Beyond the Clinic Walls: Examining Radiology Technicians’ Experiences in Home-Based Radiography
Abstract
1. Introduction
1.1. Background
1.2. The Rationale for the Study and Purpose
2. Methods
- Single choice questions;
- Multiple choice questions;
- Evaluation (graded) questions (with a 6-level psychometric scale);
- Likert questions with a 6-level scale;
- Open-ended questions (in a few cases).
3. Results
3.1. The Outcome of the Electronic Survey
3.1.1. Insights into the Study Participants: Unveiling Characteristics of the Sample
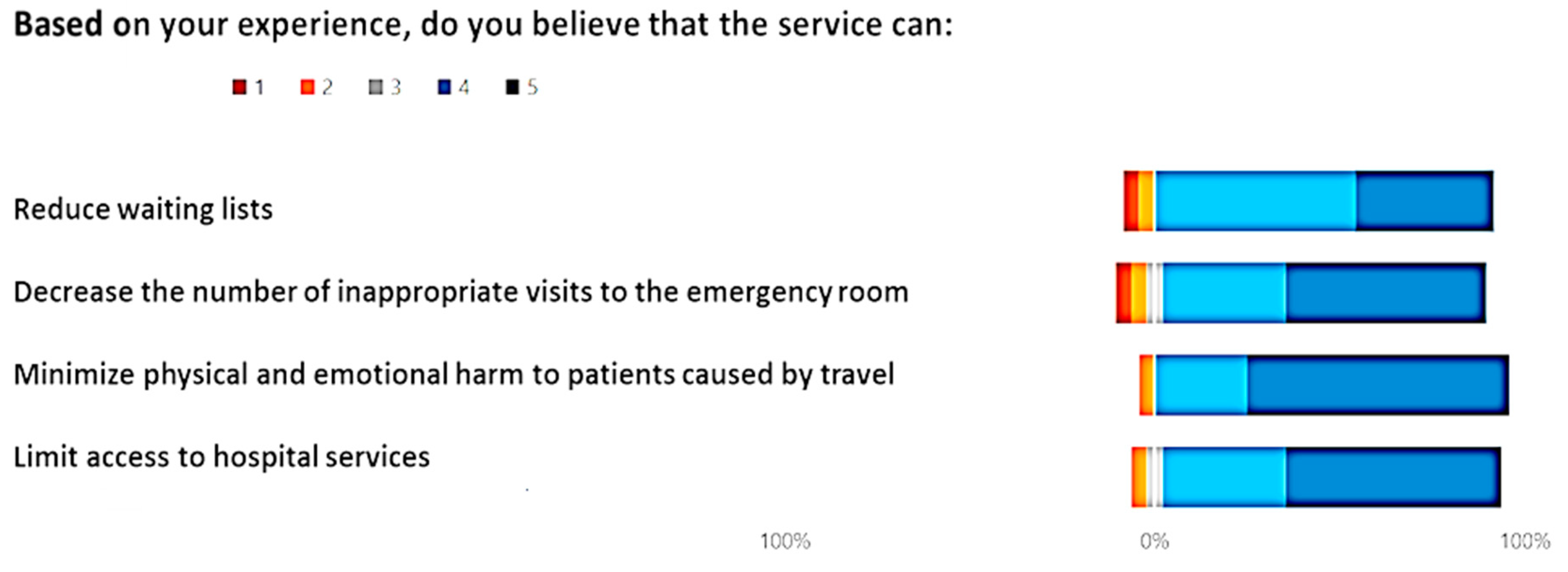
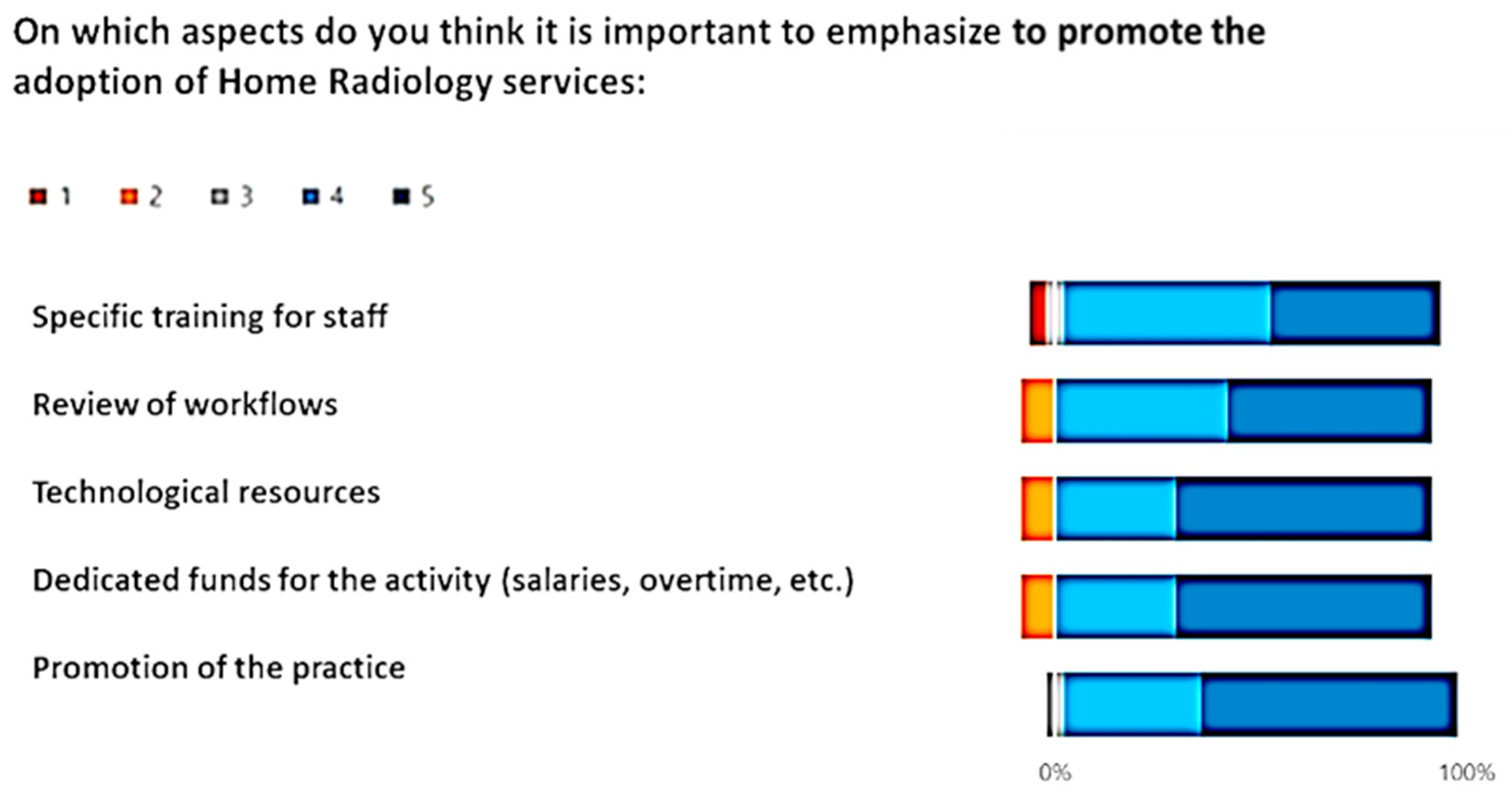
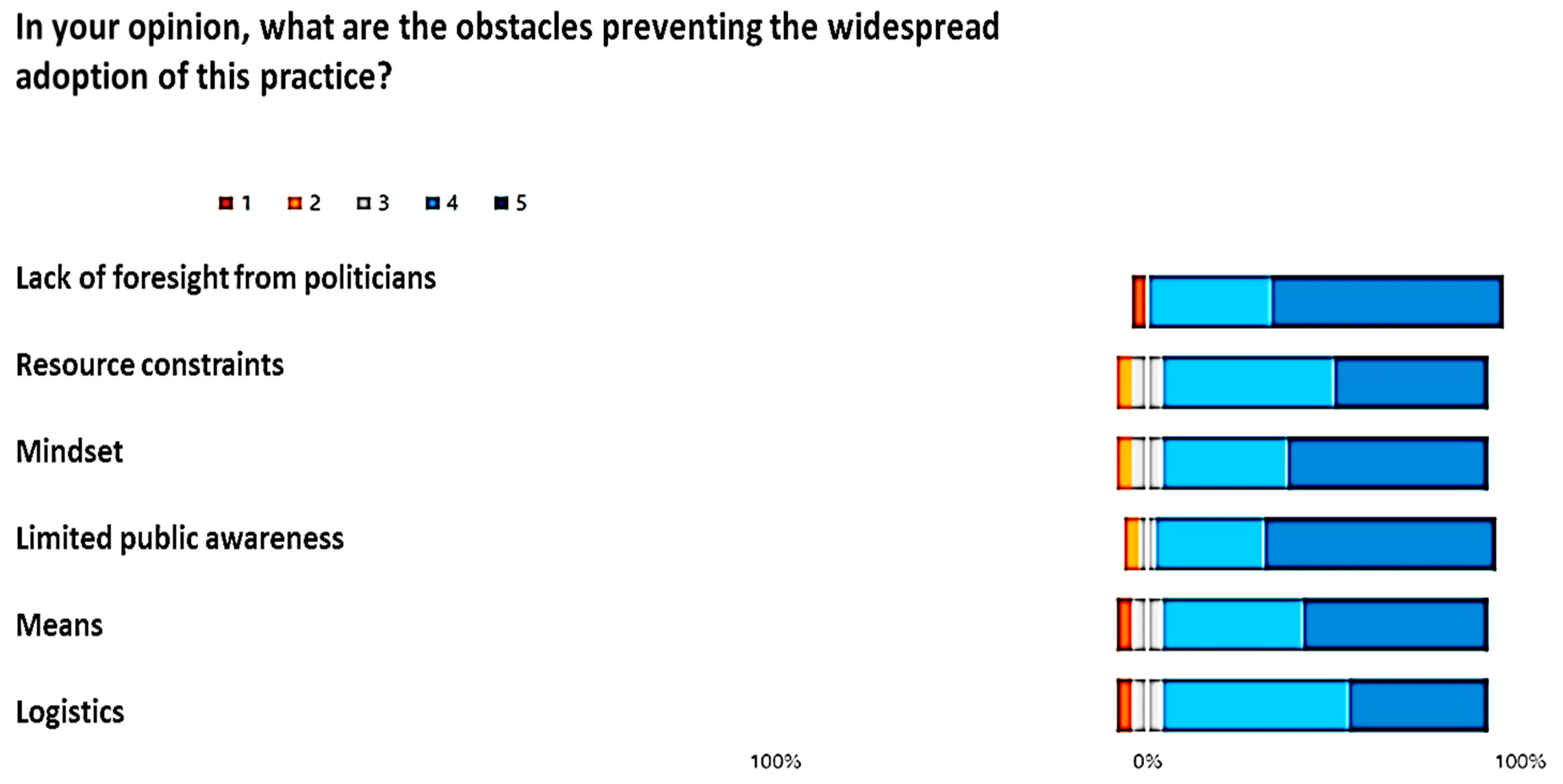
3.1.2. Findings from Graded, Multiple-Choice, and Likert Scale Questions
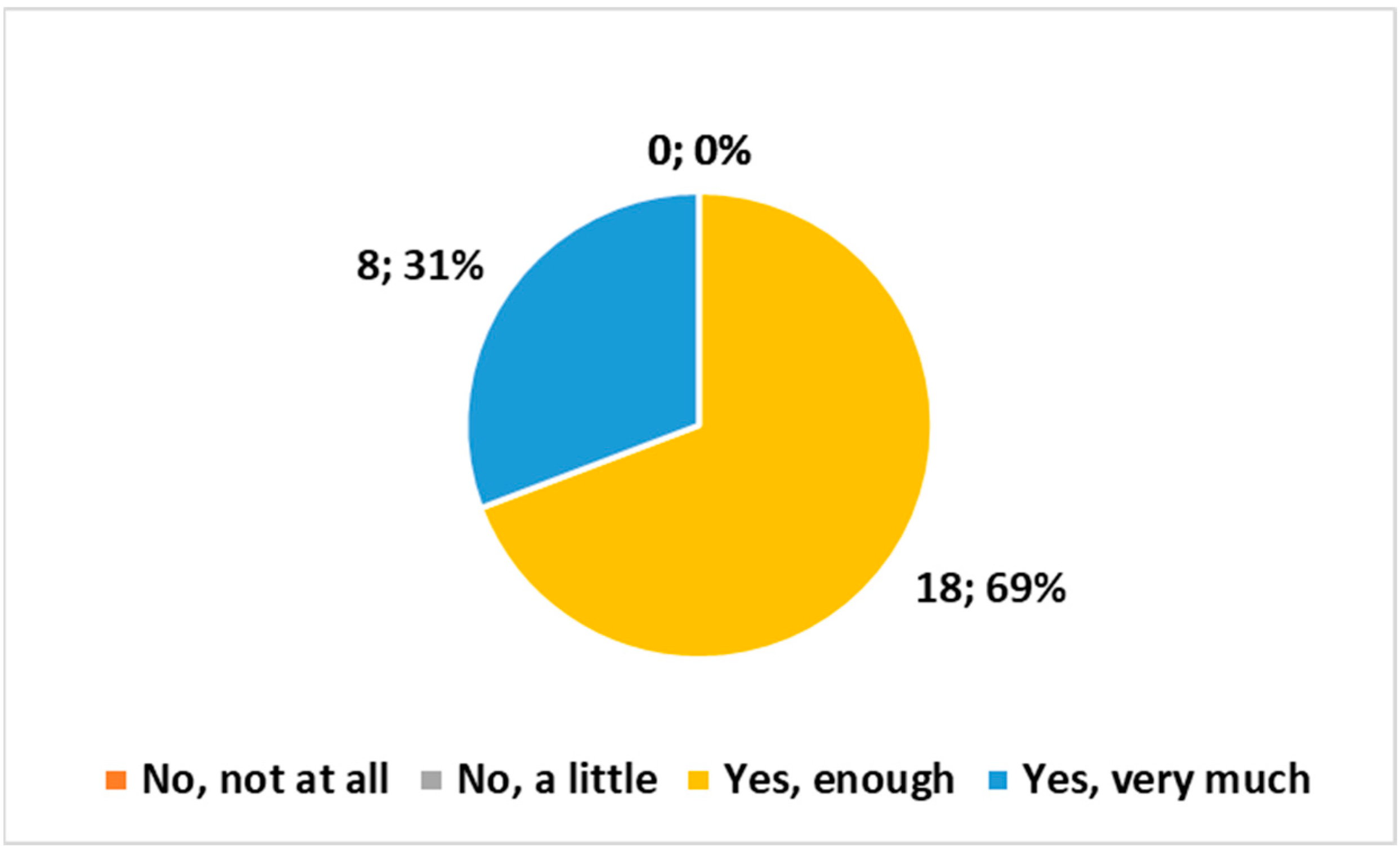
- “Do you believe that the examination conducted at home complies with the safety requirements regarding exposure to ionizing radiation?”
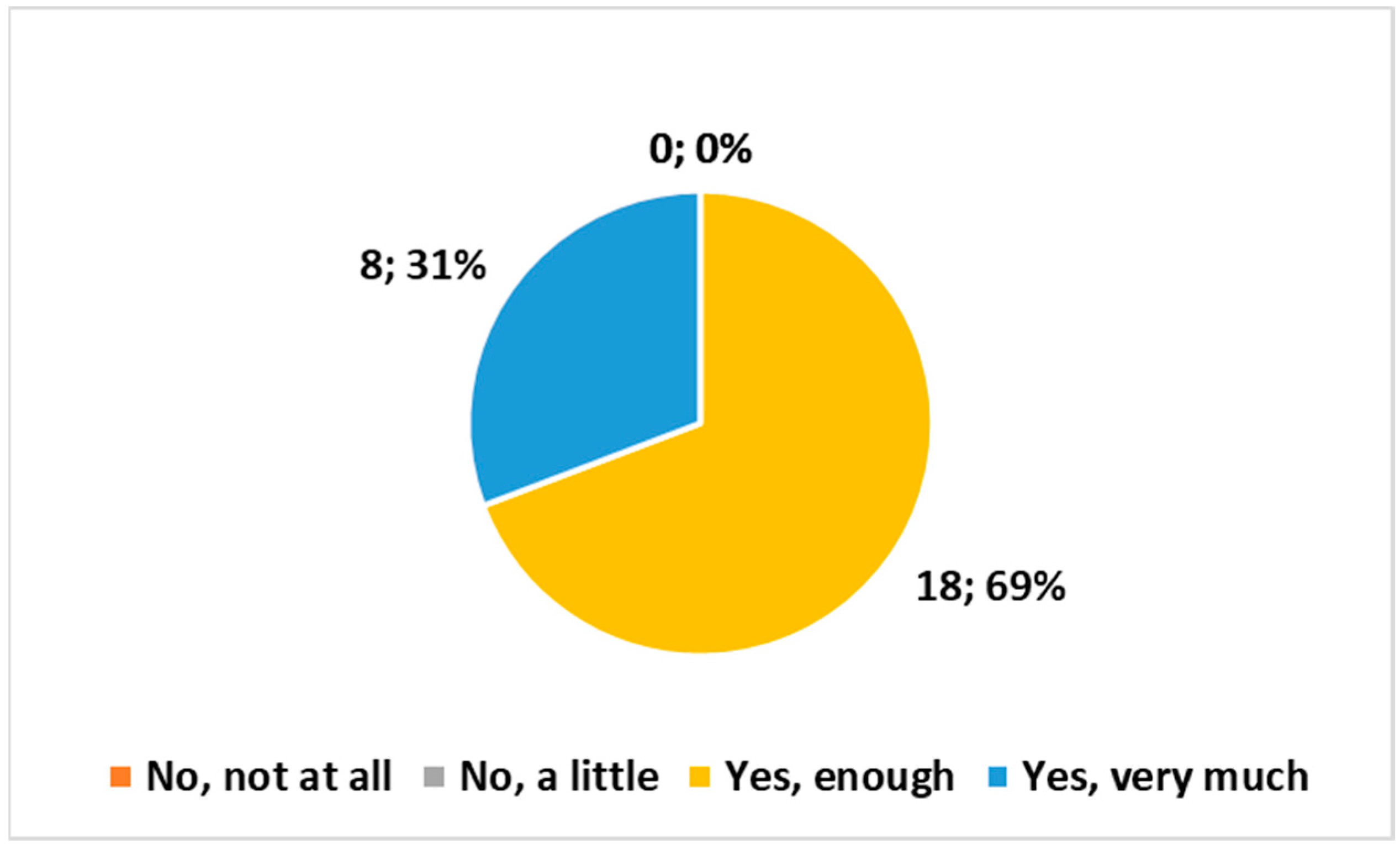
- “Are the means and technologies (vehicle, PC, radiological equipment, etc.) provided by the Health Authority suitable for delivering the service?”
- “Do you believe it is important for the MRT to be part of the Integrated Home Care team?”
- “How important do you consider listening to the problems of the patient or family/caregivers?”
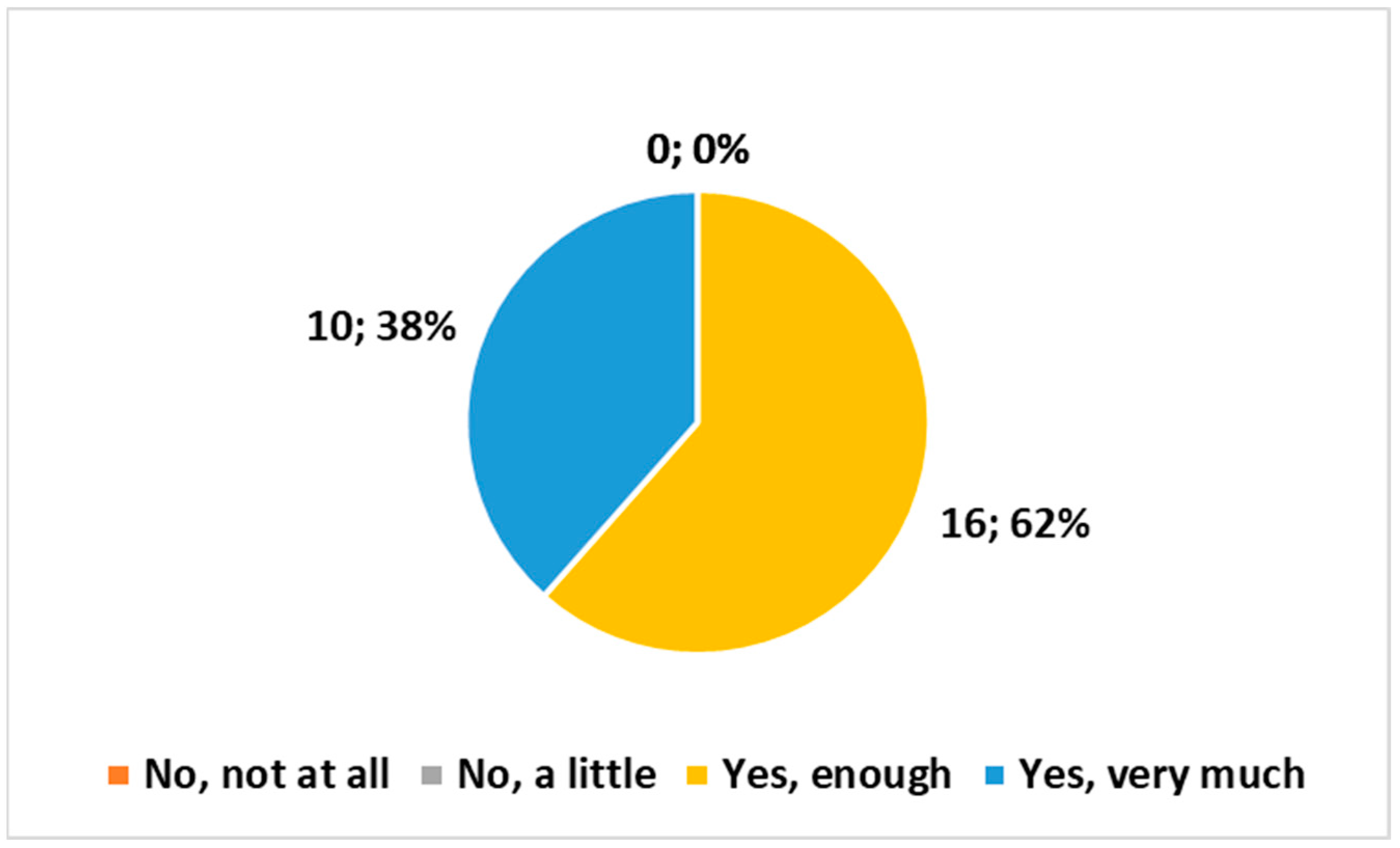
- “Overall, how satisfied are you with the Home Radiology service?”
3.1.3. Unveiling Insights from Open-Ended Responses: A Dual Perspective on Feedback and the Future of Home Radiology
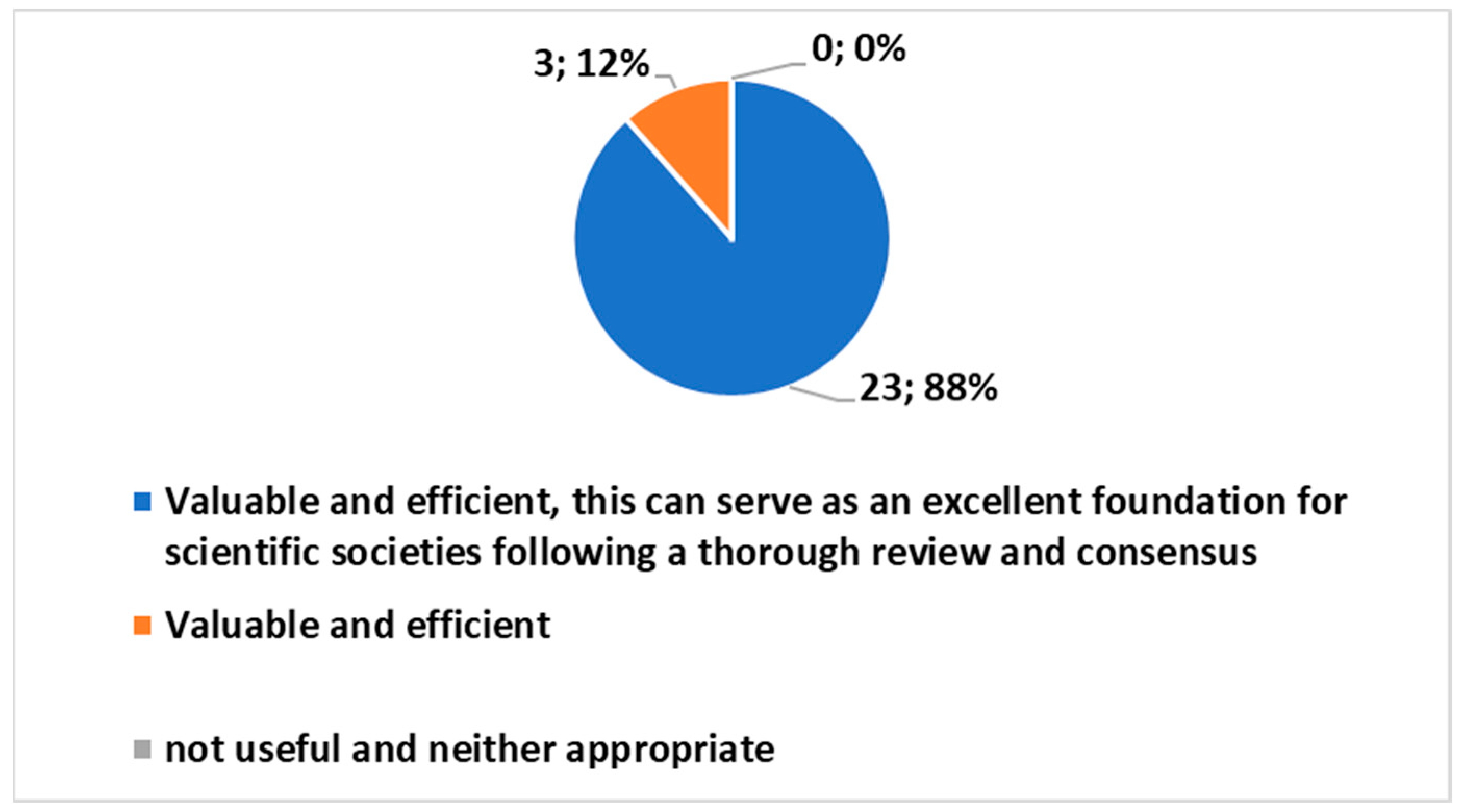
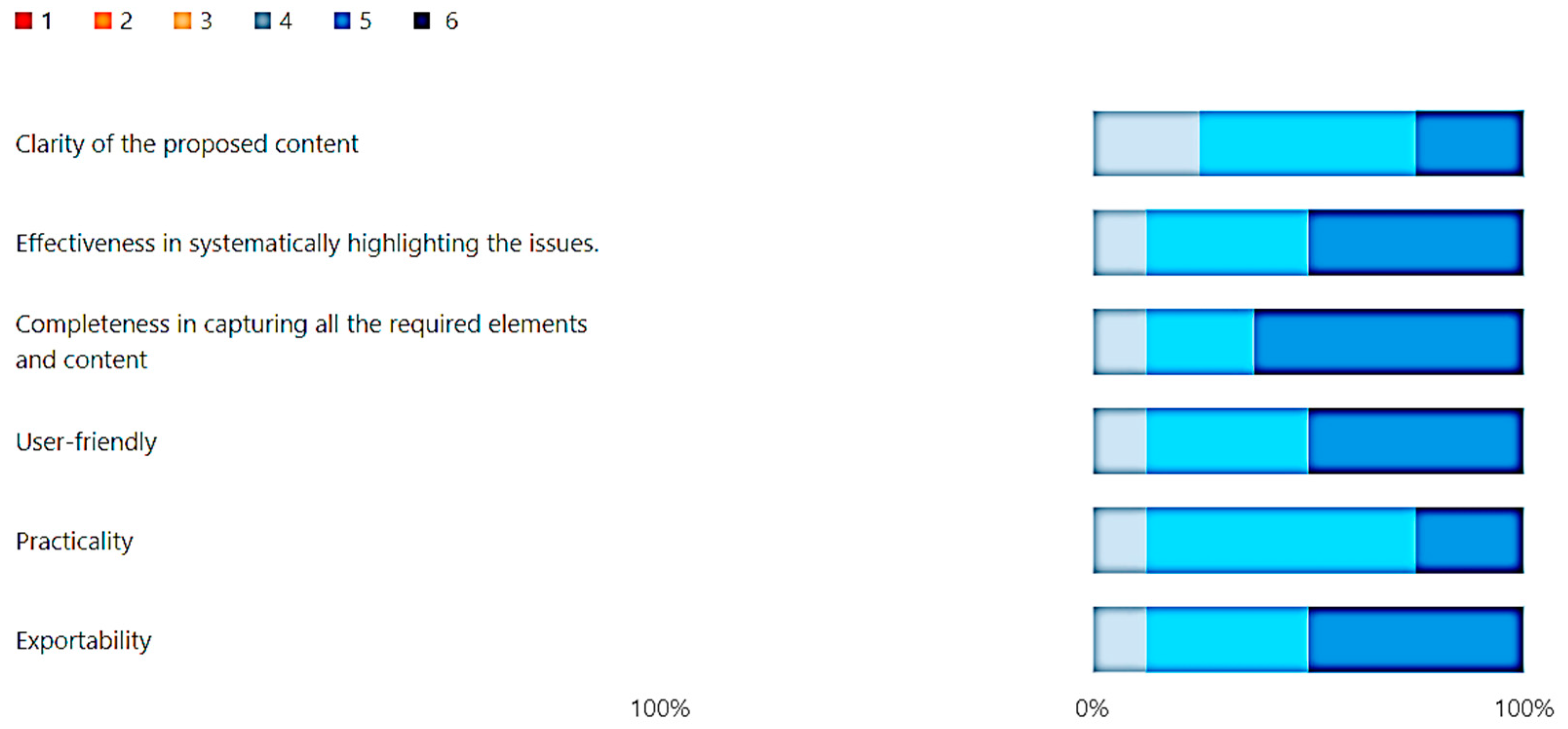
3.2. The Outcome of the Electronic Feedback Form
3.2.1. Identification of the Expert Observer Group
3.2.2. In-Depth Feedback through the Electronic Feedback Form
3.3. Comprehensive Insights Summary
3.3.1. Insight Summary from the Electronic Survey
3.3.2. Insight Summary from the Electronic Feedback Form
4. Discussion
4.1. Key Discoveries: Opportunities, Challenges, and Issues
- The CAWI ES Tool:
- High Acceptance Level of the ES CAWI tool:
- CAWI Tools:
- Specific Outcome:
4.2. Takeaway Message
4.3. Work in Progress
4.4. Key Recommendations for Advancing Further Research
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Toppenberg, M.D.; Christiansen, T.E.M.; Rasmussen, F.; Nielsen, C.P.; Damsgaard, E.M. Mobile X-ray outside the hospital: A scoping review. BMC Health Serv. Res. 2020, 20, 767. [Google Scholar] [CrossRef]
- LOSEV, I.K. Improvement of quality of roentgenological work in villages by improvement of mobile x-ray units. Vestn. Rentgenol. Radiol. 1958, 33, 86–87. (In Russian) [Google Scholar]
- Mark, S.; Henderson, D.; Brealey, J. Taking acute medical imaging to the patient, the domiciliary based X-ray response team. Radiography 2022, 28, 550–552. [Google Scholar] [CrossRef]
- Kjelle, E.; Kleven, L.; Olerud, H.M.; Melberg, H.O. Cost analysis of mobile radiography services for nursing home residents in Southeast Norway. J. Eval. Clin. Pract. 2019, 25, 275–281. [Google Scholar] [CrossRef]
- Andersen, P.A.B.; Precht, H.; McEntee, M.F.; Pedersen, M.R.V. How to set up a mobile X-ray unit in the community—Implementation initiatives for patient-centred care. Radiography 2023, 29 (Suppl. S1), S148–S151. [Google Scholar] [CrossRef]
- Dollard, J.; Edwards, J.; Yadav, L.; Gaget, V.; Tivey, D.; Inacio, M.; Maddern, G.; Visvanathan, R. Residents’ perspectives of mobile X-ray services in support of healthcare-in-place in residential aged care facilities: A qualitative study. BMC Geriatr. 2022, 22, 525. [Google Scholar] [CrossRef]
- Sawyer, R.H.; Patel, U.; Horrocks, A.W. Domiciliary radiography: An important service? Clin. Radiol. 1995, 50, 51–55. [Google Scholar] [CrossRef]
- Aldridge, R.W.; Hayward, A.C.; Hemming, S.; Possas, L.; Ferenando, G.; Garber, E.; Lipman, M.; McHugh, T.D.; Story, A. Effectiveness of peer educators on the uptake of mobile X-ray tuberculosis screening at homeless hostels: A cluster randomised controlled trial. BMJ Open 2015, 5, e008050. [Google Scholar] [CrossRef]
- Kjelle, E.; Lysdahl, K.B. Mobile radiography services in nursing homes: A systematic review of residents’ and societal outcomes. BMC Health Serv. Res. 2017, 17, 231. [Google Scholar] [CrossRef] [PubMed]
- Datta, B.; Hazarika, A.; Shewade, H.D.; Ayyagari, K.; Kumar, A.M. Digital chest X-ray through a mobile van: Public private partnership to detect sputum negative pulmonary TB. BMC Res. Notes 2017, 10, 96. [Google Scholar] [CrossRef]
- Dicle, O.; Şenol, U.; Özmen, M.N.; Aydıngöz, Ü. A snapshot of teleradiology practice in Turkey: The results of a survey among radiologists. Diagn. Interv. Radiol. 2023, 29, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Dzefi-Tettey, K.; Kobina Mesi Edzie, E.; Brakohiapa, E.K.; Gorleku, P.N.; Amankwa, A.T.; Abdulai, A.B.; Yabasin, I.B.; Kekessie, K.K.; Idun, E.A.; Ntiamoah-Koufie, C.E.; et al. Career in radiology; the Ghanaian clinical medical Student’s perception. Heliyon 2022, 8, e12603. [Google Scholar] [CrossRef] [PubMed]
- Vabo, S.; Steen, K.; Brudvik, C.; Hunskaar, S.; Morken, T. Patient-reported outcomes after initial conservative fracture treatment in primary healthcare—A survey study. BMC Prim. Care 2022, 23, 191. [Google Scholar] [CrossRef] [PubMed]
- Macedo, F.S.; Silva, P.G.B.; Marçal, E.B.F.; Rolim, J.P.M.L. Evaluation of Usability, Perception of Usefulness, and Efficiency of an Application in Interpreting Imaging Examinations and Supporting Decision-Making in Orthopedics. Telemed. e-Health 2021, 27, 561–567. [Google Scholar] [CrossRef] [PubMed]
- Florin, M.; Pinar, U.; Chavigny, E.; Bouaboula, M.; Jarboui, L.; Coulibaly, A.; Lemogne, C.; Fournier, L. Socio-economic and psychological impact of the COVID-19 outbreak on private practice and public hospital radiologists. Eur. J. Radiol. 2020, 132, 109285. [Google Scholar] [CrossRef] [PubMed]
- Yamashiro, T.; Kumamaru, K.K.; Kido, A.; Namoto Matsubayashi, R.; Ota, H.; Ida, M.; Aoki, S. Joint Committee for Diversity Promotion and Work-Style Reform of the Japan Radiological Society and the Japanese College of Radiology. Work-style reform and use of information and communication technology among diagnostic radiologists in Japan: Results of the 2018 JRS/JCR joint survey. Jpn. J. Radiol. 2020, 38, 636–642. [Google Scholar] [CrossRef] [PubMed]
- van Hoek, J.; Huber, A.; Leichtle, A.; Härmä, K.; Hilt, D.; von Tengg-Kobligk, H.; Heverhagen, J.; Poellinger, A. A survey on the future of radiology among radiologists, medical students and surgeons: Students and surgeons tend to be more skeptical about artificial intelligence and radiologists may fear that other disciplines take over. Eur. J. Radiol. 2019, 121, 108742. [Google Scholar] [CrossRef] [PubMed]
- Coppola, F.; Bibbolino, C.; Grassi, R.; Pierotti, L.; Silverio, R.; Lassandro, F.; Neri, E.; Regge, D. Results of an Italian survey on teleradiology. La Radiol. Medica 2016, 121, 652–659. [Google Scholar] [CrossRef]
- Jacobs, J.J.W.M.; Ekkelboom, R.; Jacobs, J.P.A.M.; van der Molen, T.; Sanderman, R. Patient satisfaction with a teleradiology service in general practice. BMC Fam. Pract. 2016, 17, 17. [Google Scholar] [CrossRef]
- Brenke, C.; Lassel, E.A.; Terris, D.; Kurt, A.; Schmieder, K.; Schoenberg, S.O.; Weisser, G. On-call service of neurosurgeons in Germany: Organization, use of communication services, and personal acceptance of modern technologies. J. Neurol. Surg. Part A Cent. Eur. Neurosurg. 2013, 75, 217–223. [Google Scholar] [CrossRef]
- Kim, J.E.; Song, Y.M.; Park, J.H.; Lee, J.R. Attitude of korean primary care family physicians towards telehealth. Korean J. Fam. Med. 2011, 32, 341–351. [Google Scholar] [CrossRef]
- Lindsay, R.; McKinstry, S.; Vallely, S.; Thornbury, G. What influences clinician’s satisfaction with radiology services? Insights Imaging 2011, 2, 425–430. [Google Scholar] [CrossRef]
- Winblad, I.; Hämäläinen, P.; Reponen, J. What is found positive in healthcare information and communication technology implementation?-the results of a nationwide survey in Finland. Telemed. e-Health 2011, 17, 118–123. [Google Scholar] [CrossRef]
- Ninos, K.; Spiros, K.; Glotsos, D.; Georgiadis, P.; Sidiropoulos, K.; Dimitropoulos, N.; Kalatzis, I.; Cavouras, D. Development and evaluation of a PDA-based teleradiology terminal in thyroid nodule diagnosis. J. Telemed. Telecare 2010, 16, 232–236. [Google Scholar] [CrossRef]
- Giansanti, D.; Di Basilio, F. The Artificial Intelligence in Digital Radiology: Part 1: The Challenges, Acceptance and Consensus. Healthcare 2022, 10, 509. [Google Scholar] [CrossRef] [PubMed]
- Di Basilio, F.; Esposisto, G.; Monoscalco, L.; Giansanti, D. The Artificial Intelligence in Digital Radiology: Part 2: Towards an Investigation of acceptance and consensus on the Insiders. Healthcare 2022, 10, 153. [Google Scholar] [CrossRef] [PubMed]
- Giansanti, D.; Rossi, I.; Monoscalco, L. Lessons from the COVID-19 Pandemic on the Use of Artificial Intelligence in Digital Radiology: The Submission of a Survey to Investigate the Opinion of Insiders. Healthcare 2021, 9, 331. [Google Scholar] [CrossRef] [PubMed]
- Papi, R.; Grosso, M.; Cardelli, D.; Nocentini, C.; Lorenzini, C.; Messina, G.; Nante, N. Sperimentazione di un servizio di Radiologia Domiciliare per non deambulanti nell’Azienda USL Toscana Sud Est. Mondo Sanit. 2018, 25, 1–18. [Google Scholar]
- Lepri, G.; Pentiricci, A.; Ferranti, A.; Abbritti, E.; Rossi, G.; Nappini, M.; Fiordelli, P.; Papa, V. La Radiologia Domiciliare, alla luce dell’applicazione del D.M. 77/2022: Modelli e Standard per lo sviluppo, dell’Assistenza nel Territorio. In “Sfide e Opportunità per il S.S.N. I Professionisti Della Salute Leva per il Cambiamento” Supplemento Sanità 4.0; Pubblicazione dei Forum di Federsanità; Confederazione Federsanità ANCI Regionali: Torino, Italy, 2023; pp. 234–237. [Google Scholar]
- Lennartz, S.; Dratsch, T.; Zopfs, D.; Persigehl, T.; Maintz, D.; Hokamp, N.G.; Dos Santos, D.P. Use and Control of Artificial Intelligence in Patients Across the Medical Workflow: Single-Center Questionnaire Study of Patient Perspectives. J. Med. Internet Res. 2021, 23, e24221. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Citardi, D.; Wang, D.; Genc, Y.; Shan, J.; Fan, X. Patients’ perceptions of using artificial intelligence (AI)-based technology to comprehend radiology imaging data. Health Inform. J. 2021, 27, 14604582211011215. [Google Scholar] [CrossRef]
- Ongena, Y.P.; Haan, M.; Yakar, D.; Kwee, T.C. Patients’ views on the implementation of artificial intelligence in radiology: Development and validation of a standardized questionnaire. Eur. Radiol. 2020, 30, 1033–1040. [Google Scholar] [CrossRef] [PubMed]
- Hendrix, N.; Hauber, B.; Lee, C.I.; Bansal, A.; Veenstra, D.L. Artificial intelligence in breast cancer screening: Primary care provider preferences. J. Am. Med. Inform. Assoc. 2021, 28, 1117–1124. [Google Scholar] [CrossRef]
- Abuzaid, M.M.; Elshami, W.; McConnell, J.; Tekin, H.O. An extensive survey on radiographers from the Middle East and India on artificial intelligence integration in radiology practice. Health Technol. 2021, 11, 1045–1050. [Google Scholar] [CrossRef] [PubMed]
- Abuzaid, M.M.; Tekin, H.O.; Reza, M.; Elhag, I.R.; Elshami, W. Assessment of MRI technologists in acceptance and willingness to integrate artificial intelligence into practice. Radiography 2021, 27, S83–S87. [Google Scholar] [CrossRef] [PubMed]
- Abuzaid, M.M.; Elshami, W.; Tekin, H.; Issa, B. Assessment of the Willingness of Radiologists and Radiographers to Accept the Integration of Artificial Intelligence into Radiology Practice. Acad. Radiol. 2020, 29, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Alelyani, M.; Alamri, S.; Alqahtani, M.S.; Musa, A.; Almater, H.; Alqahtani, N.; Alshahrani, F.; Alelyani, S. Radiology Community Attitude in Saudi Arabia about the Applications of Artificial Intelligence in Radiology. Healthcare 2021, 9, 834. [Google Scholar] [CrossRef] [PubMed]
- European Society of Radiology (ESR). Impact of artificial intelligence on radiology: A EuroAIM survey among members of the European Society of Radiology. Insights Imaging 2019, 10, 105. [Google Scholar] [CrossRef]
- Galán, G.C.; Portero, F.S. Medical students’ perceptions of the impact of artificial intelligence in Radiology. Radiologia, 2021; in press. [Google Scholar]
- Aldosari, B. User acceptance of a picture archiving and communication system (PACS) in a Saudi Arabian hospital radiology department. BMC Med. Inform. Decis. Mak. 2012, 12, 44. [Google Scholar] [CrossRef]


| Study | Location | Focus |
|---|---|---|
| Andersen et al. (2023) [5] | Community settings | Implementation initiatives for patient-centered care through setting up a mobile X-ray unit in the community |
| Dollard et al. (2022) [6] | Residential aged care facility | Residents’ perspectives on mobile X-ray services supporting healthcare-in-place in aged care facilities |
| Kjelle et al. (2019) [4] | Nursing homes in Southeast Norway | Cost analysis of mobile radiography services for nursing home residents |
| Aldridge et al. (2015) [8] | Homeless hostels | Effectiveness of peer educators on the uptake of mobile X-ray tuberculosis screening |
| Kjelle and Lysdahl (2017) [9] | Nursing homes | Investigation on services in nursing homes, examining residents’ and societal outcomes |
| Datta et al. (2017) [10] | Public–private partnership | Detection of sputum-negative pulmonary TB through digital chest X-ray conducted via a mobile van |
| Participants | Males/Females | Min Age/Max Age | Mean Age |
|---|---|---|---|
| 186 | 80/106 | 34/59 | 45.6 |
| Experience in HR | Males/Females | Min Age/Max Age | Mean Age |
|---|---|---|---|
| 26 | 16/10 | 33/58 | 46.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lepri, G.; Oddi, F.; Gulino, R.A.; Giansanti, D. Beyond the Clinic Walls: Examining Radiology Technicians’ Experiences in Home-Based Radiography. Healthcare 2024, 12, 732. https://doi.org/10.3390/healthcare12070732
Lepri G, Oddi F, Gulino RA, Giansanti D. Beyond the Clinic Walls: Examining Radiology Technicians’ Experiences in Home-Based Radiography. Healthcare. 2024; 12(7):732. https://doi.org/10.3390/healthcare12070732
Chicago/Turabian StyleLepri, Graziano, Francesco Oddi, Rosario Alfio Gulino, and Daniele Giansanti. 2024. "Beyond the Clinic Walls: Examining Radiology Technicians’ Experiences in Home-Based Radiography" Healthcare 12, no. 7: 732. https://doi.org/10.3390/healthcare12070732
APA StyleLepri, G., Oddi, F., Gulino, R. A., & Giansanti, D. (2024). Beyond the Clinic Walls: Examining Radiology Technicians’ Experiences in Home-Based Radiography. Healthcare, 12(7), 732. https://doi.org/10.3390/healthcare12070732






