Music Therapy Outcomes in Older Adults Using Cochlear Implants, Hearing Aids, or Combined Bimodal Devices: A Systematic Review
Abstract
1. Introduction
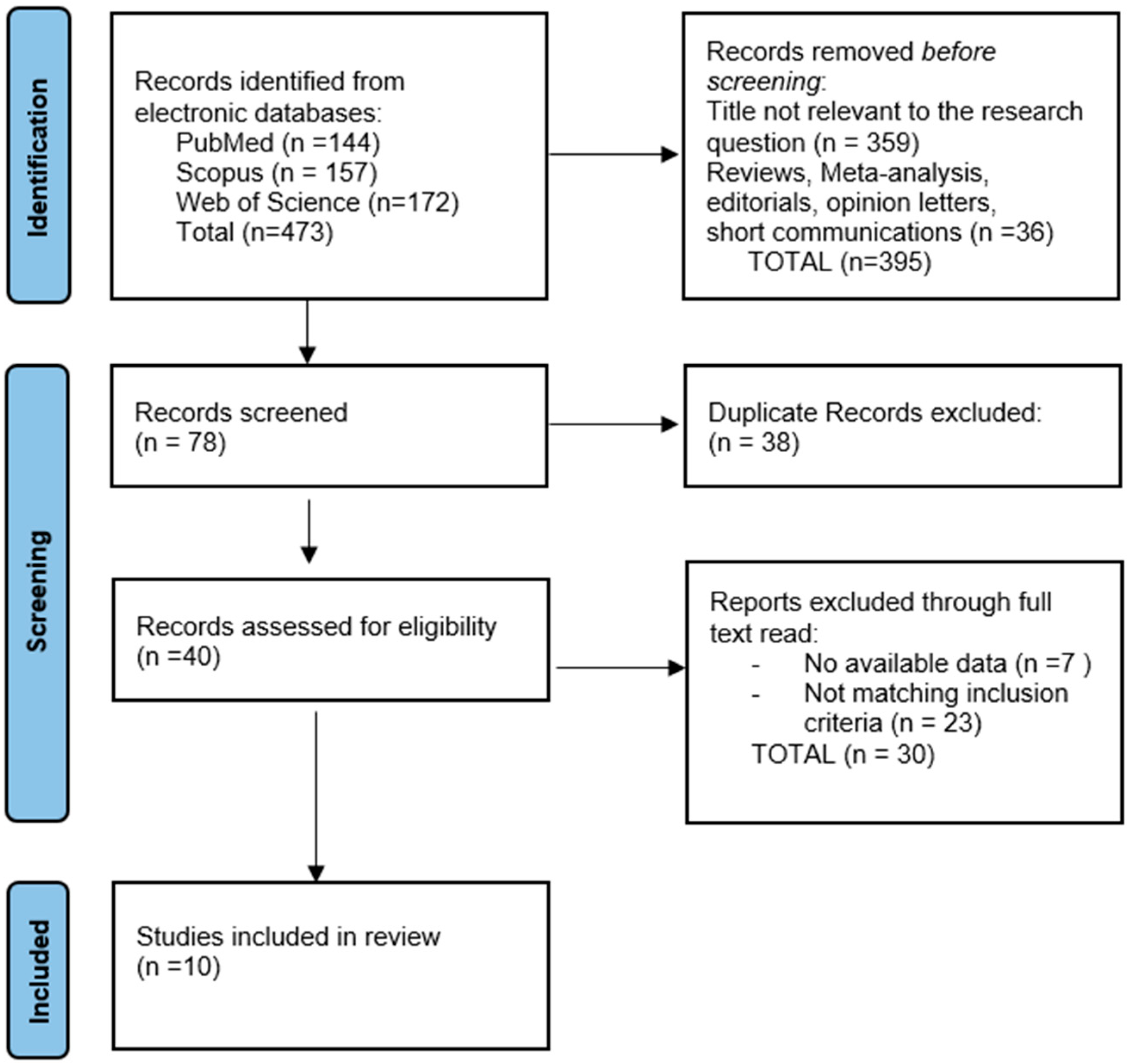
2. Materials and Methods
2.1. The Protocol and Registration
2.2. Eligibility Criteria
- Study population: Only studies including participants with a mean age over 60 years who used cochlear implants and/or hearing aids were eligible.
- Focus of the study: Included research had to specifically assess the impact of music therapy on the quality of life and self-esteem in older adults with hearing loss. This encompassed studies evaluating variables such as auditory rehabilitation, auditory benefit, musical training, auditory and musical perception, and psychological outcomes.
- Study design: Eligible designs included prospective studies, cross-sectional studies, longitudinal studies, and pilot studies.
- Outcome measures: Studies had to report validated instruments or clearly defined parameters assessing the quality of life, self-esteem, musical perception, auditory perception, or auditory benefit.
- Language: Only articles published in English were included.
- Studies not conducted on human subjects;
- Studies lacking specific results or outcome data;
- Grey literature, such as non-peer-reviewed articles, conference abstracts, editorials, and general commentaries, which were excluded to ensure methodological rigor and data credibility.
2.3. Definitions
2.4. Data Collection Process
2.5. Risk of Bias and Quality Assessment
3. Results
3.1. Study Characteristics
3.2. Study Characteristics and Design Overview
3.2.1. Intervention Type and Participation
3.2.2. Device Configuration and Performance
3.2.3. Large-Scale and Neurophysiological Assessments
Musical Perception: Tone, Rhythm, Timbre, and Stereo
- Bimodal users (CI + HAs) achieved better musical perception scores than CI-only users [22];
- Postlingual CI users were able to restore semantic musical processing, while prelingual users could not [27];
- Bilateral CI users consistently outperformed unilateral users in auditory tasks, particularly those involving stereo detection and spatial sound localization [19].
3.3. Disease Characteristics
3.4. Quality of Life (QoL)
4. Discussion
4.1. Principal Findings and Interpretation
4.2. Differential Impact Based on Implant Type and Hearing History
4.3. Quality of Life and Psychosocial Reintegration
4.4. Influence of Training Duration and MT Modality
4.5. Subjective Sound Quality Perception
4.6. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Laske, R.D.; Veraguth, D.; Dillier, N.; Binkert, A.; Holzmann, D.; Huber, A.M. Subjective and objective results after bilateral cochlear implantation in adults. Otol. Neurotol. 2009, 30, 313–318. [Google Scholar] [CrossRef] [PubMed]
- Arnautu, S.-F.; Arnautu, D.-A.; Jianu, D.-C.; Tomescu, M.-C.; Blajovan, M.-D.; Banciu, C.-D.; Malita, D.-C. Elderly Individuals Residing in Nursing Homes in Western Romania Who Have Been Diagnosed with Hearing Loss are at a Higher Risk of Experiencing Cognitive Impairment. J. Multidiscip. Health 2024, 17, 881–888. [Google Scholar] [CrossRef] [PubMed]
- Yoon, C.Y.; Kong, T.H.; Lee, J.; Seo, Y.J.; Ahn, J.J. Epidemiology of idiopathic sudden sensorineural hearing loss in the era of big data. Eur. Arch. Otorhinolaryngol. 2023, 280, 2181–2190. [Google Scholar] [CrossRef] [PubMed]
- Sidenna, M.; Fadl, T.; Zayed, H. Genetic Epidemiology of Hearing Loss in the 22 Arab Countries: A Systematic Review. Otol. Neurotol. 2020, 41, e152–e162. [Google Scholar] [CrossRef] [PubMed]
- Sheffield, A.M.; Smith, R.J.H. The Epidemiology of Deafness. Cold Spring Harb. Perspect. Med. 2019, 9, a033258. [Google Scholar] [CrossRef] [PubMed]
- Feier, C.V.I.; Paunescu, I.A.; Faur, A.M.; Cozma, G.V.; Blidari, A.R.; Muntean, C. Sexual Functioning and Impact on Quality of Life in Patients with Early-Onset Colorectal Cancer: A Systematic Review. Diseases 2024, 12, 66. [Google Scholar] [CrossRef] [PubMed]
- Lima, J.P.; Iervolino, S.M.S.; Schochat, E. Musical and temporal auditory skills in cochlear implant users after music therapy. Habilidades auditivas musicais e temporais em usuários de implante coclear após musicoterapia. CoDAS 2018, 30, e20180006. [Google Scholar] [CrossRef] [PubMed]
- Driscoll, V.D.; Oleson, J.; Jiang, D.; Gfeller, K. Effects of training on recognition of musical instruments presented through cochlear implant simulations. J. Am. Acad. Audiol. 2009, 20, 71–82. [Google Scholar] [CrossRef] [PubMed]
- Galvin, J.J., 3rd; Fu, Q.-J.; Nogaki, G. Melodic contour identification by cochlear implant listeners. Ear Hear. 2007, 28, 302–319. [Google Scholar] [CrossRef] [PubMed]
- Feier, C.V.I.; Muntean, C.; Faur, A.M.; Blidari, A.; Contes, O.E.; Streinu, D.R.; Olariu, S. The Changing Landscape of Thyroid Surgery during the COVID-19 Pandemic: A Four-Year Analysis in a University Hospital in Romania. Cancers 2023, 15, 3032. [Google Scholar] [CrossRef] [PubMed]
- Intartaglia, B.; Prud’Homme, M.-A.; Foster, N.E.V.; Zeitouni, A.G.; Lehmann, A. Visual cortex plasticity in cochlear implant users revealed in a visual motion detection task. Clin. Neurophysiol. 2022, 137, 11–24. [Google Scholar] [CrossRef] [PubMed]
- Glennon, E.; Svirsky, M.A.; Froemke, R.C. Auditory cortical plasticity in cochlear implant users. Curr. Opin. Neurobiol. 2020, 60, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Thai-Van, H.; Veuillet, E.; Norena, A.; Guiraud, J.; Collet, L. Plasticity of tonotopic maps in humans: Influence of hearing loss, hearing aids and cochlear implants. Acta Oto Laryngol. 2010, 130, 333–337. [Google Scholar] [CrossRef] [PubMed]
- Irvine, D.R.F. Plasticity in the auditory system. Hear. Res. 2018, 362, 61–73. [Google Scholar] [CrossRef] [PubMed]
- McDermott, H.J. Music perception with cochlear implants: A review. Trends Amplif. 2004, 8, 49–82. [Google Scholar] [CrossRef] [PubMed]
- Looi, V.; She, J. Music perception of cochlear implant users: A questionnaire, and its implications for a music training program. Int. J. Audiol. 2010, 49, 116–128. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Magele, A.; Wirthner, B.; Schoerg, P.; Ploder, M.; Sprinzl, G.M. Improved Music Perception after Music Therapy following Cochlear Implantation in the Elderly Population. J. Pers. Med. 2022, 12, 443. [Google Scholar] [CrossRef] [PubMed]
- Hutter, E.; Argstatter, H.; Grapp, M.; Plinkert, P. Music therapy as specific and complementary training for adults after cochlear implantation: A pilot study. Cochlea Implant. Int. 2015, 16 (Suppl. S3), S13–S21. [Google Scholar] [CrossRef] [PubMed]
- Amann, E.; Anderson, I. Development and validation of a questionnaire for hearing implant users to self-assess their auditory abilities in everyday communication situations: The Hearing Implant Sound Quality Index (HISQUI19). Acta Oto laryngol. 2014, 134, 915–923. [Google Scholar] [CrossRef] [PubMed]
- Peterson, N.; Bergeson, T.R. Contribution of hearing aids to music perception by cochlear implant users. Cochlea- Implant. Int. 2015, 16 (Suppl. S3), S71–S78. [Google Scholar] [CrossRef] [PubMed]
- Mick, P.; Parfyonov, M.; Wittich, W.; Phillips, N.; Guthrie, D.; Kathleen Pichora-Fuller, M. Associations between sensory loss and social networks, participation, support, and loneliness: Analysis of the Canadian Longitudinal Study on Aging. Can. Fam. Physician 2018, 64, e33–e41, correction appears in Can. Fam. Physician 2018, 64, 92. [Google Scholar] [PubMed]
- Neuman, A.C.; Waltzman, S.B.; Shapiro, W.H.; Neukam, J.D.; Zeman, A.M.; Svirsky, M.A. Self-Reported Usage, Functional Benefit, and Audiologic Characteristics of Cochlear Implant Patients Who Use a Contralateral Hearing Aid. Trends Hear. 2017, 21, 2331216517699530. [Google Scholar] [CrossRef] [PubMed]
- Sarant, J.; Harris, D.; Busby, P.; Maruff, P.; Schembri, A.; Lemke, U.; Launer, S. The Effect of Hearing Aid Use on Cognition in Older Adults: Can We Delay Decline or Even Improve Cognitive Function? J. Clin. Med. 2020, 9, 254. [Google Scholar] [CrossRef] [PubMed]
- Fuller, C.D.; Galvin, J.J., 3rd; Maat, B.; Başkent, D.; Free, R.H. Comparison of Two Music Training Approaches on Music and Speech Perception in Cochlear Implant Users. Trends Hear. 2018, 22, 2331216518765379. [Google Scholar] [CrossRef] [PubMed]
- Bruns, L.; Mürbe, D.; Hahne, A. Understanding music with cochlear implants. Sci. Rep. 2016, 6, 32026. [Google Scholar] [CrossRef] [PubMed]
- Buechner, A.; Krueger, B.; Klawitter, S.; Zimmermann, D.; Fredelake, S.; Holube, I.; Eshraghi, A.A. The perception of the stereo effect in bilateral and bimodal cochlear implant users and its contribution to music enjoyment. PLoS ONE 2020, 15, e0235435. [Google Scholar] [CrossRef] [PubMed]
- Satici, S.; Derinsu, U.; Akdeniz, E. Evaluation of self-esteem in hearing aid and cochlear implant users. Eur. Arch. Otorhinolaryngol. 2023, 280, 2735–2740. [Google Scholar] [CrossRef] [PubMed]
- Nieman, C.L.; Morales, E.E.G.; Huang, A.R.; Reed, N.S.; Yasar, S.; Oh, E.S. Prevalence of Hearing Loss and Hearing Aid Use Among Persons Living With Dementia in the US. JAMA Netw. Open 2024, 7, e2440400. [Google Scholar] [CrossRef] [PubMed]
- Feier, C.V.I.; Muntean, C.; Bolboacă, S.D.; Olariu, S. Exploratory Evaluation of Pre-Treatment Inflammation Profiles in Patients with Colorectal Cancer. Diseases 2024, 12, 61. [Google Scholar] [CrossRef] [PubMed]
- Lerousseau, J.P.; Hidalgo, C.; Schön, D. Musical Training for Auditory Rehabilitation in Hearing Loss. J. Clin. Med. 2020, 9, 1058. [Google Scholar] [CrossRef] [PubMed]
- Picou, E.M.; Singh, G.; Goy, H.; Russo, F.; Hickson, L.; Oxenham, A.J.; Buono, G.H.; Ricketts, T.A.; Launer, S. Hearing, Emotion, Amplification, Research, and Training Workshop: Current Understanding of Hearing Loss and Emotion Perception and Priorities for Future Research. Trends Hear. 2018, 22, 2331216518803215. [Google Scholar] [CrossRef] [PubMed]
- Illg, A.; Lenarz, T. Cochlear Implantation in Hearing-Impaired Elderly: Clinical Challenges and Opportunities to Optimize Outcome. Front. Neurosci. 2022, 16, 887719. [Google Scholar] [CrossRef] [PubMed]
- Peterson, N.R.; Pisoni, D.B.; Miyamoto, R.T. Cochlear implants and spoken language processing abilities: Review and assessment of the literature. Restor. Neurol. Neurosci. 2010, 28, 237–250. [Google Scholar] [CrossRef] [PubMed]
- Holder, J.T.; Holcomb, M.A.; Snapp, H.; Labadie, R.F.; Vroegop, J.; Rocca, C.; Elgandy, M.S.; Dunn, C.; Gifford, R.H. Guidelines for Best Practice in the Audiological Management of Adults Using Bimodal Hearing Configurations. Otol. Neurotol. Open 2022, 2, e011. [Google Scholar] [CrossRef] [PubMed]
- Feier, C.V.I.; Bardan, R.; Muntean, C.; Feier, O.; Olariu, A.; Olariu, S. The consequences of the Covid-19 pandemic on elective surgery for colon cancer. Ann. Ital. Di Chir. 2022, 93, 599–605. [Google Scholar]
- Jaiswal, A.; Aldersey, H.; Wittich, W.; Mirza, M.; Finlayson, M.; Soundy, A. Participation experiences of people with deafblindness or dual sensory loss: A scoping review of global deafblind literature. PLoS ONE 2018, 13, e0203772. [Google Scholar] [CrossRef] [PubMed]
- Brennan, M.; Bally, S.J. Psychosocial adaptations to dual sensory loss in middle and late adulthood. Trends Amplif. 2007, 11, 281–300. [Google Scholar] [CrossRef] [PubMed]
- Feier, C.V.I.; Santoro, R.R.; Faur, A.M.; Muntean, C.; Olariu, S. Assessing Changes in Colon Cancer Care during the COVID-19 Pandemic: A Four-Year Analysis at a Romanian University Hospital. J. Clin. Med. 2023, 12, 6558. [Google Scholar] [CrossRef] [PubMed]
- Fuller, C.; Mallinckrodt, L.; Maat, B.; Başkent, D.; Free, R. Music and quality of life in early-deafened late-implanted adult cochlear implant users. Otol. Neurotol. 2013, 34, 1041–1047. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Park, K.H.; Han, W. The Effects of Music-Based Auditory Training on Hearing-Impaired Older Adults With Mild Cognitive Impairment. Clin. Exp. Otorhinolaryngol. 2024, 17, 26–36. [Google Scholar] [CrossRef] [PubMed]
- Magele, A.; Wirthner, B.; Schoerg, P.; Sprinzl, G.M. Effects of Musical Training in Music Therapy Following Cochlear Implantation—A Case Report. Audiol. Res. 2024, 14, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Veltman, J.; Maas, M.J.; Beijk, C.; Groenhuis, A.Y.; Versnel, H.; Vissers, C.; Huinck, W.J.; Hoetink, A.E. Development of the Musi-CI Training, A Musical Listening Training for Cochlear Implant Users: A Participatory Action Research Approach. Trends Hear. 2023, 27, 23312165231198368. [Google Scholar] [CrossRef] [PubMed]
- Grenier, A.S.; Lafontaine, L.; Sharp, A. Use of Music Therapy as an Audiological Rehabilitation Tool in the Elderly Population: A Mini-Review. Front. Neurosci. 2021, 15, 662087. [Google Scholar] [CrossRef] [PubMed]
- A Berg, K.; Noble, J.H.; Dawant, B.M.; Gifford, R.H. Evaluating Selective Apical Electrode Deactivation for Improving Cochlear Implant Outcomes. Trends Hear. 2025, 29, 23312165251353638. [Google Scholar] [CrossRef] [PubMed]
- Gfeller, K.; Driscoll, V.; Schwalje, A. Beyond Technology: The Interaction of Perceptual Accuracy and Experiential Factors in Pediatric Music Engagement. Otol. Neurotol. 2019, 40, e290–e297. [Google Scholar] [CrossRef] [PubMed]
- Lam, C.; Moore, B.C.J.; Salorio-Corbetto, M.; Vickers, D.A. The Relationship Between Hearing Experiences, Music-Listening Behaviors, and Chord-Discrimination Abilities for Cochlear Implant Users. Trends Hear. 2022, 26, 23312165221143902. [Google Scholar] [CrossRef]
- Creech, A. Using Music Technology Creatively to Enrich Later-Life: A Literature Review. Front. Psychol. 2019, 10, 117. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, M.L.; Deroche, M.L.D.; Jiradejvong, P.; Barrett, K.C.; Limb, C.J. Cochlear Implant Compression Optimization for Musical Sound Quality in MED-EL Users. Ear Hear. 2022, 43, 862–873. [Google Scholar] [CrossRef] [PubMed]
| Study | Sample Size | Country of Origin | Gender Distribution Women: Men | Comparison Group | Brand of CI/HA |
|---|---|---|---|---|---|
| 1. Magele et al. [19] | 11 | Austria | 5:6 | with MT without MT | CI: Med-EL (OPUS22/Sonnet) Cochlear (CI522/Kanso); HA:NR |
| 2. Hutter et al. [20] | 12 | Germany | NR | MSCS and MS | NR |
| 3. Amann et al. [21] | 70 | Austria | IC > 60 years IC < 60 years | NR | |
| 4. Peterson et al. [22] | 14 | USA | NR | IC with CI + HAs | NR |
| 5. Mick et al. [23] | 21,241 | Canada | NR | SD | NR |
| 6. Neuman et al. [24] | 94 | USA | NR | IC + HA | CI: Med-EL (OPUS22/Sonnet) Cochlear (N5/N6); HA: Phonak, Oticon, Unitron, Siemens, Telex, Widex, Audibel |
| 7. Sarant et al. [25] | 98 | Australia | 53:45 | SD/GML/DET/ONB/IDN/OCL | |
| 8. Fuller et al. [26] | 19 | Netherlands | NR | CTMTA | CI: CI24RE, HiRes90 K Helix, CI512, CI24R CS, CI24RECA |
| 9. Bruns et al. [27] | 53 | Germany | 21:32 | 15PreCIU38PostCIU | Med-EL, Cochlear, Advanced Bionics |
| 10. Buechner et al. [28] | 20 | Germany | NR | Bilateral CI | NR |
| Study Number | Duration of Deafness (y) | Onset/Severity of Hearing Loss | Surgical History | Treatment |
|---|---|---|---|---|
| 1. Magele et al. [19] | 18, 25 ± 19, 50 years | PH/NR | PMB | CI |
| 2. Hutter et al. [20] | NR | PH/NR | PMU | CI |
| 3. Amann et al. [21] | <20 years; >20 years | PH/NR | PMU | CI |
| 4. Peterson et al. [22] | NR | PH/NR | PMU | CI + HA |
| 5. Mick et al. [23] | 45–89 years | NR | NR | NR |
| 6. Neuman et al. [24] | 64, 5–64,8 years | NR/Severe/profound hearing loss | PMU | CI + HA |
| 7. Sarant et al. [25] | 23 years | NR/Moderate hearing loss | PMB | HA |
| 8. Fuller et al. [26] | 35 years | PH/NR | PMB | CI |
| 9. Bruns et al. [27] | 31 years | PH/PRH/NR | PMB | CI |
| 10. Buechner et al. [28] | NR | NR | PMB | CI |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Padurean, L.L.; Ștefanescu, H.E.; Muntean, C.; Gaborean, V.; Horhat, I.D. Music Therapy Outcomes in Older Adults Using Cochlear Implants, Hearing Aids, or Combined Bimodal Devices: A Systematic Review. Healthcare 2025, 13, 1795. https://doi.org/10.3390/healthcare13151795
Padurean LL, Ștefanescu HE, Muntean C, Gaborean V, Horhat ID. Music Therapy Outcomes in Older Adults Using Cochlear Implants, Hearing Aids, or Combined Bimodal Devices: A Systematic Review. Healthcare. 2025; 13(15):1795. https://doi.org/10.3390/healthcare13151795
Chicago/Turabian StylePadurean, Liviu Lucian, Horatiu Eugen Ștefanescu, Calin Muntean, Vasile Gaborean, and Ioana Delia Horhat. 2025. "Music Therapy Outcomes in Older Adults Using Cochlear Implants, Hearing Aids, or Combined Bimodal Devices: A Systematic Review" Healthcare 13, no. 15: 1795. https://doi.org/10.3390/healthcare13151795
APA StylePadurean, L. L., Ștefanescu, H. E., Muntean, C., Gaborean, V., & Horhat, I. D. (2025). Music Therapy Outcomes in Older Adults Using Cochlear Implants, Hearing Aids, or Combined Bimodal Devices: A Systematic Review. Healthcare, 13(15), 1795. https://doi.org/10.3390/healthcare13151795







