Assessing the Impact of Telemedicine on Patient Satisfaction Before and During the COVID-19 Pandemic
Abstract
1. Introduction
2. Related Works
3. Methods
3.1. Study Design
3.2. Data Source and Sample
3.3. Survey Instrument
3.4. Data Analysis
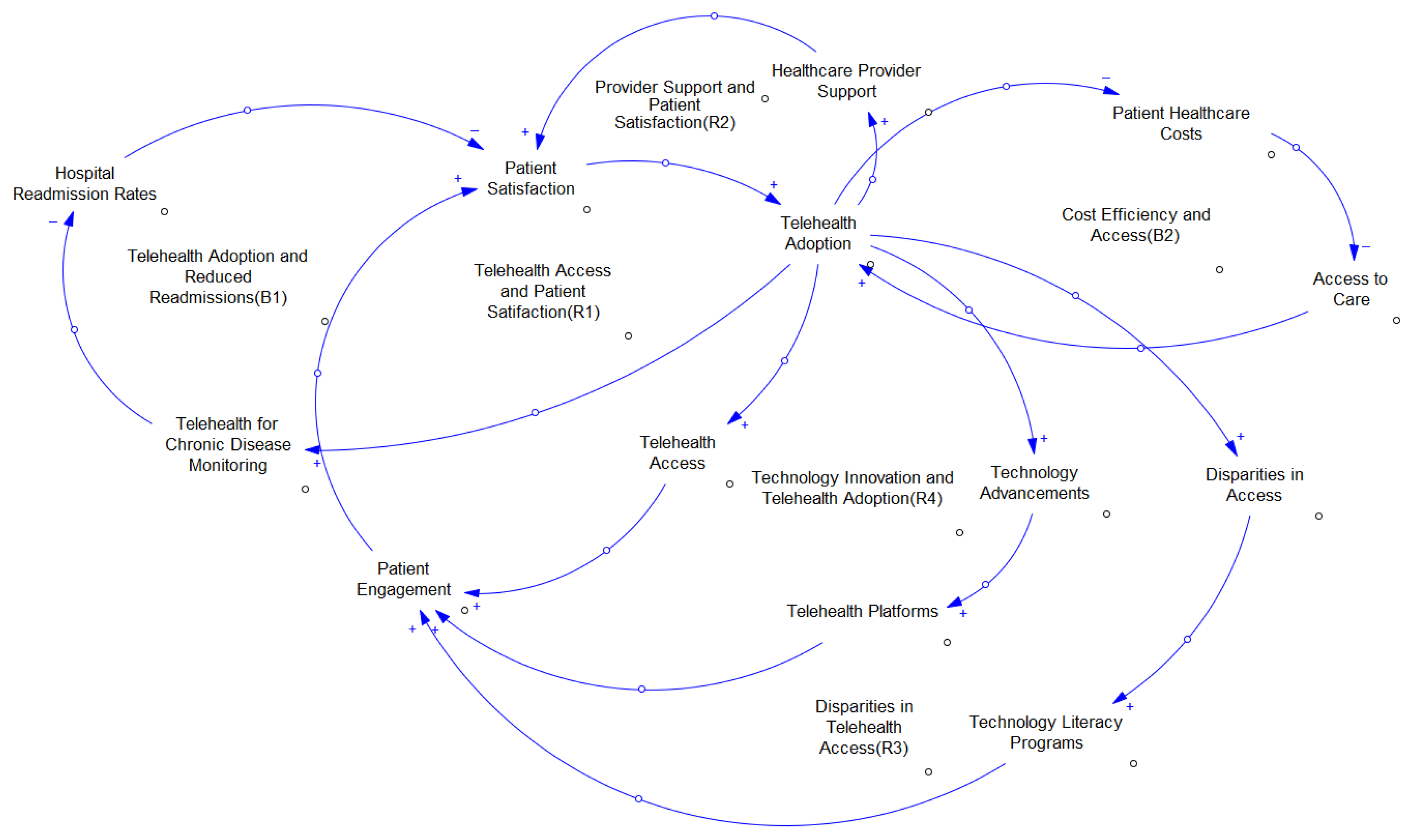
3.5. Causal Model
4. Descriptive Analysis Results
4.1. Healthcare Providers Offered Telemedicine
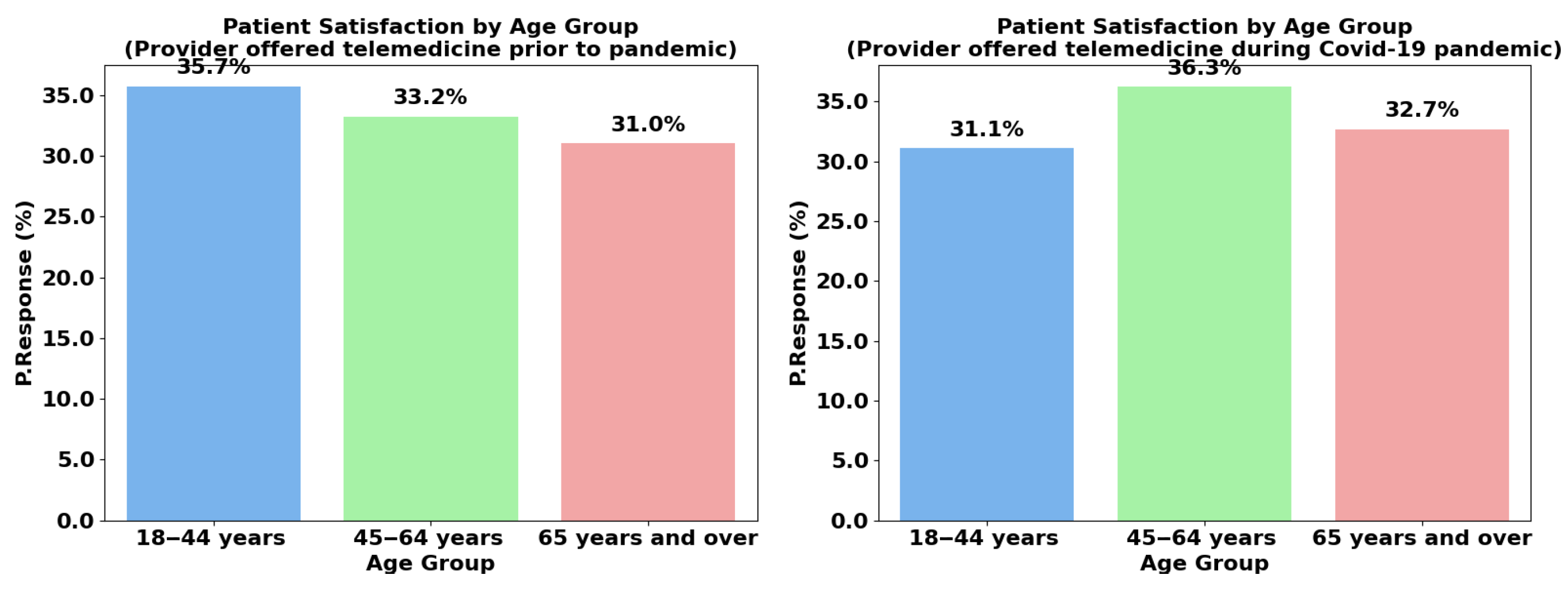
4.2. Age Group
4.3. Gender
4.4. Urbanization
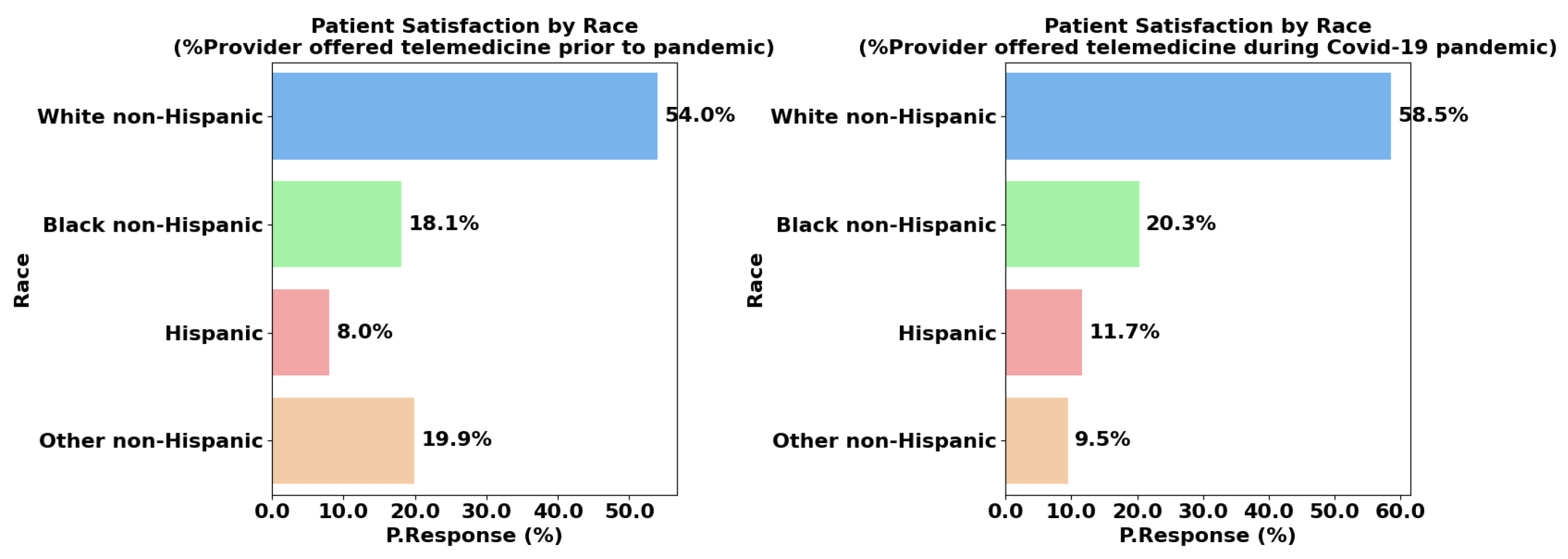
4.5. Race/Hispanic Origin
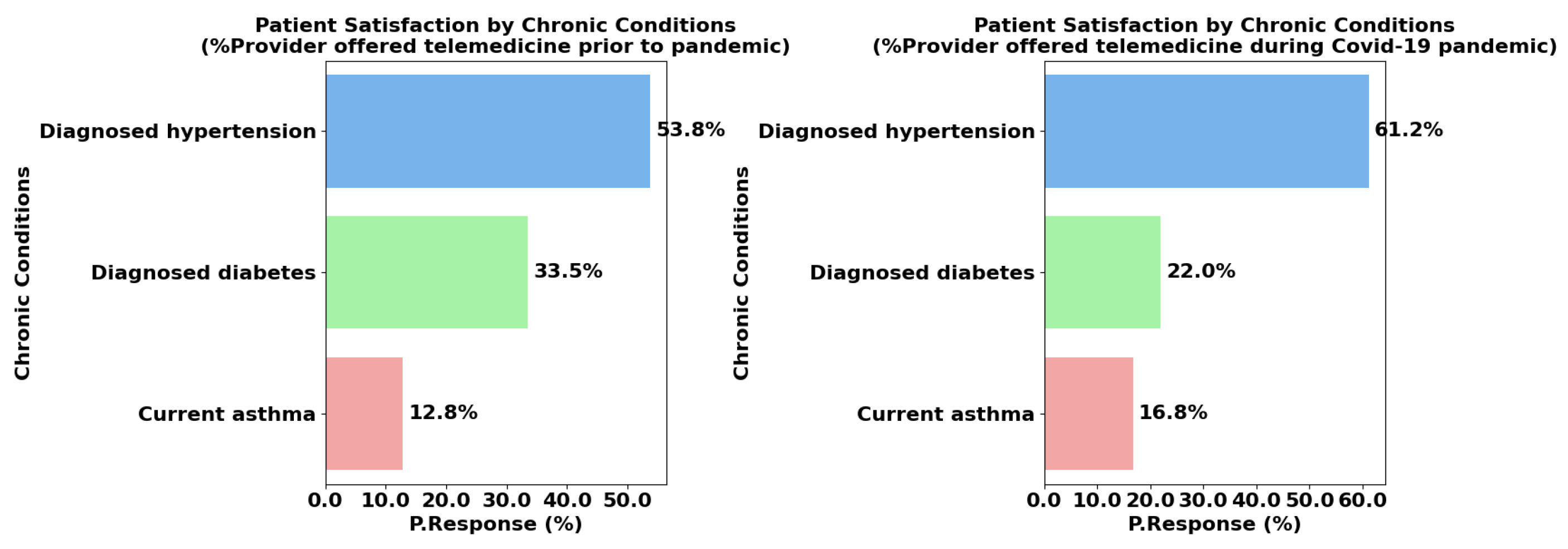
4.6. Chronic Conditions Management
4.7. Inferential Statistical Analysis
4.7.1. The 95% Confidence Interval (CI)
- = sample mean;
- = critical value from the t-distribution for 95% confidence (based on degrees of freedom, );
- s = sample standard deviation;
- n = number of data points (sample size).
4.7.2. p-Value (One-Sample t-Test)
- t = t-statistic;
- = sample mean;
- = hypothesized population mean (usually 0 for a one-sample t-test);
- s = sample standard deviation;
- n = number of data points (sample size).
5. Discussion
5.1. Limitations of Telemedicine
5.2. Strategies to Enhance Telemedicine Adoption
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jazieh, A.R.; Kozlakidis, Z. Healthcare transformation in the post-coronavirus pandemic era. Front. Med. 2020, 7, 429. [Google Scholar] [CrossRef]
- Weinstein, R.S.; Lopez, A.M.; Joseph, B.A.; Erps, K.A.; Holcomb, M.; Barker, G.P.; Krupinski, E.A. Telemedicine, telehealth, and mobile health applications that work: Opportunities and barriers. Am. J. Med. 2014, 127, 183–187. [Google Scholar] [CrossRef]
- Serper, M.; Volk, M.L. Current and future applications of telemedicine to optimize the delivery of care in chronic liver disease. Clin. Gastroenterol. Hepatol. 2018, 16, 157–161. [Google Scholar] [CrossRef]
- Bashshur, R.L.; Howell, J.D.; Krupinski, E.A.; Harms, K.M.; Bashshur, N.; Doarn, C.R. The empirical foundations of telemedicine interventions in primary care. Telemed. e-Health 2016, 22, 342–375. [Google Scholar] [CrossRef]
- Scott Kruse, C.; Karem, P.; Shifflett, K.; Vegi, L.; Ravi, K.; Brooks, M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J. Telemed. Telecare 2018, 24, 4–12. [Google Scholar] [CrossRef]
- Uleman, J.F.; Stronks, K.; Rutter, H.; Arah, O.A.; Rod, N.H. Mapping complex public health problems with causal loop diagrams. Int. J. Epidemiol. 2024, 53, dyae091. [Google Scholar] [CrossRef]
- Feuerriegel, S.; Frauen, D.; Melnychuk, V.; Schweisthal, J.; Hess, K.; Curth, A.; Bauer, S.; Kilbertus, N.; Kohane, I.S.; van der Schaar, M. Causal machine learning for predicting treatment outcomes. Nat. Med. 2024, 30, 958–968. [Google Scholar] [CrossRef]
- Sterman, J. System Dynamics: Systems Thinking and Modeling for a Complex World; McGraw-Hill Education Ltd.: New York, NY, USA, 2002. [Google Scholar]
- Centers for Disease Control and Prevention, CDC. Access and Use of Telemedicine During COVID-19. 2024. Available online: https://data.cdc.gov/NCHS/Access-and-Use-of-Telemedicine-During-COVID-19/8xy9-ubqz/data_preview (accessed on 18 June 2025).
- Vudathaneni, V.K.P.; Lanke, R.B.; Mudaliyar, M.C.; Movva, K.V.; Kalluri, L.M.; Boyapati, R. The Impact of Telemedicine and Remote Patient Monitoring on Healthcare Delivery: A Comprehensive Evaluation. Cureus 2024, 16, e55534. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens. Int. 2021, 2, 100117. [Google Scholar] [CrossRef]
- Corbett, J.A.; Opladen, J.M.; Bisognano, J.D. Telemedicine can revolutionize the treatment of chronic disease. Int. J. Cardiol. Hypertens. 2020, 7, 100051. [Google Scholar] [CrossRef]
- Lannon, C. Causal loop construction: The basics. Syst. Think. 2012, 23, 7–8. [Google Scholar]
- Cheng, Y.; Goodin, A.J.; Pahor, M.; Manini, T.; Brown, J.D. Healthcare utilization and physical functioning in older adults in the United States. J. Am. Geriatr. Soc. 2020, 68, 266–271. [Google Scholar] [CrossRef]
- World Health Organization. Gender Analysis in Health: A Review of Selected Tools; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Nouri, S.; Khoong, E.C.; Lyles, C.R.; Karliner, L. Addressing equity in telemedicine for chronic disease management during the Covid-19 pandemic. NEJM Catal. Innov. Care Deliv. 2020, 1. [Google Scholar] [CrossRef]
- Azad, A.D.; Charles, A.G.; Ding, Q.; Trickey, A.W.; Wren, S.M. The gender gap and healthcare: Associations between gender roles and factors affecting healthcare access in Central Malawi, June–August 2017. Arch. Public Health 2020, 78, 119. [Google Scholar] [CrossRef]
- Dluhos-Sebesto, C.; Jethwa, T.E.; Bertasi, T.G.; Bertasi, R.A.; Nishi, L.Y.M.; Pantin, S.A.L.; Argenio, S.L.; Shahsamand, A.; Omololu, A.; Pujalte, G.G. Women’s health information survey: Common health concerns and trusted sources of health information among different populations of female patients. Women’s Health Rep. 2021, 2, 173–181. [Google Scholar] [CrossRef]
- Oster, N.V.; Patterson, D.G.; Skillman, S.M.; Frogner, B.K. COVID-19 and the Rural Health Workforce: The Impact of Federal Pandemic Funding to Address Workforce Needs; Center for Health Workforce Studies, University of Washington: Seattle, WA, USA, 2022. [Google Scholar]
- Cuadros, D.F.; Branscum, A.J.; Mukandavire, Z.; Miller, F.D.; MacKinnon, N. Dynamics of the COVID-19 epidemic in urban and rural areas in the United States. Ann. Epidemiol. 2021, 59, 16–20. [Google Scholar] [CrossRef]
- Ullrich, F.; Mueller, K. Metropolitan/Nonmetropolitan COVID-19 Confirmed Cases and General ICU Beds; RUPRI Center for Rural Health Policy Analysis: Iowa City, IA, USA, 2020; Available online: https://rupri.public-health.uiowa.edu/publications/policybriefs/2020/COVID%20and%20Hospital%20Beds.pdf (accessed on 18 June 2025).
- Schroeder, S. Rural Communities: Age, Income, and Health Status; Rural Health Research RECAP: Grand Forks, ND, USA, 2018. [Google Scholar]
- Graves, J.M.; Abshire, D.A.; Alejandro, A.G. System-and individual-level barriers to accessing medical care services across the rural-urban spectrum, Washington State. Health Serv. Insights 2022, 15, 11786329221104667. [Google Scholar] [CrossRef] [PubMed]
- Read, J.G.; Lynch, S.M.; West, J.S. Disaggregating heterogeneity among non-Hispanic Whites: Evidence and implications for US racial/ethnic health disparities. Popul. Res. Policy Rev. 2021, 40, 9–31. [Google Scholar] [CrossRef]
- Copeland, V.C. African Americans: Disparities in health care access and utilization. Health Soc. Work 2005, 30, 265–270. [Google Scholar] [CrossRef]
- Callahan, S.T.; Hickson, G.B.; Cooper, W.O. Health care access of Hispanic young adults in the United States. J. Adolesc. Health 2006, 39, 627–633. [Google Scholar] [CrossRef]
- Chunara, R.; Zhao, Y.; Chen, J.; Lawrence, K.; Testa, P.A.; Nov, O.; Mann, D.M. Telemedicine and healthcare disparities: A cohort study in a large healthcare system in New York City during COVID-19. J. Am. Med Inform. Assoc. 2021, 28, 33–41. [Google Scholar] [CrossRef]
- Adepoju, O.E.; Chae, M.; Ojinnaka, C.O.; Shetty, S.; Angelocci, T. Utilization gaps during the COVID-19 pandemic: Racial and ethnic disparities in telemedicine uptake in federally qualified health center clinics. J. Gen. Intern. Med. 2022, 37, 1191–1197. [Google Scholar] [CrossRef]
- Badr, J.; Motulsky, A.; Denis, J.L. Digital health technologies and inequalities: A scoping review of potential impacts and policy recommendations. Health Policy 2024, 146, 105122. [Google Scholar] [CrossRef]
- Carey, R.M.; Wright, J.T., Jr.; Taler, S.J.; Whelton, P.K. Guideline-driven management of hypertension: An evidence-based update. Circ. Res. 2021, 128, 827–846. [Google Scholar] [CrossRef]
- Egan, A.M.; Dinneen, S.F. What is diabetes? Medicine 2019, 47, 1–4. [Google Scholar] [CrossRef]
- Sockrider, M.; Fussner, L. What is asthma? Am. J. Respir. Crit. Care Med. 2020, 202, P25–P26. [Google Scholar] [CrossRef]
- Gajarawala, S.N.; Pelkowski, J.N. Telehealth benefits and barriers. J. Nurse Pract. 2021, 17, 218–221. [Google Scholar] [CrossRef]
- Wosik, J.; Fudim, M.; Cameron, B.; Gellad, Z.F.; Cho, A.; Phinney, D.; Curtis, S.; Roman, M.; Poon, E.G.; Ferranti, J.; et al. Telehealth transformation: COVID-19 and the rise of virtual care. J. Am. Med. Inform. Assoc. 2020, 27, 957–962. [Google Scholar] [CrossRef]
- Fikri, E. Rural, Regional, Racial Disparities in Telemedicine Use During the COVID-19 Pandemic Among US Adults: 2021 National Health Interview Survey (NHIS). Patient Prefer. Adherence 2024, 18, 89–90. [Google Scholar] [CrossRef]
- Fitzpatrick, P.J. Improving health literacy using the power of digital communications to achieve better health outcomes for patients and practitioners. Front. Digit. Health 2023, 5, 1264780. [Google Scholar] [CrossRef]
- Ma, Y.; Zhao, C.; Zhao, Y.; Lu, J.; Jiang, H.; Cao, Y.; Xu, Y. Telemedicine application in patients with chronic disease: A systematic review and meta-analysis. BMC Med. Inform. Decis. Mak. 2022, 22, 105. [Google Scholar] [CrossRef] [PubMed]



| Groups | Subgroups | Mean | 95% CI (Lower) | 95% CI (Upper) | p-Value |
|---|---|---|---|---|---|
| Age Group | 18–44 years | 434 | 157.73 | 710.94 | 0.010 |
| 45–64 years | 475 | 107.68 | 842.32 | 0.021 | |
| 65+ years | 432 | 124.43 | 739.91 | 0.015 | |
| Sex | Male | 606 | 271.80 | 941.87 | 0.006 |
| Female | 775 | 218.99 | 1331.01 | 0.016 | |
| Urbanization | Metropolitan | 1146 | 320.17 | 1971.83 | 0.016 |
| Non-Metropolitan | 146 | 31.77 | 261.56 | 0.022 | |
| Race/Hispanic Origin | White NH | 948 | 372.52 | 1523.48 | 0.008 |
| Black NH | 325 | 93.29 | 556.71 | 0.015 | |
| Hispanic | 172 | 34.55 | 310.79 | 0.024 | |
| Other Hispanic | 220 | 4.92 | 436.75 | 0.047 | |
| Chronic Conditions | Hypertension | 601 | 189.52 | 1012.48 | 0.013 |
| Diabetes | 263 | 76.23 | 450.44 | 0.015 | |
| Asthma | 158 | 39.99 | 276.68 | 0.018 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adeogun, A.; Faezipour, M. Assessing the Impact of Telemedicine on Patient Satisfaction Before and During the COVID-19 Pandemic. Healthcare 2025, 13, 2095. https://doi.org/10.3390/healthcare13172095
Adeogun A, Faezipour M. Assessing the Impact of Telemedicine on Patient Satisfaction Before and During the COVID-19 Pandemic. Healthcare. 2025; 13(17):2095. https://doi.org/10.3390/healthcare13172095
Chicago/Turabian StyleAdeogun, Ashiat, and Misa Faezipour. 2025. "Assessing the Impact of Telemedicine on Patient Satisfaction Before and During the COVID-19 Pandemic" Healthcare 13, no. 17: 2095. https://doi.org/10.3390/healthcare13172095
APA StyleAdeogun, A., & Faezipour, M. (2025). Assessing the Impact of Telemedicine on Patient Satisfaction Before and During the COVID-19 Pandemic. Healthcare, 13(17), 2095. https://doi.org/10.3390/healthcare13172095






