Implementing Lived Experience Workshops in Regional Areas of British Columbia to Enhance Clinicians’ Confidence in Spinal Cord Injury Care: An Evaluation
Abstract
1. Introduction
2. Materials and Methods
2.1. Persons with Lived Experience Participants and Priorities
2.2. Clinician Participants and Priorities
2.3. Educational Workshops—A Quality Improvement Project
2.4. Post-Workshop Data Collection
2.5. Data Analysis
3. Results
3.1. Community Perspectives and Priorities
3.1.1. Persons with Lived Experience Participants’ Community Priorities
3.1.2. Clinical Team Members Priorities
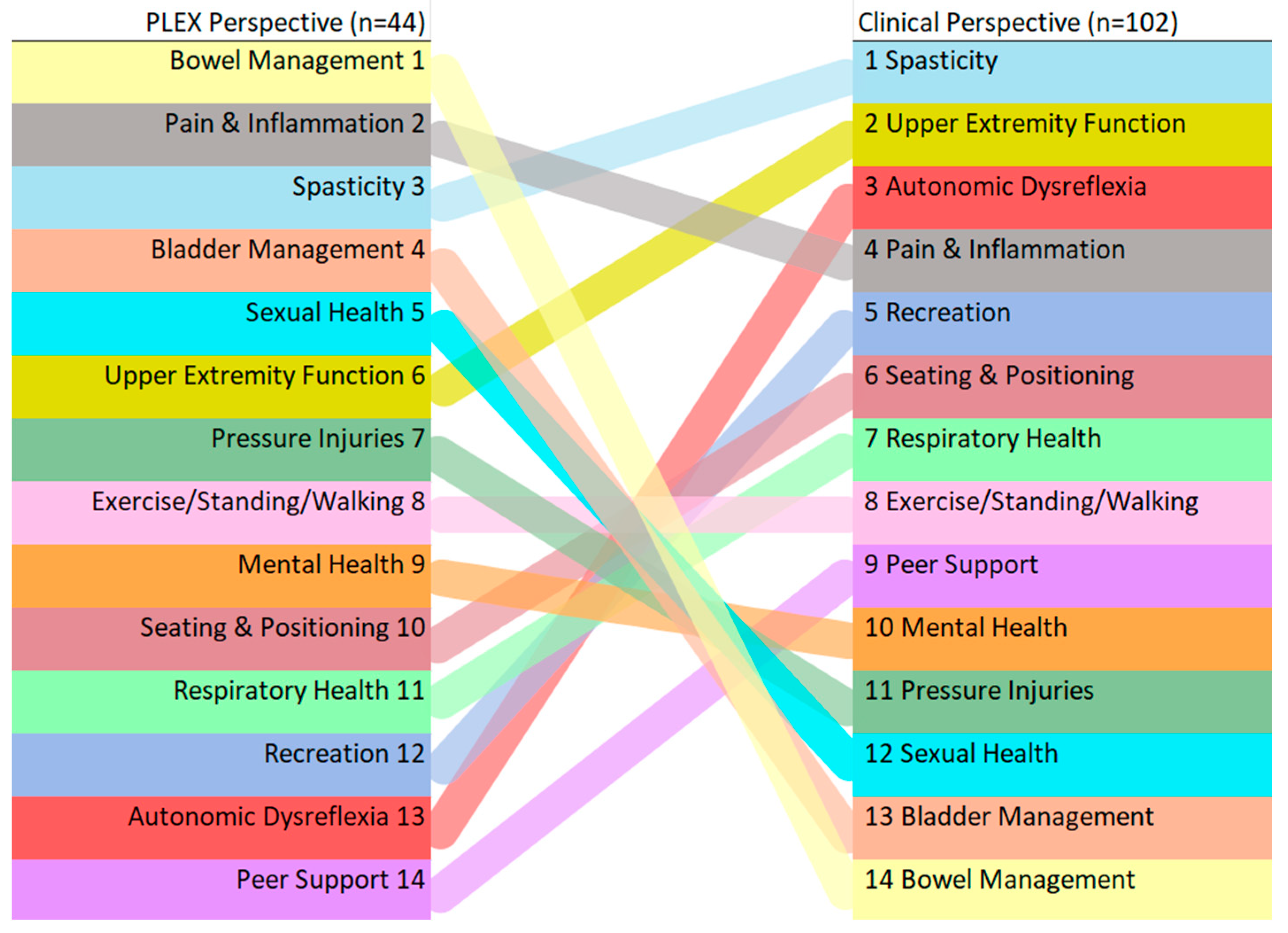
3.1.3. Comparing Community Rankings of Priority Spinal Cord Injury—Health-Related Topics
3.2. Workshop Surveys and Feedback
3.2.1. Spinal Cord Injury 101 Session Survey Results
- 1.
- Spasticity (15/29);
- 2.
- Transitioning from rehab to community (14/29);
- 3t.
- Bladder/bowel management (12/29);
- 3t.
- Sexual health (12/29).
3.2.2. Pressure Injury Workshop Survey Results
- Hearing personal experiences of pressure injuries (33/39);
- Learning about quality of life and financial costs of PI (27/39);
- Impacts of healthcare system of pressure injuries (25/39);
- Prevention of pressure injuries (17/39).
- Better education for staff (24/39);
- Funding shortages (22/39);
- Awareness of the complicated/sensitive nature of pressure injuries (14/39);
- Client involvement * (12/39) (* Client participation in treatment plans is mainly out of the client’s control, making client involvement challenging to measure and improve).
- Access to specialized equipment/supplies (27/39);
- Workload limitation/time (26/39);
- Lack of specialized clinicians (22/39);
- Resources—where/how to find information (17/39).
3.2.3. Persons with Lived Experience Panel Session Survey Results
- 1t.
- Transitioning from rehab to community (29/31);
- 1t.
- Challenges with the healthcare system (29/31);
- 3.
- Bladder/bowel management (24/31);
- 4.
- Psychosocial adjustment to SCI (18/31).
- Increased knowledge and confidence (15/31);
- Better ability to provide client-centred care (10/31);
- Mindfulness of language used when speaking with PLEX (8/31);
- Expanding treatment goals (3/31).
- 1.
- Resources—where/how to find information (20/31);
- 2.
- Lack of specialized clinicians (19/31);
- 3t.
- Access to specialized equipment/supplies (16/31);
- 3t.
- Workload limitation/time (16/31).
3.2.4. Workshop Participants Feedback
4. Discussion
4.1. Comparing Experiences of Persons with Lived Experience with Those with Clinical Perspectives and Priorities
4.2. Educational Workshop Feedback
4.3. Next Steps and Project Recommendations
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Health Topics of Interest | |
|---|---|
| Activity-Based Therapy | Peer Support/Mentorship |
| Aging with SCI | Pressure Injuries |
| Autonomic Dysreflexia | Recreational Options |
| Bladder Function | Respiratory Health |
| Bowel Function | Seating and Positioning |
| Cardiovascular Health | Sexual Health |
| Diabetes/Diet | Social Assistance Programs |
| Epidural and Transcutaneous Spinal Cord Stimulation | Spasticity |
| Equipment | Sport Performance/Paralympics |
| Exercise, Standing, and Walking | Upper Extremity Function |
| Mental Health | Vehicle Modifications and Transportation |
| Nerve and Tendon Transfer | Wheelchair Accessible Housing |
| Pain and Inflammation | |
References
- Noonan, V.K.; Fingas, M.; Farry, A.; Baxter, D.; Singh, A.; Fehlings, M.G.; Dvorak, M.F. Incidence and prevalence of spinal cord injury in Canada: A national perspective. Neuroepidemiology 2012, 38, 219–226. [Google Scholar] [CrossRef]
- Ronca, E.; Scheel-Sailer, A.; Koch, H.G.; Gemperli, A. Health care utilization in persons with spinal cord injury: Part 2—Determinants, geographic variation and comparison with the general population. Spinal Cord 2017, 55, 828–833. [Google Scholar] [CrossRef]
- Ding, W.; Hu, S.; Wang, P.; Kang, H.; Peng, R.; Dong, Y.; Li, F. Spinal cord injury: The global incidence, prevalence, and disability rrom the Global Burden of Disease Study 2019. Spine 2022, 47, 1532. [Google Scholar] [CrossRef] [PubMed]
- Ronca, E.; Scheel-Sailer, A.; Koch, H.G.; Essig, S.; Brach, M.; Münzel, N.; Gemperli, A. Satisfaction with access and quality of healthcare services for people with spinal cord injury living in the community. J. Spinal Cord Med. 2020, 43, 111–121. [Google Scholar] [CrossRef]
- Ronca, E.; Brunkert, T.; Koch, H.G.; Jordan, X.; Gemperli, A. Residential location of people with chronic spinal cord injury: The importance of local health care infrastructure. BMC Health Serv. Res. 2018, 18, 657. [Google Scholar] [CrossRef] [PubMed]
- Glennie, R.A.; Batke, J.; Fallah, N.; Cheng, C.L.; Rivers, C.S.; Noonan, V.K.; Dvorak, M.F.; Fisher, C.G.; Kwon, B.K.; Street, J.T. Rural and urban living in persons with spinal cord injury and comparing environmental barriers, their health, and quality-of-life outcomes. J. Neurotrauma 2017, 34, 2877–2882. [Google Scholar] [CrossRef]
- Goodridge, D.; Rogers, M.; Klassen, L.; Jeffery, B.; Knox, K.; Rohatinsky, N.; Linassi, G. Access to health and support services: Perspectives of people living with a long-term traumatic spinal cord injury in rural and urban areas. Disabil. Rehabil. 2015, 37, 1401–1410. [Google Scholar] [CrossRef] [PubMed]
- Pilusa, S.; Myezwa, H.; Potterton, J. Views of health care users and providers: Solutions to improve the prevention of secondary health conditions among people with spinal cord injury, South Africa. Spinal Cord Ser. Cases 2022, 8, 67. [Google Scholar] [CrossRef]
- Roots, R.; Brown, H.; Bainbridge, L.; Li, L. Rural rehabilitation practice: Perspectives of occupational therapists and physical therapists in British Columbia, Canada. Rural Remote Health 2014, 14, 2506. [Google Scholar] [CrossRef]
- Johnston, K.N.; Young, M.; Kay, D.; Booth, S.; Spathis, A.; Williams, M.T. Attitude change and increased confidence with management of chronic breathlessness following a health professional training workshop: A survey evaluation. BMC Med. Educ. 2020, 20, 90. [Google Scholar] [CrossRef]
- Mickan, S.; Hilder, J.; Wenke, R.; Thomas, R. The impact of a small-group educational intervention for allied health professionals to enhance evidence-based practice: Mixed methods evaluation. BMC Med. Educ. 2019, 19, 131. [Google Scholar] [CrossRef] [PubMed]
- Schoen, D.E.; Gausia, K.; Glance, D.G.; Thompson, S.C. Improving rural and remote practitioners’ knowledge of the diabetic foot: Findings from an educational intervention. J. Foot Ankle Res. 2016, 9, 26. [Google Scholar] [CrossRef] [PubMed]
- Smekal, M.D.; Bello, A.K.; Donald, M.; Zaidi, D.; McBrien, K.; Nicholson, K.; Novak, E.; Hemmelgarn, B. Enhancing primary care capacity in chronic kidney disease management: A quality improvement educational initiative. BMJ Open 2021, 11, e046068. [Google Scholar] [CrossRef]
- Miller, D.M.; Neelon, L.; Kish-Smith, K.; Whitney, L.; Burant, C.J. Pressure injury knowledge in critical care nurses. J. Wound Ostomy Cont. Nurs. 2017, 44, 455. [Google Scholar] [CrossRef]
- Hitzig, S.L.; Hunter, J.P.; Ballantyne, E.C.; Katz, J.; Rapson, L.; Craven, B.C.; Boschen, K.A. Outcomes and reflections on a consensus-building workshop for developing a spinal cord injury-related chronic pain research agenda. J. Spinal Cord Med. 2017, 40, 258–267. [Google Scholar] [CrossRef]
- Baehr, L.A.; Fisher, K.; Finley, M. Perspectives on health with spinal cord injury now and in the future: A qualitative descriptive study. Phys. Ther. 2023, 103, pzad011. [Google Scholar] [CrossRef]
- Melin, J.; Axwalter, E.; Åhrén, G.; Sunnerhagen, K.S.; Lundgren-Nilsson, Å.; Wangdell, J. Research priorities to enhance life for people with spinal cord injury: A Swedish priority setting partnership. Spinal Cord 2023, 61, 570–577. [Google Scholar] [CrossRef] [PubMed]
- Huh, S.; Ko, H.-Y. Recovery target priorities of people with spinal cord injuries in Korea compared with other countries: A survey. Spinal Cord 2020, 58, 998–1003. [Google Scholar] [CrossRef] [PubMed]
- Lam, C.Y.; Koljonen, P.A.; Yip, C.C.H.; Su, I.Y.W.; Hu, Y.; Wong, Y.W.; Cheung, K.M.C. Functional recovery priorities and community rehabilitation service preferences of spinal cord injury individuals and caregivers of Chinese ethnicity and cultural background. Front. Neurol. 2022, 13, 941256. [Google Scholar] [CrossRef]
- French, J.S.; Anderson-Erisman, K.D.; Sutter, M. What do spinal cord injury consumers want? A review of spinal cord injury consumer priorities and neuroprosthesis from the 2008 neural interfaces conference. Neuromodul. J. Int. Neuromodul. Soc. 2010, 13, 229–231. [Google Scholar] [CrossRef]
- Lo, C.; Tran, Y.; Anderson, K.; Craig, A.; Middleton, J. Functional priorities in persons with spinal cord injury: Using discrete choice experiments to determine preferences. J. Neurotrauma 2016, 33, 1958–1968. [Google Scholar] [CrossRef]
- Simpson, L.A.; Eng, J.J.; Hsieh, J.T.C.; Dalton L. Wolfe and the Spinal Cord Injury Rehabilitation Evidence (SCIRE) Research Team. The health and life priorities of individuals with spinal cord injury: A Systematic Review. J. Neurotrauma 2012, 29, 1548–1555. [Google Scholar] [CrossRef] [PubMed]
- Pryor, J.; Haylen, D.; Fisher, M. Problems people with spinal cord injury experience accessing help with bowel care when hospitalised outside a specialist spinal injury service. J. Clin. Nurs. 2021, 30, 1633–1644. [Google Scholar] [CrossRef] [PubMed]
- Potharaju, K.A.; Fields, J.D.; Cemballi, A.G.; Pantell, M.S.; Desai, R.; Akom, A.; Shah, A.; Cruz, T.; Nguyen, K.H.; Lyles, C.R. Assessing alignment of patient and clinician perspectives on community health resources for chronic disease management. Healthcare 2022, 10, 2006. [Google Scholar] [CrossRef]
- Crowe, S.; Fenton, M.; Hall, M.; Cowan, K.; Chalmers, I. Patients’, clinicians’ and the research communities’ priorities for treatment research: There is an important mismatch. Res. Involv. Engagem. 2015, 1, 2. [Google Scholar] [CrossRef] [PubMed]
- Anderson, K.D. Equitable partnerships between scientists and persons living with spinal cord injury will strengthen research scope, quality, and outcomes. Curr. Opin. Neurol. 2021, 34, 783–788. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, P.; Kable, A.; Levett-Jones, T. The effectiveness of internet-based e-learning on clinician behavior and patient outcomes: A systematic review protocol. JBI Evid. Synth. 2015, 13, 52. [Google Scholar] [CrossRef] [PubMed]
- McWilliams, T.; Hendricks, J.; Twigg, D.; Wood, F. Burns education for non-burn specialist clinicians in Western Australia. Burn. J. Int. Soc. Burn Inj. 2015, 41, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Orr, L.; Houghton, P.; Holyoke, P.; Lala, D. A quasi-experimental evaluation of an education program for the use of electrical stimulation therapy to heal pressure injuries. Wound Manag. Prev. 2020, 66, 14–23. [Google Scholar] [CrossRef]
- Kim, S.; Bayer, I.; Gewurtz, R.; Larivière, N.; Letts, L. Comparing web-based and in-person educational workshops for Canadian occupational therapists and understanding their learning experiences: Mixed methods study. JMIR Med. Educ. 2022, 8, e31634. [Google Scholar] [CrossRef]
- Martinengo, L.; Yeo, N.J.Y.; Markandran, K.D.; Olsson, M.; Kyaw, B.M.; Car, L.T. Digital health professions education on chronic wound management: A systematic review. Int. J. Nurs. Stud. 2020, 104, 103512. [Google Scholar] [CrossRef] [PubMed]
- Sargeant, J.; Curran, V.; Jarvis-Selinger, S.; Ferrier, S.; Allen, M.; Kirby, F.; Ho, K. Interactive online continuing medical education: Physicians’ perceptions and experiences. J. Contin. Educ. Health Prof. 2004, 24, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Engaging People with Spinal Cord Injury. Praxis Spinal Cord Institute. Available online: https://praxisinstitute.org/living-with-sci/plex-team/ (accessed on 18 November 2023).
- Ørtenblad, L.; Maribo, T.; Quistgaard, B.; Madsen, E.; Handberg, C. Goal-Setting in clinical practice: A study of healthcare professionals’ perspectives in outpatient multidisciplinary rehabilitation of patients with spinal cord injury. Disabil. Rehabil. 2023, 45, 3330–3341. [Google Scholar] [CrossRef] [PubMed]
- Wheeler, T.L.; de Groat, W.; Eisner, K.; Emmanuel, A.; French, J.; Grill, W.; Kennelly, M.J.; Krassioukov, A.; Santacruz, B.G.; Biering-Sørensen, F.; et al. Translating promising strategies for bowel and bladder management in spinal cord injury. Exp. Neurol. 2018, 306, 169–176. [Google Scholar] [CrossRef]
- October, T.W.; Dizon, Z.B.; Hamilton, M.F.; Madrigal, V.N.; Arnold, R.M. Communication training for inter-specialty clinicians. Clin. Teach. 2019, 16, 242–247. [Google Scholar] [CrossRef]
| Workshop Title | Description |
|---|---|
| SCI 101 | This session was a high-level presentation geared for clinicians to enhance their knowledge of SCI, specific needs, and a variety of SCI topics to improve confidence when working with people with SCI. Information shared and issues discussed include the following: Canadian SCI Registry, best practices, common terminology for types/levels of injury, statistics, Canadian SCI Care pathway, effects of SCI on body systems beyond motor paralysis, International Standards for the Neurological Classification of SCI (ISNCSCI) Assessment overview, secondary health conditions, pressure injuries, neuropathic pain, autonomic dysreflexia, bladder/bowel function, respiratory health, sexual health, clinical care considerations, psychosocial adjustments to SCI, peer support, adaptive travel considerations, recreation opportunities, and sharing of resources. |
| Pressure Injuries | This session was focused on pressure injuries and was supported by PLEX personal stories and a presentation for SCI clinicians to enhance their knowledge of pressure injuries related to SCI and prevention techniques. Information shared included defining pressure injuries, stages, understanding their significance, statistics, costs of prevention, prevention methods/equipment, and many other resources. There was also time for Q&A discussions and PLEX sharing the personal impacts and their experiences related to pressure injuries. |
| PLEX Panel | A panel of 4–5 individuals with lived experience of SCI shared their journeys from the early days post-injury to transitioning to living in the community. Discussion topics varied from who was sharing and the questions asked by attendees and clinicians. PLEX panels also often included both men and women with a variety of injury types, levels of injury, paraplegics and tetraplegics, as well as new and experienced PLEX (from 6 months to 40 years post-SCI). |
| Question Number | Description |
|---|---|
| 1 | How familiar and confident would you consider yourself with the following topics related to SCI: autonomic dysreflexia, bladder/bowel management, pain management, pressure injury, psychosocial, recreational/peer opportunities, respiratory health, sexual health, spasticity? (note: each SCI topics are rated) |
| 2 | How useful did you find the session? |
| 3 | What messages from the discussion did you find helpful? |
| 4 | How will this session influence your future clinical practice? |
| 5 | As a clinician, what would you identify as potential gaps in service implementation for individuals living with SCI in your region? |
| 6 | For future workshops, what SCI-related topics would you like to learn more about, and which would be of most interest to your clinical practice? |
| SCI Topic | PLEX Perspective (n = 44) | Clinical Perspective (n = 102) | ||
|---|---|---|---|---|
| N (%) | Rank | N (%) | Rank | |
| Activity-Based Therapy | 5 (11.4) | t-14 | NA | |
| Aging With SCI | 20 (45.5) | 1 | NA | |
| Autonomic Dysreflexia | 2 (4.5) | 23 | 61 (59.8) | 3 |
| Bladder Function/Management | 11 (25.0) | t-5 | 37 (36.3) | 13 |
| Bowel Function/Management | 13 (29.5) | 2 | 36 (35.3) | 14 |
| Cardiovascular Health | 6 (13.6) | t-9 | NA | |
| Diabetes/Diet | 6 (13.6) | t-9 | NA | |
| Epidural and Transcutaneous Spinal Cord Stimulation | 6 (13.6) | t-9 | NA | |
| Equipment | 11 (25.0) | t-5 | NA | |
| Exercise, Standing, and Walking | 5 (11.4) | t-14 | 54 (52.9) | 8 |
| Mental Health | 5 (11.4) | t-14 | 45 (44.1) | 10 |
| Nerve and Tendon Transfer | 5 (11.4) | t-14 | NA | |
| Pain and Inflammation | 12 (27.3) | t-3 | 60 (58.8) | 4 |
| Peer Support/Mentorship | 1 (2.3) | t-24 | 48 (47.1) | 9 |
| Pressure Injuries | 6 (13.6) | t-9 | 39 (38.2) | 11 |
| Recreational Options | 3 (6.8) | t-20 | 59 (57.8) | 5 |
| Research Initiatives | NA | 50 (49.0) | ||
| Respiratory Health | 3 (6.8) | t-20 | 56 (54.9) | t-6 |
| Seating and Positioning (Wheelchair Mobility) | 4 (9.1) | 19 | 56 (54.9) | t-6 |
| Sexual Health | 10 (22.7) | 7 | 39 (38.2) | t-11 |
| Social Assistance Programs | 5 (11.4) | t-14 | NA | |
| Spasticity | 12 (27.3) | t-3 | 78 (76.5) | 1 |
| Sport Performance/Paralympics | 3 (6.8) | t-20 | NA | |
| Upper Extremity Function | 9 (20.5) | 8 | 70 (68.6) | 2 |
| Vehicle Modifications and Transportation | 1 (2.3) | t-24 | NA | |
| Wheelchair Accessible Housing | 6 (13.6) | t-9 | NA | |
| Main Theme (n = Frequency) | Quote Examples/Excerpts |
|---|---|
| Benefits of lived experience (n = 14) | “The personal experience was especially eye-opening.” “Hearing real stories. Sometimes, it is easier to remember important things if they are delivered via experience. I had no idea that bowel care/continence is so much of a big deal, if not hearing it first-hand.” |
| Learning about the secondary impacts of SCI (n = 7) | “It was also great to hear about the other aspects of what people with SCI deal with on a daily basis that we may not necessarily always think about.” “It makes us consider what other things we need to consider prior to discharge.” “So very moving. It’s easy to forget the ‘unseen’ injury that happens to the loved ones of our patients. This really helped to remind me of that, and what an incredible job the informal caregivers do in so many patients lives.” |
| Needs for resources (n = 7) | “How do I quickly and easily access expert advice when I have a patient with SCI.” “More funding options for equipment.” |
| Recommendations for future workshops (n = 5) | “Really enjoyed the session and wanted it to go on longer. Could be 2 or 2.5 h next time.” “It would be nice to write down a couple of the questions there were unable to be answered and address them on following sessions for 5–10 min.” “I wish I could have had a “Where are they now.” |
| Education is key (n = 5) | “How do we help educate and positively impact clients who have limited funding and decreased engagement in their wellness goals.” “Information given was actionable as well as informative.” |
| Require more clinical information (n = 3) | “I would just encourage the panel to keep it more clinical focused as best they can.” |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prins, H.; Donia, S.; Rockall, S.; Hektner, J.; Hawes, S.; Laskin, J.J.; Chernesky, J.; Noonan, V.K. Implementing Lived Experience Workshops in Regional Areas of British Columbia to Enhance Clinicians’ Confidence in Spinal Cord Injury Care: An Evaluation. Healthcare 2024, 12, 731. https://doi.org/10.3390/healthcare12070731
Prins H, Donia S, Rockall S, Hektner J, Hawes S, Laskin JJ, Chernesky J, Noonan VK. Implementing Lived Experience Workshops in Regional Areas of British Columbia to Enhance Clinicians’ Confidence in Spinal Cord Injury Care: An Evaluation. Healthcare. 2024; 12(7):731. https://doi.org/10.3390/healthcare12070731
Chicago/Turabian StylePrins, Hannah, Scott Donia, Shannon Rockall, James Hektner, Spring Hawes, James J. Laskin, John Chernesky, and Vanessa K. Noonan. 2024. "Implementing Lived Experience Workshops in Regional Areas of British Columbia to Enhance Clinicians’ Confidence in Spinal Cord Injury Care: An Evaluation" Healthcare 12, no. 7: 731. https://doi.org/10.3390/healthcare12070731
APA StylePrins, H., Donia, S., Rockall, S., Hektner, J., Hawes, S., Laskin, J. J., Chernesky, J., & Noonan, V. K. (2024). Implementing Lived Experience Workshops in Regional Areas of British Columbia to Enhance Clinicians’ Confidence in Spinal Cord Injury Care: An Evaluation. Healthcare, 12(7), 731. https://doi.org/10.3390/healthcare12070731






