Translation and Validation of the Malay Doctor–Patient Communication Questionnaire: A Cross-Sectional Study Among Patients Receiving Hemodialysis in Kelantan, Malaysia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Participants and Sampling
2.3. Instrument Translation and Adaptation
2.4. The Translation Process Followed the Guidelines Proposed by Beaton et al. [36]
2.5. Data Collection Procedures
2.6. Statistical Analysis
2.7. Ethical Approval
3. Results
3.1. Participant Characteristics
3.2. Descriptive Statistics of Doctor–Patient Communication
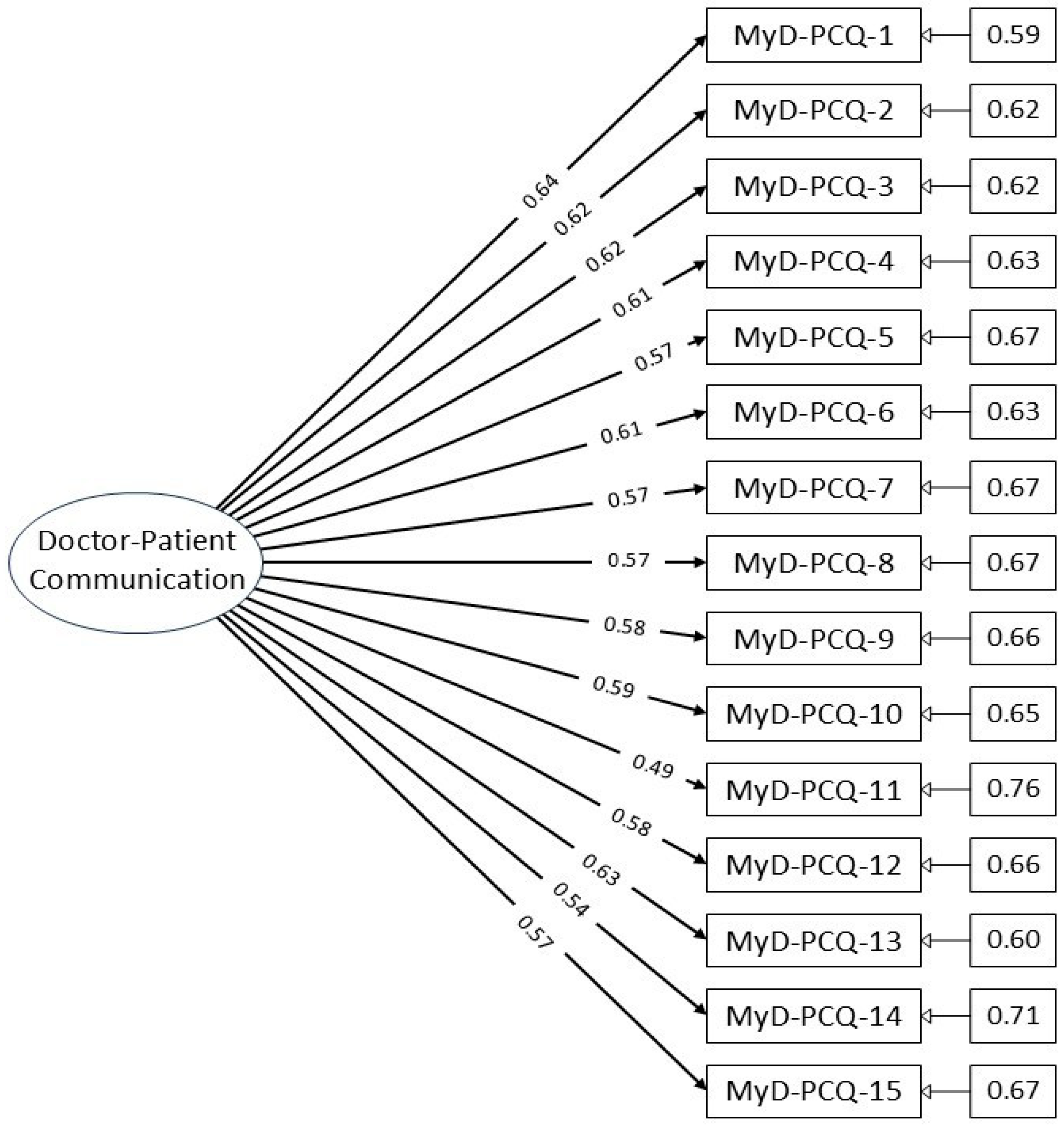
3.3. Confirmatory Factor Analysis Results
3.4. Factor Loadings and Reliability
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| MyD-PCQ | Malay version of the Doctor–Patient Communication Questionnaire |
| CFA | Confirmatory factor analysis |
| CFI | Comparative fit index |
| TLI | Tucker–Lewis index |
| AIC | Akaike information criterion |
| BIC | Bayesian information criterion |
| SRMR | Standardized root mean square residual |
| RMSEA | Root mean square error of approximation |
References
- Selinger, C.P. The right to consent: Is it absolute? Br. J. Med. Pract. 2009, 2, 50–54. [Google Scholar]
- Browning, P.E. Professional patient relationship. In How to Reference Books; Longe, J.L., Ed.; Gale: Farmington Hills, MI, USA, 2018. [Google Scholar]
- Curran, J. The doctor, his patient, and the illness. BMJ 2007, 335, 941–945. [Google Scholar] [CrossRef]
- Goold, S.D.; Lipkin, M. The doctor–patient relationship. J. Gen. Intern. Med. 1999, 14, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Kelley, J.M.; Kraft-Todd, G.; Schapira, L.; Kossowsky, J.; Riess, H. The influence of the patient–clinician relationship on healthcare outcomes: A systematic review and meta-analysis of randomized controlled trials. PLoS ONE 2014, 9, e94207. [Google Scholar] [CrossRef] [PubMed]
- Dwolatzky, T.; Clarfield, A.M. Doctor–patient relationships. In Encyclopedia of Aging; Schulz, R., Ed.; Springer Publishing Company: Berlin/Heidelberg, Germany, 2006. [Google Scholar]
- Duffy, F.D.; Gordon, G.H.; Whelan, G.; Cole-Kelly, K.; Frankel, R. Assessing competence in communication and interpersonal skills: The Kalamazoo II Report. Acad. Med. 2004, 79, 495–507. [Google Scholar] [CrossRef]
- Arora, N.K. Interacting with cancer patients: The significance of physicians’ communication behavior. Soc. Sci. Med. 2003, 57, 791–806. [Google Scholar] [CrossRef]
- Tongue, J.R.; Epps, H.R.; Forese, L.L. Communication skills for patient-centered care: Research-based, easily learned techniques for medical interviews that benefit orthopedic surgeons and their patients. J. Bone Jt. Surg. Am. 2005, 87, 652–658. [Google Scholar] [CrossRef]
- Lee, S.J.; Back, A.L.; Block, S.D.; Stewart, S.K. Enhancing physician–patient communication. Hematol. Am. Soc. Hematol. Educ. Program. 2002, 2002, 464–483. [Google Scholar] [CrossRef]
- Kindler, C.H.; Szirt, L.; Sommer, D.; Hausler, R.; Langewitz, W. A quantitative analysis of anesthetist–patient communication during the pre-operative visit. Anaesthesia 2005, 60, 53–59. [Google Scholar] [CrossRef]
- Middleton, S.; Gattellari, M.; Harris, J.P.; Ward, J.E. Assessing surgeons’ disclosure of risk information before carotid endarterectomy. ANZ J. Surg. 2006, 76, 618–624. [Google Scholar] [CrossRef]
- Foy, R.; Walker, A.; Ramsay, C.; Penney, G.; Grimshaw, J.; Francis, J. Frequency of patient–physician contact in chronic kidney disease care and achievement of clinical performance targets. Int. J. Qual. Health Care 2005, 17, 115–121. [Google Scholar] [CrossRef]
- Pinheiro, J.; Maia, M.; Alves, H. The physician–patient relationship in dialysis. Port. J. Nephrol. Hypert 2013, 27, 179–185. [Google Scholar]
- Argentero, P.; Dell’Olivo, B.; Ferretti, M.S. Staff burnout and satisfaction with the quality of dialysis care. Am. J. Kidney Dis. 2008, 51, 80–92. [Google Scholar] [CrossRef] [PubMed]
- Kovac, J.A.; Patel, S.S.; Peterson, R.A.; Kimmel, P.L. Patient satisfaction with care and behavioral compliance in end-stage renal disease patients treated with hemodialysis. Am. J. Kidney Dis. 2002, 39, 1236–1244. [Google Scholar] [CrossRef]
- Jha, A.K.; Orav, E.J.; Zheng, J.; Epstein, A.M. Patients’ perception of hospital care in the United States. N. Engl. J. Med. 2008, 359, 1921–1931. [Google Scholar] [CrossRef]
- Mazairac, A.H.; de Wit, G.A.; Penne, E.L.; van der Weerd, N.C.; de Jong, B.; Grooteman, M.P.; van den Dorpel, M.A.; Buskens, E.; Dekker, F.W.; Nubé, M.J.; et al. Changes in quality of life over time: Dutch hemodialysis patients and general population compared. Nephrol. Dial. Transplant. 2011, 26, 1984–1989. [Google Scholar] [CrossRef]
- Manzoor, F.; Wei, L.; Hussain, A.; Asif, M.; Shah, S.I.; Akram, M.N. Patient satisfaction with health care services: An application of physician’s behavior as a moderator. Int. J. Environ. Res. Public Health 2019, 16, 3318. [Google Scholar] [CrossRef]
- Ridd, M.; Shaw, A.; Lewis, G.; Salisbury, C. The patient–doctor relationship: A synthesis of the qualitative literature on patients’ perspectives. Br. J. Gen. Pract. 2009, 59, e116–e133. [Google Scholar] [CrossRef]
- Huggard, P. Compassion fatigue: How much can I give? Med. Educ. 2003, 37, 163–164. [Google Scholar] [CrossRef]
- Smith, J.A. Evaluating the contribution of interpretive phenomenological analysis. Health Psychol. Rev. 2011, 5, 9–27. [Google Scholar] [CrossRef]
- Bennett, J.; O’Donovan, D. Substance misuse by doctors, nurses, and other healthcare workers. Curr. Opin. Psychiatry 2001, 14, 195–199. [Google Scholar] [CrossRef]
- Tyssen, R.; Vaglum, P. Mental health problems among young doctors: An updated review of prospective studies. Harv. Rev. Psychiatry 2002, 10, 154–165. [Google Scholar] [CrossRef] [PubMed]
- Ball, L.; Maben, J.; Griffiths, P. Questionnaires that measure the quality of relationships between patients and primary care providers: A systematic review. BMC Health Serv. Res. 2018, 18, 866. [Google Scholar] [CrossRef] [PubMed]
- Carretta, E.; Bond, T.G.; Cappiello, G.; Fantini, M.P. Looking through the patients’ eyes: Measuring patient satisfaction in a public hospital. J. Patient Exp. 2017, 4, 121–128. [Google Scholar] [CrossRef]
- Xie, Z.; Or, C. Associations between waiting times, service times, and patient satisfaction in an endocrinology outpatient department: A time study and questionnaire survey. Health Serv. Res. 2017, 54, 527–532. [Google Scholar] [CrossRef]
- Silverman, J.; Kurtz, S.; Draper, J. Skills for Communicating with Patients. Ann. R. Coll. Surg. Engl. 2006, 88, 84–88. [Google Scholar] [CrossRef]
- Sustersic, M.; Jeannin, A.; Sandoz, V.; Cerutti, B.; Junod Perron, N. A scale assessing doctor–patient communication in a context of acute conditions based on a systematic review. PLoS ONE 2018, 13, e0192306. [Google Scholar] [CrossRef]
- Freburger, J.K.; Callahan, L.F.; Currey, S.S.; Anderson, L.A. Use of the Trust in Physician Scale in patients with rheumatic disease: Psychometric properties and correlates of trust in the rheumatologist. Arthritis Rheum. 2003, 49, 51–58. [Google Scholar] [CrossRef]
- Hatcher, R.L.; Gillaspy, J.A. Development and validation of a revised short version of the Working Alliance Inventory. Psychother. Res. 2006, 16, 12–25. [Google Scholar] [CrossRef]
- Munder, T.; Wilmers, F.; Leonhart, R.; Linster, H.W.; Barth, J. Working Alliance Inventory-Short Revised (WAI-SR): Psychometric properties in outpatients and inpatients. Clin. Psychol. Psychother. 2010, 17, 231–239. [Google Scholar] [CrossRef]
- Andersson, L.A.; Dedrick, R.F. Development of the Trust in Physician Scale: A measure to assess interpersonal trust in patient–physician relationships. Psychol. Rep. 1990, 67, 1091–1100. [Google Scholar] [CrossRef] [PubMed]
- Thom, D.H.; Ribisl, K.M.; Stewart, A.L.; Luke, D.A. Further validation and reliability testing of the Trust in Physician Scale. Med. Care 1999, 37, 510–517. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Malaysia. Malaysia Health System Performance. 2017. Available online: http://www.moh.gov.my/ (accessed on 13 June 2025).
- Wild, D.; Grove, A.; Martin, M.; Eremenco, S.; McElroy, S.; Verjee-Lorenz, A.; Erikson, P.; ISPOR Task Force for Translation and Cultural Adaptation. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: Report of the ISPOR task force for translation and cultural adaptation. Value Health 2005, 8, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Martinez, S.M.; Ainsworth, B.E.; Elder, J.P. A review of physical activity measures used among US Latinos: Guidelines for developing culturally appropriate measures. Ann. Behav. Med. 2008, 36, 195–207. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 6th ed.; Pearson Education: Boston, MA, USA, 2013. [Google Scholar]
- Cook, D.A.; Beckman, T.J. Current concepts in validity and reliability for psychometric instruments: Theory and application. Am. J. Med. 2006, 119, 166.e7–166.e16. [Google Scholar] [CrossRef]
- Raykov, T. Estimation of congeneric scale reliability using covariance structure analysis with nonlinear constraints. Br. J. Math. Stat. Psychol. 2001, 54, 315–323. [Google Scholar] [CrossRef]
- Pituch, K.A.; Stevens, J.P. Applied Multivariate Statistics for the Social Sciences: Analyses with SAS and IBM’s SPSS; Routledge: London, UK, 2015. [Google Scholar]
- Schreiber, J.B.; Nora, A.; Stage, F.K.; Barlow, E.A.; King, J. Reporting structural equation modeling and confirmatory factor analysis results: A review. J. Educ. Res. 2006, 99, 323–338. [Google Scholar] [CrossRef]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research; Guilford Publications: New York, NY, USA, 2014. [Google Scholar]
- Blais, M.A. Development of an inpatient treatment alliance scale. J. Nerv. Ment. Dis. 2004, 192, 487–493. [Google Scholar] [CrossRef]
| Variables | Frequency (n) | Percent (%) |
|---|---|---|
| Gender | ||
| Male | 106 | 35.3% |
| Female | 194 | 64.7% |
| Age group | ||
| 18–27 Years Old | 50 | 16.7% |
| 28–37 Years Old | 38 | 12.7% |
| 38–47 Years Old | 40 | 13.3% |
| 48–57 Years Old | 70 | 23.3% |
| Over 58 Years Old | 102 | 34.0% |
| Ethnicity | ||
| Malay | 142 | 47.3% |
| Chinese | 72 | 24.0% |
| Indian | 42 | 14.0% |
| Others | 44 | 14.7% |
| Marital Status | ||
| Bachelor | 40 | 13.3% |
| Married | 176 | 58.7% |
| Widow/Widower | 84 | 28.0% |
| Education Level | ||
| O level | 108 | 36.0% |
| A level | 80 | 26.7% |
| Diploma | 48 | 16.0% |
| Degree | 64 | 21.3% |
| Type of Occupation | ||
| Government | 26 | 8.7% |
| Private | 60 | 20.0% |
| Self-employed | 64 | 21.3% |
| Housemaker | 68 | 22.7% |
| Student | 16 | 5.3% |
| Not Working | 66 | 22.0% |
| Income level (MYR) | ||
| 1000–4360 | 180 | 60.0% |
| 4361–9620 | 90 | 30.0% |
| 9621 and above | 30 | 10.0% |
| Do you agree with and support the treatment provided? | ||
| No | 38 | 12.7% |
| Yes | 262 | 87.3% |
| Are you satisfied with the service provided by the doctor? | ||
| No | 36 | 12.0% |
| Yes | 264 | 88.0% |
| Is your doctor easily reachable? | ||
| No | 32 | 10.7% |
| Yes | 268 | 89.3% |
| Is your doctor ready to treat you? | ||
| No | 28 | 9.3% |
| Yes | 272 | 90.7% |
| Statements | Mean (SD) | n (Percent (%)) | |||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||
| Did the doctor listen to you carefully during the consultation? | 2.48 (0.53) | 2 (0.7) | 156 (52.0) | 138 (46.0) | 4 (1.3) |
| Did the doctor allow you to talk without interrupting you? | 2.50 (0.55) | 3 (1.0) | 148 (49.3) | 144 (48.0) | 5 (1.7) |
| Did the doctor encourage you to express yourself/talk? | 2.45 (0.56) | 5 (1.7) | 150 (53.3) | 130 (43.3) | 5 (1.7) |
| Did the doctor examine you thoroughly? | 2.52 (0.56) | 4 (1.3) | 142 (47.3) | 147 (49.0) | 7 (2.3) |
| Do you feel that the doctor understood you? | 2.47 (0.56) | 5 (1.7) | 152 (50.7) | 138 (46.0) | 5 (1.7) |
| Was it easy to understand what the doctor said? | 2.45 (0.57) | 9 (3.0) | 151 (50.3) | 136 (45.3) | 4 (1.3) |
| Do you feel you were given all the necessary information? | 2.49 (0.55) | 3 (1.0) | 150 (53.3) | 142 (47.3) | 5 (1.7) |
| Did the doctor explain the advantages and disadvantages of the treatment or care strategy? | 2.49 (0.53) | 3 (1.0) | 149 (49.7) | 145 (48.3) | 3 (1.0) |
| Did the doctor involve you in the decision-making? | 2.49 (0.55) | 6 (2.0) | 143 (47.7) | 148 (49.3) | 3 (1.0) |
| In your opinion, did the doctor have a reassuring attitude and way of talking? | 2.50 (0.52) | 1 (0.3) | 149 (49.7) | 147 (49.0) | 3 (1.0) |
| Do you think the doctor was in general respectful? | 2.48 (0.56) | 7 (2.3) | 145 (48.3) | 145 (48.3) | 3 (1.0) |
| Did the doctor make sure that you understood his explanations and instructions? | 2.48 (0.55) | 6 (2.0) | 146 (48.7) | 145 (48.3) | 3 (1.0) |
| Do you think the doctor told the whole truth? | 2.47 (0.53) | 2 (0.7) | 156 (52.0) | 139 (46.3) | 3 (1.0) |
| Do you have confidence in this doctor? | 2.49 (0.53) | 1 (0.3) | 153 (51.0) | 142 (47.3) | 4 (1.3) |
| Did the doctor reply to all your expectations and concerns? | 2.50 (0.53) | 4 (1.3) | 142 (47.3) | 152 (50.7) | 2 (0.7) |
| Total score | 37.31 | ||||
| Model | (df) | /df | p | SRMR | RMSEA | 90% CI | CFI | TLI | AIC | BIC |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 112.663 (90) | 1.25 | 0.053 | 0.037 | 0.029 | 0.000, 0.045 | 0.982 | 0.979 | 6187.240 | 6298.354 |
| MyPDRQ Items | Factor Loading | Raykov’s Rho |
|---|---|---|
| Q01 | 0.640 | 0.887 |
| Q02 | 0.618 | |
| Q03 | 0.619 | |
| Q04 | 0.608 | |
| Q05 | 0.573 | |
| Q06 | 0.605 | |
| Q07 | 0.574 | |
| Q08 | 0.571 | |
| Q09 | 0.580 | |
| Q10 | 0.595 | |
| Q11 | 0.493 | |
| Q12 | 0.584 | |
| Q13 | 0.534 | |
| Q14 | 0.542 | |
| Q15 | 0.574 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ab Aziz, A.F.F.; Ibrahim, M.I.; Yaacob, N.M.; A Rahim, A.I. Translation and Validation of the Malay Doctor–Patient Communication Questionnaire: A Cross-Sectional Study Among Patients Receiving Hemodialysis in Kelantan, Malaysia. Healthcare 2025, 13, 2037. https://doi.org/10.3390/healthcare13162037
Ab Aziz AFF, Ibrahim MI, Yaacob NM, A Rahim AI. Translation and Validation of the Malay Doctor–Patient Communication Questionnaire: A Cross-Sectional Study Among Patients Receiving Hemodialysis in Kelantan, Malaysia. Healthcare. 2025; 13(16):2037. https://doi.org/10.3390/healthcare13162037
Chicago/Turabian StyleAb Aziz, Ab Farid Fajilah, Mohd Ismail Ibrahim, Najib Majdi Yaacob, and Afiq Izzudin A Rahim. 2025. "Translation and Validation of the Malay Doctor–Patient Communication Questionnaire: A Cross-Sectional Study Among Patients Receiving Hemodialysis in Kelantan, Malaysia" Healthcare 13, no. 16: 2037. https://doi.org/10.3390/healthcare13162037
APA StyleAb Aziz, A. F. F., Ibrahim, M. I., Yaacob, N. M., & A Rahim, A. I. (2025). Translation and Validation of the Malay Doctor–Patient Communication Questionnaire: A Cross-Sectional Study Among Patients Receiving Hemodialysis in Kelantan, Malaysia. Healthcare, 13(16), 2037. https://doi.org/10.3390/healthcare13162037








