Understanding No-Show Patterns in Healthcare: A Retrospective Study from Northern Italy †
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Collection
2.2. Statistical Analysis
3. Results
3.1. Bivariate Analysis
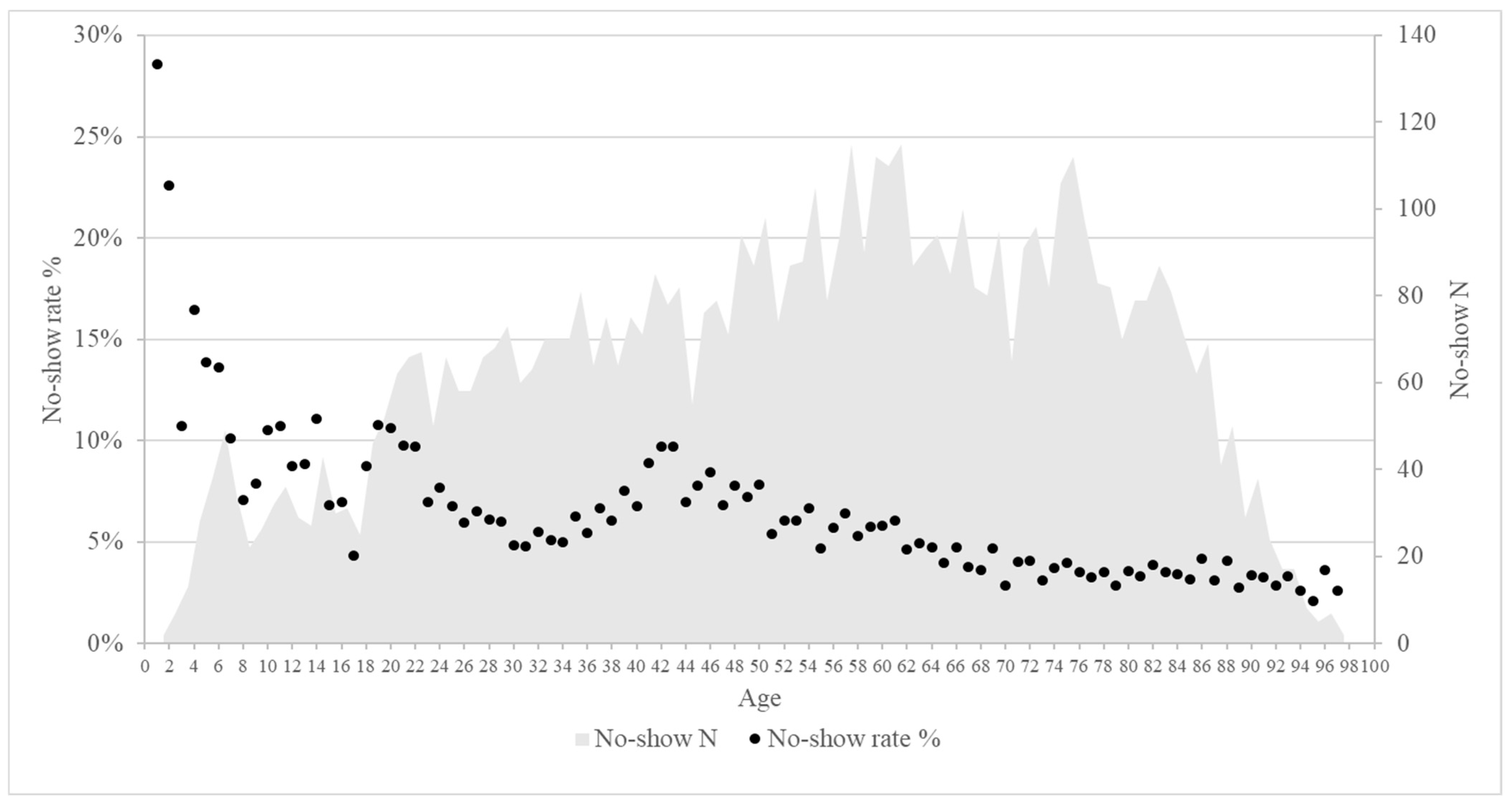
3.2. Patient Characteristics and No-Show Percentages
3.3. Logistic Regression Analysis of Predictors for No-Show
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Khan, Z.; Khan, Z. The Emerging Challenges and Strengths of the National Health Services: A Physician Perspective. Cureus 2023, 15, e38617. [Google Scholar] [CrossRef] [PubMed]
- Signorelli, C.; Odone, A.; Oradini-Alacreu, A.; Pelissero, G. Universal Health Coverage in Italy: Lights and shades of the Italian National Health Service which celebrated its 40th anniversary. Health Policy 2020, 124, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Dantas, L.F.; Fleck, J.L.; Cyrino Oliveira, F.L.; Hamacher, S. No-shows in appointment scheduling—A systematic literature review. Health Policy 2018, 122, 412–421. [Google Scholar] [CrossRef] [PubMed]
- Bech, M. The economics of non-attendance and the expected effect of charging a fine on non-attendees. Health Policy 2005, 74, 181–191. [Google Scholar] [CrossRef]
- Shah, S.J.; Cronin, P.; Hong, C.S.; Hwang, A.S.; Ashburner, J.M.; Bearnot, B.I.; A Richardson, C.; Fosburgh, B.W.; Kimball, A.B. Targeted Reminder Phone Calls to Patients at High Risk of No-Show for Primary Care Appointment: A Randomized Trial. J. Gen. Intern. Med. 2016, 31, 1460–1466. [Google Scholar] [CrossRef]
- Marbouh, D.; Khaleel, I.; Shanqiti KAl Tamimi MAl Simsekler, M.C.E.; Ellahham, S.; Alibazoglu, D.; Alibazoglu, H. Evaluating the Impact of Patient No-Shows on Service Quality. Risk Manag. Healthc. Policy 2020, 13, 509–517. [Google Scholar] [CrossRef]
- Barrera Ferro, D.; Brailsford, S.; Bravo, C.; Smith, H. Improving healthcare access management by predicting patient no-show behaviour. Decis. Support. Syst. 2020, 138, 113398. [Google Scholar] [CrossRef]
- Kheirkhah, P.; Feng, Q.; Travis, L.M.; Tavakoli-Tabasi, S.; Sharafkhaneh, A. Prevalence, predictors and economic consequences of no-shows. BMC Health Serv. Res. 2016, 16, 13. [Google Scholar] [CrossRef]
- Parente, C.A.; Salvatore, D.; Gallo, G.M.; Cipollini, F. Using overbooking to manage no-shows in an Italian healthcare center. BMC Health Serv. Res. 2018, 18, 185. [Google Scholar] [CrossRef] [PubMed]
- Oikonomidi, T.; Norman, G.; McGarrigle, L.; Stokes, J.; Van Der Veer, S.N.; Dowding, D. Predictive model-based interventions to reduce outpatient no-shows: A rapid systematic review. J. Am. Med. Inf. Assoc. 2023, 30, 559–569. [Google Scholar] [CrossRef]
- Parikh, A.; Gupta, K.; Wilson, A.C.; Fields, K.; Cosgrove, N.M.; Kostis, J.B. The effectiveness of outpatient appointment reminder systems in reducing no-show rates. Am. J. Med. 2010, 123, 542–548. [Google Scholar] [CrossRef] [PubMed]
- Xie, X.; Fan, Z.; Zhong, X. Appointment Capacity Planning With Overbooking for Outpatient Clinics With Patient No-Shows. IEEE Trans. Autom. Sci. Eng. 2022, 19, 864–883. [Google Scholar] [CrossRef]
- Laganga, L.R.; Lawrence, S.R. Clinic Overbooking to Improve Patient Access and Increase Provider Productivity. Decis. Sci. 2007, 38, 251–276. [Google Scholar] [CrossRef]
- Ministero Della Salute. Piano Nazionale di Governo Delle Liste di Attesa Per il Triennio 2019–2021. 2019. Available online: https://www.salute.gov.it/portale/listeAttesa/dettaglioPubblicazioniListeAttesa.jsp?lingua=italiano&id=2824 (accessed on 16 September 2024).
- Regione Piemonte. D.G.R. n. 20-6920. Approvazione Della Rimodulazione del Piano Operativo Regionale Per il Recupero Delle Liste di Attesa Delle Prestazioni di Specialistica Ambulatoriale, di Ricovero e di Screening Oncologici. 2023. Available online: https://www.regione.piemonte.it/web/temi/sanita/accesso-ai-servizi-sanitari/tempi-attesa (accessed on 16 September 2024).
- QuotidianoSanità. Liste D’attesa. Piemonte Approva Riparto Risorse Aggiuntive. 2022. Available online: https://www.quotidianosanita.it/piemonte/articolo.php?articolo_id=104098 (accessed on 16 September 2024).
- Azienda Sanitaria Locale “Città di Torino.” Strutture Territoriali. Available online: https://www.aslcittaditorino.it/strutture-sanitarie/strutture-territoriali/ (accessed on 16 September 2024).
- Servizio Statistica Della Città di Torino. Dati Statistici. Available online: http://www.comune.torino.it/statistica/dati/demog.htm (accessed on 16 September 2024).
- Ragusa, P.; Russotto, A.; Catozzi, D.; De Angelis, A.; Durbano, A.; Orecchia, S.; Siliquini, R. Managing no-shows in healthcare: Insights from an urban Health District in Northern Italy. Eur. J. Public Health 2024, 34, ckae144.1622. [Google Scholar] [CrossRef]
- Steyerberg, E.W. Clinical Prediction Models; Springer Nature: Dordrecht, The Netherlands, 2009. [Google Scholar] [CrossRef]
- Harrell, F.E. Regression Modeling Strategies; Springer Nature: Dordrecht, The Netherlands, 2001. [Google Scholar] [CrossRef]
- Kaplan-Lewis, E.; Percac-Lima, S. No-Show to Primary Care Appointments. J. Prim. Care Community Health 2013, 4, 251–255. [Google Scholar] [CrossRef] [PubMed]
- Cavalieri, M. Geographical variation of unmet medical needs in Italy: A multivariate logistic regression analysis. Int. J. Health Geogr. 2013, 12, 27. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.J.; Chae, E.; Peterson, E.; Ko, A.B. Predictors of repeated “no-showing” to clinic appointments. Am. J. Otolaryngol. 2015, 36, 411–414. [Google Scholar] [CrossRef] [PubMed]
- De Vito, E.; De Waure, C.; Specchia, M.L.; Parente, P.; Azzolini, E.; Frisicale, E.M.; Favale, M.; Teleman, A.A.; Ricciardi, W. Are undocumented migrants’ entitlements and barriers to healthcare a public health challenge for the European Union? Public Health Rev. 2016, 37, 13. [Google Scholar] [CrossRef] [PubMed]
- Wolff, D.L.; Waldorff, F.B.; von Plessen, C.; Mogensen, C.B.; Sørensen, T.L.; Houlind, K.C.; Bogh, S.B.; Rubin, K.H. Rate and predictors for non-attendance of patients undergoing hospital outpatient treatment for chronic diseases: A register-based cohort study. BMC Health Serv. Res. 2019, 19, 386. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.E.; Anisimowicz, Y.; Miedema, B.; Hogg, W.; Wodchis, W.P.; Aubrey-Bassler, K. The influence of gender and other patient characteristics on health care-seeking behaviour: A QUALICOPC study. BMC Fam. Pract. 2016, 17, 38. [Google Scholar] [CrossRef] [PubMed]
| Variable | No-Show * | Show * | p-Value | No-Show Percentage (%) ** |
|---|---|---|---|---|
| Characteristics of the healthcare services | ||||
| Healthcare services sites, n (%) | <0.001 1 | |||
| Site 1 | 2638 (42.6%) | 57,929 (50.7%) | 4.4% | |
| Site 2 | 2262 (36.5%) | 31,078 (27.2%) | 6.8% | |
| Site 3 | 1298 (20.9%) | 25,200 (22.1%) | 4.9% | |
| Healthcare services categories, n (%) | <0.001 1 | |||
| First access | 2441 (39.4%) | 37,430 (32.8%) | 6.1% | |
| Others | 3757 (60.6%) | 76,777 (67.2%) | 4.7% | |
| Healthcare services priority, n (%) | <0.001 1 | |||
| Urgent | 7 (0.1%) | 315 (0.3%) | 2.2% | |
| Short-term | 474 (7.6%) | 14,065 (12.3%) | 3.3% | |
| Deferrable | 1702 (27.5%) | 25,486 (22.3%) | 6.3% | |
| Schedulable | 4015 (64.8%) | 74,341 (65.1%) | 5.1% | |
| Specialty type, n (%) | <0.001 1 | |||
| Anaesthesiology/Analgesia | 74 (1.2%) | 2174 (1.9%) | 3.3% | |
| Cardiology | 1466 (23.7%) | 29,472 (25.8%) | 4.7% | |
| Dentistry and Stomatology | 821 (13.3%) | 7231 (6.3%) | 10.2% | |
| Dermatology | 257 (4.2%) | 3756 (3.3%) | 6.4% | |
| Diabetology | 307 (5%) | 3623 (3.2%) | 7.8% | |
| Endocrinology | 309 (5%) | 4601 (4%) | 6.3% | |
| General Surgery | 94 (1.5%) | 1744 (1.5%) | 5.1% | |
| Geriatrics | 68 (1.1%) | 1874 (1.6%) | 3.5% | |
| Neurology | 278 (4.5%) | 4500 (3.9%) | 5.8% | |
| Obstetrics and Gynaecology | 502 (8.1%) | 11,969 (10.5%) | 4% | |
| Ophthalmology | 600 (9.7%) | 10,305 (9%) | 5.5% | |
| Orthopaedics and Traumatology | 553 (8.9%) | 7071 (6.2%) | 7.3% | |
| Otorhinolaryngology | 556 (9%) | 7434 (6.5%) | 7% | |
| Rheumatology | 86 (1.4%) | 1622 (1.4%) | 5% | |
| Urology | 118 (1.9%) | 4148 (3.6%) | 2.8% | |
| Other Specialties | 109 (1.8%) | 12,683 (11.1%) | 0.9% | |
| Co-payment value in euros, median (IQR) | 20.7 (12.9–20.7) | 20.7 (12.9–20.7) | NS 2 | / |
| Waiting days, median (IQR) | 70 (21–130) | 21 (6–75) | <0.001 2 | / |
| Patients’ characteristics | ||||
| Gender, n (%) | <0.001 1 | |||
| Male | 2705 (43.7%) | 46,790 (41%) | 5.5% | |
| Female | 3493 (56.3%) | 67,417 (59%) | 4.9% | |
| Age, n (%) | <0.001 1 | |||
| <18 years | 472 (7.6%) | 4592 (4.0%) | 9.3% | |
| 18–65 years | 3634 (58.6%) | 53,496 (46.8%) | 6.4% | |
| >65 years | 2092 (33.8%) | 56,119 (49.1%) | 3.6% | |
| Residency, n (%) | <0.001 1 | |||
| Turin | 4897 (79%) | 92,343 (80.9%) | 5% | |
| Turin Province | 949 (15.3%) | 17,784 (15.6%) | 5.1% | |
| Piedmont | 100 (1.6%) | 1402 (1.2%) | 6.7% | |
| Italy | 150 (2.4%) | 1887 (1.7%) | 7.4% | |
| Abroad | 102 (1.6%) | 791 (0.7%) | 11.4% | |
| Co-payment exemption, n (%) | <0.001 1 | |||
| No | 2123 (34.3%) | 29,908 (26.2%) | 6.6% | |
| Yes, by income | 2041 (32.9%) | 35,689 (31.3%) | 5.4% | |
| Yes, due to clinical conditions | 2034 (32.8%) | 48,610 (42.6%) | 4% | |
| Total | N = 6198 | N = 114,207 | 5.1% |
| Variable | OR * | 95% CI * | p-Value * |
|---|---|---|---|
| Characteristics of the healthcare services | |||
| Healthcare services sites | |||
| 2–1 | 1.52 | 1.42–1.62 | <0.001 |
| 3–1 | 1.18 | 1.10–1.27 | <0.001 |
| Healthcare services categories | |||
| First access–Others | 1.11 | 1.04–1.18 | <0.001 |
| Healthcare services priority | |||
| Urgent–Schedulable | 0.61 | 0.29–1.30 | NS |
| Short-term–Schedulable | 0.86 | 0.78–0.96 | 0.005 |
| Deferrable–Schedulable | 1.22 | 1.15–1.30 | <0.001 |
| Co-payment value in euros | 1.00 | 1.00–1.00 | 0.014 |
| Waiting days | 1.01 | 1.01–1.01 | <0.001 |
| Patients’ characteristics | |||
| Gender | |||
| Male–Female | 1.17 | 1.11–1.24 | <0.001 |
| Age | |||
| 18–65 years–>65 years | 2.32 | 2.17–2.47 | <0.001 |
| <18 years–>65 years | 2.46 | 2.20–2.74 | <0.001 |
| Residency | |||
| Foreigner–Turin | 2.46 | 1.98–3.04 | <0.001 |
| Italian–Turin | 1.31 | 1.10–1.55 | 0.002 |
| Piedmont–Turin | 1.15 | 0.94–1.42 | NS |
| Turin Province–Turin | 0.92 | 0.86–0.99 | 0.024 |
| Co-payment exemption | |||
| No–Yes, due to clinical conditions | 1.36 | 1.27–1.46 | <0.001 |
| Yes, by income–Yes, due to clinical conditions | 1.82 | 1.69–1.95 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Russotto, A.; Ragusa, P.; Catozzi, D.; De Angelis, A.; Durbano, A.; Siliquini, R.; Orecchia, S. Understanding No-Show Patterns in Healthcare: A Retrospective Study from Northern Italy. Healthcare 2025, 13, 1869. https://doi.org/10.3390/healthcare13151869
Russotto A, Ragusa P, Catozzi D, De Angelis A, Durbano A, Siliquini R, Orecchia S. Understanding No-Show Patterns in Healthcare: A Retrospective Study from Northern Italy. Healthcare. 2025; 13(15):1869. https://doi.org/10.3390/healthcare13151869
Chicago/Turabian StyleRussotto, Antonino, Paolo Ragusa, Dario Catozzi, Aldo De Angelis, Alessandro Durbano, Roberta Siliquini, and Stefania Orecchia. 2025. "Understanding No-Show Patterns in Healthcare: A Retrospective Study from Northern Italy" Healthcare 13, no. 15: 1869. https://doi.org/10.3390/healthcare13151869
APA StyleRussotto, A., Ragusa, P., Catozzi, D., De Angelis, A., Durbano, A., Siliquini, R., & Orecchia, S. (2025). Understanding No-Show Patterns in Healthcare: A Retrospective Study from Northern Italy. Healthcare, 13(15), 1869. https://doi.org/10.3390/healthcare13151869







