. Ed. J. 2024, 15, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Olson, S.M.; Odo, N.U.; Duran, A.M.; Pereira, A.G.; Mandel, J.H. Burnout and Physical Activity in Minnesota Internal Medicine Resident Physicians. J. Grad. Med. Educ. 2014, 6, 669–674. [Google Scholar] [CrossRef] [PubMed]
- Donthu, N.; Kumar, S.; Mukherjee, D.; Pandey, N.; Lim, W.M. How to conduct a bibliometric analysis: An overview and guidelines. J. Bus. Res. 2021, 133, 285–296. [Google Scholar] [CrossRef]
- Cheek, J.; Garnham, B.; Quan, J. What’s in a number? Issues in providing evidence of impact and quality of research(ers). Qual Health Res. 2006, 16, 423–435. [Google Scholar] [CrossRef]
- Salinas-Ríos, K.; García López, A.é.J. Bibliometrics, a useful tool within the field of research. J. Basic Appl. Psychol. Res. 2022, 3, 9–16. [Google Scholar] [CrossRef]
- Chaabeni, A.; Slama, M.M.; Kalai, A.; Ben Saad, H.; López-Valenciano, A.; Ben Salah Frih, Z.; Jellad, A. A Bibliometric Analysis of the 100 Most-Cited Articles on Soccer Injuries. Cureus 2025, 17, e82636. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Symes, H.A.; Boulet, J.; Yaghmour, N.A.; Wallowicz, T.; McKinley, D.W. International Medical Graduate Resident Wellness: Examining Qualitative Data From J-1 Visa Physician Recipients. Acad. Med. J. Assoc. Am. Med. Coll. 2022, 97, 420–425. [Google Scholar] [CrossRef]
- Nelson, V.; Dubov, A.; Morton, K.; Fraenkel, L. Using nominal group technique among resident physicians to identify key attributes of a burnout prevention program. PLoS ONE 2022, 17, e0264921. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Burnet, G.; Platnick, C.; Krishnan, P.; Robinson, C.K.; Sauaia, A.; Burlew, C.C.; Nehler, M.R.; Jaiswal, K.; Platnick, K.B. Muffins and Meditation: Combatting Burnout in Surgical Residents. J. Surg. Educ. 2023, 80, 185–193. [Google Scholar] [CrossRef]
- Adler, D.A.; Tseng, V.W.-S.; Qi, G.; Scarpa, J.; Sen, S.; Choudhury, T. Identifying Mobile Sensing Indicators of Stress-Resilience. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2021, 5, 51. [Google Scholar] [CrossRef]
- Bai, S.; Chang, Q.; Yao, D.; Zhang, Y.; Wu, B.; Zhao, Y. Anxiety in Residents in China: Prevalence and Risk Factors in a Multicenter Study. Acad. Med. J. Assoc. Am. Med. Coll. 2021, 96, 718–727. [Google Scholar] [CrossRef] [PubMed]
- Chu, W.M.; Ho, H.E.; Lin, Y.L.; Li, J.Y.; Lin, C.F.; Chen, C.H.; Shieh, G.J.; Chan, W.C.; Tsan, Y.T. Risk Factors Surrounding an Increase in Burnout and Depression Among Health Care Professionals in Taiwan During the COVID-19 Pandemic. J. Am. Med. Dir. Assoc. 2023, 24, 164–170.e3. [Google Scholar] [CrossRef] [PubMed]
- Shah, H.P.; Salehi, P.P.; Ihnat, J.; Kim, D.D.; Salehi, P.; Judson, B.L.; Azizzadeh, B.; Lee, Y.H. Resident Burnout and Well-being in Otolaryngology and Other Surgical Specialties: Strategies for Change. Otolaryngol.--Head Neck Surg. Off. J. Am. Acad. Otolaryngol.-Head Neck Surg. 2023, 168, 165–179. [Google Scholar] [CrossRef] [PubMed]
- Elhadi, Y.A.M.; Ahmed, A.; Salih, E.B.; Abdelhamed, O.S.; Ahmed, M.H.H.; El Dabbah, N.A. A cross-sectional survey of burnout in a sample of resident physicians in Sudan. PLoS ONE 2022, 17, e0265098. [Google Scholar] [CrossRef]
- Karim Alenezi, N.; Hamad Alyami, A.; Omar Alrehaili, B.; Adnan Arruhaily, A.; Kareem Alenazi, N.; Abdo Radman Al-Dubai, S. Prevalence and Associated Factors of Burnout Among Saudi Resident Doctors: A Multicenter Cross-Sectional Study. Alpha Psychiatry 2022, 23, 173–183. [Google Scholar] [CrossRef]
- Maghbouli, N.; Fatehi, F.; Mafinejad, M.K.; Pourhassan, S.; Sohrabpour, A.A.; Ali, J.H. Épuisement professionnel et environnement d’apprentissage clinique chez les résidents à Téhéran: Étude transversale. Heliyon 2021, 7, e07238. [Google Scholar] [CrossRef]
- Obeng Nkrumah, S.; Adu, M.K.; Agyapong, B.; Da Luz Dias, R.; Agyapong, V.I.O. Prevalence and Correlates of Depression, Anxiety, and Burnout Among Physicians and Postgraduate Medical Trainees: A Scoping Review of Recent Literature. Front. Public Health 2025, 13, 1537108. [Google Scholar] [CrossRef]
- Schneider, R.H.; Travis, F.; Nader, T. Addressing Clinician Burnout: A Unifying Systems Medicine Model with Meditation as a Heart-Mind Intervention. Heart Mind 2024, 8, 5–11. [Google Scholar] [CrossRef]
- Wright, T.; Mughal, F.; Babatunde, O.; Dikomitis, L.; Mallen, C.; Helliwell, T. Burnout among Primary Health-Care Professionals in Low- and Middle-Income Countries: Systematic Review and Meta-Analysis. Bull. World Health Organ. 2022, 100, 385A–401A. [Google Scholar] [CrossRef]
- Hiver, C.; Villa, A.; Bellagamba, G.; Lehucher-Michel, M.-P. Burnout Prevalence among European Physicians: A Systematic Review and Meta-Analysis. Int. Arch. Occup. Environ. Health 2022, 95, 259–273. [Google Scholar] [CrossRef] [PubMed]
- Naji, L.; Singh, B.; Shah, A.; Naji, F.; Dennis, B.; Kavanagh, O.; Banfield, L.; Alyass, A.; Razak, F.; Samaan, Z.; et al. Global Prevalence of Burnout among Postgraduate Medical Trainees: A Systematic Review and Meta-Regression. CMAJ Open 2021, 9, E189–E200. [Google Scholar] [CrossRef] [PubMed]
- Musa, S.; Dergaa, I.; Bachiller, V.; Saad, H.B. Global Implications of COVID-19 Pandemic on Adults’ Lifestyle Behavior: The Invisible Pandemic of Noncommunicable Disease. Int. J. Prev. Med. 2023, 14, 15. [Google Scholar] [CrossRef] [PubMed]
- Akbari, H.A.; Pourabbas, M.; Yoosefi, M.; Briki, W.; Attaran, S.; Mansoor, H.; Moalla, W.; Damak, M.; Dergaa, I.; Teixeira, A.L.; et al. How Physical Activity Behavior Affected Well-Being, Anxiety and Sleep Quality during COVID-19 Restrictions in Iran. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 7847–7857. [Google Scholar] [CrossRef]
- Taheri, M.; Saad, H.B.; Washif, J.A.; Reynoso-Sánchez, L.F.; Mirmoezzi, M.; Youzbashi, L.; Trabelsi, K.; Moshtagh, M.; Muñoz-Helú, H.; Mataruna-Dos-Santos, L.J.; et al. Comparative Study of the Long-Term Impact of the COVID-19 Pandemic on Mental Health and Nutritional Practices Among International Elite and Sub-Elite Athletes: A Sample of 1420 Participants from 14 Countries. Sports Med-Open 2023, 9, 104. [Google Scholar] [CrossRef]
- Taylor, C.E.; Scott, E.J.; Owen, K. Physical Activity, Burnout and Quality of Life in Medical Students: A Systematic Review. Clin. Teach. 2022, 19, e13525. [Google Scholar] [CrossRef]
- Dziadkowiec, O.; Durbin, J.S.; Novak, M.L.; Patt-Rappaport, Z.; Guldner, G. A Two-Year Longitudinal, Cross-Sectional Evaluation of Resident Physician Burnout: An Exploration of the Effects of Stress, Satisfaction, Exercise and EMR. HCA Healthc. J. Med. 2021, 2, 8. [Google Scholar] [CrossRef]
- Ahmad, R.G.; Gadah, Y.S.; Yamani, R.A.; Almaimani, B.H.; Alganas, B.M.; Alsaleh, A.; Ahmed, M.E. The Relationship between Physical Activity and Burnout among Respiratory Therapists in Jeddah City, Saudi Arabia. Can. J. Respir. Ther. 2022, 58, 204–208. [Google Scholar] [CrossRef]
- Zhu, L.; Hou, J.; Zhou, B.; Xiao, X.; Wang, J.; Jia, W. Physical Activity, Problematic Smartphone Use, and Burnout among Chinese College Students. PeerJ 2023, 11, e16270. [Google Scholar] [CrossRef]
- Leridis, I.; Matsouka, O.; Bebetsos, E.; Kosta, G. The Effect of Physical Activity on Burnout Syndrome in Emergency Room Nurses Working in Public Hospitals. Sport. Mont. 2023, 21, 49–54. [Google Scholar] [CrossRef]
- Naczenski, L.M.; De Vries, J.D.; Van Hooff, M.L.M.; Kompier, M.A.J. Systematic Review of the Association between Physical Activity and Burnout. J. Occup. Health 2017, 59, 477–494. [Google Scholar] [CrossRef]
- Ali, A.; Ranjha, A.N.; Bukhari, S.M.H. Relationship Between Physical Activity and Burnout Among University Faculty in Pakistan. J. Bus. Soc. Rev. Emerg. Econ. 2020, 6, 1–8. [Google Scholar] [CrossRef]
- Low, Z.X.; Yeo, K.A.; Sharma, V.K.; Leung, G.K.; McIntyre, R.S.; Guerrero, A.; Lu, B.; Sin Fai Lam, C.C.; Tran, B.X.; Nguyen, L.H.; et al. Prevalence of Burnout in Medical and Surgical Residents: A Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 1479. [Google Scholar] [CrossRef]
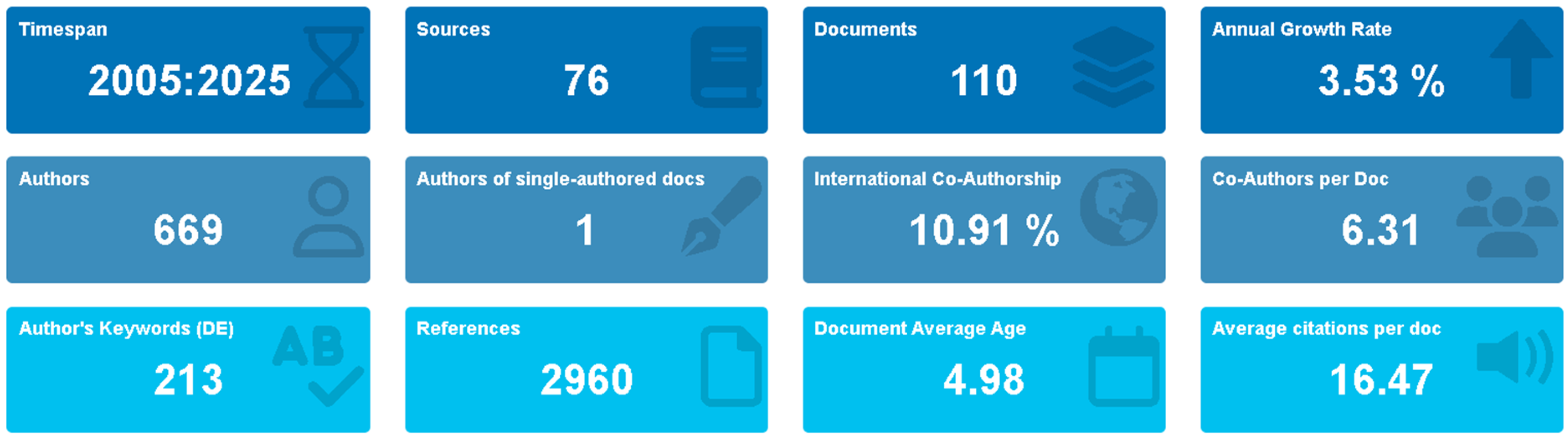


| Category | Metric | Value |
|---|---|---|
| Publication Trends | Total publications analyzed | 110 |
| Temporal scope | 2005–2025 | |
| Annual growth rate | 3.35% | |
| Peak publication year | 2019 (16 articles) | |
| Average citations per document | 16.47 | |
| Geographic Distribution | Leading country | USA (68.0%) |
| Secondary contributors | Canada (5.5%); China (4.5%) | |
| International collaboration | Limited outside high-income countries | |
| Institutional Leadership | Most productive institution | University of Michigan (13 articles) |
| Secondary institutions | Medical University of South Carolina (10); Taichung Veterans General Hospital (9) | |
| Author Productivity | Most prolific researcher | Spiotta, A.M. (5 publications) |
| Most influential researcher | Shanafelt, T.D. (H-index: 107) | |
| Research Focus | Primary thematic clusters | Stress management; occupational health; institutional support |
| Emerging research areas | Digital health interventions; pandemic impacts |
| Authors | Articles | H-Index |
|---|---|---|
| Spiotta, Alejandro M. | 5 | 46.00 |
| Fargen, Kyle M. | 3 | 40.00 |
| Patel, Sunil | 3 | 25.00 |
| Turner IV, Raymond D. | 3 | 41.00 |
| Shanafelt, Tait D. | 2 | 107.00 |
| Srijan Sen | 2 | 37.00 |
| Dyer, George Sinclair Mitchell | 2 | 24.00 |
| Chang, Qing | 2 | 19.00 |
| Morgan, Helen K. | 2 | 16.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Henchiri, H.; Chaabeni, A.; Dergaa, I.; Ceylan, H.İ.; Stefanica, V.; Dhahbi, W.; Harrathi, C.; Abidi, S.; Allihebi, A.H.; Jellad, A.; et al. Analyzing Global Research Trends on Medical Resident Burnout and Physical Activity: A Bibliometric Analysis (2005–2025). Healthcare 2025, 13, 2535. https://doi.org/10.3390/healthcare13192535
Henchiri H, Chaabeni A, Dergaa I, Ceylan Hİ, Stefanica V, Dhahbi W, Harrathi C, Abidi S, Allihebi AH, Jellad A, et al. Analyzing Global Research Trends on Medical Resident Burnout and Physical Activity: A Bibliometric Analysis (2005–2025). Healthcare. 2025; 13(19):2535. https://doi.org/10.3390/healthcare13192535
Chicago/Turabian StyleHenchiri, Hamdi, Amr Chaabeni, Ismail Dergaa, Halil İbrahim Ceylan, Valentina Stefanica, Wissem Dhahbi, Chayma Harrathi, Safa Abidi, Abdullah H. Allihebi, Anis Jellad, and et al. 2025. "Analyzing Global Research Trends on Medical Resident Burnout and Physical Activity: A Bibliometric Analysis (2005–2025)" Healthcare 13, no. 19: 2535. https://doi.org/10.3390/healthcare13192535
APA StyleHenchiri, H., Chaabeni, A., Dergaa, I., Ceylan, H. İ., Stefanica, V., Dhahbi, W., Harrathi, C., Abidi, S., Allihebi, A. H., Jellad, A., & Azaiez, F. (2025). Analyzing Global Research Trends on Medical Resident Burnout and Physical Activity: A Bibliometric Analysis (2005–2025). Healthcare, 13(19), 2535. https://doi.org/10.3390/healthcare13192535












