Wearables in Healthcare Organizations: Implications for Occupational Health, Organizational Performance, and Economic Outcomes
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
- addressed the use of wearable technologies in healthcare settings;
- evaluated outcomes related to occupational health, staff safety, organizational resilience, or business continuity;
- examined barriers, facilitators, or economic implications of implementation.
2.2. Information Sources and Search Strategy
- Wearable technologies (e.g., wearable devices, sensors, smart helmets, exoskeletons, biosensors, wearable monitoring systems);
- Healthcare workers (e.g., healthcare staff, clinical personnel, employees, nurses, physicians, allied health professionals, hospital workers);
- Outcomes and organizational aspects (e.g., occupational health, staff safety, workplace safety, organizational resilience, business continuity, absenteeism, productivity).
- PubMed: ((“wearable devices” [MeSH] OR “wearable” [tiab] OR “sensors” [tiab] OR “biosensors” [MeSH] OR “exoskeleton*” [tiab] OR “smart helmet*” [tiab]) AND (“health personnel” [MeSH] OR “healthcare worker*” [tiab] OR “hospital staff” [tiab] OR “nurse*” [tiab] OR “physician*” [tiab] OR “employee*” [tiab]) AND (“occupational health” [MeSH] OR “staff safety” [tiab] OR “workplace safety” [tiab] OR “organizational resilience” [tiab] OR “business continuity” [tiab] OR “absenteeism” [MeSH] OR “productivity” [MeSH])).
- Scopus: (TITLE-ABS-KEY (“wearable device*” OR “wearable” OR “sensor*” OR “exoskeleton*” OR “smart helmet*” OR “biosensor*”) AND TITLE-ABS-KEY (“healthcare worker*” OR “hospital staff” OR “nurse*” OR “physician*” OR “employee*”) AND TITLE-ABS-KEY (“occupational health” OR “staff safety” OR “workplace safety” OR “organizational resilience” OR “business continuity” OR “absenteeism” OR “productivity”)).
- Web of Science: TS = (“wearable device*” OR “wearable” OR “sensor*” OR “exoskeleton*” OR “smart helmet*” OR “biosensor*”) AND TS = (“healthcare worker*” OR “hospital staff” OR “nurse*” OR “physician*” OR “employee*”) AND TS = (“occupational health” OR “staff safety” OR “workplace safety” OR “organizational resilience” OR “business continuity” OR “absenteeism” OR “productivity”).
- Embase: (‘wearable device’/exp OR ‘wearable’:ti,ab OR ‘sensor’/exp OR ‘sensor*’:ti,ab OR ‘exoskeleton’/exp OR ‘exoskeleton*’:ti,ab OR ‘smart helmet*’:ti,ab OR ‘biosensor’/exp OR ‘biosensor*’:ti,ab) AND (‘health care personnel’/exp OR ‘healthcare worker*’:ti,ab OR ‘hospital staff’:ti,ab OR ‘nurse*’:ti,ab OR ‘physician*’:ti,ab OR ‘employee*’:ti,ab) AND (‘occupational health’/exp OR ‘staff safety’:ti,ab OR ‘workplace safety’:ti,ab OR ‘organizational resilience’:ti,ab OR ‘business continuity’:ti,ab OR ‘absenteeism’/exp OR ‘productivity’/exp).
- CINAHL: (“wearable device*” OR “wearable” OR “sensor*” OR “exoskeleton*” OR “smart helmet*” OR “biosensor*”) AND (“healthcare worker*” OR “hospital staff” OR “nurse*” OR “physician*” OR “employee*”) AND (“occupational health” OR “staff safety” OR “workplace safety” OR “organizational resilience” OR “business continuity” OR “absenteeism” OR “productivity”).
3. Results
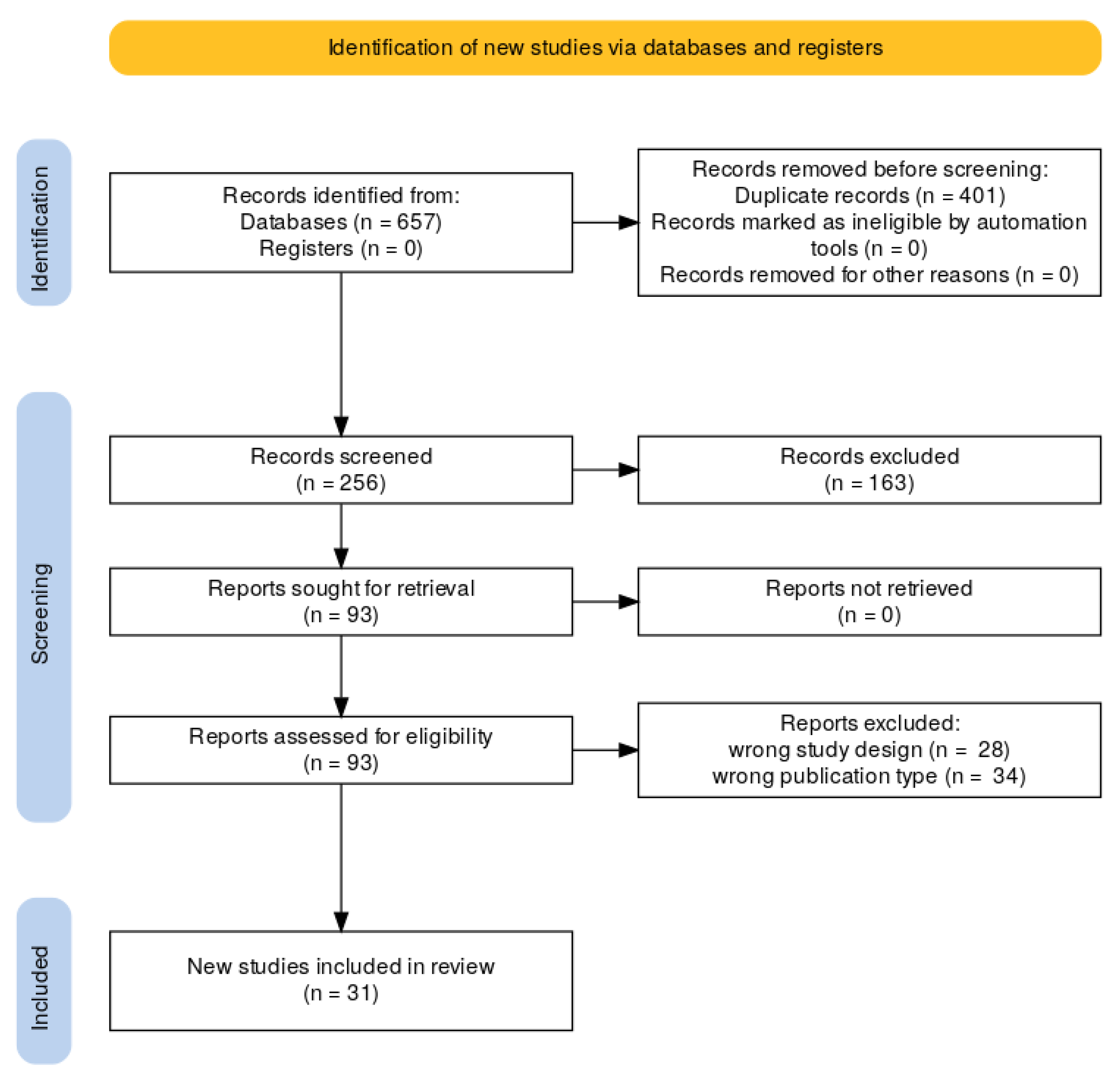
3.1. Literature Search
3.2. General Characteristics of the Included Studies
3.2.1. Staff Safety
3.2.2. Stress and Burnout
3.2.3. Absenteeism and Presenteeism
3.2.4. Economic and Cost Implications
3.3. Results of Characteristics Referred to PICOS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alabduljabbar, Z.M.; Al Beshri, Z.S.; Alhejji, E.A.; Qismayn, A.I.; Al Shuhaib, J.Y.; Abushomi, H.Q.; A Musad, A.A.; Alshammari, B.S.S.; Alyahya, A.A.; Alghanem, A.M.A. A Review of Psychological and Moral Challenges Faced by Medical Staff in High-Stress Environments. J. Ecohumanism 2024, 3, 983–990. [Google Scholar] [CrossRef]
- Honda, H.; Iwata, K. Personal Protective Equipment and Improving Compliance among Healthcare Workers in high-risk settings. Curr. Opin. Infect. Dis. 2016, 29, 400–406. [Google Scholar] [CrossRef]
- Foghammar, L.; Jang, S.; Kyzy, G.A.; Weiss, N.; Sullivan, K.A.; Gibson-Fall, F.; Irwin, R. Challenges in Researching Violence Affecting Health Service Delivery in Complex Security Environments. Soc. Sci. Med. 2016, 162, 219–226. [Google Scholar] [CrossRef]
- Ahmad, I.A.; Osei, E. Occupational Health and Safety Measures in Healthcare Settings during COVID-19: Strategies for Protecting Staff, Patients and Visitors. Disaster Med. Public Health Prep. 2021, 17, e48. [Google Scholar] [CrossRef]
- Lowe, A.; Gibbs, S. How Should Health Care Organizations Protect Personnel in Environmental Services and Related Fields? AMA J. Ethics 2022, 24, E846–E852. [Google Scholar] [CrossRef]
- Lamb, L.E.; Cox, A.; Fletcher, T.; McCourt, A. Formulating and Improving Care While Mitigating Risk in a Military Ebo La Virus Disease Treatment Unit. J. R. Army Med. Corps 2016, 163, 2–6. [Google Scholar] [CrossRef]
- Fast, L.; Wille, C. To Stay or Go? The Complexities of Providing Healthcare in Insecure Environments. World Health Popul. 2016, 16, 38–42. [Google Scholar] [CrossRef]
- Edgar, M.; Selvaraj, S.A.; Lee, K.E.; Caraballo-Arias, Y.; Harrell, M.; Rodríguez-Morales, A. Healthcare Workers, Epidemic Biological Risks—Recommendations Based on the Experience with COVID-19 and Ebolavirus. Infez. Med. 2022, 30, 168. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, L.; Sala, R.; Navarro, J.-B. Resilience and Occupational Health of Health Care Workers: A Moderator Analysis of Organizational Resilience and Sociodemographic Attributes. Int. Arch. Occup. Env. Health 2021, 95, 223–232. [Google Scholar] [CrossRef] [PubMed]
- Tamanna, M.; Sharma, S. Do Resilient Organizations Enhance Organizational Performance? Int. J. Sci. Technol. Res. 2020, 9, 3610–3612. [Google Scholar]
- Lundstrom, T.; Pugliese, G.; Bartley, J.; Cox, J.; Guither, C. Organizational and Environmental Factors That Affect Worker Health and Safety and Patient Outcomes. Am. J. Infect. Control 2002, 30, 93–106. [Google Scholar] [CrossRef] [PubMed]
- Gaspar, T.; Gomez-Baya, D.; Guedes, F.B.; Correia, M.F. Health Management: Evaluating the Relationship between Organizational Factors, Psychosocial Risks at Work, Performance Management, and Hospital Outcomes. Healthcare 2023, 11, 2744. [Google Scholar] [CrossRef]
- Miller, K. Risk Factors and Impacts of Occupational Injury in Healthcare Workers: A Critical Review. OA Musculoskelet. Med. 2013, 1, 4. [Google Scholar] [CrossRef][Green Version]
- Boczkowska, K.; Niziołek, K. Health and Safety Strategy in Medical Institutions: Employee Participation. In Organizational Change and Relational Resources; Routledge: Abingdon, UK, 2021; pp. 197–210. ISBN 978-1-00-317260-4. [Google Scholar]
- Darrow, L. Exploring the Factors That Drive Organizational Resilience: Lessons from Healthcare. Master’s Thesis, Oregon State University, Corvallis, OR, USA, 2017. [Google Scholar]
- Cotton, P.; Hart, P.M. Occupational Wellbeing and Performance: A Review of Organisational Health Research. Aust. Psychol. 2003, 38, 118–127. [Google Scholar] [CrossRef]
- Kuster, S.P.; Böni, J.; Kouyos, R.D.; Huber, M.; Schmutz, S.; Shah, C.; Bischoff-Ferrari, H.A.; Distler, O.; Battegay, E.; Giovanoli, P.; et al. Absenteeism and Presenteeism in Healthcare Workers Due to Respiratory Illness. Infect. Control Hosp. Epidemiol. 2020, 42, 268–273. [Google Scholar] [CrossRef]
- Gianino, M.M.; Politano, G.; Scarmozzino, A.; Stillo, M.; Amprino, V.; Di Carlo, S.; Benso, A.; Zotti, C.M. Cost of Sickness Absenteeism during Seasonal Influenza Outbreaks of Medium Intensity among Health Care Workers. Int. J. Environ. Res. Public Health 2019, 16, 747. [Google Scholar] [CrossRef]
- Van Buynder, P.G.; Konrad, S.; Kersteins, F.; Preston, E.; Brown, P.D.; Keen, D.; Murray, N.J. Healthcare Worker Influenza Immunization Vaccinate or Mask Policy: Strategies for Cost Effective Implementation and Subsequent Reductions in Staff Absenteeism Due to Illness. Vaccine 2015, 33, 1625–1628. [Google Scholar] [CrossRef] [PubMed]
- Imai, C.; Toizumi, M.; Hall, L.; Lambert, S.; Halton, K.; Merollini, K. A Systematic Review and Meta-Analysis of the Direct Epidemiological and Economic Effects of Seasonal Influenza Vaccination on Healthcare Workers. PLoS ONE 2018, 13, e0198685. [Google Scholar] [CrossRef] [PubMed]
- Strömberg, C.; Aboagye, E.; Hagberg, J.; Bergström, G.; Lohela-Karlsson, M. Estimating the Effect and Economic Impact of Absenteeism, Presenteeism, and Work Environment–Related Problems on Reductions in Productivity from a Managerial Perspective. Value Health 2017, 20, 1058–1064. [Google Scholar] [CrossRef]
- Davis, K.; Collins, S.; Doty, M.; Ho, A.; Holmgren, A.L. Health and Productivity Among U.S. Workers. Issue Brief 2005, 856, 1–10. [Google Scholar]
- Nechita, P.; Oroian, B.A.; Schipor, P.D.; Enache, A.L.; Popa, M.V. The Link Between Work Stress, Absenteeism, and Sickness absence: The Impact of Burnout on Healthcare Workers. Bull. Integr. Psychiatry 2025, 2, 29–39. [Google Scholar] [CrossRef]
- Naidoo, R.; Naidoo, S.; Hariparsad, S. Disabling health: The Challenge of Incapacity Leave and Sickness Abse Nce Management in the Public Health Sector in KwaZulu-Natal Province. S. Afr. Health Rev. 2016, 2016, 61–72. [Google Scholar]
- Tarakci, H.; Kulkarni, S.; Ozdemir, Z.D. The Impact of Wearable Devices and Performance Payments on Health Outcomes. Int. J. Prod. Econ. 2018, 200, 291–301. [Google Scholar] [CrossRef]
- Rane, N.; Choudhary, S.; Rane, J. Leading-Edge Wearable Technologies in Enhancing Personalized Safety on Construction Sites: A Review. SSRN J. 2023. [Google Scholar] [CrossRef]
- Patel, V.; Chesmore, A.; Legner, C.M.; Pandey, S. Trends in Workplace Wearable Technologies and Connected-Worker Solutions for Next-Generation Occupational Safety, Health, and Productivity. Adv. Intell. Syst. 2021, 4, 2100099. [Google Scholar] [CrossRef]
- Pavón, I.; Sigcha, L.; Arezes, P.; Costa, N.; Arcas, G.; López, J.M. Wearable Technology for Occupational Risk Assessment: Potential Avenue s for Applications. In Occupational Safety and Hygiene VI; CRC Press: Boca Raton, FL, USA, 2018; pp. 447–452. ISBN 978-1-351-00888-4. [Google Scholar]
- Banerjee, S.; Hempel, M.; Sharif, H. A Review of Workspace Challenges and Wearable Solutions in Railroads a Nd Construction. In Proceedings of the 2017 13th International Wireless Communications and Mobile Computing Conference (IWCMC), Valencia, Spain, 26–30 June 2017; IEEE: New York, NY, USA, 2017; pp. 91–96. [Google Scholar]
- Kritzler, M.; Bäckman, M.; Tenfält, A.; Michahelles, F. Wearable Technology as a Solution for Workplace Safety. In Proceedings of the 14th International Conference on Mobile and Ubiquitous Multimedia, Linz, Austria, 30 November–2 December 2015; ACM: New York, NY, USA, 2015; pp. 213–217. [Google Scholar]
- Barata, J.; da Cunha, P.R. Safety Is the New Black: The Increasing Role of Wearables in Occupational Health and Safety in Construction. In Lecture Notes in Business Information Processing; Springer International Publishing: Berlin/Heidelberg, Germany, 2019; pp. 526–537. ISBN 978-3-030-20484-6. [Google Scholar]
- De Vasconcelos, F.M.; Almeida, C.F.M.; Gualtieri, S.R.; Danesin, L.A.; Kagan, N.; Cruz, L.H.; Mollica, D.; de Demuner, S.V.R.; Dominice, A.; Filho, J.S. Wearable Sensing for Work Safety and Occupational Health Applied to an Electric Power Distributor. IET Conf. Proc. 2021, 2021, 1717–1721. [Google Scholar] [CrossRef]
- Schall, M.C., Jr.; Sesek, R.F.; Cavuoto, L.A. Barriers to the Adoption of Wearable Sensors in the Workplace: A Surve y of Occupational Safety and Health Professionals. Hum. Factors 2018, 60, 351–362. [Google Scholar] [CrossRef] [PubMed]
- Reid, C.R.; Schall, M.C., Jr.; Amick, R.Z.; Schiffman, J.M.; Lu, M.-L.; Smets, M.; Moses, H.R.; Porto, R. Wearable Technologies: How Will We Overcome Barriers to Enhance Worker Performance, Health, And Safety? Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2017, 61, 1026–1030. [Google Scholar] [CrossRef]
- Dos Schwambach, S.G.C.; Sott, M.K.; Schwambach, R.E. Wearable Devices and Workplace Productivity: A Bibliometric Analysis of Their Integration into Professional Environments. Dataset Rep. 2024, 3, 101–106. [Google Scholar] [CrossRef]
- Biswas, A.; Begum, M.; Van Eerd, D.; Johnston, H.; Smith, P.M.; Gignac, M.A.M. Integrating Safety and Health Promotion in Workplaces: A Scoping Revie w of Facilitators, Barriers, and Recommendations. Health Promot. Pract. 2021, 23, 984–998. [Google Scholar] [CrossRef]
- Busetto, L.; Luijkx, K.; Calciolari, S.; Ortiz, L.G.G.; Vrijhoef, H.J.M. Barriers and Facilitators to Workforce Changes in Integrated Care. Int. J. Integr. Care 2018, 18, 17. [Google Scholar] [CrossRef] [PubMed]
- Maltseva, K. Wearables in the Workplace: The Brave New World of Employee Engagement. Bus. Horiz. 2020, 63, 493–505. [Google Scholar] [CrossRef]
- Bhullar, G. “Wear” Is the Manufacturing Future: The Latest Fashion Hitting the Workplace. In Lecture Notes in Computer Science; Springer International Publishing: Berlin/Heidelberg, Germany, 2015; pp. 49–56. ISBN 978-3-319-26137-9. [Google Scholar]
- Arksey, H.; O’Malley, L. Scoping Studies: Towards a Methodological Framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping Studies: Advancing the Methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Rayyan. Available online: https://www.rayyan.ai/ (accessed on 12 August 2025).
- Briscoe, S.; Bethel, A.; Rogers, M. Conduct and Reporting of Citation Searching in Cochrane Systematic Reviews: A Cross-Sectional Study. Res. Synth. Methods 2020, 11, 169–180. [Google Scholar] [CrossRef]
- Agarwal, A.K.; Gonzales, R.; Scott, K.; Merchant, R. Investigating the Feasibility of Using a Wearable Device to Measure Physiologic Health Data in Emergency Nurses and Residents: Observational Cohort Study. JMIR Form. Res. 2024, 8, e51569. [Google Scholar] [CrossRef] [PubMed]
- Paradiso, R.; Krijnen, E.; Vannetti, F. Wearable System for the evaluation of Well-Being in the Workplace. In Cognitive Computing and Internet of Things; AHFE International: New York, NY, USA, 2024. [Google Scholar] [CrossRef]
- Shishavan, H.H.; Garza, J.; Henning, R.; Cherniack, M.; Hirabayashi, L.; Scott, E.; Kim, I. Continuous Physiological Signal Measurement over 24-Hour Periods to Assess the Impact of Work-Related Stress and Workplace Violence. Appl. Ergon. 2023, 108, 103937. [Google Scholar] [CrossRef]
- Clingan, C.A.; Dittakavi, M.; Rozwadowski, M.; Gilley, K.N.; Cislo, C.R.; Barabas, J.; Sandford, E.; Olesnavich, M.; Flora, C.; Tyler, J.; et al. Monitoring Health Care Workers at Risk for COVID-19 Using Wearable Sensors and Smartphone Technology: Protocol for an Observational mHealth Study. JMIR Res. Protoc. 2021, 10, e29562. [Google Scholar] [CrossRef]
- Keller, S.C.; Salinas, A.B.; Oladapo-Shittu, O.; Cosgrove, S.E.; Lewis-Cherry, R.; Osei, P.; Gurses, A.P.; Jacak, R.; Zudock, K.K.; Blount, K.M.; et al. The Case for Wearable Proximity Devices to Inform Physical Distancing among Healthcare Workers. JAMIA Open 2021, 4, ooab095. [Google Scholar] [CrossRef]
- Ghosh, K.; Nanda, S.; Hurt, R.T.; Schroeder, D.R.; West, C.P.; Fischer, K.M.; Bauer, B.A.; Fokken, S.C.; Ganesh, R.; Hanson, J.L.; et al. Mindfulness Using a Wearable Brain Sensing Device for Health Care Professionals During a Pandemic: A Pilot Program. J. Prim. Care Community Health 2023, 14, 21501319231162308. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Lee, H. The Effect of Communication in Emergency Department Isolation Rooms Using Smart Glasses: A Mixed-Methods Study. J. Clin. Nurs. 2025, 34, 4340–4350. [Google Scholar] [CrossRef]
- Weenk, M.; Bredie, S.J.; Koeneman, M.; Hesselink, G.; van Goor, H.; van de Belt, T.H. Continuous Monitoring of Vital Signs in the General Ward Using Wearable Devices: Randomized Controlled Trial. J. Med. Internet Res. 2020, 22, e15471. [Google Scholar] [CrossRef]
- Kooij, L.; Peters, G.M.; Doggen, C.J.M.; van Harten, W.H. Remote Continuous Monitoring with Wireless Wearable Sensors in Clinical Practice, Nurses Perspectives on Factors Affecting Implementation: A Qualitative Study. BMC Nurs. 2022, 21, 53. [Google Scholar] [CrossRef]
- Scott, A. Confronting Challenge: Enabling Care Home Staff to Understand and Work Effectively with Challenging Behaviours in Dementia. Eur. Psychiatry 2008, 23, S395. [Google Scholar] [CrossRef]
- O’Dwyer, B.; Jaana, M.; Hui, C.; Chreim, S.; Ellis, J. Digital Contact Tracing Implementation Among Leaders and Health Care Workers in a Pediatric Hospital During the COVID-19 Pandemic: Qualitative Interview Study. JMIR Public Health Surveill. 2024, 10, e64270. [Google Scholar] [CrossRef] [PubMed]
- Rosiello, F.; Pietrantonio, F.; Di Lorenzo, J.; Bertani, G.; Anzidei, A.; Laurelli, G.; Cipriano, E.; Di Iorio, C.; Montagnese, F.; Pascucci, M. Could the Miniaturize Techonologies Improve Patients Adherence and Assure Better Quality of Life? Eur. J. Public Health 2021, 31, iii398. [Google Scholar] [CrossRef]
- Schonck, F.; Luyer, M.; van der Meer, N.; Bouwman, A.; Nienhuijs, S. Implementation of a Surgical Ward Innovation: Telemonitoring Controlled by Healthdot [SWITCH-Trial PROTOCOL]. PLoS ONE 2025, 20, e0322472. [Google Scholar] [CrossRef]
- Joshi, M.; Archer, S.; Morbi, A.; Ashrafian, H.; Arora, S.; Khan, S.; Cooke, G.; Darzi, A. Perceptions on the Use of Wearable Sensors and Continuous Monitoring in Surgical Patients: Interview Study Among Surgical Staff. JMIR Form. Res. 2022, 6, e27866. [Google Scholar] [CrossRef]
- Iqbal, F.M.; Joshi, M.; Khan, S.; Ashrafian, H.; Darzi, A. Implementation of Wearable Sensors and Digital Alerting Systems in Secondary Care: Protocol for a Real-World Prospective Study Evaluating Clinical Outcomes. JMIR Res. Protoc. 2021, 10, e26240. [Google Scholar] [CrossRef]
- Brewster, L.; Mountain, G.; Wessels, B.; Kelly, C.; Hawley, M. Factors Affecting Front Line Staff Acceptance of Telehealth Technologies: A Mixed-method Systematic Review. J. Adv. Nurs. 2013, 70, 21–33. [Google Scholar] [CrossRef]
- Iqbal, F.M.; Joshi, M.; Fox, R.; Koutsoukou, T.; Sharma, A.; Wright, M.; Khan, S.; Ashrafian, H.; Darzi, A. Outcomes of Vital Sign Monitoring of an Acute Surgical Cohort with Wearable Sensors and Digital Alerting Systems: A Pragmatically Designed Cohort Study and Propensity-Matched Analysis. Front. Bioeng. Biotechnol. 2022, 10, 895973. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.; Moukhtarian, T.R.; Russell, S.; Daly, G.; Walasek, L.; Tang, N.K.Y.; Toro, C.; Meyer, C. Digital Cognitive Behavioural Therapy Intervention in the Workplace: Study Protocol for a Feasibility Randomised Waitlist-Controlled Trial to Improve Employee Mental Well-Being, Engagement and Productivity. BMJ Open 2022, 12, e060545. [Google Scholar] [CrossRef] [PubMed]
- Santomauro, C.; McCurdie, T.; Pollard, C.; Shuker, M. Exploring the Feasibility of Wearable Technologies to Provide Interactive Telepresence Sub-Specialist Support to Remote Clinicians Treating Patients with Traumatic Injuries. Prehospital Disaster Med. 2019, 34, s85. [Google Scholar] [CrossRef]
- Shah, A.; Guessi, M.; Wali, S.; Ware, P.; McDonald, M.; O’Sullivan, M.; Posada, J.D.; Ross, H.; Seto, E. The Resilience of Cardiac Care Through Virtualized Services During the COVID-19 Pandemic: Case Study of a Heart Function Clinic. JMIR Cardio 2021, 5, e25277. [Google Scholar] [CrossRef]
- Buss, A.; Areia, C.; Biggs, C.; Edmundson, H.; Young, L.; Roman, C.; Santos, M.; Tarassenko, L.; Watkinson, P.; Vollam, S. Using a Novel Ambulatory Monitoring System to Support Patient Safety on an Acute Infectious Disease Ward During an Unfolding Pandemic. J. Adv. Nurs. 2023, 80, 2452–2461. [Google Scholar] [CrossRef] [PubMed]
- Meltzer, A.J.; Hallbeck, M.S.; Morrow, M.M.; Lowndes, B.R.; Davila, V.J.; Stone, W.M.; Money, S.R. Measuring Ergonomic Risk in Operating Surgeons by Using Wearable Technology. JAMA Surg. 2020, 155, 444. [Google Scholar] [CrossRef]
- Claudio, D.; Velázquez, M.A.; Bravo-Llerena, W.; Okudan, G.E.; Freivalds, A. Perceived Usefulness and Ease of Use of Wearable Sensor-Based Systems in Emergency Departments. IIE Trans. Occup. Ergon. Hum. Factors 2015, 3, 177–187. [Google Scholar] [CrossRef]
- Carreon, H.F.; Dutra, D. Inpatient Outcomes of a Hands-Free, Wireless Communication Device Implementation. CIN Comput. Inform. Nurs. 2020, 38, 323–328. [Google Scholar] [CrossRef]
- Yesmin, T.; Carter, M.W.; Gladman, A.S. Internet of Things in Healthcare for Patient Safety: An Empirical Study. BMC Health Serv. Res. 2022, 22, 278. [Google Scholar] [CrossRef]
- Jones, D.D.; Heaton, H.A.; Wallerich, T.J.; Riekmann, L.A.; Handmacher, B.H.; Hatton, R.L. Wearable Real Time Location Services Technology for Staff Duress in Healthcare. In Proceedings of the 2023 IEEE 13th International Conference on RFID Technology and Applications (RFID-TA), Aveiro, Portugal, 4–6 September 2023; IEEE: New York, NY, USA, 2023; pp. 127–129. [Google Scholar]
- Jovanov, E.; Frith, K.; Anderson, F.; Milosevic, M.; Shrove, M.T. Real-Time Monitoring of Occupational Stress of Nurses. In Proceedings of the 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Boston, MA, USA, 30 August–3 September 2011; IEEE: New York, NY, USA, 2011; pp. 3640–3643. [Google Scholar]
- Hanna, S. Sensors and Wearables in Oncology: A Study of the Barriers and Facilitators to Adoption. Ph.D. Thesis, George Washington University, Washington, DC, USA, 2020. [Google Scholar] [CrossRef]
- McLean, K.A.; Sgrò, A.; Brown, L.R.; Buijs, L.F.; Mozolowski, K.; Daines, L.; Cresswell, K.; Potter, M.A.; Bouamrane, M.-M.; Harrison, E.M. Implementation of Digital Remote Postoperative Monitoring in Routine Practice: A Qualitative Study of Barriers and Facilitators. BMC Med. Inform. Decis. Mak. 2024, 24, 307. [Google Scholar] [CrossRef]
- Lokmic-Tomkins, Z.; Lin, Y.-F.; Robinson, E.; Bichel-Findlay, J.; Faisal, M.; Dowding, D. Insights from the Rapid Implementation of Digital Technologies in Nursing Practice during COVID-19—A Survey. Contemp. Nurse 2025. [Google Scholar] [CrossRef]
- Joshi, M.; Archer, S.; Morbi, A.; Arora, S.; Kwasnicki, R.; Ashrafian, H.; Khan, S.; Cooke, G.; Darzi, A. Short-Term Wearable Sensors for In-Hospital Medical and Surgical Patients: Mixed Methods Analysis of Patient Perspectives. JMIR Perioper Med. 2021, 4, e18836. [Google Scholar] [CrossRef] [PubMed]
- González Ramírez, M.L.; García Vázquez, J.P.; Rodríguez, M.D.; Padilla-López, L.A.; Galindo-Aldana, G.M.; Cuevas-González, D. Wearables for Stress Management: A Scoping Review. Healthcare 2023, 11, 2369. [Google Scholar] [CrossRef]
- Barac, M.; Scaletty, S.; Hassett, L.C.; Stillwell, A.; Croarkin, P.E.; Chauhan, M.; Chesak, S.; Bobo, W.V.; Athreya, A.P.; Dyrbye, L.N. Wearable Technologies for Detecting Burnout and Well-Being in Health Care Professionals: Scoping Review. J. Med. Internet Res. 2024, 26, e50253. [Google Scholar] [CrossRef]
- Vries, H.D.; Kamphuis, W.; Oldenhuis, H.K.E.; Schans, C.; Sanderman, R. Modelling Employee Resilience Using Wearables and Apps: A Conceptual Framework and Research Design. Int. J. Adv. Life Sci. 2019, 11, 110–118. [Google Scholar]
- Roussel, L.A. On-the-Go Strategies to Enhance Resilience and Self-Care. Nurs. Clin. N. Am. 2022, 57, 501–512. [Google Scholar] [CrossRef]
- Mistretta, E.G.; Davis, M.C.; Temkit, M.; Lorenz, C.; Darby, B.; Stonnington, C.M. Resilience Training for Work-Related Stress Among Health Care Workers. J. Occup. Environ. Med. 2018, 60, 559–568. [Google Scholar] [CrossRef] [PubMed]
- De Sario Velasquez, G.D.; Borna, S.; Maniaci, M.J.; Coffey, J.D.; Haider, C.R.; Demaerschalk, B.M.; Forte, A.J. Economic Perspective of the Use of Wearables in Health Care: A Systematic Review. Mayo Clin. Proc. Digit. Health 2024, 2, 299–317. [Google Scholar] [CrossRef] [PubMed]
- Souza, M.; Miyagawa, T.; Melo, P.; Maciel, F. Wellness Programs: Wearable Technologies Supporting Healthy Habits and Corporate Costs Reduction. In Communications in Computer and Information Science; Springer International Publishing: Berlin/Heidelberg, Germany, 2017; pp. 293–300. ISBN 978-3-319-58752-3. [Google Scholar]
- Lewy, H. Wearable Technologies—Future Challenges for Implementation in Health Care Services. Healthc. Technol. Lett. 2015, 2, 2–5. [Google Scholar] [CrossRef] [PubMed]
- Leenen, J.P.L.; Leerentveld, C.; van Dijk, J.D.; van Westreenen, H.L.; Schoonhoven, L.; Patijn, G.A. Current Evidence for Continuous Vital Signs Monitoring by Wearable Wireless Devices in Hospitalized Adults: Systematic Review. J. Med. Internet Res. 2020, 22, e18636. [Google Scholar] [CrossRef]
- Rost, K.; Smith, J.L.; Dickinson, M. The Effect of Improving Primary Care Depression Management on Employee Absenteeism and Productivity. Med. Care 2004, 42, 1202–1210. [Google Scholar] [CrossRef] [PubMed]
- Mattison, G.; Canfell, O.; Forrester, D.; Dobbins, C.; Smith, D.; Töyräs, J.; Sullivan, C. The Influence of Wearables on Health Care Outcomes in Chronic Disease: Systematic Review. J. Med. Internet Res. 2022, 24, e36690. [Google Scholar] [CrossRef]
- Kuratomi, D.; Shin, C.; Duffy, V.G. Systematic Literature Review on the Advances of Wearable Technologies. In Lecture Notes in Computer Science; Springer Nature: Cham, Switzerland, 2023; pp. 78–95. ISBN 978-3-031-48046-1. [Google Scholar]
- D’ettorre, G.; Greco, M. Healthcare Work and Organizational Interventions to Prevent Work-Related Stress in Brindisi, Italy. Saf. Health Work 2015, 6, 35–38. [Google Scholar] [CrossRef] [PubMed]
- Haas, E.J.; Cauda, E. Using Core Elements of Health and Safety Management Systems to Support Worker Well-Being During Technology Integration. Int. J. Environ. Res. Public Health 2022, 19, 13849. [Google Scholar] [CrossRef]
- Ruotsalainen, J.; Verbeek, J.; Mariné, A.; Serra, C. Preventing Occupational Stress in Healthcare Workers. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef]
- Crotty, A.; Killian, J.M.; Miller, A.; Chilson, S.; Wright, R. Using Wearable Technology to Prevent Pressure Injuries: An Integrative Review. Worldviews Evid.-Based Nurs. 2023, 20, 351–360. [Google Scholar] [CrossRef]
- Santoro, A.; Di Prinzio, R.R.; Camisa, V.; Vinci, M.R.; Dalmasso, G.; Dosi, A.; De Santis, M.; Macina, N.M.; Raponi, M.; Mesolella, V.; et al. P-596 the Evaluation of Workplace Disability Management Program for Healthcare Workers in the Total Worker Health® Approach: The Return on Investment. Occup. Med. 2024, 74. [Google Scholar] [CrossRef]
- Noben, C.; Evers, S.; Nieuwenhuijsen, K.; Ketelaar, S.; Gärtner, F.; Sluiter, J.; Smit, F. Protecting and Promoting Mental Health of Nurses in the Hospital Setting: Is It Cost-Effective from an Employer’s Perspective? Int. J. Occup. Med. Environ. Health 2015, 28, 891–900. [Google Scholar] [CrossRef]
- Slight, S.P.; Franz, C.; Olugbile, M.; Brown, H.V.; Bates, D.W.; Zimlichman, E. The Return on Investment of Implementing a Continuous Monitoring Syste m in General Medical-Surgical Units. Crit. Care Med. 2014, 42, 1862–1868. [Google Scholar] [CrossRef] [PubMed]
| Population (P) | Healthcare workers, including nurses, physicians, hospital staff, and allied health professionals, employed in clinical and hospital settings. These individuals operate in high-risk occupational environments characterized by psychosocial stressors, absenteeism, and the need for continuous service delivery. |
| Intervention (I) | Implementation of wearable technologies (e.g., physiological sensors, biometric patches, smart glasses, real-time location systems, exoskeletons, and continuous monitoring devices). The intervention focuses on enhancing occupational health, staff safety, and organizational resilience through continuous monitoring, predictive analytics, and integration with occupational health protocols. |
| Comparison (C) | Standard occupational health and safety practices without the use of wearable devices, or alternative types of wearable technologies/implementation strategies. |
| Outcomes (O) |
|
| Study design (S) | All study designs were eligible, including experimental (e.g., randomized controlled trials, pilot studies), observational (e.g., cohort, cross-sectional, longitudinal), qualitative, and mixed-methods studies. |
| Study | Study Design | Healthcare Setting | Technology Type | Primary Outcomes | Adoption Rate | User Satisfaction | Implementation Challenges | Measured Impact | Cost Implications | Implementation Requirements |
|---|---|---|---|---|---|---|---|---|---|---|
| Agarwal et al., 2024 [45] | Pilot, Longitudinal | Academic, urban, level 1 trauma center (US) | WHOOP band | Device use, acceptance, burnout, HRV, sleep | 50% consistent use | Residents more engaged | Device features, engagement | Device use, mild anxiety, low fulfillment | No economic analysis | Device optimization |
| Paradiso et al., 2024 [46] | Pilot study | No mention found | Wearable Wellness System (WWS) by Smartex | Heart rate (HR), HRV, stress, posture | No mention found | Designed for comfort | No mention found | Stress, posture | No economic analysis | Comfortable design |
| Shishavan et al., 2022 [47] | Pilot, Longitudinal | Intensive care unit, no mention found | Multiparameter armband | HRV, pulse transit time (PTT), stress | High | Well accepted | No mention found | Stress detection | No economic analysis | High signal quality |
| Clingan et al., 2021 [48] | Longitudinal, Pilot | Academic institution (Michigan, US) | Fitbit Charge 3, TempTraq | Feasibility, HR, temperature, COVID-19 detection | No mention found | No mention found | Internet access, digital literacy | Feasible, mood/symptom tracking | No economic analysis | Digital literacy |
| Keller et al., 2021 [49] | Pilot study | Inpatient unit, no mention found | Proximity beacons | No mention found | No mention found | No mention found | Feasibility, physical distancing | No mention found | No economic analysis | Feasibility |
| Ghosh et al., 2023 [50] | Pilot study | No mention found | MUSE-S™ | Stress, resilience, quality of life (QoL), cognition | High | 91.9% felt relaxed, 73% would continue | No mention found | Improved stress, resilience | No economic analysis | Ease of use |
| Park and Lee, 2025 [51] | Mixed-methods, pretest-posttest | Emergency department | Smart glasses | Communication clarity, workload | No mention found | Improved communication | User interface, privacy, workload | Improved clarity, workload | No economic analysis | Training, privacy |
| Weenk et al., 2019 [52] | Randomized controlled trial (RCT) | University hospital (Netherlands) | ViSi Mobile, HealthPatch | Psychological distress, usability | No mention found | Generally positive | Device size, training | Positive, reduced workload | Reduced workload, costs | Training, monitoring |
| Kooij et al., 2022 [53] | Qualitative | Teaching hospitals (Netherlands) | Philips Biosensor, SensiumPatch | No mention found | No mention found | Mixed | Sensor quality, Wi-Fi, workload | Mixed, reduced stays | Reduced stays, home recovery | Interoperability |
| Scott, 2008 [54] | Case study, qualitative | Dementia care homes (UK) | Location-tracking devices | No mention found | No mention found | No mention found | Privacy, alarms, training | Enhanced safety | No economic analysis | Stakeholder involvement |
| O’Dwyer et al., 2024 [55] | Qualitative | Pediatric hospital (Canada) | No mention found | No mention found | No mention found | High satisfaction | Risk assessment, staffing | Positive, feasible | No economic analysis | Human-centered design |
| Rosiello et al., 2021 [56] | Pilot, RCT | Multiple hospitals, no mention found | Wireless Vital Parameter Monitoring (WVPCM) system | Clinical-economic impact | No mention found | No mention found | Nursing time reduction | Reduced complications, readmissions | €54-90 saved per patient | Nursing time reduction |
| Schonck et al., 2025 [57] | Observational, Longitudinal | Surgical ward, no mention found | Healthdot (Philips) | Workload (Individual Workload Scale), implementation outcomes | No mention found | Assessed via System Usability Scale, Evidence-Based Practice Attitude Scale | Workload, complexity | No mention found | No economic analysis | Efficiency, workload |
| Joshi et al., 2021 [58] | Cross-sectional | Academic hospital (UK) | SensiumVitals | No mention found | No mention found | High engagement | Alerts, workload | No mention found | No economic analysis | Alerts, comfort |
| Iqbal et al., 2021 [59] | Pre-post, Observational | National Health Service (NHS) hospital (UK) | SensiumVitals | Clinical outcomes | No mention found | No mention found | No mention Found | No mention found | No economic analysis | Integration, training |
| Brewster et al., 2014 [60] | Mixed-method review | No mention found | Telehealth | No mention found | No mention found | No mention found | Service change, technical | No mention found | No economic analysis | Service change |
| Iqbal et al., 2022 [61] | Observational cohort | Surgical unit (UK) | SensiumVitals | Clinical outcomes | No mention found | Favorable | Alert fatigue, workflow | No mention found | No economic analysis | Workflow, policies |
| Patel et al., 2022 [62] | Mixed methods | General Medicine (Canada) | Fitbit Charge 2/3 | No mention found | No mention found | Patients positive, nurses mixed | Device design workflow | No mention found | No economic analysis | Device design |
| Santomauro et al., 2019 [63] | Pilot study | Rural/regional hospitals | Near-field display devices | No mention found | No mention found | Positive | Functionality preferences | No mention found | No economic analysis | Usability testing |
| Shah et al., 2021 [64] | Case study, qualitative | Academic hospital (Canada) | Medly (mobile) | No mention found | No mention found | No mention found | Siloed systems workflow | No mention found | No economic analysis | Leadership, connectivity |
| Buss et al., 2023 [65] | Qualitative evaluation | Academic hospital (UK) | VitalPatch, WristOx2 | No mention found | No mention found | Supportive over time | Device numbers contact | Supportive, workload | No economic analysis | Device numbers |
| Meltzer et al., 2020 [66] | Case series | Academic hospital (US) | IMUs | Ergonomic risk | No mention found | Encouraged | Sample size | Risk factors identified | No economic analysis | Mindfulness |
| Claudio et al., [67] | Pilot study | Emergency departments | Wireless sensor system | No mention found | No mention found | High | No mention found | Positive | No economic analysis | User feedback |
| Carreon and Dutra, 2020 [68] | Observational no mention found) | No mention found | Hands-free communication device | No mention found | No mention found | No mention found | Communication failures | Improved workflow | No economic analysis | Infrastructure |
| Yesmin et al., 2022 [69] | Longitudinal | Hospital ward (Canada) | No mention found | Patient safety outcomes | No mention found | Positive | Training, device issues | Improved care time | No economic analysis | Training, device |
| Joshi et al., 2022 [58] | Interview study | Academic hospital (UK) | SensiumVitals | No mention found | No mention found | High engagement | Equipment, staff | No mention found | No economic analysis | Comfort, future |
| Jones et al., 2023 [70] | Pilot study (no mention found) | Academic medical center (US) | Real-time location system (RTLS) | No mention found | No mention found | No mention found | No mention found | Improved safety | No economic analysis | Real-time location system rollout |
| Jovanov et al., 2011 [71] | Pilot study | Academic nursing (US) | UAHealth (iPhone, Ant+) | Stress index, HRV | No mention found | Facilitated by user interface | No mention found | Stress index, heart rate variability | No economic analysis | User interface, support |
| Hanna, 2020 [72] | Qualitative study | Multiple (US) | Multiple sensor types | No mention found | No mention found | No mention found | Cost, communication | No mention found | High cost barrier | Collaboration |
| Mclean et al., 2024 [73] | Qualitative implementation | Tertiary hospitals (UK) | No mention found | No mention found | No mention found | Mixed | Information technology, workload | No mention found | No economic analysis | Information technology, strategy |
| Lokmic-Tomkins et al., 2025 [74] | Cross-sectional | Clinical settings (Australia) | No mention found | No mention found | No mention found | No mention found | Infrastructure, support | No mention found | No economic analysis | Infrastructure, support |
| Element | Summary (Bullet Points) |
|---|---|
| Population (P) | • Healthcare professionals (nurses, physicians, residents, allied health staff, support staff). • Predominantly hospital and clinical settings (e.g., ICUs, surgical wards, EDs, academic hospitals). • Smaller number in community care, dementia homes, pediatric hospitals. |
| Intervention (I) | • Continuous physiological monitoring systems (e.g., SensiumVitals, Philips Biosensor/Healthdot, ViSi Mobile/HealthPatch, WVPCM). • Consumer-grade wearables (Fitbit, WHOOP, MUSE-S™) • Specialized technologies (smart glasses, proximity beacons, real-time location systems, exoskeletons, wireless sensors). |
| Comparison (C) | • Standard occupational health and safety practices. • Alternative wearable devices or implementation strategies. • Limited number of formal comparative analyses. |
| Outcomes (O) | • Primary: Staff safety, occupational health, stress/burnout reduction, organizational resilience, workflow efficiency. • Secondary: Absenteeism/presenteeism, productivity, adoption and satisfaction, usability, cost implications. |
| Study Design (S) | • Pilot/feasibility studies (~40%). • Observational cohort or cross-sectional (~25%). • Qualitative (~15%). • Mixed-methods (~10%). • RCTs and case studies/series (<10%). |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Virgillito, D.; Catalfo, P.; Ledda, C. Wearables in Healthcare Organizations: Implications for Occupational Health, Organizational Performance, and Economic Outcomes. Healthcare 2025, 13, 2289. https://doi.org/10.3390/healthcare13182289
Virgillito D, Catalfo P, Ledda C. Wearables in Healthcare Organizations: Implications for Occupational Health, Organizational Performance, and Economic Outcomes. Healthcare. 2025; 13(18):2289. https://doi.org/10.3390/healthcare13182289
Chicago/Turabian StyleVirgillito, Daniele, Pierluigi Catalfo, and Caterina Ledda. 2025. "Wearables in Healthcare Organizations: Implications for Occupational Health, Organizational Performance, and Economic Outcomes" Healthcare 13, no. 18: 2289. https://doi.org/10.3390/healthcare13182289
APA StyleVirgillito, D., Catalfo, P., & Ledda, C. (2025). Wearables in Healthcare Organizations: Implications for Occupational Health, Organizational Performance, and Economic Outcomes. Healthcare, 13(18), 2289. https://doi.org/10.3390/healthcare13182289







