Telemedicine in Obstetrics and Gynecology: A Scoping Review of Enhancing Access and Outcomes in Modern Healthcare
Abstract
1. Introduction
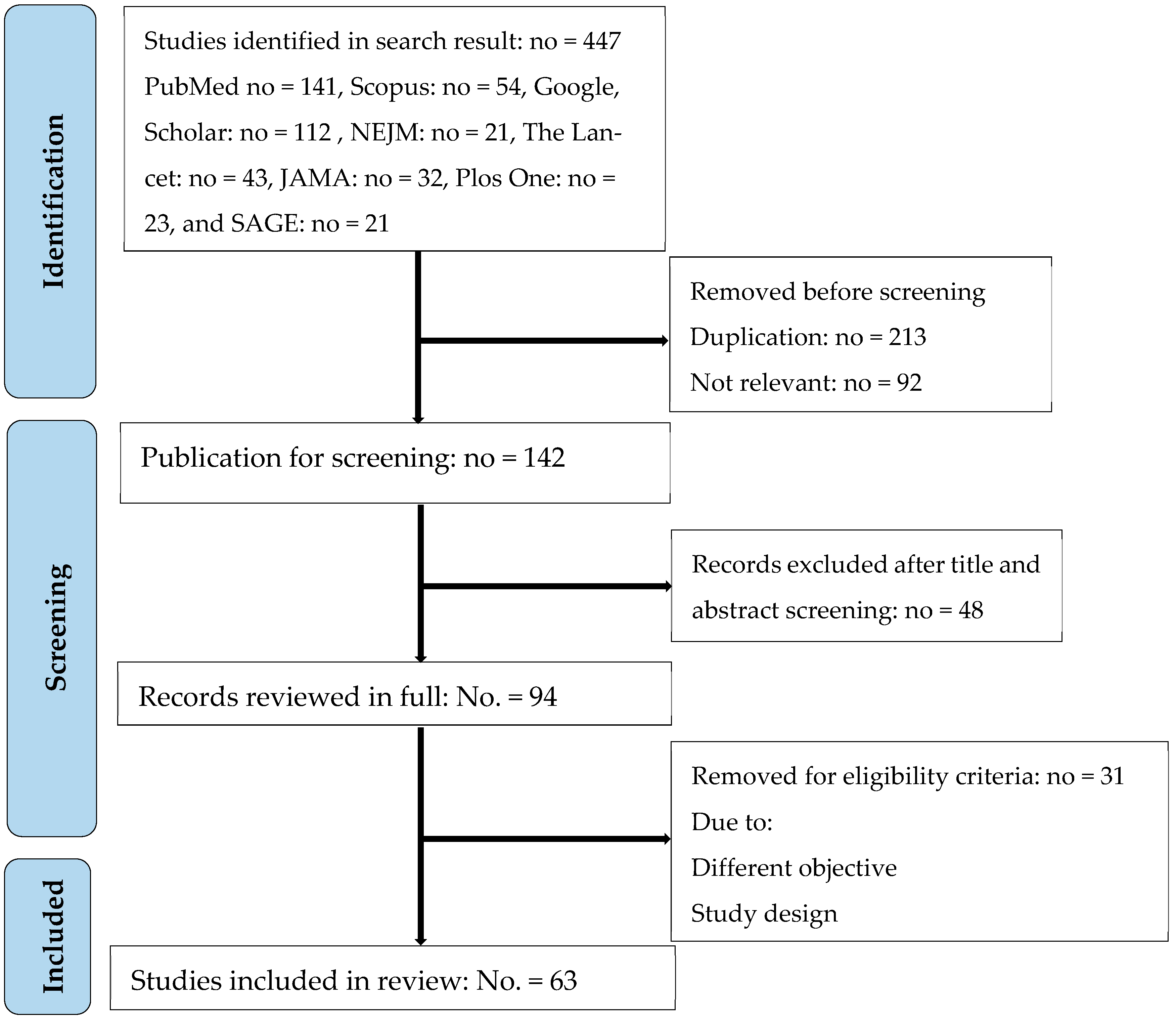
2. Materials and Methods
2.1. Study Design
2.2. Information Sources and Search Strategy
2.3. Eligibility Criteria
- Published in English in peer-reviewed journals between 2010 and 2023.
- Focused explicitly on telemedicine or digital health interventions within obstetrics and/or gynecology.
- Reported empirical data from rural and/or urban healthcare settings.
- Included application or evaluation of advanced technologies such as artificial intelligence (AI), mobile health (mHealth), or wearable devices.
- For COVID-19-era studies (2020–2023), explicit reference to the pandemic context or impact was required.
- Publications not in English.
- Studies focusing exclusively on telemedicine in unrelated specialties.
- Non-empirical works such as reviews without original data.
2.4. Study Selection and Data Extraction
2.5. Quality Appraisal
2.6. Data Synthesis and Analysis
2.7. Ethical Considerations
2.8. Limitations
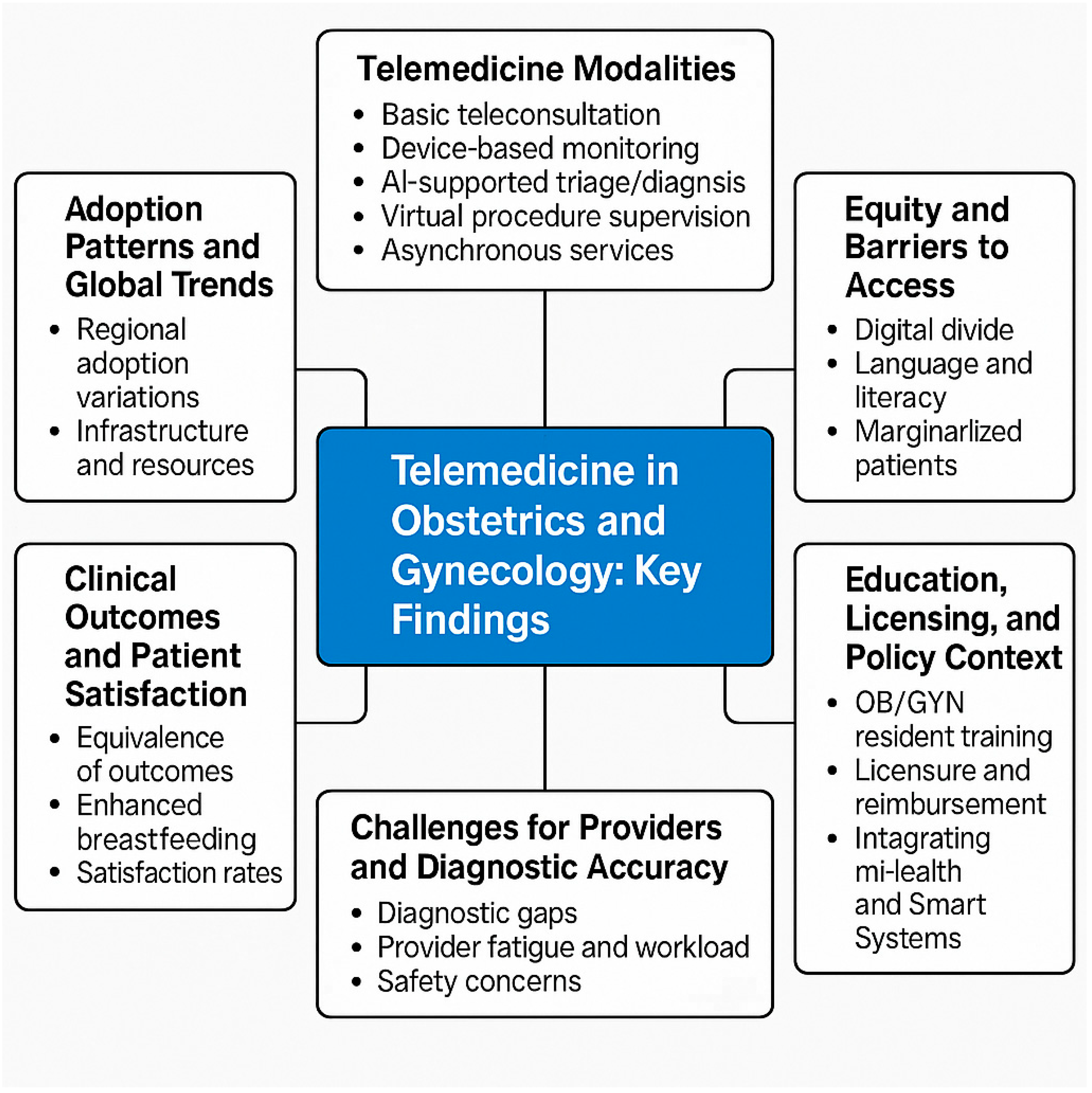
3. Results
3.1. COVID-19 as a Catalyst for Structural Transformation
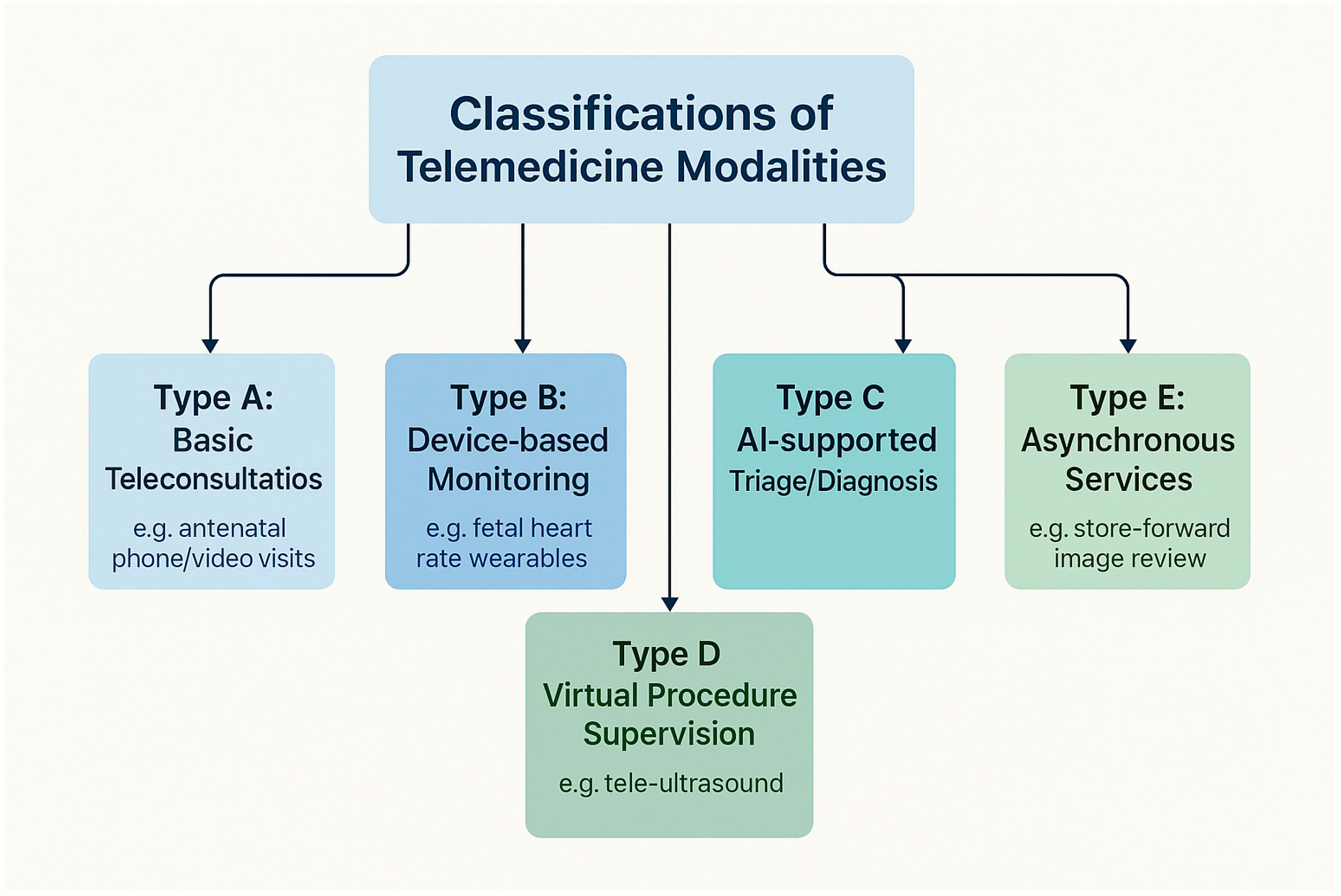
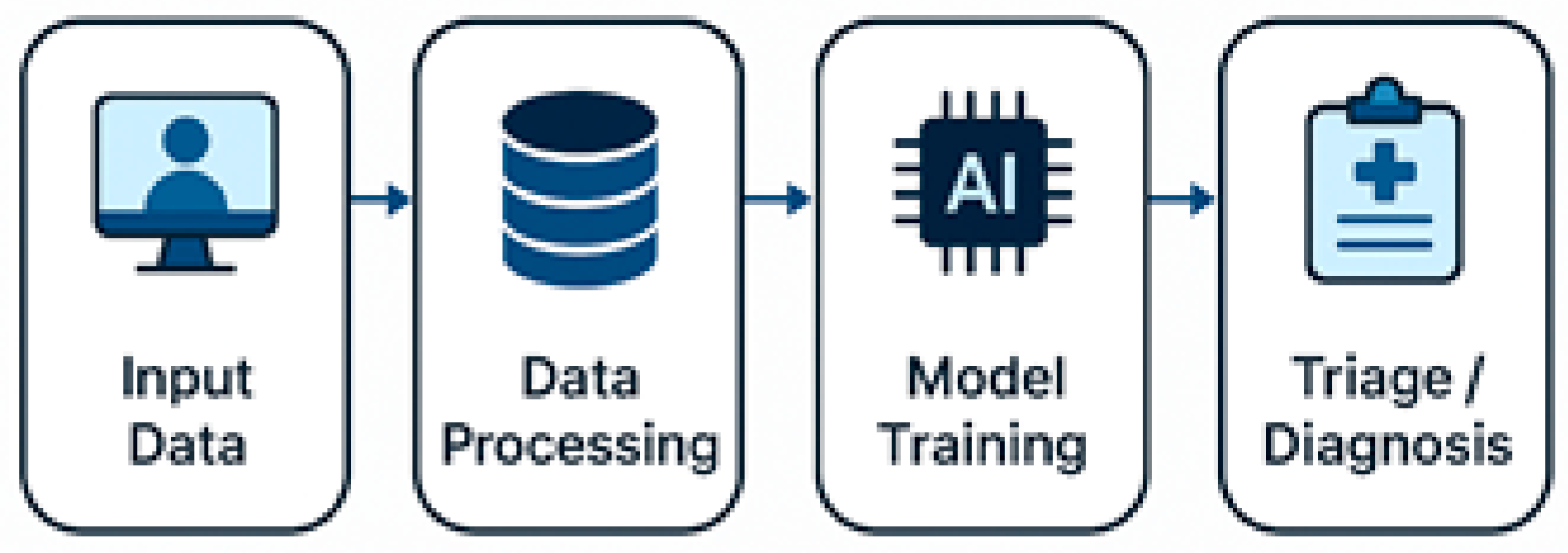
3.2. Modalities and Technological Innovations
3.3. Utilization Patterns and Health System Integration
3.4. Health Equity and Digital Divide
3.5. Clinical Effectiveness and Health Outcomes
3.6. Provider Experience and Readiness
3.7. Policy, Regulation, and Sustainability
| Theme | Telemedicine Modality/Key Findings | Clinical or System Outcomes | Geographic Focus | References |
|---|---|---|---|---|
| Modalities and Innovations | Synchronous (video/audio), asynchronous (store-and-forward), remote monitoring, AI triage, tele-guided ultrasound | +89% diagnostic concordance (AI); 35% faster triage; 22% improved hypertension detection | US, India, Brazil, Ethiopia | [1,14,15,22,26,27,34,46,50] |
| Utilization and Adoption | >500% increase during COVID-19; sustained 9–12% post-pandemic use; <30% coverage in some LMICs | Improved continuity; increased prenatal visit adherence | US, UK, Nigeria, Saudi Arabia | [5,13,14,24,27,35,38,43] |
| Equity and Accessibility | Barriers: internet access, language, digital literacy, cultural norms | 2.2× lower use in non-English speakers; 57% missed visits due to connectivity; 43% of rural clinics lacked internet | US, Senegal, Lebanon, Uganda, Sub-Saharan Africa | [18,19,27,28,54,55,56,57] |
| Clinical Effectiveness | Virtual prenatal/postnatal care; SMS/mHealth interventions | Equivalent maternal/neonatal outcomes; −3.1 PHQ-9 depression score; +15–20% breastfeeding rates | US, Brazil, Bangladesh, Nigeria, India | [4,11,14,22,24,31,38,40,46] |
| Provider Experience | Satisfaction, burnout, training gaps | 80% perceived benefit; 41–68% screen fatigue; <50% felt emotionally prepared | US, Saudi Arabia, Pakistan | [2,5,15,28,29,32,33,59] |
| Policy and Reimbursement | Licensing constraints; legal frameworks; reimbursement; data privacy | Limited cross-border services; 74% reduced telehealth post-funding | US, Latin America, Canada, Europe | [9,13,16,39,54,61,62] |
| Technology and AI Integration | mHealth apps; AI diagnostics; smart city platforms | +25–42% adherence; >90% cervical cancer AI sensitivity; 34% fewer transfers | Brazil, Saudi Arabia, Ethiopia, Ghana | [7,34,37,38,46,47,48] |
| COVID-19 as Catalyst | Pandemic-driven expansion; emergency tool implementation | 1818% funding increase; sustained hybrid models; 27% oncology treatment delays | Global and US | [24,39,41,42,43,58] |
| Reproductive Health in Adolescents | Tele-contraceptive and educational services | 41% adolescent preference for virtual visits; increased access in underserved areas | Kenya and US | [51,52] |
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| STROBE | Strengthening the Reporting of Observational Studies in Epidemiology |
| MMAT | Mixed Methods Appraisal Tool |
| CASP | Critical Appraisal Skills Program |
| JBI | Joanna Briggs Institute Critical Appraisal Tools |
| AMSTAR 2 | A Measurement Tool to Assess Systematic Reviews |
Appendix A
| No. | Author (s) | Study Design | Year | Location | Main Findings (Concise) |
|---|---|---|---|---|---|
| [1] | Garg S et al. | Review/Commentary | 2020 | India | Telemedicine rapidly embraced during COVID-19, enhancing virtual care delivery. |
| [2] | Hollander JE, Carr BG | Commentary | 2020 | USA | Telemedicine seen as essential and nearly “perfect” solution during COVID-19. |
| [3] | Barbosa W et al. | Review | 2021 | USA | Telemedicine improves access across multiple medical specialties. |
| [4] | Mbunge E et al. | Systematic Review | 2022 | South Africa | Digital health and virtual services deployed effectively in South Africa during COVID-19. |
| [5] | López Seguí F et al. | Cost-Minimization Analysis | 2020 | Catalonia, Spain | Telemedicine more efficient and cost-effective compared to usual care. |
| [6] | Pinnock H et al. | Review | 2022 | UK | Telemedicine and virtual respiratory care expanded during COVID-19. |
| [7] | Burrell DN | Dynamic Evaluation Study | 2023 | USA | Evaluates telehealth tech and AI applications in healthcare organizations. |
| [8] | Chia MA, Turner AW | Review | 2022 | Australia | AI and telemedicine integration benefits outreach eye care. |
| [9] | Haleem A et al. | Review | 2021 | India | Discusses capabilities, barriers, and applications of telemedicine. |
| [10] | Anawade PA et al. | Comprehensive Review | 2024 | India | Telemedicine positively impacts healthcare accessibility. |
| [11] | Amin S et al. | Cross-Sectional | 2024 | Bangladesh | Awareness and barriers to telemedicine adoption among patients identified. |
| [12] | Zobair KM et al. | Cross-Sectional | 2020 | Bangladesh | Barriers to telemedicine adoption in rural areas identified. |
| [13] | Al-Samarraie H et al. | Review | 2020 | Middle East | Progress and policy gaps in telemedicine in Middle Eastern countries. |
| [14] | Du Y et al. | Mixed Methods Study | 2022 | China | Factors affecting telemedicine use in rural China examined. |
| [15] | Arora S et al. | Scoping Review | 2024 | India | Challenges and facilitators of telemedicine implementation described. |
| [16] | Graf C et al. | Review | 2023 | Latin America | Telemedicine adoption in Latin American rheumatology post-COVID. |
| [17] | Haimi M | Narrative Review | 2023 | Not specified | Paradoxical effects of telemedicine on healthcare disparities highlighted. |
| [18] | Hamnvik O-PR et al. | Review/Commentary | 2020 | USA | Telemedicine access inequities in transgender healthcare explored. |
| [19] | Haynes N et al. | Commentary | 2021 | USA | Racial and ethnic disparities in telehealth usage addressed. |
| [20] | Masterson Creber R et al. | Scientific Statement | 2023 | USA | Telehealth and equity considerations in heart failure care in older adults. |
| [21] | Brown HL, Denicola N | Review | 2020 | USA | Telehealth use in maternity care reviewed. |
| [22] | Denicola N et al. | Systematic Review | 2020 | USA | Telehealth interventions improve obstetric and gynecologic outcomes. |
| [23] | Fix L et al. | Qualitative Study | 2020 | Australia | Patient experiences with at-home telemedicine for abortion analyzed. |
| [24] | Gyamfi-Bannerman G et al. | Cohort Study | 2020 | USA | Telehealth effective for high-risk pregnancy management during COVID-19. |
| [25] | Schummers L et al. | Observational Study | 2022 | Canada | Safety and use of medical abortion with telemedicine confirmed. |
| [26] | Lapadula MC et al. | Cross-Sectional Survey | 2021 | USA | High satisfaction with telemedicine prenatal consults during COVID-19. |
| [27] | Fryer K et al. | Implementation Study | 2020 | USA | Obstetric telehealth rapidly implemented during COVID-19. |
| [28] | Sengupta A et al. | Qualitative Study | 2023 | Australia | Telemedicine in specialist outpatient care during COVID-19 explored. |
| [29] | Smith WR et al. | Implementation Guide | 2020 | USA | Rapid outpatient telemedicine program integration during pandemic described. |
| [30] | Apathy NC et al. | Observational Study | 2023 | USA | Physician telemedicine usage varies significantly. |
| [31] | Kung LH et al. | Empirical Study | 2024 | Taiwan | Usage differences in telemedicine by rural vs. urban patients studied. |
| [32] | Iancu AM et al. | Commentary/Experience | 2020 | USA | Telemedicine in medical education during COVID-19 enhances student engagement. |
| [33] | Jumreornvong O et al. | Commentary/Review | 2020 | USA | Telemedicine’s role in medical education during COVID-19 expanded. |
| [34] | Ly BA et al. | Descriptive Study | 2017 | Senegal | Physician perceptions and determinants of telemedicine use described. |
| [35] | Wubante SM et al. | Cross-Sectional | 2022 | Ethiopia | Readiness of health professionals to implement telemedicine assessed. |
| [36] | Olufunlayo TF et al. | Cross-Sectional | 2023 | Nigeria | Telemedicine maturity assessed in tertiary hospitals. |
| [37] | Mohammadzadeh Z et al. | Systematic Review | 2023 | Developing Nations | Smart city healthcare tech and indicators reviewed. |
| [38] | Taha AR et al. | Cross-Sectional | 2022 | UAE | Integration of mHealth in telemedicine during COVID-19 described. |
| [39] | Zobair KM et al. | Predictive Modeling Study | 2021 | Bangladesh | Machine learning predicts telemedicine patient satisfaction. |
| [40] | Baughman DJ et al. | Comparative Study | 2022 | USA | Quality of care measures comparable between telemedicine and in-person visits. |
| [41] | Abdulwahab S, Zedan H | Cross-Sectional | 2021 | Saudi Arabia | Factors influencing patient satisfaction with telemedicine identified. |
| [42] | Palmer KR et al. | Interrupted Time Series | 2021 | Australia | Low-cost antenatal telehealth widely implemented during COVID-19. |
| [43] | Patel SY et al. | Observational Study | 2021 | USA | Community factors influencing telemedicine use during COVID-19 analyzed. |
| [44] | Reed M et al. | Observational Study | 2021 | USA | Telemedicine visits linked to comparable follow-up and treatment as in-person visits. |
| [45] | Larsen SB et al. | Descriptive/Policy Paper | 2015 | Denmark | Proposal for shared telemedicine service center. |
| [46] | Silva AB et al. | Regulatory Review | 2020 | Brazil | Telemedicine regulatory framework mapped over 30 years. |
| [47] | Sageena G et al. | Review | 2021 | India | Evolution of telemedicine during COVID-19 described. |
| [48] | MacDonald SM, Berv J | Commentary | 2022 | USA | Telemedicine may risk weakening patient–provider relationship. |
| [49] | Ncube B et al. | Exploratory Study | 2023 | Botswana | Patient and provider attitudes toward telemedicine examined. |
| [50] | Khatana SAM et al. | Database Analysis | 2022 | USA | Predictors of telemedicine use during COVID-19 identified. |
| [51] | Waqas A et al. | Bibliometric Analysis | 2020 | UK | Telemedicine research trends analyzed. |
| [52] | Tye ML et al. | Perception Survey | 2020 | USA | School-based telemedicine model perceptions evaluated. |
| [53] | Chiu CY et al. | Survey Study | 2021 | USA (NYC) | Internal medicine residents’ telemedicine experiences during COVID-19 documented. |
| [54] | Stoltzfus M et al. | Review | 2023 | India | Comprehensive telemedicine role update. |
| [55] | Hsueh L et al. | Observational Study | 2021 | USA | Limited English proficiency patients face disparities in video telemedicine use. |
| [56] | Eberly LA et al. | Observational Study | 2020 | USA | Patient factors influencing telemedicine access during COVID-19 studied. |
| [57] | Reed ME et al. | Observational Study | 2020 | USA | Patient characteristics associated with telemedicine choice analyzed. |
| [58] | Waseem N et al. | Observational Study | 2022 | USA | Telemedicine success disparities linked to adverse outcomes in thoracic cancer patients. |
| [59] | Demaerschalk BM et al. | Diagnostic Concordance Study | 2022 | USA | High diagnostic concordance between video telemedicine and in-person consultations. |
| [60] | Scott AC et al. | Program Description | 2020 | Australia | Cardiovascular telemedicine program improves rural healthcare. |
| [61] | Mehrotra A, Uscher-Pines L | Commentary | 2022 | USA | Telemedicine reimbursement knowledge gaps highlighted. |
| [62] | Mehrotra A et al. | Commentary | 2021 | USA | Telemedicine medical licensure reform discussed. |
| [63] | Wang Y et al. | Case Analysis | 2021 | China | Telemedicine application during COVID-19 pandemic analyzed. |
Appendix B. Full Search String
- Databases Searched:
- PubMed.
- Scopus.
- Google Scholar.
- Search Period:
- January 2010–December 2023.
- Search Strategy (example used in PubMed):
- (“telemedicine”[MeSH Terms] OR “telemedicine”[All Fields] OR “telehealth”[All Fields] OR “remote consultation”[All Fields]).
- AND (“obstetrics”[MeSH Terms] OR “obstetrics”[All Fields] OR “gynecology”[MeSH Terms] OR “gynecology”[All Fields]).
- AND (“rural health”[MeSH Terms] OR “rural healthcare”[All Fields] OR “urban health”[MeSH Terms] OR “urban healthcare”[All Fields]).
- AND (“digital literacy”[All Fields] OR “health literacy”[MeSH Terms]).
- AND (“artificial intelligence”[MeSH Terms] OR “AI”[All Fields] OR “machine learning”[All Fields]).
- AND (“COVID-19”[MeSH Terms] OR “pandemic”[All Fields]).
- Filters Applied:
- Language: English.
- Article type: Peer-reviewed articles.
- Study types: Empirical studies, program evaluations, case studies.
- Population: Human subjects.
- Additional Sources:
- Manual screening of reference lists from included studies.
Appendix C
Appendix D
| Study ID | Author (s) | Country | Study Design | Quality Assessment Tool | Overall Quality Rating |
|---|---|---|---|---|---|
| S1 | [2] | Bangladesh | Cross-sectional | STROBE | Moderate |
| S2 | [4] | India | Mixed methods | MMAT | High |
| S3 | [11] | China | Mixed methods | MMAT | Moderate |
| S4 | [12] | Australia | Qualitative | CASP | High |
| S5 | [13] | USA | Observational | STROBE | High |
| S6 | [14] | USA | Case series | JBI | Moderate |
| S7 | [17] | USA | Survey | STROBE | Moderate |
| S8 | [24] | Multi-country | Cohort | STROBE | High |
| S9 | [25] | South Africa | Systematic review | AMSTAR 2 | High |
| S10 | [34] | Bangladesh | Survey | STROBE | Moderate |
References
- Garg, S.; Gangadharan, N.; Bhatnagar, N.; Singh, M.M.; Raina, S.K.; Galwankar, S. Telemedicine: Embracing virtual care during COVID-19 pandemic. J. Fam. Med. Prim. Care 2020, 9, 4516–4520. [Google Scholar] [CrossRef]
- Hollander, J.E.; Carr, B.G. Virtually perfect? Telemedicine for COVID-19. N. Engl. J. Med. 2020, 382, 1679–1681. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, W.; Dorsey, E.R.; Zhou, K.; Waddell, E.; Myers, T. Improving access to care: Telemedicine across medical domains. Annu. Rev. Public Health 2021, 42, 463–481. [Google Scholar] [CrossRef]
- Mbunge, E.; Batani, J.; Gaobotse, G.; Muchemwa, B. Virtual healthcare services and digital health technologies deployed during coronavirus disease 2019 (COVID-19) pandemic in South Africa: A systematic review. Glob. Health J. 2022, 6, 102–113. [Google Scholar] [CrossRef]
- López Seguí, F.; García Cuyàs, F.; Vidal-Alaball, J.; Mendioroz Peña, J.; Gironès García, X.; Adroher Mas, C.; García-Altés, A.; Vidal-Alaball, J. A cost-minimization analysis of a medical record-based, store and forward and provider-to-provider telemedicine compared to usual care in Catalonia: More agile and efficient, especially for users. Int. J. Environ. Res. Public Health 2020, 17, 2008. [Google Scholar] [CrossRef]
- Pinnock, H.; Vogiatzis, I.; Murphie, P.; Poberezhets, V. Telemedicine and virtual respiratory care in the era of COVID-19. ERJ Open Res. 2022, 8, 00111-2022. [Google Scholar] [CrossRef] [PubMed]
- Burrell, D.N. Dynamic evaluation approaches to telehealth technologies and artificial intelligence (AI) telemedicine applications in healthcare and biotechnology organizations. Merits 2023, 3, 700–721. [Google Scholar] [CrossRef]
- Chia, M.A.; Turner, A.W. Benefits of integrating telemedicine and artificial intelligence into outreach eye care: Stepwise approach and future directions. Front. Med. 2022, 9, 835804. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens. Int. 2021, 2, 100117. [Google Scholar] [CrossRef] [PubMed]
- Anawade, P.A.; Sharma, D.; Gahane, S. A comprehensive review on exploring the impact of telemedicine on healthcare accessibility. Cureus 2024, 16, e55996. [Google Scholar] [CrossRef]
- Amin, S.; Mustofa, M.; Barman, H.; Rahman, A. An exploratory cross-sectional study of awareness and barriers to adoption of telemedicine services among patients in Bangladesh. Future Health 2024, 2, 107–113. [Google Scholar] [CrossRef]
- Zobair, K.M.; Sanzogni, L.; Sandhu, K. Telemedicine healthcare service adoption barriers in rural Bangladesh. Australas. J. Inf. Syst. 2020, 24. [Google Scholar] [CrossRef]
- Al-Samarraie, H.; Ghazal, S.; Alzahrani, A.I.; Moody, L. Telemedicine in Middle Eastern countries: Progress, barriers, and policy recommendations. Int. J. Med. Inform. 2020, 141, 104232. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.; Tang, W.; Xue, H.; Sylvia, S.; Zhang, Z.; Hoelzer, S.; Zhou, Q.; Cheng, W.; Liang, Y.; Ma, X.; et al. Factors influencing adoption and use of telemedicine services in rural areas of China: Mixed methods study. JMIR Public Health Surveill. 2022, 8, e40771. [Google Scholar] [CrossRef]
- Arora, S.; Huda, R.K.; Verma, S.; Khetan, M.; Sangwan, R.K. Challenges, barriers, and facilitators in telemedicine implementation in India: A scoping review. Cureus 2024, 16, e67388. [Google Scholar] [CrossRef]
- Graf, C.; Soriano, E.R.; Fernández-Ávila, D.G.; Plazzotta, F. Telehealth and telemedicine in Latin American rheumatology, a new era after COVID-19. J. Clin. Rheumatol. 2023, 29, 165–169. [Google Scholar] [CrossRef]
- Haimi, M. The tragic paradoxical effect of telemedicine on healthcare disparities—A time for redemption: A narrative review. BMC Med. Inform. Decis. Mak. 2023, 23, 95. [Google Scholar] [CrossRef]
- Hamnvik, O.-P.R.; Ahnallen, C.G.; Agarwal, S.; Reisner, S.L.; Goldman, A.L. Telemedicine and inequities in health care access: The example of transgender health. Transgend. Health 2020, 7, 113–116. [Google Scholar] [CrossRef]
- Haynes, N.; Haynes, M.; Swain, J.; Nunes, K.; Gumbs, E.; Ezekwesili, A. “Can you see my screen?” Addressing racial and ethnic disparities in telehealth. Curr. Cardiol. Risk Rep. 2021, 15, 23. [Google Scholar] [CrossRef]
- Masterson Creber, R.; Bidwell, J.; Harmon Still, C.; Dodson, J.A.; Lyles, C.; Ooi, S.Y.; Breathett, K.; Yancy, C.; Kitsiou, S. Telehealth and health equity in older adults with heart failure: A scientific statement from the American Heart Association. Circ. Cardiovasc. Qual. Outcomes 2023, 16, e0000123. [Google Scholar] [CrossRef] [PubMed]
- Brown, H.L.; Denicola, N. Telehealth in maternity care. Obstet. Gynecol. Clin. N. Am. 2020, 47, 497–502. [Google Scholar] [CrossRef]
- Denicola, N.; Witkop, C.T.; Sonalkar, S.; Henderson, J.T.; Butler Tobah, Y.S.; Ganju, N.; Grossman, D.; Marko, K.; Butler, J.; Lowery, C.; et al. Telehealth interventions to improve obstetric and gynecologic health outcomes: A systematic review. Obstet. Gynecol. 2020, 135, 371–382. [Google Scholar] [CrossRef]
- Fix, L.; Mazza, D.; Sandhu, M.V.; Seymour, J.W.; Thompson, T.-A.; Melville, C. At-home telemedicine for medical abortion in Australia: A qualitative study of patient experiences and recommendations. BMJ Sex. Reprod. Health 2020, 46, 172–176. [Google Scholar] [CrossRef] [PubMed]
- Gyamfi-Bannerman, C.; Friedman, A.M.; Aziz, A.; Yates, H.S.; Miller, R.S.; Moroz, L.; Zork, N.; Aubey, J.J.; Baptiste, C.D.; D’Alton, M.E.; et al. Telehealth for high-risk pregnancies in the setting of the COVID-19 pandemic. Am. J. Perinatol. 2020, 37, 800–808. [Google Scholar] [CrossRef] [PubMed]
- Schummers, L.; Darling, E.K.; Dunn, S.; McGrail, K.; Gayowsky, A.; Law, M.R.; Laba, T.-L.; Kaczorowski, J.; Norman, W.V. Abortion safety and use with normally prescribed mifepristone in Canada. N. Engl. J. Med. 2022, 386, 57–67. [Google Scholar] [CrossRef]
- Lapadula, M.C.; Clark, T.; Makkar, A.; Szyld, E.G.; Rolfs, S.; Hallford, G.; McCoy, M.; McKnight, S. Evaluating patients’ and neonatologists’ satisfaction with the use of telemedicine for neonatology prenatal consultations during the COVID-19 pandemic. Front. Pediatr. 2021, 9, 642369. [Google Scholar] [CrossRef]
- Fryer, K.; Foti, T.; Delgado, A.; Reid, C.N.; Marshall, J. Implementation of obstetric telehealth during COVID-19 and beyond. Matern. Child Health J. 2020, 24, 1104–1110. [Google Scholar] [CrossRef]
- Sengupta, A.; Jenkins, C.R.; Pettigrew, S. Telemedicine in specialist outpatient care during COVID-19: A qualitative study. Intern. Med. J. 2023, 54, 54–61. [Google Scholar] [CrossRef]
- Smith, W.R.; Atala, A.J.; Terlecki, R.P.; Kelly, E.E.; Matthews, C.A. Implementation guide for rapid integration of an outpatient telemedicine program during the COVID-19 pandemic. J. Am. Coll. Surg. 2020, 231, 216–222.e2. [Google Scholar] [CrossRef] [PubMed]
- Apathy, N.C.; Dixit, R.A.; Boxley, C.L.; Adams, K.T.; Booker, E.; Ratwani, R.M. Variations in physician telemedicine provision. JAMA Netw. Open 2023, 6, e2321955. [Google Scholar] [CrossRef]
- Kung, L.H.; Yan, Y.H.; Kung, C.M. Empirical study on the usage of telemedicine by rural and urban health care consumers in Taiwan: Integrating the perspectives of technology acceptance model and theory of planned behavior. Telemed. J. E-Health 2024, 30, 2630–2636. [Google Scholar] [CrossRef]
- Iancu, A.M.; Alam, H.B.; Kemp, M.T. Unmuting medical students’ education: Utilizing telemedicine during the COVID-19 pandemic and beyond. J. Med. Internet Res. 2020, 22, e19667. [Google Scholar] [CrossRef]
- Jumreornvong, O.; Appel, J.; Race, J.; Yang, E. Telemedicine and medical education in the age of COVID-19. Acad. Med. 2020, 95, 1838–1843. [Google Scholar] [CrossRef]
- Ly, B.A.; Labonté, R.; Bourgeault, I.L.; Niang, M.N. The individual and contextual determinants of the use of telemedicine: A descriptive study of the perceptions of Senegal’s physicians and telemedicine projects managers. PLoS ONE 2017, 12, e0181070. [Google Scholar] [CrossRef]
- Wubante, S.M.; Nigatu, A.M.; Jemere, A.T. Health professionals’ readiness and its associated factors to implement telemedicine system at private hospitals in Amhara region, Ethiopia 2021. PLoS ONE 2022, 17, e0275133. [Google Scholar] [CrossRef] [PubMed]
- Olufunlayo, T.F.; Ojo, O.O.; Ozoh, O.B.; Agabi, O.P.; Opara, C.R.; Taiwo, F.T.; A Fasanmade, O.; Okubadejo, N.U. Telemedicine ready or not? A cross-sectional assessment of telemedicine maturity of federally funded tertiary health institutions in Nigeria. Digit. Health 2023, 9, 20552076221150072. [Google Scholar] [CrossRef] [PubMed]
- Mohammadzadeh, Z.; Saeidnia, H.R.; Lotfata, A.; Hassanzadeh, M.; Ghiasi, N. Smart city healthcare delivery innovations: A systematic review of essential technologies and indicators for developing nations. BMC Health Serv. Res. 2023, 23, 236. [Google Scholar] [CrossRef] [PubMed]
- Taha, A.R.; Shehadeh, M.; Alshehhi, A.; Altamimi, T.; Housser, E.; Simsekler, M.C.E.; Alfalasi, B.; Al Memari, S.; Al Hosani, F.; Al Zaabi, Y.; et al. The integration of mHealth technologies in telemedicine during the COVID-19 era: A cross-sectional study. PLoS ONE 2022, 17, e0264436. [Google Scholar] [CrossRef]
- Zobair, K.M.; Islam, M.Z.; Houghton, L.; Sanzogni, L. Forecasting care seekers’ satisfaction with telemedicine using machine learning and structural equation modelling. PLoS ONE 2021, 16, e0257300. [Google Scholar] [CrossRef]
- Baughman, D.J.; Jabbarpour, Y.; Westfall, J.M.; Jetty, A.; Zain, A.; Baughman, K.; Pollak, B.; Waheed, A. Comparison of quality performance measures for patients receiving in-person vs telemedicine primary care in a large integrated health system. JAMA Netw. Open 2022, 5, e2233267. [Google Scholar] [CrossRef]
- Abdulwahab, S.; Zedan, H. Factors affecting patient perceptions and satisfaction with telemedicine in outpatient clinics. J. Patient Exp. 2021, 8, 23743735211063780. [Google Scholar] [CrossRef]
- Palmer, K.R.; Tanner, M.; Davies-Tuck, M.; Rindt, A.; Papacostas, K.; Giles, M.L.; Brown, K.; Diamandis, H.; Fradkin, R.; E Stewart, A.; et al. Widespread implementation of a low-cost telehealth service in the delivery of antenatal care during the COVID-19 pandemic: An interrupted time-series analysis. Lancet 2021, 398, 41–52. [Google Scholar] [CrossRef]
- Patel, S.Y.; Rose, S.; Barnett, M.L.; Huskamp, H.A.; Uscher-Pines, L.; Mehrotra, A. Community factors associated with telemedicine use during the COVID-19 pandemic. JAMA Netw. Open 2021, 4, e2110330. [Google Scholar] [CrossRef] [PubMed]
- Reed, M.; Huang, J.; Graetz, I.; Muelly, E.; Millman, A.; Lee, C. Treatment and follow-up care associated with patient-scheduled primary care telemedicine and in-person visits in a large integrated health system. JAMA Netw. Open 2021, 4, e2132793. [Google Scholar] [CrossRef] [PubMed]
- Larsen, S.B.; Sørensen, N.S.; Petersen, M.G.; Kjeldsen, G.F. Towards a shared service center for telemedicine: Telemedicine in Denmark, and a possible way forward. Health Inform. J. 2015, 22, 815–827. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.B.; da Silva, R.M.; Ribeiro, G.d.R.; Guedes, A.C.C.M.; Santos, D.L.; Nepomuceno, C.C.; Caetano, R.; Makkar, A. Three decades of telemedicine in Brazil: Mapping the regulatory framework from 1990 to 2018. PLoS ONE 2020, 15, e0242869. [Google Scholar] [CrossRef]
- Sageena, G.; Kapur, A.; Sharma, M. Evolution of smart healthcare: Telemedicine during COVID-19 pandemic. J. Inst. Eng. India Ser. B 2021, 102, 1319–1324. [Google Scholar] [CrossRef]
- MacDonald, S.M.; Berv, J. Losing contact—COVID-19, telemedicine, and the patient-provider relationship. N. Engl. J. Med. 2022, 387, 775–777. [Google Scholar] [CrossRef] [PubMed]
- Ncube, B.; Mars, M.; Scott, R.E. Perceptions and attitudes of patients and healthcare workers towards the use of telemedicine in Botswana: An exploratory study. PLoS ONE 2023, 18, e0281754. [Google Scholar] [CrossRef]
- Khatana, S.A.M.; Yang, L.; Eberly, L.A.; Julien, H.M.; Adusumalli, S.; Groeneveld, P.W. Predictors of telemedicine use during the COVID-19 pandemic in the United States: An analysis of a national electronic medical record database. PLoS ONE 2022, 17, e0269535. [Google Scholar] [CrossRef]
- Waqas, A.; Teoh, S.H.; Lapão, L.V.; Messina, L.A.; Correia, J.C. Harnessing telemedicine for the provision of health care: Bibliometric and scientometric analysis. J. Med. Internet Res. 2020, 22, e18835. [Google Scholar] [CrossRef] [PubMed]
- Tye, M.L.; Honey, M.; Day, K. School-based telemedicine: Perceptions about a telemedicine model of care. Health Inform. J. 2020, 26, 2030–2041. [Google Scholar] [CrossRef] [PubMed]
- Chiu, C.Y.; Sarwal, A.; Jawed, M.; Chemarthi, V.S.; Shabarek, N. Telemedicine experience of NYC internal medicine residents during COVID-19 pandemic. PLoS ONE 2021, 16, e0246762. [Google Scholar] [CrossRef]
- Stoltzfus, M.; Kaur, A.; Chawla, A.; Anamika, F.N.U.; Jain, R.; Gupta, V. The role of telemedicine in healthcare: An overview and update. Egypt. J. Intern. Med. 2023, 35, 26. [Google Scholar] [CrossRef]
- Hsueh, L.; Huang, J.; Millman, A.K.; Gopalan, A.; Parikh, R.K.; Teran, S.; Reed, M.E. Disparities in use of video telemedicine among patients with limited English proficiency during the COVID-19 pandemic. JAMA Netw. Open 2021, 4, e2133129. [Google Scholar] [CrossRef]
- Eberly, L.A.; Kallan, M.J.; Julien, H.M.; Haynes, N.; Khatana, S.A.M.; Nathan, A.S.; Snider, C.; Chokshi, N.P.; Eneanya, N.D.; Takvorian, S.U.; et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw. Open 2020, 3, e2031640. [Google Scholar] [CrossRef]
- Reed, M.E.; Huang, J.; Graetz, I.; Lee, C.; Muelly, E.; Kennedy, C.; Kim, E. Patient characteristics associated with choosing a telemedicine visit vs office visit with the same primary care clinicians. JAMA Netw. Open 2020, 3, e205873. [Google Scholar] [CrossRef]
- Waseem, N.; Boulanger, M.; Yanek, L.R.; Feliciano, J.L. Disparities in telemedicine success and their association with adverse outcomes in patients with thoracic cancer during the COVID-19 pandemic. JAMA Netw. Open 2022, 5, e2220543. [Google Scholar] [CrossRef]
- Demaerschalk, B.M.; Pines, A.; Butterfield, R.; Haglin, J.M.; Haddad, T.C.; Yiannias, J.; Colby, C.E.; TerKonda, S.P.; Ommen, S.R.; Bushman, M.S.; et al. Assessment of clinician diagnostic concordance with video telemedicine in the integrated multispecialty practice at Mayo Clinic during the beginning of COVID-19 pandemic from March to June 2020. JAMA Netw. Open 2022, 5, e2229958. [Google Scholar] [CrossRef]
- Scott, A.C.; McDonald, A.; Roberts, T.; Martin, C.; Manns, T.; Webster, M.; Walker, D.; Sandford, A.; Scuffham, P.; Atherton, J.J. Cardiovascular telemedicine program in rural Australia. N. Engl. J. Med. 2020, 383, 883–884. [Google Scholar] [CrossRef] [PubMed]
- Mehrotra, A.; Uscher-Pines, L. Informing the debate about telemedicine reimbursement—What do we need to know? N. Engl. J. Med. 2022, 387, 1821–1823. [Google Scholar] [CrossRef] [PubMed]
- Mehrotra, A.; Nimgaonkar, A.; Richman, B. Telemedicine and medical licensure—Potential paths for reform. N. Engl. J. Med. 2021, 384, 687–690. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Yang, J.; Ma, H.; Dong, X.; Xie, G.; Ye, S.; Du, J. Application of telemedicine in the COVID-19 epidemic: An analysis of Gansu Province in China. PLoS ONE 2021, 16, e0249872. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Medani, I.E.; Hakami, A.M.; Chourasia, U.H.; Rahamtalla, B.; Adawi, N.M.; Fadailu, M.; Salih, A.; Abdelmola, A.; Hashim, K.N.; Dawelbait, A.M.; et al. Telemedicine in Obstetrics and Gynecology: A Scoping Review of Enhancing Access and Outcomes in Modern Healthcare. Healthcare 2025, 13, 2036. https://doi.org/10.3390/healthcare13162036
Medani IE, Hakami AM, Chourasia UH, Rahamtalla B, Adawi NM, Fadailu M, Salih A, Abdelmola A, Hashim KN, Dawelbait AM, et al. Telemedicine in Obstetrics and Gynecology: A Scoping Review of Enhancing Access and Outcomes in Modern Healthcare. Healthcare. 2025; 13(16):2036. https://doi.org/10.3390/healthcare13162036
Chicago/Turabian StyleMedani, Isameldin Elamin, Ahlam Mohammed Hakami, Uma Hemant Chourasia, Babiker Rahamtalla, Naser Mohsen Adawi, Marwa Fadailu, Abeer Salih, Amani Abdelmola, Khalid Nasralla Hashim, Azza Mohamed Dawelbait, and et al. 2025. "Telemedicine in Obstetrics and Gynecology: A Scoping Review of Enhancing Access and Outcomes in Modern Healthcare" Healthcare 13, no. 16: 2036. https://doi.org/10.3390/healthcare13162036
APA StyleMedani, I. E., Hakami, A. M., Chourasia, U. H., Rahamtalla, B., Adawi, N. M., Fadailu, M., Salih, A., Abdelmola, A., Hashim, K. N., Dawelbait, A. M., Yousf, N. M., Hassan, N. M., Ali, N. A., & Rizig, A. A. (2025). Telemedicine in Obstetrics and Gynecology: A Scoping Review of Enhancing Access and Outcomes in Modern Healthcare. Healthcare, 13(16), 2036. https://doi.org/10.3390/healthcare13162036






