Abstract
Background: Promoting the health of transgender and gender diverse people requires healthcare providers who are competent in gender-affirming communication and care. However, transgender health education is often absent in health professions curricula or isolated to a single course. This is partly attributed to faculty feeling unprepared to train students on key concepts in transgender health. Purpose: The purpose of this short communication is to describe the development and implementation of a novel Faculty Fellowship in Transgender Health, the outcome of which is a curricular map of integrated transgender health content in various healthcare professions. Five faculty members participated in the inaugural fellowship from the disciplines of physician assistant, nursing, athletic training, social work, and clinical psychology programs. Recommendations: By providing resources, training, and a network of peer educators, institutions can support faculty to think holistically about content relevant to transgender health and potential curricular adaptations in their respective disciplines.
1. Introduction
Transgender patients are poorly served by the United States (US) healthcare system. Nearly one in four (24%) transgender adults did not see a doctor when they needed to in the last year due to fear of mistreatment [1]. Among those who did see a healthcare provider in the past year, nearly one in two (48%) reported at least one negative experience related to their gender, such as being refused healthcare, being misgendered, having a provider use harsh or abusive language towards them, or having a provider be physically rough or abusive [1]. Lack of training in transgender health for health professional students drives the negative experiences of transgender patients [2,3]; patients reported anticipating highly negative experiences with healthcare providers, avoiding healthcare altogether, and having to educate their providers on aspects of their own care [4]. Other challenges persist related to insurance barriers and state-level restrictions on gender-affirming care [1,5].
1.1. Educational Interventions Are Often Limited
Sexual and gender minority-health related content is not required for medical school accreditation or medical student training [6,7]. Nonetheless, many educational programs have successfully modeled the efficacy of brief interventions to improve student knowledge, attitudes, beliefs, comfort, and confidence in caring for transgender clients [2,3,8,9]. Most programs have utilized lectures as an educational intervention to address this gap. Other programs included simulations, videos or films, guest speakers, reading assignments, reflective writing assignments, guided discussions, or problem-based learning, among others [2,8]. Most educational interventions have been situated within a single course [2,3] or in individual clinical supervision with trained supervisors [10]. Few studies have modeled an interprofessional education approach [11,12], despite relevant skills that intersect all healthcare professions. The lack of long-term follow-up data and varied nature of interventions further limit existing research [9]. While research supports that brief educational interventions, including as little as a one-hour lecture, may effectively improve student learning outcomes specific to transgender health [11,12], students still desire more training to feel competent in providing gender-affirming care [13].
Novel approaches have sought to integrate transgender health content throughout a curriculum, such as the Transgender Curriculum Integration Project which focused on five courses in an accelerated Bachelor’s in Nursing Science program [12,13]. Others have created an optional certificate in lesbian, gay, bisexual and transgender (LGBT) Health [14]. These developments are promising but are limited to a single discipline or are optional to students. Infusing transgender health content throughout curricula is necessary to better prepare health professionals to provide gender-affirming care for the future patients and clients [15,16].
1.2. Faculty Feel Unprepared to Deliver Transgender Health Content
Frequently cited reasons for the absence of transgender health content are that faculty feel unprepared, time-constrained by other workload demands, or under-qualified to adequately address relevant topics [2,8,17,18,19,20,21]. Other barriers include limited curricular time, poor institutional support, or a perception of irrelevance [8]. Importantly, state-level legislation banning diversity, equity, and inclusion (DEI) efforts at public institutions [22] will require faculty to think critically and creatively about how to prepare their students to provide culturally competent care for diverse populations. Thus, efforts toward faculty development, competency, and institutional support are warranted [8,17].
Scholars have studied faculty readiness [19,20] and emphasized the need for robust faculty development programs to sustainably integrate transgender health into curricula [2,8,14,15]. However, these recommendations are largely informed by the expertise of scholars in transgender health. Descriptions of actual faculty development programs, especially for faculty with little knowledge in transgender health, are largely lacking. As one example, the Transgender Curriculum Integration Project briefly described the process for contacting nursing faculty members, soliciting agreement their agreement to participate, and coaching them on how to adopt new content in their courses [14]. Detailed, robust descriptions of faculty development approaches are necessary ensure this important recommendation can be actualized in health education.
1.3. Current Recommendations for Health Professional Student Education in Transgender Health
Current recommendations for student education in transgender health emphasize the importance of integrating content throughout curricula to widely address critical topics that may naturally fit in various courses, such as gender-affirming communication, clinical assessment, and gender identity development [15,17,18,23,24]. This approach has been modeled by scholars in the fields of nursing [14,15,24], medicine [17], and athletic training [25], among others. By thinking holistically about their curricula, educators can consider how to best address relevant content at appropriate points in their curricula and integrate a range of biological, psychosocial, and clinical perspectives.
The current literature also emphasizes the value of fostering interprofessional collaboration among faculty seeking to adapt their curricula [2,17]. Faculty champions may emerge organically as they collaborate with transgender health experts in other disciplines, clinical partners, and community-based organizations [2]. Strategies to cultivate faculty collaboration include developing a health education interest directory, making informal introductions among individuals or groups with a shared interest in transgender health, or issuing institutional calls for participating in relevant projects [17].
1.4. Purpose
The purpose of this short communication is to describe the development of a Faculty Fellowship in Transgender Health and to disseminate an exemplar curricular map of transgender health content across multiple healthcare professions.
2. Faculty Fellowship in Transgender Health: Development and Implementation
The Transgender Health Collaborative at Saint Louis University is a network of faculty researchers, educators, and clinicians working with the transgender community throughout Saint Louis University and community organizations. Our core team consists of non-binary and cisgender faculty from marital and family therapy, medicine, and nutrition and dietetics.
We developed a Faculty Fellowship in Transgender Health designed for educators in a broad spectrum of health professions, including allied health, mental health, and behavioral health disciplines. The purpose was to support faculty members in healthcare disciplines seeking to advance the inclusion of transgender and gender diverse identities within their courses and across their curricula.
Five faculty members were invited to participate in the fellowship program. We elected to invite faculty to represent a range of disciplines and who had previously worked with the Transgender Health Collaborative at Saint Louis University and therefore were likely to be enthusiastic about the opportunity. We also sought to include faculty who were serving in leadership roles given the recommendation to catalyze interest from curriculum developers [17]. The five faculty members were from the physician assistant, nursing, athletic training, social work, and clinical psychology programs. Three fellows were also program directors (physician assistant, athletic training, social work), and one was a director of clinical services (clinical psychology). Faculty fellows were remunerated with a stipend. The fellowship was supported through a grant from the Josiah Macy Jr. Foundation.
2.1. Four Components of the Faculty Fellowship in Transgender Health
The Faculty Fellowship in Transgender Health consisted of four components throughout the fall semester (Figure 1). The fellowship was limited to one semester given the challenge of working with time-constrained faculty and the subsequent recommendation to avoid overburdening individuals [17].
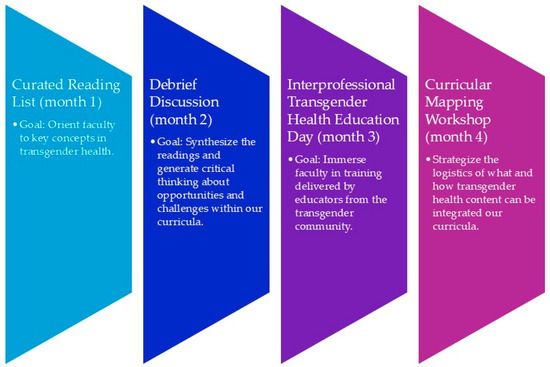
Figure 1.
Four elements of the faculty fellowship in transgender health.
First, we provided fellows with a curated reading list that included selected publications from the field of transgender health more broadly, as well as those germane to their disciplines. All fellows were assigned to read My Child is Trans, Now What? A Joy-Centered Approach to Support by Ben Greene, a St. Louis-based author and educator. Fellows were also assigned to read a resource authored by the Transgender Health Collaborative at Saint Louis University titled “Advancing Inclusion of Transgender & Gender Diverse Identities in Clinical Education: A Toolkit for Clinical Educators” [23]. The remaining assigned readings included position statements, commentaries, and additional learning resources (Table 1).

Table 1.
Reading list for five faculty fellows.
Second, we hosted a 90 min lunch discussion where we debriefed on the readings and reflected on challenges and opportunities to better integrate transgender health content in our curricula (Table 2). Third, all fellows participated in the 2024 Interprofessional Transgender Health Education Day. This is a full-day training on introductory concepts in transgender health and gender-affirming communication and care. The learning objectives, session descriptions, and outcomes of this training have been reported previously [33].

Table 2.
Debrief discussion guide for the faculty fellowship in transgender health.
Fourth, we hosted a second 90 min lunch workshop where we discussed what we learned from the Interprofessional Transgender Health Education Day and began developing a curricular map of how we could better integrate transgender health content in our respective curricula (Table 3). We also incorporated our own disciplines (nutrition and dietetics and marital and family therapy) into the work as an opportunity to improve our own curricula and work alongside the faculty fellows. Faculty were given three additional weeks to complete the curricular mapping after the workshop, the outcomes of which are detailed in the next section.

Table 3.
Discussion guide for the curricular mapping workshop of the faculty fellowship in transgender health.
2.2. Integration of Concepts in Transgender Health Throughout Health Professions Curricula
Supplementary File S1 depicts the curricular map of key concepts in transgender health in our respective disciplines. The Fellows first determined the key concepts in transgender health that should be reflected in a health professions curriculum, which were also informed by the current literature. These included seven concepts: Gender identity development [17]; gender minority populations [14,15]; historical and social context of transgender people [8,14,15,17]; legal, policy, and ethical implications for transgender people [8,14,15]; counseling and communication skills with transgender clients [14,17]; practicum and simulation with transgender patients or clients [8]; and research methods and sex, sexual orientation, and gender identity (SOGI) data [17]. The seven broad concepts invited an intersectional approach to consider a range of life experiences such as race, ethnicity, education, income level, and social class [34]. For example, the concept of “historical and social context of transgender people” could be applied to educate students on differences within the transgender population, such as the higher rates of poverty, homelessness, and violence experienced by transgender people of color [1].
Fellows were challenged to identify courses, learning objectives, readings, and learning activities for each key concept (Supplementary File S1). They were encouraged to think about a curriculum in their field more broadly, rather than the specific program in place for their discipline at Saint Louis University, to support generalizability of the curricular map to various institutions. Fellows were also encouraged to focus only on their ideas for the ideal content, rather than the logistics of who, when, and how the content would be operationalized.
3. Discussion and Future Directions
The Fellows successfully identified multiple courses in their disciplines to deliver each key concept (Supplementary File S1). For example, the concept of gender identity development could be taught in a Lifespan Development and/or a Human Diversity Course within a clinical psychology program. This underpins the flexible nature of how curricula may be adapted at different institutions according to faculty strengths, time, and desire. In addition, the Fellows identified readings and learning activities that could be readily utilized by other healthcare disciplines. For example, a proposed learning activity from the nursing fellow involved critically evaluating a nursing research study to assess how the researchers collected SOGI data and identifying potential improvements in data collection practices. This exercise could be adapted for any healthcare discipline by using an article relevant to their field. Thus, even if an academic program was not prepared to adapt their entire curriculum, components could still be utilized on a smaller scale, such as new readings, case studies, or learning objectives in a single course.
Successful implementation of the curricular map will require stakeholder buy-in from the faculty and administration in the respective programs. Faculty members would need to make changes to their courses such as adding or modifying the course objectives, incorporating new assignments and reading materials, and developing evaluation methods for new assignments [14]. This requires both curricular time and faculty time, which are known challenges to incorporating transgender health content [17]. A potential risk is that some faculty members would readily make changes to their courses, while others would not, thus creating a possible fracturing in how the content is presented cohesively and consistently across the curriculum. This risk could be ameliorated by clear and tangible support from university leaders, such as provosts, deans, department chairs, and program directors, as well as accrediting bodies who actively influence the curriculum. Notably, curricular adaptation on a smaller scale, such as one or two courses with updated reading materials, would still be an improvement from a dearth of transgender health content.
In addition, successful implementation would require faculty to update content somewhat frequently given the rapidly evolving nature of transgender health research [35]. Faculty support would be needed to ensure the content is up to date, such as access to high quality continuing education, subscription to relevant journals in the university library, and connections to peer colleagues engaged in similar work [2,17]. While continuing education requirements of all healthcare professionals create opportunities to obtain up-to-date transgender health information, providers may feel challenged to balance this need with other ongoing field-specific requirements for continuing education credits (CEUs).
Successful implementation would also require approaches to ensure stability of the content in the curriculum, which may be challenged by faculty turnover or reassignment to different courses. Realistically, when a complete curricular change is unrealistic or unsupported, content may still be championed by one or two faculty members. Methods could include a “warm hand-off” from one faculty member to the next with the sharing of readings, assignments, or guest speakers, integration of the content within program learning outcomes that may be regularly assessed and reported, and clear alignment with competencies determined by the accrediting body of health profession education programs.
Lastly, faculty expertise around transgender healthcare may become clustered within certain departments of healthcare professions at teaching institutions, as faculty may naturally collaborate more frequently with those within their discipline or department. Scholars have recommended strategies to foster intellectual exchange and collaboration related to transgender health more broadly, such as institution-wide participation calls, informal introductions, or a transgender health education interest directory [17]. In our experience, the formation of a “collaborative,” or essentially, a network of faculty formally recognized by the university, has led to rich and interdisciplinary collaboration in our research, teaching, and clinical practice [36]. The interprofessional nature of the Faculty Fellowship in Transgender Health allowed expert faculty to provide training across professional and institutional divides, thus strengthening trainee education in transgender healthcare for the institution as a whole.
Limitations
This short communication describes the development and implementation of a novel program rather than a traditional research study. As such, inherent limitations included the lack of measurable outcomes; future research may explore outcomes related to faculty experiences, teaching evaluations, and student reception of new content. Furthermore, this fellowship was implemented at a single institution with five faculty members and therefore may not be generalizable to institutions of other sizes, regions, or public versus private affiliation. Institutions may need to consider what adaptations would make a faculty fellowship program successful at their unique institution.
4. Conclusions
Development and implementation of a Faculty Fellowship in Transgender Health was an important capacity-building step towards better incorporating transgender health in various curricula. By providing resources, training, and a network of peer educators, faculty were supported to think holistically about relevant content and curricular adaptations. While challenges will persist such as faculty buy-in and turnover, this model offers a promising approach to build faculty competency and foster collaboration. This fellowship required relatively limited time commitments from faculty across only one semester, making it more feasible for faculty participation. As this short communication describes development and implementation of a new program, future research can systematically evaluate outcomes of interest, such as faculty experiences and student learning. Ultimately, integration of transgender health content throughout curricula is essential to ensure that the next generation of healthcare professionals are equipped to deliver excellent care for their future patients and clients.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare13172124/s1. File S1: Curricular Map of Transgender Health Content Throughout Seven Health Professions.
Author Contributions
Conceptualization, W.R.L. and K.H.-R.; writing—original draft preparation, W.R.L. and K.H.-R.; writing—review and editing, M.R.D., R.R., T.D., L.B., G.D.R., K.S., A.D.S., K.R. and R.H.; project administration, W.R.L. and K.H.-R.; funding acquisition, W.R.L., K.H.-R., M.R.D. and T.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Josiah Macy Jr. Foundation, grant number P24-07.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| US | United States |
| LGBT | Lesbian, gay, bisexual and transgender |
| DEI | Diversity, equity and inclusion |
| APA | American Psychological Association |
| LGBTQIA+ | Lesbian, gay, bisexual, transgender, queer, intersex, asexual plus |
| SOGI | Sex, sexual orientation, and gender identity |
| CEUs | Continuing education units |
References
- James, S.E.; Herman, J.L.; Durso, L.E.; Heng-Lehtinen, R. Early Insights: A Report of the 2022 U.S. Transgender Survey; National Center for Transgender Equality: Washington, DC, USA, 2024; Available online: https://transequality.org/sites/default/files/2024-02/2022%20USTS%20Early%20Insights%20Report_FINAL.pdf (accessed on 20 August 2025).
- Lim, F.; Eda, O.S. Methods of teaching transgender health in undergraduate nursing programs: A narrative review. Nurse Educ. 2024, 49, 130–136. [Google Scholar] [CrossRef]
- Tanenbaum, G.J.; Holden, L.R. A review of patient experiences and provider education to improve transgender health inequities in the USA. Int. J. Environ. Res. Public Health 2023, 20, 6949. [Google Scholar] [CrossRef]
- Heiden-Rootes, K.; Meyer, D.; Sledge, R.; Davis, B.K.; Drallmeier, T.; Linsenmeyer, W.; Levine, S.; Dalton, M.R. Seeking gender-affirming medical care: A phenomenological inquiry on skillful coping with transgender and non-binary adults in the United States Midwest. Qual. Res. Med. Healthc. 2023, 7, 11485. [Google Scholar] [CrossRef]
- American Civil Liberties Union. The ACLU is Tracking 574 Anti-LGBTQ Bills in the U.S. 6 December 2024. Available online: https://www.aclu.org/legislative-attacks-on-lgbtq-rights-2024 (accessed on 20 August 2025).
- Fitzgerald, B.; Terndrup, C.; Streed, C.G.; Lee, R.S., Jr.; Patel, V.V.; Nall, R. Prepared on behalf of the SGIM LGBTQ+ Interest Group the Society of General Internal Medicine’s Recommendations to Improve LGBTQ + Health. J. Gen. Intern. Med. 2024, 39, 323–330. [Google Scholar] [CrossRef]
- Streed, C.G.; Siegel, J.; Davis, J.A. Keeping Our Promise to LGBTQ+ Patients; Association of American Medical Colleges: Washington, DC, USA, 2019; Available online: https://www.aamc.org/news/viewpoints/keeping-our-promise-lgbtq-patients (accessed on 20 August 2025).
- Dubin, S.N.; Nolan, I.T.; Streed, C.G.; Greene, R.E., Jr.; Radix, A.E.; Morrison, S.D. Transgender health care: Improving medical students’ and residents’ training and awareness. Adv. Med. Educ. Pract. 2018, 9, 377–391. [Google Scholar] [CrossRef]
- Nolan, I.T.; Blasdel, G.; Dubin, S.N.; Goetz, L.G.; Greene, R.E.; Morrison, S.D. Current State of Transgender Medical Education in the United States and Canada: Update to a Scoping Review. J. Med. Educ. Curric. Dev. 2020, 7, 2382120520934813. [Google Scholar] [CrossRef]
- Dalton, M.R.; Veasey, A.W.; Norton, A.M. Supervising with a feminist lens: Improving transgender competency. Contemp. Fam. Ther. 2022, 44, 397–407. [Google Scholar] [CrossRef]
- Allison, M.K.; Marshall, S.A.; Archie, D.S.; Neher, T.; Stewart, G.; Anders, M.E.; Stewart, M.K. Community-engaged development, implementation, and evaluation of an interprofessional education workshop on gender-affirming care. Transgender Health 2019, 4, 280–286. [Google Scholar] [CrossRef]
- Hudson, H.; Scheidler, B.; Cremer, K.; Wright, L. Utilizing interprofessional education to foster diversity, equity, and inclusion concepts related to gender affirming care. J. Interprof. Educ. Pract. 2024, 34, 100691. [Google Scholar] [CrossRef]
- Linsenmeyer, W.; Heiden-Rootes, K.; Drallmeier, T.; Rahman, R.; Buxbaum, E.; Walcott, K.; Rosen, W.; Gombos, B.E. The power to help or harm: Student perceptions of transgender health education using a qualitative approach. BMC Med. Educ. 2023, 23, 836. [Google Scholar] [CrossRef]
- McDowell, A.; Bower, K.M. Transgender health care for nurses: An innovative approach to diversifying nursing curricula to address health inequities. J. Nurs. Educ. 2016, 55, 476–479. [Google Scholar] [CrossRef] [PubMed]
- Sherman, A.D.F.; McDowell, A.; Clark, K.D.; Balthazar, M.; Klepper, M.; Bower, K. Transgender and gender diverse health education for future nurses: Students’ knowledge and attitudes. Nurse Educ. Today 2021, 97, 104690. [Google Scholar] [CrossRef]
- Sawning, S.; Steinbock, S.; Croley, R.; Combs, R.; Shaw, A.; Ganzel, T. A first step in addressing medical education Curriculum gaps in lesbian-, gay-, bisexual-, and transgender-related content: The University of Louisville Lesbian, Gay, Bisexual, and Transgender Health Certificate Program. Educ. Health 2017, 30, 108–114. [Google Scholar] [CrossRef]
- Solotke, M.; Sitkin, N.A.; Schwartz, M.L.; Encandela, J.A. Twelve tips for incorporating and teaching sexual and gender minority health in medical school curricula. Med. Teach. 2019, 41, 141–146. [Google Scholar] [CrossRef]
- Hana, T.; Butler, K.; Young, L.T.; Zamora, G.; Lam, J.S.H. Transgender health in medical education. Bull. World Health Organ. 2021, 99, 296–303. [Google Scholar] [CrossRef]
- Lim, R.; Johnson, M.; Eliason, M. A national survey of faculty knowledge, experience, and readiness for teaching lesbian, gay, bisexual, and transgender health in baccalaureate nursing programs. Nurs. Educ. Perspect. 2015, 36, 144–152. [Google Scholar] [CrossRef]
- Nye, C.M.; Livingston, J.A.; Foltz-Ramos, K.; Hequembourg, A. Undergraduate nursing faculty knowledge, beliefs, and experiences with teaching LGBTQ+ content: A scoping review. J. Prof. Nurs. Off. J. Am. Assoc. Coll. Nurs. 2024, 54, 205–215. [Google Scholar] [CrossRef]
- Rolls, J.; Davis, J.; Backman, R.; Wood, T.; Honda, T. Curricular approaches to transgender health in physician assistant education. Acad. Med. J. Assoc. Am. Med. Coll. 2020, 95, 1563–1569. [Google Scholar] [CrossRef]
- Gretzinger, E.; Hicks, M.; Dutton, C.; Smith, J. Tracking higher ed’s dismantling of DEI. The Chronicle of Higher Education. 13 December 2024. Available online: https://www.chronicle.com/article/tracking-higher-eds-dismantling-of-dei (accessed on 20 August 2025).
- Linsenmeyer, W.; Heiden-Rootes, K.; Drallmeier, T.; Rahman, R.; Buxbaum, E.; Rosen, W.; Gombos, B.; Otte, A. Advancing inclusion of transgender and gender-diverse identities in clinical education: A toolkit for clinical educators. Health Promot. Pract. 2024, 25, 741–743. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, E.; Luctkar-Flude, M.; Carroll, B.; Tyerman, J.; Chumbley, L.; Shortall, C. Development of an online educational toolkit for sexual orientation and gender identity minority nursing care. Rev. Lat.-Am. De Enferm. 2021, 29, e3470. [Google Scholar] [CrossRef]
- Schulman, E.H.; Eberman, L.E.; Crossway, A.K.; Nye, E.A.; Uriegas, N.A.; Connell, S.A.; Winkelmann, Z.K. Integration of an inclusive health care curriculum for sexual health and gender minorities. Athl. Train. Educ. J. 2022, 17, 251–261. [Google Scholar] [CrossRef]
- National LGBTQIA+ Health Education Center. Learning Resources–Transgender Health. 2024. Available online: https://www.lgbtqiahealtheducation.org/resources/in/transgender-health/ (accessed on 20 August 2025).
- American Nursing Association Ethics Advisory Board. ANA position statement: Nursing advocacy for LGBTQ+ populations. Online J. Issues Nurs. 2018, 24, 1–6. [Google Scholar] [CrossRef]
- Rogers, S.M.; Lopez, R.M.; Crossway, A.K.; Moffit, D.M.; Sturtevant, J.; Hansen, A. The Role of the athletic trainer in providing care to transgender and gender-diverse patients: Foundational knowledge and disparities–Part I. J. Athl. Train. 2024, 59, 338–344. [Google Scholar] [CrossRef]
- Crossway, A.K.; Rogers, S.M.; Hansen, A.; Sturtevant, J.; Moffit, D.M.; Lopez, R.M. The Role of the athletic trainer in providing care to transgender and gender-diverse patients: Considerations for medical affirmation–Part II. J. Athl. Train. 2024, 59, 345–353. [Google Scholar] [CrossRef]
- American Psychological Association. APA Policy Statement on Affirming Evidence-Based Inclusive Care for Transgender, Gender Diverse, and Nonbinary Individuals, Addressing Misinformation, and the Role of Psychological Practice and Science. 2024. Available online: https://www.apa.org/about/policy/transgender-nonbinary-inclusive-care.pdf (accessed on 20 August 2025).
- National Association of Social Workers. LGBTQIA2S+. 2024. Available online: https://www.socialworkers.org/Practice/LGBT (accessed on 20 August 2025).
- Greene, B. My Child is Trans, Now What? A Joy-Centered Approach to Support; Rowman Littlefield Publishers: Lanham, MD, USA, 2024. [Google Scholar]
- Linsenmeyer, W.; Stiles, D.; Drallmeier, T.; Heiden-Rootes, K.; Rahman, R.; Buxbaum, E.; Gombos, B.; Harris, N.; Johnson, S.; Lantz, C.; et al. Advancing inclusion of transgender identities in health professional education programs: The interprofessional transgender health education day. J. Allied Health 2023, 52, 24–31. [Google Scholar]
- Crenshaw, K. Mapping the margins: Intersectionality, identity politics, and violence against women of color. Stanf. Law Rev. 1991, 43, 1241–1299. [Google Scholar] [CrossRef]
- Coleman, E.; Radix, A.E.; Bouman, W.P.; Brown, G.R.; de Vries, A.L.C.; Deutsch, M.B.; Ettner, R.; Fraser, L.; Goodman, M.; Green, J.; et al. Standards of care for the health of transgender and gender diverse people, version 8. Int. J. Transgender Health 2022, 23, S1–S259. [Google Scholar] [CrossRef]
- Saint Louis University. Transgender Health Collaborative at Saint Louis University; Saint Louis University: Saint Louis, MO, USA, 2024; Available online: https://www.slu.edu/doisy/clinics-and-community/transgender-health-collaborative.php (accessed on 20 August 2025).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).