The Effect of Integrative Treatment on Improving Functional Level in Stroke Patients: A Retrospective Chart Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
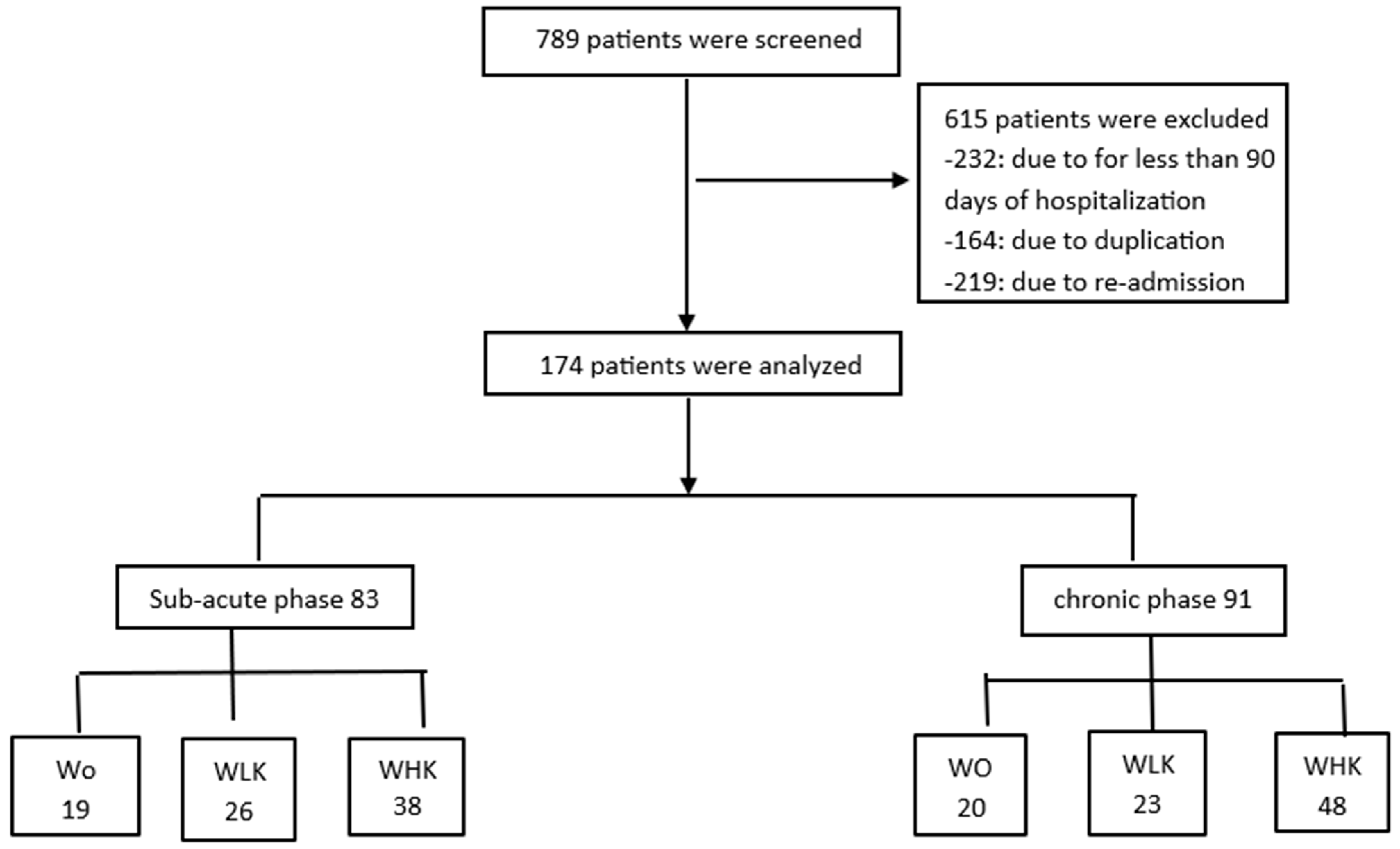
2.2. Patients
2.3. Functional Assessment Index
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
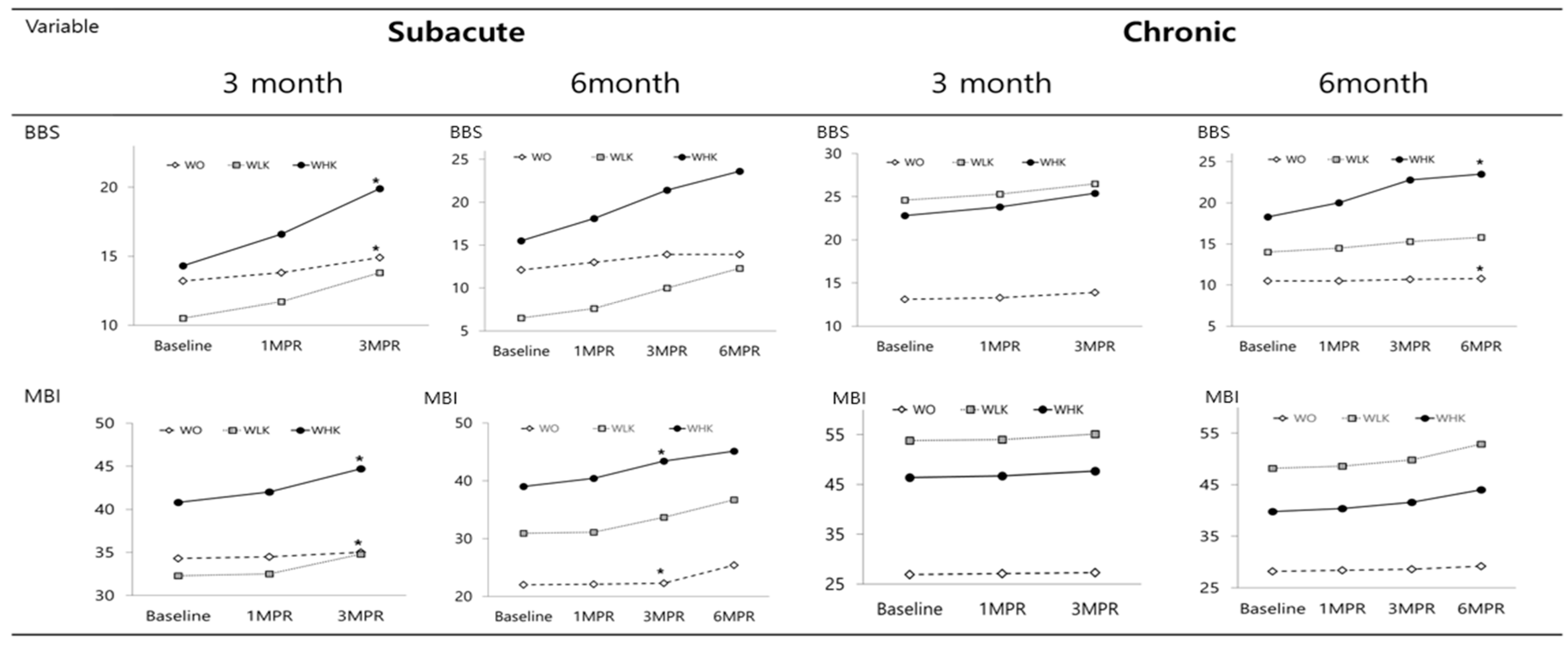
3.2. Effects on Functional Recovery
3.2.1. 3 Months Post-Treatment
3.2.2. 6 Months Post-Treatment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| WO | Western rehabilitation treatment only |
| WLK | Western rehabilitation treatment plus low-frequency Korean medicine |
| WHK | Western rehabilitation treatment plus high-frequency Korean medicine |
| BBS | Berg Balance Scale |
| FIM | functional independence measure |
| MBC | modified Brunnstrom classification |
| ANOVA | one-way analysis of variance |
| MBI | modified Barthel index |
| MPT | months post-treatment |
| K-MMSE | Korean mini-mental state examination |
| CDR | clinical dementia rating |
| MMT | manual muscle test |
| MFT | manual function test |
| MAS | modified Ashworth scale |
References
- Strong, K.; Mathers, C.; Bonita, R. Preventing stroke: Saving lives around the world. Lancet Neurol. 2007, 6, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Clinical Research Center for Stroke. Clinical Research Center for Stroke. Clinical Practice Guideline for Stroke. In Preamble; Clinical Research Center Designated by Ministry of Health & Welfare: Seoul, Republic of Korea, 2013; p. 4. [Google Scholar]
- De Wit, L.; Putman, K.; Schuback, B.; Komárek, A.; Angst, F.; Baert, I.; Berman, P.; Bogaerts, K.; Brinkmann, N.; Connell, L.; et al. Motor and functional recovery after stroke: A comparison of 4 European rehabilitation centers. Stroke 2007, 38, 2101–2107. [Google Scholar] [CrossRef]
- Han, D.W.; An, T.S.; Choi, S.J.; Kim, J.W. Attitude towards traditional Korean medicine use among hemiplegic patients after cerebrovascular accident. J. Soc. Prev. Korean Med. 2011, 15, 67–81. [Google Scholar]
- Chavez, L.M.; Huang, S.S.; MacDonald, I.; Lin, J.G.; Lee, Y.C.; Chen, Y.H. Mechanisms of Acupuncture Therapy in Ischemic Stroke Rehabilitation: A Literature Review of Basic Studies. Int. J. Mol. Sci. 2017, 18, 2270. [Google Scholar] [CrossRef]
- Park, S.U.; Cho, S.Y.; Park, J.M.; Ko, C.N.; Park, H.J.; Walls, L.; Cotter, A.C.; Park, J.J. Integrative treatment modalities for stroke victims in Korea. Complement. Ther. Clin. Pract. 2014, 20, 37–41. [Google Scholar] [CrossRef]
- Kim, K.H. Research on Doctors Who Cooperate with Korean Medicine Hospitals; Research Institute for Healthcare Policy Research Report: Seoul, Republic of Korea, 2004; pp. 1–88. [Google Scholar]
- Na, S. Philosophical issues concerning the East-West corroborative medical care. Third Med. 2004, 7, 59–64. [Google Scholar]
- Kim, M.S.; Yun, J.M. Comparison of the functional recovery of stroke patients treated with eastern-western integrative medical care and western single rehabilitation therapy. J. Int. Korean Med. 2016, 37, 645–652. [Google Scholar] [CrossRef]
- Mehrholz, J.; Wagner, K.; Rutte, K.; Meiβner, D.; Pohl, M. Predictive validity and responsiveness of the functional ambulation category in hemiparetic patients after stroke. Arch. Phys. Med. Rehabil. 2007, 88, 1314–1319. [Google Scholar] [CrossRef]
- Moon, S.R.; Keum, D.H. Effect of East-West Integrative Rehabilitation on Activity of Daily Living and Cognitive Functional Recovery in Stroke Patients: A Retrospective Study. J. Korean Med. Rehabil. 2020, 30, 105–123. [Google Scholar] [CrossRef]
- Berg, K.O.; Wood-Dauphinee, S.L.; Williams, J.I.; Maki, B. Measuring balance in the elderly: Validation of an instrument. Can. J. Public Health 1992, 83, S7–S11. [Google Scholar]
- Jung, H.Y.; Park, B.G.; Shin, H.S.; Kang, Y.K.; Pyun, S.B.; Paik, N.J.; Kim, S.H.; Kim, T.H.; Han, T.R. Development of the Korean version of Modified Barthel Index (K-MBI): Multi-center study for subjects with strike. Ann. Rehabil. Med. 2007, 31, 283–297. [Google Scholar]
- Hislop, H.J.; Montgomery, J. Daniels and Worthingham’s Muscle Testing, 8th ed.; Saunders/Elsevier: St. Louis, MO, USA, 2007. [Google Scholar]
- Michimata, A.; Kondo, T.; Suzukamo, Y.; Chiba, M.; Izumi, S.I. The manual function test: Norms for 20- to 90-year-olds and effects of age, gender, and hand dominance on dexterity. Tohoku J. Exp. Med. 2008, 214, 257–267. [Google Scholar] [CrossRef] [PubMed]
- Bohannon, R.W.; Smith, M.B. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys. Ther. 1987, 67, 206–207. [Google Scholar] [CrossRef]
- Charles, H.C.; Sandra, L.R.; Kristine, L.H. Functional evaluation and management of self-care and other activities of daily living. In Physical Medicine and Rehabilitation: Principle and Practice, 5th ed.; Delisa, J.A., Ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2010; pp. 243–288. [Google Scholar]
- Brunnstrom, S. Motor testing procedures in hemiplegia: Based on sequential recovery stages. Phys. Ther. 1966, 46, 357–375. [Google Scholar] [CrossRef]
- Kim, Y.D.; Park, K.C.; Kang, Y.G.; Lee, H.O.; Lee, S.K.; Lee, Y.J.; Bae, C.Y. The relationship between the Alzheimer’s disease Assessment Scale and other measures of dementia. Korean J. Fam. Med. 2000, 21, 876–883. [Google Scholar]
- Choi, S.H.; Na, D.L.; Lee, B.H.; Hahm, D.S.; Jeong, J.H.; Yoon, S.J.; Yoo, K.H.; Ha, C.K.; Han, I.W. Estimating the validity of the Korean version of expanded clinical dementia rating (CDR) scale. J. Korean Neurol. Assoc. 2001, 19, 585–591. [Google Scholar]
- Clarke, D.J.; Forster, A. Improving post-stroke recovery: The role of the multidisciplinary health care team. J. Multidiscip. Healthc. 2015, 8, 433–442. [Google Scholar] [CrossRef]
- Wang, H.-Q.; Hou, M.; Li, H.; Bao, C.-L.; Min, L.; Dong, G.-R.; Jiao, Z.-H. Effects of acupuncture treatment on motor function in patients with subacute hemorrhagic stroke: A randomized controlled study. Complement. Ther. Med. 2020, 49, 102296. [Google Scholar] [CrossRef]
- Hiengkaew, V.; Jitaree, K.; Chaiyawat, P. Minimal detectable changes of the Berg Balance Scale, Fugl-Meyer Assessment Scale, Timed “Up & Go” Test, gait speeds, and 2-minute walk test in individuals with chronic stroke with different degrees of ankle plantarflexor tone. Arch. Phys. Med. Rehabil. 2012, 93, 1201–1208. [Google Scholar] [CrossRef]
- Chen, L.; Fang, J.; Ma, R.; Gu, X.; Chen, L.; Li, J.; Xu, S. Additional effects of acupuncture on early comprehensive rehabilitation in patients with mild to moderate acute ischemic stroke: A multicenter randomized controlled trial. BMC Complement. Altern. Med. 2016, 16, 226. [Google Scholar] [CrossRef]
- Hsieh, Y.W.; Wang, C.H.; Wu, S.C.; Chen, P.C.; Sheu, C.F.; Hsieh, C.L. Establishing the minimal clinically important difference of the Barthel Index in stroke patients. Neurorehabil. Neural Repair 2007, 21, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Sze, F.K.; Wong, E.; Yi, X.; Woo, J. Does acupuncture have additional value to standard poststroke motor rehabilitation? Stroke 2002, 33, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Wayne, P.M.; Krebs, D.E.; Macklin, E.A.; Schnyer, R.; Kaptchuk, T.J.; Parker, S.W.; Scarborough, D.M.; McGibbon, C.A.; Schaechter, J.D.; Stein, J.; et al. Acupuncture for upper-extremity rehabilitation in chronic stroke: A randomized sham-controlled study. Arch. Phys. Med. Rehabil. 2005, 86, 2248–2255. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.; Zhou, Y.-M.; Liao, C.-X.; Tang, Y.-Z.; Li, Y.-X.; Qiu, L.-H.; Qin, W.; Zeng, F.; Liang, F.-R.; Zhang, M. Structural changes induced by acupuncture in the recovering brain after ischemic stroke. Evid. Based Complement. Alternat. Med. 2018, 2018, 5179689. [Google Scholar] [CrossRef]
- Han, X.; Jin, H.; Li, K.; Ning, Y.; Jiang, L.; Chen, P.; Liu, H.; Zhang, Y.; Zhang, H.; Tan, Z.; et al. Acupuncture modulates disrupted whole-brain network after ischemic stroke: Evidence based on graph theory analysis. Neural Plast. 2020, 2020, 8838498. [Google Scholar] [CrossRef] [PubMed]
- Nierhaus, T.; Chang, Y.; Liu, B.; Shi, X.; Yi, M.; Witt, C.M.; Pach, D. Somatosensory stimulation with XNKQ acupuncture modulates functional connectivity of motor areas. Front. Neurosci. 2019, 13, 147. [Google Scholar] [CrossRef]
- Zhu, W.; Ye, Y.; Liu, Y.; Wang, X.R.; Shi, G.X.; Zhang, S.; Liu, C.Z. Mechanisms of Acupuncture Therapy for Cerebral Ischemia: An Evidence-Based Review of Clinical and Animal Studies on Cerebral Ischemia. J. Neuroimmune Pharmacol. 2017, 12, 575–592. [Google Scholar] [CrossRef]
- Kim, J.S. Sex Difference in the Functional Recovery After Acute Stroke. Master’s Thesis, Department of Neurology, College of Medicine, Soonchunhyang University, Asan, Republic of Korea, 2010. [Google Scholar]
- Rexrode, K.M.; Madsen, T.E.; Yu, A.Y.X.; Carcel, C.; Lichtman, J.H.; Miller, E.C. The Impact of Sex and Gender on Stroke. Circ. Res. 2022, 130, 512–528. [Google Scholar] [CrossRef]
| Characteristic | Duration of Onset | Group, n or Mean ± SD | p-Value | |||
|---|---|---|---|---|---|---|
| Total | WO | WLK | WHK | |||
| Number | Subacute | 83 | 19 | 26 | 38 | |
| Chronic | 91 | 20 | 23 | 48 | ||
| Age (years) | Subacute | 71.1 ± 13.5 | 73.4 ± 11.4 | 73.6 ± 12.1 | 68.2 ± 15.0 | 0.203 |
| Chronic | 62.7 ± 12.9 | 66.5 ± 13.5 | 62.7 ± 10.4 | 61.0 ± 13.7 | 0.282 | |
| Time elapsed after stroke (days) | Subacute | 66.2 ± 47.0 | 68.5 ± 38.7 | 71.0 ± 45.9 | 61.8 ± 52.0 | 0.728 |
| Chronic | 605.7 ± 391.6 | 619.6 ± 505.6 | 690.3 ± 373.5 | 559.3 ± 345.3 | 0.417 | |
| Sex (male–female) | Subacute | 30:53 | 6:13 | 9:17 | 15:23 | 0.827 |
| Chronic | 41:50 | 10:10 | 8:15 | 23:25 | 0.513 | |
| Hypertension (n) | Subacute | 37 | 8 | 14 | 15 | 0.509 |
| Chronic | 36 | 8 | 10 | 18 | 0.889 | |
| Diabetes (n) | Subacute | 20 | 3 | 11 | 6 | 0.032 (a) |
| Chronic | 22 | 7 | 7 | 8 | 0.197 | |
| Cardiovascular disease (n) | Subacute | 16 | 6 | 6 | 4 | 0.138 |
| Chronic | 8 | 4 | 3 | 0.130 | ||
| Hyperlipidemia (n) | Subacute | 5 | 1 | 1 | 3 | 0.790 |
| Chronic | 7 | 1 | 3 | 3 | 0.529 | |
| Stroke classification | ||||||
| Spontaneous intracerebral hemorrhage (n) | Subacute | 16 | 3 | 3 | 10 | |
| Chronic | 43 | 6 | 12 | 25 | ||
| Traumatic intracerebral hemorrhage (n) | Subacute | 9 | 5 | 3 | 1 | |
| Chronic | 6 | 2 | 1 | 3 | ||
| Cerebral infarction (n) | Subacute | 55 | 10 | 19 | 26 | |
| Chronic | 36 | 9 | 10 | 17 | ||
| Stroke site | ||||||
| ICH (n) | Subacute | 16 | 5 | 2 | 9 | |
| Chronic | 37 | 6 | 11 | 20 | ||
| SAH (n) | Subacute | 6 | 2 | 3 | 1 | |
| Chronic | 7 | 1 | 1 | 5 | ||
| SDH (n) | Subacute | 3 | 1 | 1 | 1 | |
| Chronic | 3 | 1 | 1 | 1 | ||
| ACA (n) | Subacute | 2 | 1 | 0 | 1 | |
| Chronic | 0 | 0 | 0 | 0 | ||
| MCA (n) | Subacute | 40 | 4 | 16 | 20 | |
| Chronic | 28 | 7 | 3 | 13 | ||
| PCA (n) | Subacute | 0 | 0 | 0 | 0 | |
| Chronic | 1 | 0 | 1 | 0 | ||
| Brain stem (n) | Subacute | 6 | 2 | 2 | 2 | |
| Chronic | 2 | 0 | 1 | 1 | ||
| Cerebellum (n) | Subacute | 2 | 1 | 1 | 0 | |
| Chronic | 2 | 01 | 0 | 1 | ||
| Small vessel (n) | Subacute | 2 | 2 | 0 | 0 | |
| Chronic | 2 | 1 | 0 | 1 | ||
| More than 2 vessels (n) | Subacute | 2 | 0 | 0 | 2 | |
| Chronic | 1 | 0 | 0 | 1 | ||
| Size of brain lesionMajor axis (cm) | Subacute | 3.9 ± 2.5 | 4.5 ± 2.6 | 4.1 ± 2.9 | 3.5 ± 2.1 | 0.486 |
| Chronic | 5.8 ± 3.5 | 8.2 ± 3.2 | 3.4 ± 2.0 | 5.9 ± 3.6 | 0.002 (b) | |
| Size of brain lesionMinor axis (cm) | Subacute | 2.2 ± 13.5 | 2.4 ± 1.2 | 2.2 ± 1.8 | 2.1 ± 1.2 | 0.789 |
| Chronic | 3.2 ± 1.8 | 3.7 ± 1.7 | 2.2 ± 1.1 | 3.6 ± 2.1 | 0.071 | |
| Urination method | ||||||
| Self-urination (n) | Subacute | 61 | 14 | 17 | 30 | |
| Chronic | 74 | 11 | 20 | 43 | ||
| Diaper (n) | Subacute | 19 | 5 | 8 | 6 | |
| Chronic | 16 | 8 | 3 | 5 | ||
| Catheter (n) | Subacute | 3 | 0 | 1 | 2 | |
| Chronic | 1 | 1 | 0 | 0 | ||
| Variable | Group | Time | ||||
|---|---|---|---|---|---|---|
| Baseline | 1 MPT | Δ1 Month | 3 MPT | Δ3 Months | ||
| BBS | WO | 13.2 ± 16.2 (a) | 13.8 ± 16.2 (a) | 0.6 ± 1.1 | 14.9 ± 16.2 (a) | 1.7 ± 2.0 (c) |
| WLK | 10.5 ± 13.4 (a) | 11.7 ± 13.5 (a) | 1.3 ± 2.0 | 13.8 ± 13.9 (a) | 3.3 ± 4.8 | |
| WHK | 14.3 ± 11.8 (a) | 16.6 ± 12.6 (a) | 2.3 ± 3.7 | 19.9 ± 12.6 (a) | 5.6 ± 5.2 (c) | |
| MBI | WO | 34.3 ± 26.3 | 34.5 ± 26.2 | 0.2 ± 0.7 | 35.0 ± 26.1 | 0.7 ± 2.1 (c) |
| WLK | 32.3 ± 22.8 (a) | 32.5 ± 22.6 (a) | 0.2 ± 0.6 | 34.8 ± 22.9 (a) | 2.5 ± 2.9 | |
| WHK | 40.8 ± 19.8 (a) | 42.0 ± 20.1 (a) | 1.2 ± 3.3 | 44.7 ± 20.2 (a) | 3.9 ± 5.5 (c) | |
| MMT | WO | 22.9 ± 9.9 | 23.5 ± 9.5 | 0.7 ± 1.6 | 24.0 ± 8.8 | 1.1 ± 2.3 |
| WLK | 24.4 ± 9.5 | 25.0 ± 9.4 | 0.5 ± 2.2 | 25.3 ± 9.4 | 0.8 ± 2.8 | |
| WHK | 24.9 ± 10.2 (a) | 25.1 ± 9.9 (a) | 0.2 ± 0.9 | 25.9 ± 9.6 (a) | 0.9 ± 1.6 | |
| MFT | WO | 15.4 ± 10.6 | 15.1 ± 10.7 | 0.1 ± 0.3 | 15.5 ± 10.4 | 1.2 ± 2.5 |
| WLK | 12.1 ± 9.7 (a) | 12.2 ± 9.8 (a) | 0.7 ± 3.9 | 13.3 ± 9.4 (a) | 1.7 ± 4.4 | |
| WHK | 11.6 ± 10.6 (a) | 12.4 ± 10.3 (a) | 0.2 ± 0.7 | 13.3 ± 10.4 (a) | 0.6 ± 1.7 | |
| MAS | WO | 0.47 ± 0.64 | 0.47 ± 0.64 | 0.00 ± 0.00 | 0.53 ± 0.74 | 0.07 ± 0.26 |
| WLK | 0.46 ± 0.59 | 0.50 ± 0.59 | 0.04 ± 0.20 | 0.58 ± 0.65 | 0.13 ± 0.45 | |
| WHK | 0.40 ± 0.55 | 0.40 ± 0.55 | 0.00 ± 0.00 | 0.43 ± 0.56 | 0.03 ± 0.17 | |
| FIM | WO | 24.2 ± 11.0 | 24.4 ± 11.1 | 0.1 ± 0.3 | 25.4 ± 11.8 | 1.2 ± 2.5 |
| WLK | 26.0 ± 10.4 | 26.8 ± 10.5 | 0.7 ± 3.9 | 27.7 ± 10.2 | 1.7 ± 4.4 | |
| WHK | 30.6 ± 10.5 (a) | 30.8 ± 10.3 (a) | 0.2 ± 0.7 | 31.2 ± 10.5 (a) | 0.6 ± 1.7 | |
| MBC | WO | 5.3 ± 5.3 | 5.3 ± 1.4 | 0.0 ± 0.0 | 5.3 ± 1.4 | 0.0 ± 0.0 |
| WLK | 5.0 ± 1.8 | 5.0 ± 1.8 | 0.0 ± 0.0 | 5.0 ± 1.8 | 0.0 ± 0.0 | |
| WHK | 3.5 ± 2.2 | 3.5 ± 2.2 | −0.1 ± 0.3 | 3.5 ± 2.2 | −0.1 ± 0.3 | |
| MF | WO | 3.2 ± 0.4 | 3.2 ± 0.4 | 0.0 ± 0.0 | 3.2 ± 0.4 | 0.0 ± 0.0 |
| WLK | 3.6 ± 1.0 | 3.7 ± 1.0 | 0.1 ± 0.4 | 3.7 ± 1.0 | 0.1 ± 0.4 | |
| WHK | 3.5 ± 0.9 | 3.5 ± 0.9 | 0.0 ± 0.1 | 3.5 ± 0.9 | 0.0± 0.1 | |
| DNM | WO | 7.8 ± 6.0 | 7.8 ± 6.0 | 0.0 ± 0.2 | 7.9 ± 6.0 | 0.1 ± 0.2 |
| WLK | 7.3 ± 7.2 | 7.6 ± 7.0 | 0.3 ± 2.6 | 8.0 ± 7.4 | 0.7 ± 3.6 | |
| WHK | 7.4 ± 9.4 | 7.7 ± 9.5 | 0.3 ± 1.2 | 7.8 ± 9.5 | 0.3 ± 1.2 | |
| Variable | Group | Time | ||||
|---|---|---|---|---|---|---|
| Baseline | 1 MPT | Δ1 Month | 3 MPT | Δ3 Months | ||
| BBS | WO | 13.1 ± 16.6 | 13.3 ± 16.7 | 0.2 ± 0.6 | 13.9 ± 17.0 | 0.8 ± 1.5 |
| WLK | 24.6 ± 15.1 (a) | 25.3 ± 15.2 (a) | 0.8 ± 0.8 | 26.5 ± 15.2 (a) | 1.8 ± 2.6 | |
| WHK | 22.8 ± 14.4 (a) | 23.8 ± 14.0 (a) | 1.0 ± 2.4 | 25.4 ± 14.3 (a) | 2.6 ± 5.6 | |
| MBI | WO | 26.9 ± 21.0 (b)(c) | 27.1 ± 21.1 | 0.2 ± 0.7 | 27.3 ± 21.2 | 0.5 ± 1.1 |
| WLK | 53.8 ± 19.3 (a)(b) | 54.0 ± 18.9 (a) | 0.3 ± 0.8 | 55.1 ± 18.7 (a) | 1.3 ± 2.0 | |
| WHK | 46.4 ± 23.6 (a)(c) | 46.7 ± 23.3 (a) | 0.4 ± 1.8 | 47.7 ± 23.0 (a) | 1.3 ± 2.5 | |
| MMT | WO | 23.5 ± 11.5 | 23.7 ± 11.5 | 0.2 ± 0.6 | 23.9 ± 11.2 | 0.4 ± 1.1 |
| WLK | 30.6 ± 5.5 (d) | 30.7 ± 5.6 | 0.2 ± 0.7 | 30.8 ± 5.6 | 0.2 ± 0.7 | |
| WHK | 25.2 ± 8.3 (a)(d) | 25.3 ± 8.2 (a) | 0.1 ± 0.4 | 25.5 ± 8.1 (a) | 0.3 ± 0.8 | |
| MFT | WO | 11.3 ± 10.9 (a) | 11.5 ± 10.7 (a) | 0.2 ± 0.9 | 11.9 ± 10.8 (a) | 0.6 ± 1.0 |
| WLK | 16.4 ± 8.1 (a)(d) | 16.5 ± 8.2 (a) | 0.1 ± 0.5 | 16.9 ± 8.3 (a) | 0.5 ± 0.7 | |
| WHK | 9.4 ± 8.4 (a)(d) | 9.7 ± 8.3 (a) | 0.3 ± 1.4 | 10.0 ± 8.3 (a) | 0.6 ± 1.6 | |
| MAS | WO | 1.21 ± 1.03 | 1.21 ± 1.03 | 0.00 ± 0.00 | 1.16 ± 1.02 | −0.05 ± 0.23 |
| WLK | 0.56 ± 0.51 | 0.56 ± 0.51 | 0.00 ± 0.00 | 0.56 ± 0.51 | 0.00 ± 0.00 | |
| WHK | 0.96 ± 0.81 | 0.93 ± 0.79 | −0.02 ± 0.15 | 0.93 ± 0.79 | 0.00 ± 0.00 | |
| FIM | WO | 24.4 ± 13.5 (b)(c) | 24.4 ± 13.5 | −0.1 ± 0.2 | 24.6 ± 13.0 | 0.2 ± 2.8 |
| WLK | 39.4 ± 9.9 (b) | 39.4 ± 9.9 | 0.1 ± 0.2 | 39.6 ± 9.6 | 0.3 ± 0.7 | |
| WHK | 33.3 ± 11.8 (c) | 33.3 ± 11.8 | 0.1 ± 0.5 | 33.8 ± 11.8 | 0.5 ± 1.7 | |
| MBC | WO | 4.3 ± 2.1 | 4.3 ± 2.1 | 0.0 ± 0.0 | 4.3 ± 2.1 | 0.0 ± 0.0 |
| WLK | 4.6 ± 1.1 | 4.6 ± 1.1 | 0.0 ± 0.0 | 4.6 ± 1.1 | 0.0 ± 0.0 | |
| WHK | 3.3 ± 2.0 | 3.3 ± 2.0 | 0.0 ± 0.0 | 3.3 ± 2.0 | 0.0 ± 0.0 | |
| MF | WO | 3.2 ± 1.5 | 3.2 ± 1.5 | 0.0 ± 0.0 | 3.2 ± 1.5 | 0.0 ± 0.0 |
| WLK | 3.7 ± 1.0 | 3.7 ± 1.0 | 0.0 ± 0.0 | 3.7 ± 1.0 | 0.0 ± 0.0 | |
| WHK | 3.4 ± 0.8 | 3.4 ± 0.8 | 0.0 ± 0.0 | 3.5 ± 0.8 | 0.1 ± 0.3 | |
| DNM | WO | 6.3 ± 10.5 | 6.2 ± 10.3 | −0.1 ± 0.6 | 6.5 ± 10.7 | 0.2 ± 0.4 |
| WLK | 8.3 ± 7.3 (a) | 8.3 ± 7.3 (a) | 0.0 ± 0.2 | 8.6 ± 7.6 (a) | 0.3 ± 0.6 | |
| WHK | 8.0 ± 10.7 | 8.1 ± 10.7 | 0.0 ± 0.3 | 8.0 ± 10.7 | −0.0 ± 0.5 | |
| Variable | Group | Time | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 1 MPT | Δ1 Month | 3 MPT | Δ3 Months | 6 MPT | Δ6 Months | ||
| BBS | WO | 12.1 ± 18.2 | 13.0 ± 18.5 | 0.9 ± 1.5 | 13.9 ± 18.3 | 1.8 ± 2.3 | 13.9 ± 18.3 | 1.8 ± 2.3 |
| WLK | 6.5 ± 11.0 (a) | 7.6 ± 11.3 (a) | 1.2 ± 1.9 | 10.0 ± 12.5 (a) | 3.5 ± 5.5 | 12.3 ± 13.9 (a) | 5.8 ± 8.4 | |
| WHK | 15.5 ± 11.7 (a) | 18.1 ± 12.8 (a) | 2.6 ± 4.3 | 21.4 ± 12.1 (a) | 5.9 ± 5.3 | 23.6 ± 12.1 (a) | 8.1 ± 6.1 | |
| MBI | WO | 22.0 ± 23.6 (a) | 22.1 ± 23.5 (a) | 0.1 ± 0.3 | 22.3 ± 23.3 (a) | 0.3 ± 0.6 (c) | 25.4 ± 23.7 (a) | 3.4 ± 3.2 |
| WLK | 30.9 ± 21.2 (a) | 31.1 ± 21.0 (a) | 0.2 ± 0.6 | 33.7 ± 21.5 (a) | 2.8 ± 2.9 | 36.7 ± 21.8 (a) | 5.8 ± 5.4 | |
| WHK | 39.0 ± 20.2 (a) | 40.4 ± 20.7 (a) | 1.4 ± 3.6 | 43.4 ± 21.0 (a) | 4.4 ± 5.9 (c) | 45.1 ± 21.3 (a) | 6.1 ± 7.0 | |
| MMT | WO | 22.6 ± 10.3 | 23.4 ± 9.8 | 0.8 ± 1.7 | 24.0 ± 9.0 | 1.4 ± 2.5 | 24.6 ± 8.7 | 24.6 ± 8.7 |
| WLK | 24.3 ± 9.3 | 24.9 ± 9.2 | 0.6 ± 2.5 | 25.2 ± 9.4 | 0.9 ± 3.2 | 25.6 ± 9.2 | 25.6 ± 9.2 | |
| WHK | 23.3 ± 10.5 (a) | 23.6 ± 10.1 (a) | 0.4 ±1.0 | 24.5 ± 10.0 (a) | 1.2 ± 1.9 | 24.6 ± 9.3 (a) | 24.6 ± 9.3 | |
| MFT | WO | 13.6 ± 9.1 | 13.1 ± 9.2 | −0.5 ± 1.7 | 13.8 ± 8.6 | 0.2 ± 2.4 | 14.3 ± 9.2 | 0.8 ± 2.8 |
| WLK | 10.5 ± 9.7 (a) | 10.6 ± 9.8 (a) | 0.1 ± 0.3 | 11.7 ± 9.4 (a) | 1.1 ± 2.1 | 12.9 ± 9.6 (a) | 2.3 ± 4.7 | |
| WHK | 9.8 ± 10.1 (a) | 10.6 ± 9.8 (a) | 0.8 ± 2.5 | 11.6 ± 10.1 (a) | 1.8 ± 3.2 | 12.1 ± 10.1 (a) | 2.3 ± 3.7 | |
| MAS | WO | 0.55 ± 0.69 | 0.55 ± 0.69 | 0.00 ± 0.00 | 0.64 ± 0.81 | 0.09 ± 0.30 | 0.64 ± 0.81 | 0.09 ± 0.30 |
| WLK | 0.48 ± 0.60 | 0.52 ± 0.60 | 0.05 ± 0.22 | 0.62 ± 0.67 | 0.14 ± 0.48 | 0.62 ± 0.67 | 0.14 ± 0.48 | |
| WHK | 0.41 ± 0.59 | 0.41 ± 0.59 | 0.00 ± 0.00 | 0.46 ± 0.60 | 0.05 ± 0.21 | 0.46 ± 0.60 | 0.05 ± 0.21 | |
| FIM | WO | 25.2 ± 11.2 | 25.3 ± 11.4 | 0.2 ± 0.4 | 26.2 ± 11.7 | 1.0 ± 2.6 | 26.5 ± 11.8 | 1.3 ± 3.5 |
| WLK | 25.3 ± 10.3 (a) | 25.3 ± 10.7 (a) | 0.0 ± 2.1 | 26.4 ± 10.5 (a) | 1.1 ± 2.6 | 27.1 ± 10.9 (a) | 1.9 ± 3.5 | |
| WHK | 28.8 ± 11.1 (a) | 29.0 ± 10.9 (a) | 0.3 ± 0.8 | 29.5 ± 11.1 (a) | 0.8 ± 2.0 | 30.8 ± 11.2 (a) | 2.0 ± 3.3 | |
| MBC | WO | 4.6 ± 1.7 | 4.6 ± 1.7 | 0.0 ± 0.0 | 4.6 ± 1.7 | 0.0 ± 0.0 | 4.6 ± 1.7 | 0.0 ± 0.0 |
| WLK | 4.7 ± 2.0 | 4.7 ± 2.0 | 0.0 ± 0.0 | 4.7 ± 2.0 | 0.0 ± 0.0 | 4.7 ± 2.0 | 0.0 ± 0.0 | |
| WHK | 3.1 ± 2.2 | 3.0 ± 2.1 | −0.1 ± 0.3 | 3.0 ± 2.1 | −0.1 ± 0.3 | 3.1 ± 2.0 | 0.0 ± 0.5 | |
| MF | WO | 3.1 ± 0.5 | 3.1 ± 0.5 | 0.0 ± 0.0 | 3.1 ± 0.5 | 0.0 ± 0.0 | 3.4 ± 0.7 | 0.3 ± 0.6 |
| WLK | 3.9 ± 1.0 | 3.9 ± 1.0 | 0.0 ± 0.0 | 3.9 ± 1.0 | 0.0 ± 0.0 | 3.9 ± 1.0 | 0.0 ± 0.1 | |
| WHK | 3.4 ± 0.6 | 3.4 ± 0.6 | 0.0 ± 0.0 | 3.4 ± 0.6 | 0.0 ± 0.0 | 3.4 ± 0.6 | 0.0 ± 0.0 | |
| DNM | WO | 7.9 ± 6.7 | 8.0 ± 6.7 | 0.1 ± 0.2 | 8.1 ± 6.7 | 0.1 ± 0.3 | 9.0 ± 6.6 | 1.1 ± 1.3 |
| WLK | 7.4 ± 7.4 | 7.8 ± 7.1 | 0.3 ± 3.0 | 8.3 ± 7.6 | 0.8 ± 4.1 | 9.0 ± 7.4 | 1.5 ± 3.9 | |
| WHK | 8.6 ± 10.7 | 8.6 ± 10.7 | 0.0 ± 0.0 | 8.7 ± 10.7 | 0.0 ± 0.2 | 8.9 ± 10.7 | 0.3 ± 1.0 | |
| K-MMSE | WO | 15.6 ± 9.7 | 13.5 ± 9.7 | |||||
| WLK | 20.4 ± 7.3 | 20.8 ± 6.9 | ||||||
| WHK | 20.1 ± 9.3 | 20.5 ± 9.8 | ||||||
| CDR | WO | 1.2 ± 1.1 | 1.6 ± 1.4 | |||||
| WLK | 0.9 ± 0.8 | 0.9 ± 0.8 | ||||||
| WHK | 1.2 ± 1.3 | 1.1 ± 1.3 |
| Variable | Group | Time | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 1 MPT | Δ1 Month | 3 MPT | Δ3 Months | 6 MPT | Δ6 Months | ||
| BBS | WO | 10.5 ± 17.2 | 10.5 ± 17.2 | 0.0 ± 0.0 | 10.7 ± 17.2 | 0.3 ± 1.0 | 10.8 ± 17.2 | 0.4 ± 1.1 (c) |
| WLK | 14.0 ± 13.3 | 14.5 ± 13.9 | 0.5 ± 0.6 | 15.3 ± 13.9 | 1.3 ± 1.0 | 15.8 ± 15.0 | 1.8 ± 1.7 | |
| WHK | 18.3 ± 14.0 (a) | 20.0 ± 13.6 (a) | 1.8 ± 3.3 | 22.8 ± 14.7 (a) | 4.5 ± 7.6 | 23.5 ± 13.3 (a) | 5.3 ± 6.4 (c) | |
| MBI | WO | 28.2 ± 22.7 | 28.4 ± 23.0 | 0.2 ± 0.8 | 28.6 ± 23.4 | 0.5 ± 1.1 | 29.2 ± 24.2 | 1.0 ± 2.3 |
| WLK | 48.2 ± 18.8 (a) | 48.6 ± 18.3 (a) | 0.4 ± 0.9 | 49.8 ± 18.4 (a) | 1.6 ± 2.2 | 52.9 ± 18.5 (a) | 4.7 ± 7.9 | |
| WHK | 39.8 ± 25.4 (a) | 40.4 ± 25.2 (a) | 0.5 ± 2.2 | 41.6 ± 24.8 (a) | 1.8 ± 3.0 | 44.0 ± 24.6 (a) | 4.1 ± 5.1 | |
| MMT | WO | 24.8 ± 10.7 | 25.0 ± 10.6 | 0.2 ± 0.6 | 25.0 ± 10.6 | 0.1 ± 0.6 | 24.1 ± 10.1 | −0.8 ± 3.4 |
| WLK | 29.0 ± 5.3 (a) | 29.3 ± 5.4 (a) | 0.3 ± 0.9 | 29.4 ± 5.6 (a) | 0.4 ± 1.0 | 30.2 ± 5.5 (a) | 1.2 ± 1.5 | |
| WHK | 24.5 ± 7.9 (a) | 24.6 ± 7.8 (a) | 0.1 ± 0.4 | 24.9 ± 7.8 (a) | 0.4 ± 0.7 | 25.2 ± 7.7 (a) | 0.7 ± 1.2 | |
| MFT | WO | 12.1 ± 12.0 (a) | 12.4 ± 11.7 (a) | 0.3 ± 1.1 | 12.9 ± 11.8 (a) | 0.8 ± 1.1 | 12.7 ± 11.8 (a) | 0.6 ± 1.3 |
| WLK | 14.2 ± 8.6 (a) | 14.4 ± 8.7 (a) | 0.1 ± 0.5 | 14.7 ± 8.8 (a) | 0.5 ± 0.9 | 15.2 ± 9.0 (a) | 1.0 ± 1.4 | |
| WHK | 8.1 ± 7.3 (a) | 8.5 ± 7.1 (a) | 0.4 ± 1.8 | 8.9 ± 7.2 (a) | 0.8 ± 1.8 | 9.4 ± 7.4 (a) | 1.3 ± 2.0 | |
| MAS | WO | 1.2 ± 1.0 | 1.2 ± 1.0 | 0.0 ± 0.0 | 1.1 ± 0.9 | −0.1 ± 0.3 | 1.1 ± 0.9 | −0.1 ± 0.3 |
| WLK | 0.7 ± 0.5 | 0.7 ± 0.5 | 0.0 ± 0.0 | 0.7 ± 0.5 | 0.0 ± 0.0 | 0.5 ± 0.5 | −0.2 ± 0.4 | |
| WHK | 1.1 ± 0.9 | 1.0 ± 0.9 | 0.0 ± 0.2 | 1.0 ± 0.9 | 0.0 ± 0.2 | 1.0 ± 0.9 | 0.0 ± 0.2 | |
| FIM | WO | 27.4 ± 13.6 | 27.4 ± 13.6 | −0.1 ± 0.3 | 27.3 ± 13.2 | −0.1 ± 3.1 | 27.0 ± 13.6 | −0.4 ± 3.3 |
| WLK | 35.2 ± 11.1 | 35.3 ± 11.2 | 0.1 ± 0.3 | 35.6 ± 10.8 | 0.5 ± 0.9 | 36.4 ± 10.6 | 1.2 ± 2.4 | |
| WHK | 30.7 ± 11.1 (a) | 30.9 ± 11.2 (a) | 0.2 ± 0.7 | 31.7 ± 11.2 (a) | 1.0 ± 2.2 | 32.0 ± 10.7 (a) | 1.2 ± 1.7 | |
| MBC | WO | 4.2 ± 2.5 | 4.2 ± 2.5 | 0.0 ± 0.0 | 4.2 ± 2.5 | 0.0 ± 0.0 | 4.2 ± 2.5 | 0.0 ± 0.0 |
| WLK | 4.4 ± 1.5 | 4.4 ± 1.5 | 0.0 ± 0.0 | 4.4 ± 1.5 | 0.0 ± 0.0 | 4.4 ± 1.5 | 0.0 ± 0.0 | |
| WHK | 2.8 ± 2.0 | 2.8 ± 2.0 | 0.0 ± 0.0 | 2.8 ± 2.0 | 0.0 ± 0.0 | 2.8 ± 2.0 | 0.0 ± 0.0 | |
| MF | WO | 3.6 ± 1.5 | 3.6 ± 1.5 | 0.0 ± 0.0 | 3.6 ± 1.5 | 0.0 ± 0.0 | 3.6 ± 1.5 | 0.0 ± 0.0 |
| WLK | 3.8 ± 0.8 | 3.8 ± 0.8 | 0.0 ± 0.0 | 3.8 ± 0.8 | 0.0 ± 0.0 | 3.9 ± 0.7 | 0.1 ± 0.3 | |
| WHK | 3.5 ± 1.0 | 3.5 ± 1.0 | 0.0 ± 0.0 | 3.5 ± 1.0 | 0.0 ± 0.0 | 3.4 ± 1.0 | 0.0 ± 0.1 | |
| DNM | WO | 8.6 ± 12.3 | 8.4 ± 12.1 | −0.2 ± 0.7 | 8.7 ± 12.5 | 0.1 ± 0.3 | 8.7 ± 12.3 | 0.1 ± 0.2 |
| WLK | 6.0 ± 7.7 | 6.1 ± 7.7 | 0.1 ± 0.3 | 6.2 ± 8.0 | 0.2 ± 0.5 | 7.3 ± 8.1 | 1.4 ± 2.5 | |
| WHK | 7.7 ± 10.3 | 7.7 ± 10.3 | 0.0 ± 0.0 | 7.5 ± 10.2 | −0.2 ± 0.5 | 7.8 ± 10.2 | 0.1 ± 0.6 | |
| MMSE | WO | 16.6 ± 11.6 | 16.4 ± 11.9 | |||||
| WLK | 15.1 ± 11.8 | 16.1 ± 10.2 | ||||||
| WHK | 19.9 ± 7.8 (e) | 20.8 ± 7.8 (e) | ||||||
| CDR | WO | 1.5 ± 1.5 | 1.5 ±1.5 | |||||
| WLK | 0.8 ± 1.1 | 1.0 ±1.0 | ||||||
| WHK | 1.1 ± 0.8 | 1.0 ±0.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, D.; Ahn, S.H.; Jung, H.J. The Effect of Integrative Treatment on Improving Functional Level in Stroke Patients: A Retrospective Chart Review. Healthcare 2025, 13, 1452. https://doi.org/10.3390/healthcare13121452
Kwon D, Ahn SH, Jung HJ. The Effect of Integrative Treatment on Improving Functional Level in Stroke Patients: A Retrospective Chart Review. Healthcare. 2025; 13(12):1452. https://doi.org/10.3390/healthcare13121452
Chicago/Turabian StyleKwon, Daegil, Sun Hee Ahn, and Hyun Jung Jung. 2025. "The Effect of Integrative Treatment on Improving Functional Level in Stroke Patients: A Retrospective Chart Review" Healthcare 13, no. 12: 1452. https://doi.org/10.3390/healthcare13121452
APA StyleKwon, D., Ahn, S. H., & Jung, H. J. (2025). The Effect of Integrative Treatment on Improving Functional Level in Stroke Patients: A Retrospective Chart Review. Healthcare, 13(12), 1452. https://doi.org/10.3390/healthcare13121452







