Home Physical Exercise Interventions in Chronic Non-Specific Low Back Pain: Systematic Review and Multivariate Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
- Population: Adult population (>18 years), experiencing NSCLBP, of three months or more of evolution. Therefore, all types of traumatic LBP and those due to specific pathologies (spondylolisthesis, stenosis, infectious and/or inflammatory processes, tumors, neurological conditions, etc.) were excluded.
- Intervention: Prescription of physical exercise exclusively at home/online (unsupervised or supervised via video). This intervention could include and even combine different modalities of physical exercise, but it could not include or be compared with other therapeutic approaches.
- Comparator/control: The comparator group must adhere to the same physical exercise prescription as the intervention group, but with supervision provided exclusively through face-to-face/in-person sessions. This approach ensures that any observed differences between groups can be attributed solely to the mode of exercise supervision (supervised versus unsupervised), rather than variations in the exercise program or type of exercise performed. Additionally, the control group may include participants receiving general advice or counseling on physical activity, exercise, and ergonomics or those maintaining their usual activities of daily living without any specific intervention.
- Outcomes: Pain intensity and functional disability. No particular scale or questionnaire was designated to quantify these outcomes.
- Study design: Only randomized clinical trials (RCTs) published in English or Spanish. Therefore, any other type of clinical trial was excluded. Reviews or meta-analyses, book sections, conference abstracts, and protocols were also excluded.
2.2. Data Sources and Search
2.3. Study Selection
2.4. Data Extraction Process
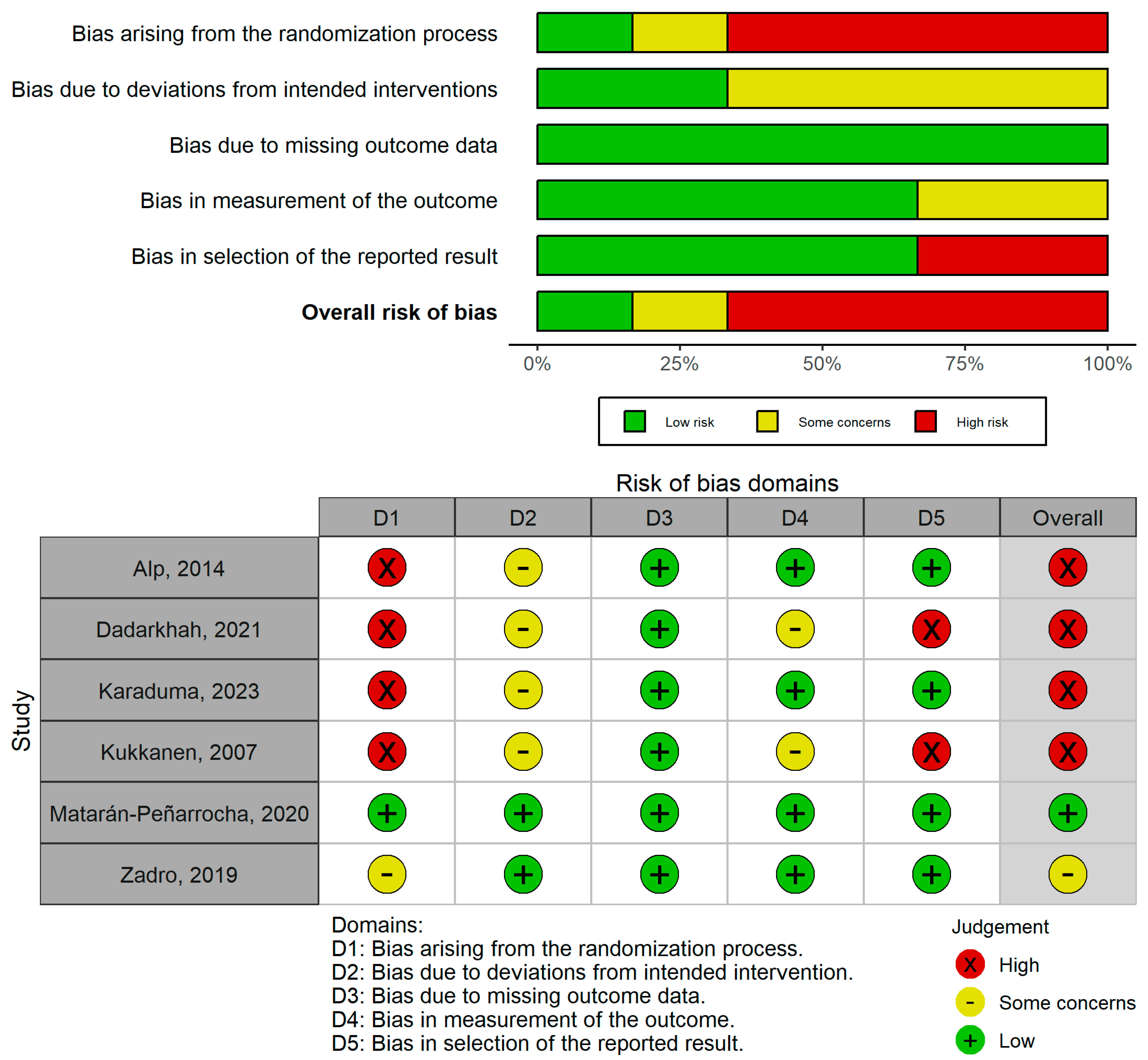
2.5. Assessment of Methodological Quality and Risk of Bias
2.6. Statistical Analysis
3. Results
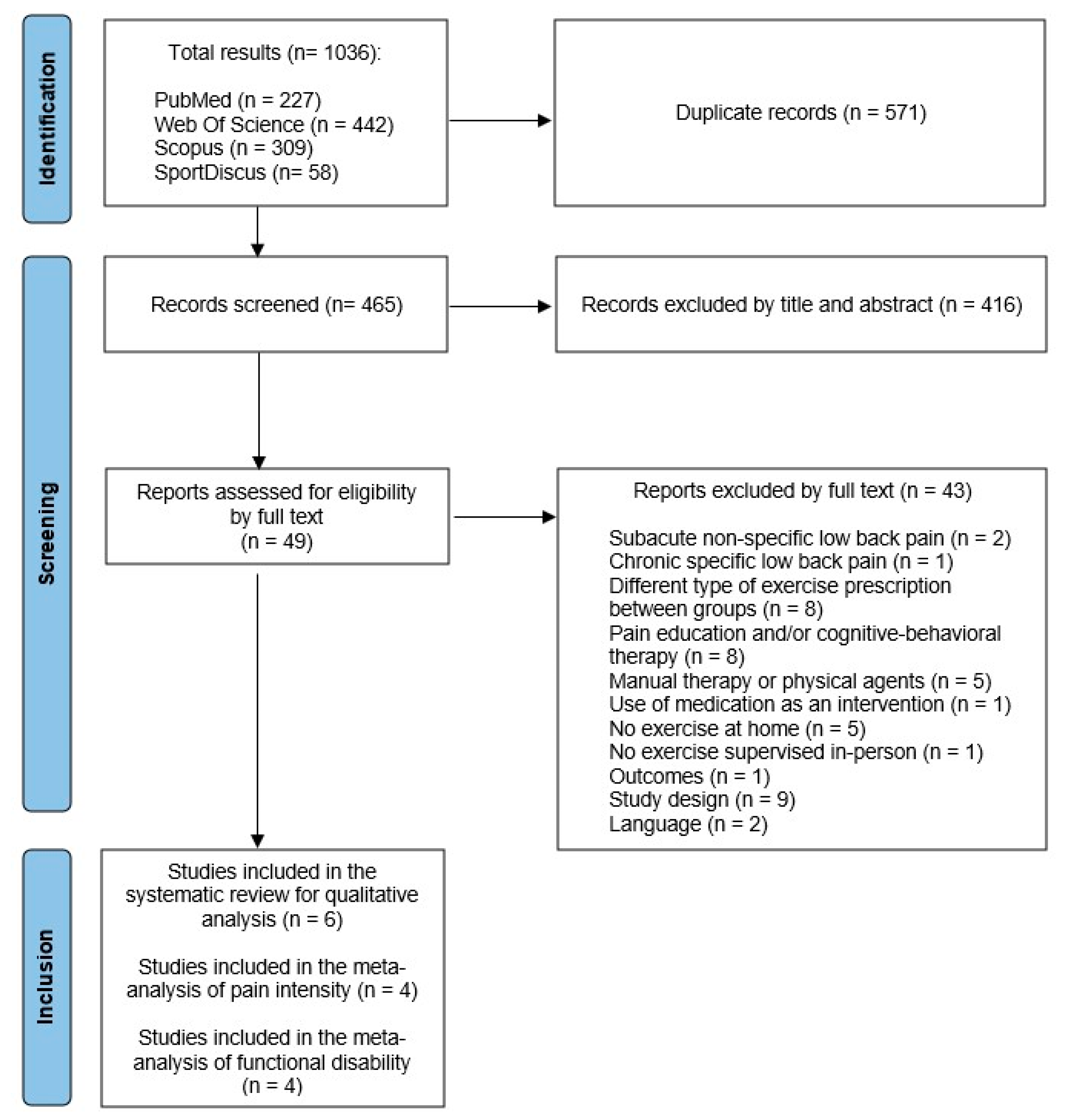
3.1. Study Selection
3.2. Study Characteristics
3.2.1. Sample Size and Characteristics
3.2.2. Design of the Groups and Description of the Intervention
3.2.3. Outcomes and Follow-Up
3.3. Methodological Quality and Risk of Bias
3.4. Review Results
3.4.1. Unsupervised Home Physical Exercise vs. Supervised In-Person Physical Exercise
3.4.2. Unsupervised Home Physical Exercise vs. No Intervention
3.4.3. Unsupervised Home Physical Exercise vs. Tele-Supervised Home Physical Exercise
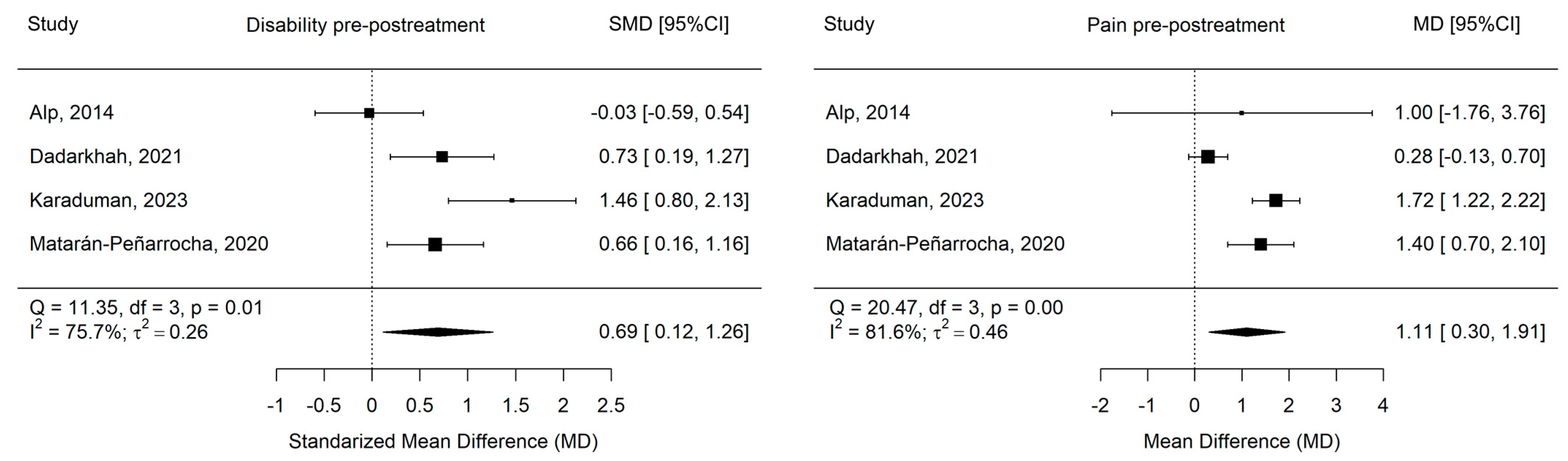
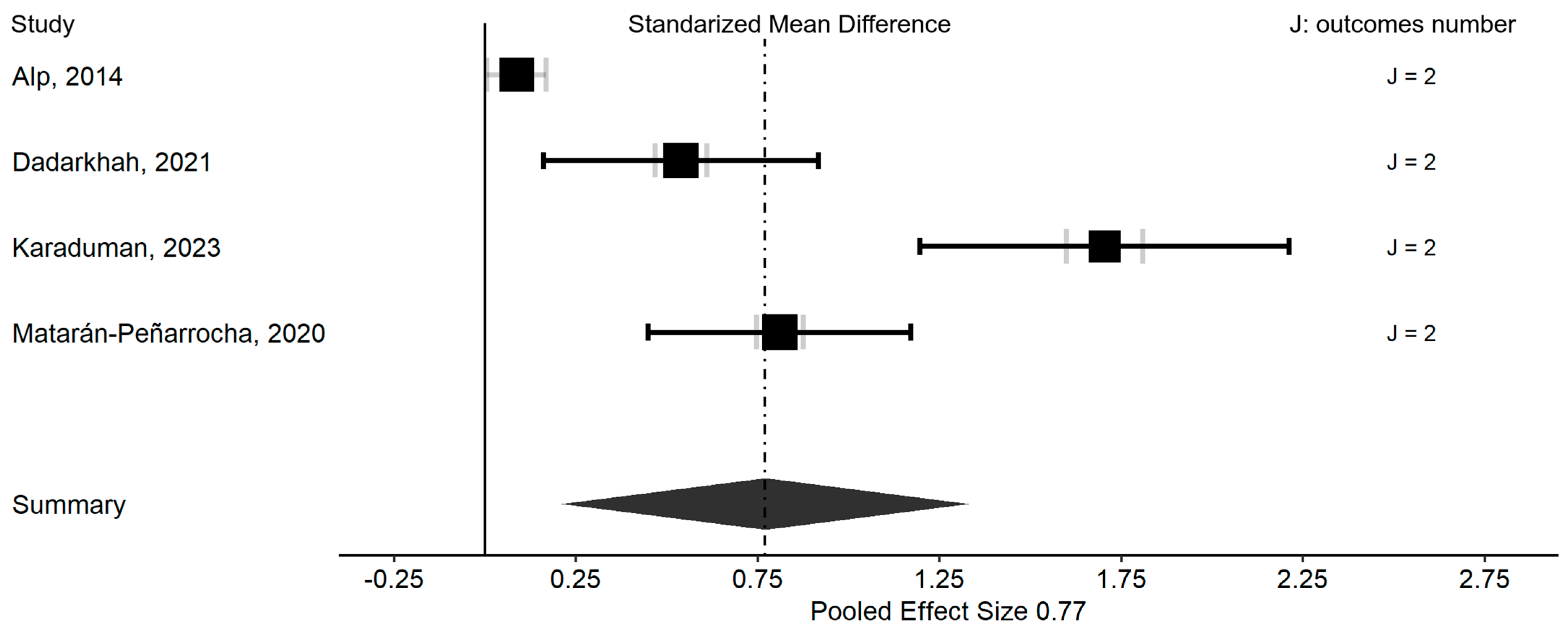
3.5. Meta-Analysis Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AIC | Akaike information coefficient |
| BMI | Body mass index |
| FTSTS | Five-times sit-to-stand test |
| LBP | Low back pain |
| LRT | Likelihood ratio test |
| MD | Mean difference |
| MMA | Multivariate meta-analysis |
| NRS | Numeric rating scale |
| NSCLBP | Non-specific chronic low back pain |
| ODI | Oswestry disability index |
| PRISMA | Preferred reporting items for systematic reviews and meta-analyses |
| PSFS | Patient-specific functional scale |
| RCT | Randomized controlled trial |
| RMDQ | Roland–Morris disability questionnaire |
| SMD | Standardized mean difference |
| VAS | Visual analogue scale |
References
- GBD 2021 Low Back Pain Collaborators. Global, regional, and national burden of low back pain, 1990–2020, its attributable risk factors, and projections to 2050: A systematic analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol. 2021, 5, e316–e329. [Google Scholar] [CrossRef]
- Wang, H.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abera, S.F.; Abraha, H.N.; Abu-Raddad, L.J.; Abu-Rmeileh, N.M.E.; et al. Global, Regional, and National under-5 Mortality, Adult Mortality, Age-Specific Mortality, and Life Expectancy, 1970–2016: A Systematic Analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1084–1150. [Google Scholar] [CrossRef]
- Herman, P.M.; Broten, N.; Lavelle, T.A.; Sorbero, M.E.; Coulter, I.D. Exploring the Prevalence and Construct Validity of High-Impact Chronic Pain Across Chronic Low-Back Pain Study Samples. Spine J. 2019, 19, 1369–1377. [Google Scholar] [CrossRef]
- World Physiotherapy. World PT Day. Available online: https://world.physio/wptday (accessed on 15 January 2025).
- Chou, R.; Shekelle, P. Will This Patient Develop Persistent Disabling Low Back Pain? J. Am. Med. Assoc. 2010, 303, 1295–1302. [Google Scholar] [CrossRef] [PubMed]
- Karoliina, L.; Maria, L.; Juhani, M. Prognostic Factors for Pain Chronicity in Low Back Pain: A Systematic Review. PAIN Rep. 2021, 6, e919. [Google Scholar] [CrossRef]
- Junqueira, D.R.G.; Ferreira, M.L.; Refshauge, K.; Maher, C.G.; Hopper, J.L.; Hancock, M.; Carvalho, M.G.; Ferreira, P.H. Heritability and Lifestyle Factors in Chronic Low Back Pain: Results of the Australian Twin Low Back Pain Study (The AUTBACK Study). Eur. J. Pain 2014, 18, 1410–1418. [Google Scholar] [CrossRef] [PubMed]
- Geneen, L.J.; Moore, R.A.; Clarke, C.; Martin, D.; Colvin, L.A.; Smith, B.H. Physical Activity and Exercise for Chronic Pain in Adults: An Overview of Cochrane Reviews. Cochrane Database Syst. Rev. 2017, 4, CD011279. [Google Scholar] [CrossRef] [PubMed]
- Hayden, J.A.; Ellis, J.; Ogilvie, R.; Malmivaara, A.; van Tulder, M.W. Exercise Therapy for Chronic Low Back Pain. Cochrane Database Syst. Rev. 2021, 9, CD009790. [Google Scholar] [CrossRef]
- Koes, B.W.; Van Tulder, M.; Lin, C.-W.C.; Macedo, L.G.; Mcauley, J.; Maher, C. An Updated Overview of Clinical Guidelines for the Management of Non-Specific Low Back Pain in Primary Care. Eur. Spine J. 2010, 19, 2075–2094. [Google Scholar] [CrossRef]
- Oliveira, C.B.; Maher, C.G.; Pinto, R.Z.; Traeger, A.C.; Lin, C.W.C.; Chenot, J.F.; van Tulder, M.; Koes, B.W. Clinical Practice Guidelines for the Management of Non-Specific Low Back Pain in Primary Care: An Updated Overview. Eur. Spine J. 2018, 27, 2791–2803. [Google Scholar] [CrossRef]
- Garg, S.; Garg, D.; Turin, T.C.; Chowdhury, M.F.U. Web-Based Interventions for Chronic Back Pain: A Systematic Review. J. Med. Internet Res. 2016, 18, e139. [Google Scholar] [CrossRef]
- Palazzo, C.; Klinger, E.; Dorner, V.; Kadri, A.; Thierry, O.; Boumenir, Y.; Martin, W.; Poiraudeau, S.; Ville, I. Barriers to Home-Based Exercise Program Adherence with Chronic Low Back Pain: Patient Expectations Regarding New Technologies. Ann. Phys. Rehabil. Med. 2016, 59, 107–113. [Google Scholar] [CrossRef]
- Bailey, J.F.; Agarwal, V.; Zheng, P.; Smuck, M.; Fredericson, M.; Kennedy, D.J.; Krauss, J. Digital Care for Chronic Musculoskeletal Pain: 10,000 Participant Longitudinal Cohort Study. J. Med. Internet Res. 2020, 22, e18250. [Google Scholar] [CrossRef] [PubMed]
- Quentin, C.; Bagheri, R.; Ugbolue, U.C.; Coudeyre, E.; Pélissier, C.; Descatha, A.; Menini, T.; Bouillon-Minois, J.B.; Dutheil, F. Effect of Home Exercise Training in Patients with Nonspecific Low-Back Pain: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 8430. [Google Scholar] [CrossRef] [PubMed]
- Sivertsson, J.; Sernert, N.; Åhlund, K. Exercise-based telerehabilitation in chronic low back pain—A scoping review. BMC Musculoskelet. Disord. 2024, 25, 948. [Google Scholar] [CrossRef] [PubMed]
- Mehendale, P.; Iyenagar, M.; Bhatt, G.; Manwadkar, S. Virtually Administered Intervention Through Telerehabilitation for Chronic Non-specific Low Back Pain: A Review of Literature. Cureus 2023, 15, e42942. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro Scale for Rating Quality of Randomized Controlled Trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef]
- Albanese, E.; Egger, M.; Bütikofer, L.; Armijo-olivo, S.; Ha, C. Construct Validity of the Physiotherapy Evidence Database (PEDro) Quality Scale for Randomized Trials: Item Response Theory and Factor Analyses. Res. Synth. Methods 2020, 11, 227–236. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, I4898. [Google Scholar] [CrossRef]
- Luo, D.; Wan, X.; Liu, J.; Tong, T. Optimally Estimating the Sample Mean from the Sample Size, Median, Mid-Range, and/or Mid-Quartile Range. Stat. Methods Med. Res. 2018, 27, 1785–1805. [Google Scholar] [CrossRef]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the Sample Mean and Standard Deviation from the Sample Size, Median, Range and/or Interquartile Range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef]
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welch, V. Cochrane Handbook for Systematic Reviews of Interventions, Version 6.3 (Updated February 2022); Cochrane: Cochrane, AB, Canada, 2022. Available online: https://training.cochrane.org/handbook (accessed on 20 March 2025).
- Drevon, D.; Fursa, S.R.; Malcolm, A.L. Intercoder Reliability and Validity of WebPlotDigitizer in Extracting Graphed Data. Behav. Modif. 2017, 41, 323–339. [Google Scholar] [CrossRef]
- Rosenthal, R. Meta-Analytic Procedures for Social Research; Sage Publications: Newbury Park, CA, USA, 1993. [Google Scholar]
- Berlim, M.T.; McGirr, A.; Rodrigues dos Santos, N.; Tremblay, S.; Martins, R. Efficacy of Theta Burst Stimulation (TBS) for Major Depression: An Exploratory Meta-Analysis of Randomized and Sham-Controlled Trials. J. Psychiatr. Res. 2017, 90, 102–109. [Google Scholar] [CrossRef]
- Kallapiran, K.; Koo, S.; Kirubakaran, R.; Hancock, K. Review: Effectiveness of Mindfulness in Improving Mental Health Symptoms of Children and Adolescents: A Meta-Analysis. Child Adolesc. Ment. Health 2015, 20, 182–194. [Google Scholar] [CrossRef]
- McGirr, A.; Berlim, M.T.; Bond, D.J.; Neufeld, N.H.; Chan, P.Y.; Yatham, L.N.; Lam, R.W. A Systematic Review and Meta-Analysis of Randomized Controlled Trials of Adjunctive Ketamine in Electroconvulsive Therapy: Efficacy and Tolerability. J. Psychiatr. Res. 2015, 62, 23–30. [Google Scholar] [CrossRef]
- Papadopoulos, V.P.; Apergis, N.; Filippou, D.K. Nocturia in CPAP-Treated Obstructive Sleep Apnea Patients: A Systematic Review and Meta-Analysis. SN Compr. Clin. Med. 2020, 2, 2799–2807. [Google Scholar] [CrossRef]
- Yagiz, G.; Akaras, E.; Kubis, H.P.; Owen, J.A. The Effects of Resistance Training on Architecture and Volume of the Upper Extremity Muscles: A Systematic Review of Randomised Controlled Trials and Meta-Analyses. Appl. Sci. 2022, 12, 1593. [Google Scholar] [CrossRef]
- Karaduman, C.; Ataş Balci, L. The Effects of In-Person-Supervised, Tele-Supervised, and Unsupervised Stabilization Exercises on Pain, Functionality, and Kinesiophobia in Patients with Chronic Low Back Pain: A Randomized, Single-Blind Trial. Physiother. Theory Pract. 2023, 40, 2492–2502. [Google Scholar] [CrossRef]
- Kersten, R.F.M.R.; Fikkers, J.; Wolterbeek, N.; Öner, F.C.; Van Gaalen, S.M. Are the Roland Morris Disability Questionnaire and Oswestry Disability Index Interchangeable in Patients after Lumbar Spinal Fusion? J. Back Musculoskelet. Rehabil. 2021, 34, 605–611. [Google Scholar] [CrossRef]
- Bielewicz, J.; Daniluk, B.; Kamieniak, P. VAS and NRS, Same or Different? Are Visual Analog Scale Values and Numerical Rating Scale Equally Viable Tools for Assessing Patients after Microdiscectomy? Pain Res. Manag. 2022, 2022, 5337483. [Google Scholar] [CrossRef]
- Varma, V.R.; Dey, D.; Leroux, A.; Di, J.; Urbanek, J.; Xiao, L.; Zipunnikov, V. Re-evaluating the effect of age on physical activity over the lifespan. Prev. Med. 2017, 101, 102–108. [Google Scholar] [CrossRef]
- Hemmingsson, E.; Ekelund, U. Is the association between physical activity and body mass index obesity dependent? Int. J. Obes. 2007, 31, 663–668. [Google Scholar] [CrossRef]
- Fernández-Castilla, B.; Declercq, L.; Jamshidi, L.; Beretvas, S.N.; Onghena, P.; van den Noortgate, W. Visual Representations of Meta-Analyses of Multiple Outcomes: Extensions to Forest Plots, Funnel Plots, and Caterpillar Plots. Methodology 2020, 16, 299–315. [Google Scholar] [CrossRef]
- Alp, A.; Mengi, G.; Avşaroǧlu, A.H.; Mert, M.; Siǧirli, D. Efficacy of Core-Stabilization Exercise and Its Comparison with Home-Based Conventional Exercise in Low Back Pain Patients. Turk. J. Phys. Med. Rehabil. 2014, 60, S36–S42. [Google Scholar] [CrossRef]
- Dadarkhah, A.; Rezaimoghadam, F.; Najafi, S.; Mohebi, B.; Azarakhsh, A.; Rezasoltani, Z. Remote Versus In-Person Exercise Instruction for Chronic Nonspecific Low Back Pain Lasting 12 Weeks or Longer: A Randomized Clinical Trial. J. Natl. Med. Assoc. 2021, 113, 278–284. [Google Scholar] [CrossRef]
- Kuukkanen, T.; Mälkiä, E.; Kautiainen, H.; Pohjolainen, T. Effectiveness of a Home Exercise Programme in Low Back Pain: A Randomized Five-Year Follow-up Study. Physiother. Res. Int. 2007, 12, 213–224. [Google Scholar] [CrossRef]
- Matarán-Peñarrocha, G.A.; Lara Palomo, I.C.; Antequera Soler, E.; Gil-Martínez, E.; Fernández-Sánchez, M.; Aguilar-Ferrándiz, M.E.; Castro-Sánchez, A.M. Comparison of Efficacy of a Supervised versus Non-Supervised Physical Therapy Exercise Program on the Pain, Functionality and Quality of Life of Patients with Non-Specific Chronic Low-Back Pain: A Randomized Controlled Trial. Clin. Rehabil. 2020, 34, 948–959. [Google Scholar] [CrossRef]
- Zadro, J.R.; Shirley, D.; Simic, M.; Mousavi, S.J.; Ceprnja, D.; Maka, K.; Sung, J.; Ferreira, P. Video-Game-Based Exercises for Older People with Chronic Low Back Pain: A Randomized Controlledtable Trial (GAMEBACK). Phys. Ther. 2019, 99, 14–27. [Google Scholar] [CrossRef]
- Hayden, J.A.; Van Tulder, M.W.; Tomlinson, G. Systematic Review: Strategies for Using Exercise Therapy to Improve Outcomes in Chronic Low Back Pain. Ann. Intern. Med. 2005, 142, 776–785. [Google Scholar] [CrossRef]
- Shirado, O.; Doi, T.; Akai, M.; Hoshino, Y.; Fujino, K.; Hayashi, K.; Marui, E.; Iwaya, T. Multicenter Randomized Controlled Trial to Evaluate the Effect of Home-Based Exercise on Patients with Chronic Low Back Pain: The Japan Low Back Pain Exercise Therapy Study. Spine 2010, 35, E811–E819. [Google Scholar] [CrossRef]
- López-Marcos, J.J.; Díaz-Arribas, M.J.; Valera-Calero, J.A.; Navarro-Santana, M.J.; Izquierdo-García, J.; Ortiz-Gutiérrez, R.M.; Plaza-Manzano, G. The Added Value of Face-to-Face Supervision to a Therapeutic Exercise-Based App in the Management of Patients with Chronic Low Back Pain: A Randomized Clinical Trial. Sensors 2024, 24, 567. [Google Scholar] [CrossRef]
- Lu, W.; Shen, Z.; Chen, Y.; Hu, X.; Ruan, C.; Ma, W.; Jiang, W. Risk Factors Analysis and Risk Prediction Model Construction of Non-Specific Low Back Pain: An Ambidirectional Cohort Study. J. Orthop. Surg. Res. 2023, 18, 545. [Google Scholar] [CrossRef]
- Li, Q.; Peng, L.; Wang, Y.; Yang, Y.; Wang, Z. Risk Factors for Low Back Pain in the Chinese Population: A Systematic Review and Meta-Analysis. BMC Public Health 2024, 24, 1181. [Google Scholar] [CrossRef]
- Yang, Y.; Lai, X.; Li, C.; Yang, Y.; Gu, S.; Hou, W.; Zhai, L.; Zhu, Y. Focus on the Impact of Social Factors and Lifestyle on the Disease Burden of Low Back Pain: Findings from the Global Burden of Disease Study 2019. BMC Musculoskelet. Disord. 2023, 24, 679. [Google Scholar] [CrossRef]
- Brooks, C.; Siegler, J.C.; Cheema, B.S.; Marshall, P.W.M. No Relationship between Body Mass Index and Changes in Pain and Disability after Exercise Rehabilitation for Patients with Mild to Moderate Chronic Low Back Pain. Spine 2013, 38, 2190–2195. [Google Scholar] [CrossRef]
- Hussain, S.M.; Urquhart, D.M.; Wang, Y.; Shaw, J.E.; Magliano, D.J.; Wluka, A.E.; Cicuttini, F.M. Fat Mass and Fat Distribution Are Associated with Low Back Pain Intensity and Disability: Results from a Cohort Study. Arthritis Res. Ther. 2017, 19, 26. [Google Scholar] [CrossRef]
- Krogsbøll, L.T.; Hrábjartsson, A.; Gøtzsche, P.C. Spontaneous Improvement in Randomised Clinical Trials: Meta-Analysis of Three-Armed Trials Comparing No Treatment, Placebo and Active Intervention. BMC Med. Res. Methodol. 2009, 9, 1. [Google Scholar] [CrossRef]
- Ma, X.; Chen, R.; Li, W.; Huang, P. A systematic review and meta-analysis of pain neuroscience education for chronic low back pain: Short-term outcomes of pain and disability. Physiother. Theory Pract. 2024, 40, 2130–2149. [Google Scholar] [CrossRef]
- Foster, N.E.; Anema, J.R.; Cherkin, D.; Chou, R.; Cohen, S.P.; Gross, D.P.; Ferreira, P.H.; Fritz, J.M.; Koes, B.W.; Peul, W.; et al. Prevention and Treatment of Low Back Pain: Evidence, Challenges, and Promising Directions. Lancet 2018, 391, 2368–2383. [Google Scholar] [CrossRef]
- Vader, K.; Donnelly, C.; French, S.D.; Grady, C.; Hill, J.C.; Tripp, D.A.; Williams, A.; Miller, J. Implementing a New Physiotherapist-Led Primary Care Model for Low Back Pain: A Qualitative Study of Patient and Primary Care Team Perspectives. BMC Prim. Care 2022, 23, 201. [Google Scholar] [CrossRef]
- Louw, A.; Zimney, K.; O’Hotto, C.; Hilton, S. The Clinical Application of Teaching People about Pain. Physiother. Theory Pract. 2016, 32, 385–395. [Google Scholar] [CrossRef]
- Diener, I.; Kargela, M.; Louw, A. Listening Is Therapy: Patient Interviewing from a Pain Science Perspective. Physiother. Theory Pract. 2016, 32, 356–367. [Google Scholar] [CrossRef]
- Johnson, R.W.; Williams, S.A.; Gucciardi, D.F.; Bear, N.; Gibson, N. Evaluating the Effectiveness of Home Exercise Programmes Using an Online Exercise Prescription Tool in Children with Cerebral Palsy: Protocol for a Randomised Controlled Trial. BMJ Open 2018, 8, 18316. [Google Scholar] [CrossRef]
- Hafner, T.; Shiffman, J. The Emergence of Global Attention to Health Systems Strengthening. Health Policy Plan. 2013, 28, 41–50. [Google Scholar] [CrossRef]
- Dalleck, L.C.; Schmidt, L.K.; Lueker, R. Cardiac Rehabilitation Outcomes in a Conventional versus Telemedicine-Based Programme. J. Telemed. Telecare 2011, 17, 217–221. [Google Scholar] [CrossRef]
- Kim, H.; Reece, J.; Kang, M. Effects of Accumulated Short Bouts of Exercise on Weight and Obesity Indices in Adults: A Meta-Analysis. Am. J. Health Promot. 2020, 34, 96–104. [Google Scholar] [CrossRef]
- McLean, S.; Nurmatov, U.; Liu, J.L.Y.; Pagliari, C.; Car, J.; Sheikh, A. Telehealthcare for Chronic Obstructive Pulmonary Disease: Cochrane Review and Meta-Analysis. Br. J. Gen. Pract. 2012, 62, e739–e749. [Google Scholar] [CrossRef]
- Baroni, M.P.; Jacob, M.F.A.; Rios, W.R.; Fandim, J.V.; Fernandes, L.G.; Chaves, P.I.; Fioratti, I.; Saragiotto, B.T. The State of the Art in Telerehabilitation for Musculoskeletal Conditions. Arch. Physiother. 2023, 13, 1. [Google Scholar] [CrossRef]
- Laver, K.E.; Adey-Wakeling, Z.; Crotty, M.; George, S.; Lannin, N.A.; Sherrington, C. Telerehabilitation Services for Stroke. Cochrane Database Syst. Rev. 2020, 1, CD010255. [Google Scholar] [CrossRef]
- Cottrell, M.A.; Galea, O.A.; O’Leary, S.P.; Hill, A.J.; Russell, T.G. Real-Time Telerehabilitation for the Treatment of Musculoskeletal Conditions Is Effective and Comparable to Standard Practice: A Systematic Review and Meta-Analysis. Clin. Rehabil. 2017, 31, 625–638. [Google Scholar] [CrossRef]
- Peterson, S. Telerehabilitation Booster Sessions and Remote Patient Monitoring in the Management of Chronic Low Back Pain: A Case Series. Physiother. Theory Pract. 2018, 34, 393–402. [Google Scholar] [CrossRef] [PubMed]
- Palacín-Marín, F.; Esteban-Moreno, B.; Olea, N.; Herrera-Viedma, E.; Arroyo-Morales, M. Agreement between Telerehabilitation and Face-to-Face Clinical Outcome Assessments for Low Back Pain in Primary Care. Spine 2013, 38, 947–952. [Google Scholar] [CrossRef] [PubMed]
- Dario, A.B.; Moreti Cabral, A.; Almeida, L.; Ferreira, M.L.; Refshauge, K.; Simic, M.; Pappas, E.; Ferreira, P.H. Effectiveness of Telehealth-Based Interventions in the Management of Non-Specific Low Back Pain: A Systematic Review with Meta-Analysis. Spine J. 2017, 17, 1342–1351. [Google Scholar] [CrossRef]
- Ferro Moura Franco, K.; Lenoir, D.; dos Santos Franco, Y.R.; Jandre Reis, F.J.; Nunes Cabral, C.M.; Meeus, M. Prescription of Exercises for the Treatment of Chronic Pain along the Continuum of Nociplastic Pain: A Systematic Review with Meta-Analysis. Eur. J. Pain 2021, 25, 51–70. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.H.; Lahart, I.; Carlin, A.; Murtagh, E. The Effects of Continuous Compared to Accumulated Exercise on Health: A Meta-Analytic Review. Sports Med. 2019, 49, 1585–1607. [Google Scholar] [CrossRef]
- Saragiotto, B.T.; Maher, C.G.; Yamato, T.P.; Costa, L.O.P.; Menezes Costa, L.C.; Ostelo, R.W.J.G.; Macedo, L.G. Motor Control Exercise for Chronic Non-Specific Low-Back Pain. Cochrane Database Syst. Rev. 2016, 2016, CD012004. [Google Scholar] [CrossRef]
- Taylor, S.J.C.; Pinnock, H.; Epiphaniou, E.; Pearce, G.; Parke, H.L.; Schwappach, A.; Purushotham, N.; Jacob, S.; Griffiths, C.J.; Greenhalgh, T.; et al. A Rapid Synthesis of the Evidence on Interventions Supporting Self-Management for People with Long-Term Conditions: PRISMS–Practical Systematic Review of Self-Management Support for Long-Term Conditions; NIHR Journals Library: Southampton, UK, 2014. [Google Scholar]
- Fillingim, R.B.; King, C.D.; Ribeiro-Dasilva, M.C.; Rahim-Williams, B.; Riley, J.L. Sex, Gender, and Pain: A Review of Recent Clinical and Experimental Findings. J. Pain 2009, 10, 447–485. [Google Scholar] [CrossRef]
| Author and Year | Sample Characteristics | Intervention | Comparator/ Control | Outcomes | Follow-Up Moments | Main Results |
|---|---|---|---|---|---|---|
| Alp, 2014 [38] | IG: n = 24 (24 M); MA = 51; BMI = 30.3 ± 5.8 CG: n = 24 (24 F); MA = 48; BMI = 29.2 ± 5.4 | Unsupervised core exercises at home | Supervised in-person core exercises | Pain intensity (VAS) Functional disability (RMDQ and FTST) | Baseline and 12 weeks | Intragroup SSI in VAS (IG: p = 0.007; CG: p < 0.001), RMDQ (IG: p = 0.005; GC: p = 0.001) and FTST (p < 0.001) No between-group SSI (VAS: p = 0.385; RMDQ: p = 0.779; FTST: p = 0.733) |
| Dadarkhah, 2021 [39] | IG: n = 28 (16F/12M); MA = 50.0 ± 8.6; BMI = 27.0 ± 2.6 CG: = 28 (16F/12M); MA = 49.0 ± 9.3; BMI = 28.0 ± 3.9 | Unsupervised core exercises at home | Supervised in-person core exercises | Pain intensity (VAS) Functional disability (ODI) | Baseline, post (4 weeks), and 12 weeks | Intragroup SSI in VAS and ODI (p < 0.05) No between-group SSI (VAS: p = 0.93; ODI: p = 0.74) |
| Karaduman, 2023 [32] | IG-1: n = 22 (15F/7M); MA = 44.0 ± 17.1; BMI = 26.9 ± 4.7; PD = 21.6 ± 5.0 weeks IG-2: n = 22 (13F/9M); MA = 46.3 ± 12.3; BMI = 26.4 ± 4.2; PD = 21.3 ± 4.3 weeks CG: n = 22 (2F/20M); MA = 46.5 ± 12.7; BMI = 25.6 ± 4.0; PD = 20.7 ± 3.7 weeks | IG-1: Unsupervised core exercises at home IG-2: Tele-supervised core exercises at home | Supervised in-person core exercises | Pain intensity (NRS) Functional disability (ODI) | Baseline and post (4 weeks) | Intragroup SSI in NRS (p < 0.001) and ODI (p < 0.001) Between-group SSI in favor of the CG and IG-2 in NRS (p < 0.017) and in favor of the CG in ODI (p < 0.05) |
| Kuukkanen, 2007 [40] | IG: n = 29 (14F/15M); MA = 41.0 ± 8.1; BMI = 25.6 ± 13.1 CG: n = 28 (15F/13M); MA = 40.0 ± 8.9; BMI = 25.5 ± 10.5 | Unsupervised core exercises at home | Usual activities of daily living | Pain intensity (Borg scale) Functional disability (ODI) | Baseline, post (12 weeks), 6 and 12 months, and 5 years | Intragroup SSI in Borg and ODI post (p < 0.05) Between-group SSI in favor of the IG at 5 years in Borg (p = 0.01), but no SSI in ODI (p = 0.270) |
| Matarán-Peñarrocha, 2020 [41] | IG: n = 32 (15F/17M); MA = 53.2 ± 8.0; PD = 51.5 ± 8.9 months CG: n = 32 (17F/15M); MA = 54.3 ± 7.9; PD = 53.2 ± 9.0 months | Unsupervised core exercises at home | Supervised in-person core exercises | Pain intensity (VAS) Functional disability (RMDQ and ODI) | Baseline, post (8 weeks), and 32 weeks | Intragroup SSI in VAS, RMDQ, and ODI (p < 0.001) Between-group SSI in favor of the CG in VAS post (p = 0.028), in RMDQ post (p = 0.004) and 32 weeks (p = 0.016), and in ODI post (p = 0.034) |
| Zadro, 2019 [42] | IG: n = 30 (18F/12M); MA = 68.8 ± 5.5; BMI = 26.9 ± 4.1 CG: n= 30 (13F/17M); MA = 67.8 ± 6.0; BMI = 27.4 ± 3.6 | Unsupervised video game exercises at home | Usual activities of daily living | Pain intensity (NRS) Functional disability (PSFS and RMDQ) | Baseline and post (8 weeks) | Between-group SSI in favor of the IG in 11-point NRS (p = 0.04) and PSFS (p = 0.03), but not in RMDQ (p = 0.33) |
| Author and Year | Type of Intervention | Frequency and Duration | Session Volume | Home Follow-Up | Aids, Tools, and Any Additional Aspects |
|---|---|---|---|---|---|
| Alp, 2014 [38] | CORE exercises (resistance) | 6 weeks | 1 set × 20 reps/exercise | Phone call 2 times/week | - |
| Dadarkhah, 2021 [39] | CORE exercises and lower limbs (resistance, stabilization, and mobility) | 4 weeks 2 sessions/day 45 min/session | 3 sets × 20–30 s/stretching 10–20 reps/exercise | Logbook Phone call 3 times/week | Illustrated booklet with exercises |
| Karaduman, 2023 [32] | CORE exercises (resistance and stabilization) | 4 weeks 3 sessions/week 20–30 min/session | 20–30 reps/exercise | IG 2: Online via video conference, under the guidance of a physiotherapist CG: Phone call every week | Progression from one position to another was achieved by holding the abdominal bracing for 8 s and completing 10 repetitions in the current position. CG: Illustrated booklet with exercises |
| Kuukkanen, 2007 [40] | CORE exercises and lower limbs (resistance and mobility) | 12 weeks 7 sessions/week | 3–4 sets × 15–20 reps/exercise | - | Detailed written explanation + illustrated booklet Progression with weekly tests + supervision once a month |
| Matarán-Peñarrocha, 2020 [41] | CORE exercises and lower limbs (resistance, stabilization, and mobility) | 8 weeks 3 sessions/week 30–35 min/session | 3 sets × 10–15 reps/exercise (except planks 30 s/exercise) | Logbook | Previous evaluation and face-to-face session (1 h) for explanation and execution of exercises + illustrated booklet Individualized program (tolerance and availability) |
| Zadro, 2019 [42] | Mobility, full-body resistance, and aerobic exercises through video games | 8 weeks 3 sessions/week 60 min/session | - | Logbook Phone call every 2 weeks | Initial session (1–2 h) for correct and safe use Participants modified the parameters of the program The exercises included video and audio instructions, in addition to providing feedback during their execution |
| Author and Year | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Alp, 2014 [38] | YES | YES | NO | YES | NO | NO | YES | YES | NO | YES | YES | 6 | High |
| Dadarkhah, 2021 [39] | YES | YES | NO | YES | NO | NO | NO | YES | NO | YES | YES | 5 | Moderate |
| Karaduma, 2023 [32] | YES | YES | NO | YES | NO | NO | YES | YES | NO | YES | YES | 6 | High |
| Kuukkanen, 2007 [40] | YES | YES | NO | YES | NO | NO | NO | YES | NO | YES | YES | 5 | Moderate |
| Matarán-Peñarrocha, 2020 [41] | YES | YES | YES | YES | NO | NO | YES | YES | YES | YES | YES | 8 | High |
| Zadro, 2019 [42] | YES | YES | YES | YES | NO | NO | YES | YES | YES | YES | YES | 8 | High |
| Coefficient (SE) | 95% CI | Z | ap Value | I2 (%) | R2 | |
|---|---|---|---|---|---|---|
| Outcome effects | ||||||
| Functional disability | 12.740 (SE = 3.791) | 5.311, 20.170 | 3.361 | 0.001 * | 68.392 | 1 |
| Pain intensity | 13.113 (SE = 3.987) | 5.298, 20.928 | 3.289 | 0.001 * | 80.710 | 0 |
| Covariable effects | ||||||
| Age over functional disability | −0.035 (SE = 0.050) | −0.133, 0.064 | −0.687 | 0.492 | 56.882 | |
| Age over pain intensity | −0.038 (SE = 0.053) | −0.141, 0.065 | −0.725 | 0.468 | 72.930 | |
| BMI over functional disability | −0.373 (SE = 0.123) | −0.615, −0.131 | −3.021 | 0.003 * | 2.492 | |
| BMI over pain intensity | −0.375 (SE = 0.126) | −0.621, −0.129 | −2.984 | 0.003 * | 72.256 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lapuente-Hernández, D.; Gil-Calvo, M.; Cuenca-Zaldívar, J.N.; Carcasona-Otal, A.; Herrero, P.; Matute-Llorente, Á. Home Physical Exercise Interventions in Chronic Non-Specific Low Back Pain: Systematic Review and Multivariate Meta-Analysis. Healthcare 2025, 13, 2094. https://doi.org/10.3390/healthcare13172094
Lapuente-Hernández D, Gil-Calvo M, Cuenca-Zaldívar JN, Carcasona-Otal A, Herrero P, Matute-Llorente Á. Home Physical Exercise Interventions in Chronic Non-Specific Low Back Pain: Systematic Review and Multivariate Meta-Analysis. Healthcare. 2025; 13(17):2094. https://doi.org/10.3390/healthcare13172094
Chicago/Turabian StyleLapuente-Hernández, Diego, Marina Gil-Calvo, Juan Nicolás Cuenca-Zaldívar, Alberto Carcasona-Otal, Pablo Herrero, and Ángel Matute-Llorente. 2025. "Home Physical Exercise Interventions in Chronic Non-Specific Low Back Pain: Systematic Review and Multivariate Meta-Analysis" Healthcare 13, no. 17: 2094. https://doi.org/10.3390/healthcare13172094
APA StyleLapuente-Hernández, D., Gil-Calvo, M., Cuenca-Zaldívar, J. N., Carcasona-Otal, A., Herrero, P., & Matute-Llorente, Á. (2025). Home Physical Exercise Interventions in Chronic Non-Specific Low Back Pain: Systematic Review and Multivariate Meta-Analysis. Healthcare, 13(17), 2094. https://doi.org/10.3390/healthcare13172094