Relationships between the Structural Characteristics of General Medical Practices and the Socioeconomic Status of Patients with Diabetes-Related Performance Indicators in Primary Care
Abstract
1. Introduction
2. Materials and Methods
2.1. Settings
2.2. Explanatory Variables
2.3. Outcome Variables: DM Care Quality Indicators
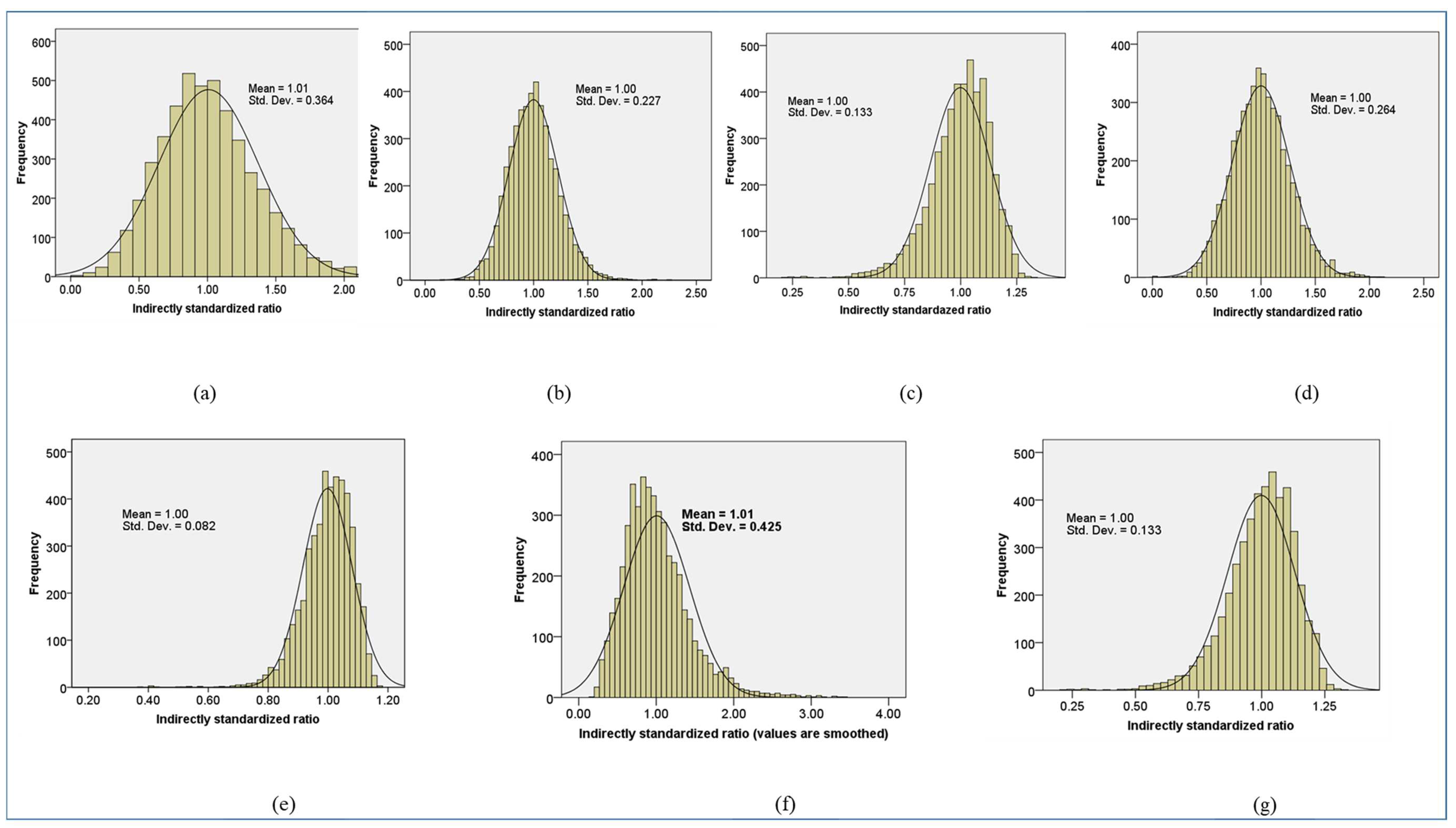
2.4. Statistical Analysis
3. Results
3.1. Descriptive Statistics
3.2. Linear Regression Modeling
4. Discussion
4.1. Main Findings
4.2. Strengths and Limitations
4.3. Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| 95% CI | 95% Confidence Interval |
| DM | Diabetes Mellitus |
| EUBIROD | The European Best Information through Regional Outcomes in Diabetes |
| GMP | General Medical Practice |
| GP | General Practitioner |
| ISR | Indirectly Standardized Ratio |
| NHIF | National Health Insurance Fund |
| NHS | National Health Service |
| NICE | The National Institute for Health and Care Excellence |
| nISR | Normalized Empirical Bayes-adjusted Indirectly Standardized Ratio |
| P4P | Pay for Performance |
| QOF | Quality and Outcomes Framework |
| rHD | Relative Housing Density |
| rRP | Relative Roma Proportion |
| SES | Socioeconomic status |
| srEDU | Standardized Relative Education |
| srEMP | Standardized Relative Employment |
| SD | Standard Deviation |
| β | Linear Regression Coefficient |
Appendix A
| HemoglobinA1c Testing | Ophthalmological Examination | Prevalence of DM Patients Aged 40–54 | Prevalence of DM Patients Aged 55–69 | Serum Creatinine Determination | Influenza Vaccination | Lipid Status Testing | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Received Care | Target Group | Received Care | Target Group | Received Care | Target Group | Received Care | Target Group | Received Care | Target Group | Received Care | Target Group | Received Care | Target Group | |
| 32.907 | 39.155 | 18.559 | 39.155 | 6.837 | 160.22 | 19.455 | 132.26 | 35.065 | 39.155 | 4.815 | 18.552 | 32.907 | 39.155 | |
| 18–19 years | 375 | 424 | 133 | 424 | 377 | 424 | 21 | 424 | 375 | 424 | ||||
| 20–24 years | 1708 | 2021 | 597 | 2021 | 1737 | 2021 | 81 | 2021 | 1708 | 2021 | ||||
| 25–29 years | 2283 | 2839 | 839 | 2839 | 2394 | 2839 | 132 | 2839 | 2283 | 2839 | ||||
| 30–34 years | 3139 | 4018 | 1170 | 4018 | 3373 | 4018 | 210 | 4018 | 3139 | 4018 | ||||
| 35–39 years | 5461 | 6968 | 2001 | 6968 | 5846 | 6968 | 424 | 6968 | 5461 | 6968 | ||||
| 40–44 years | 11,033 | 13,969 | 4279 | 13,969 | 13,969 | 794,746 | 11,726 | 13,969 | 928 | 13,970 | 11,142 | 13,969 | ||
| 45–49 years | 17,044 | 21,343 | 6716 | 21,343 | 21,343 | 664,755 | 18,065 | 21,343 | 1614 | 21,342 | 17,231 | 21,343 | ||
| 50–54 years | 26,119 | 32,630 | 10,758 | 32,630 | 32,630 | 583,072 | 27,723 | 32,630 | 3092 | 32,630 | 26,119 | 32,630 | ||
| 55–59 years | 39,932 | 49,370 | 17,400 | 49,370 | 49,370 | 548,390 | 42,727 | 49,370 | 6187 | 49,370 | 39,933 | 49,370 | ||
| 60–64 years | 67,835 | 84,683 | 31,705 | 84,683 | 84,683 | 667,123 | 73,341 | 84,683 | 15,442 | 84,682 | 67,835 | 84,683 | ||
| 65–69 years | 73,687 | 91,763 | 38,054 | 91,763 | 91,763 | 570,001 | 80,409 | 91,763 | 73,687 | 91,763 | ||||
| 70–74 years | 64,054 | 80,775 | 35,188 | 80,775 | 71,236 | 80,775 | 64,054 | 80,775 | ||||||
| 75–79 years | 48,889 | 64,265 | 27,069 | 64,265 | 55,853 | 64,265 | 48,889 | 64,265 | ||||||
| 80–84 years | 27,292 | 38,619 | 14,054 | 38,619 | 32,471 | 38,619 | 27,292 | 38,619 | ||||||
| 85–89 years | 11,213 | 17,455 | 5210 | 17,455 | 17,437 | 22,365 | 13,932 | 22,365 | ||||||
| >90 years | 2719 | 4910 | 1105 | 4910 | ||||||||||
| female | 210,188 | 271,463 | 106,910 | 271,463 | 27,419 | 1,018,978 | 108,533 | 977,814 | 234,150 | 271,463 | 12,544 | 97,176 | 210,189 | 271,463 |
| male | 192,595 | 244,589 | 89,368 | 244,589 | 40,523 | 1,023,595 | 117,283 | 807,700 | 210,565 | 244,589 | 15,587 | 121,088 | 192,595 | 244,589 |
| exemption certificate (+) | 369,225 | 472,988 | 179,898 | 472,988 | 60,763 | 2,001,258 | 205,813 | 1,705,497 | 406,802 | 472,988 | 23,914 | 194,946 | 369,226 | 472,988 |
| exemption certificate (−) | 33,558 | 43,064 | 16,380 | 43,064 | 7179 | 41,315 | 20,003 | 80,017 | 37,913 | 43,064 | 4217 | 23,318 | 33,558 | 43,064 |
| total | 402,783 | 516,052 | 196,278 | 516,052 | 67,942 | 2,042,573 | 225,816 | 1,785,514 | 444,715 | 516,052 | 28,131 | 218,264 | 402,784 | 516,052 |
| crude indicator | 78.05% | 38.03% | 3.33% | 12.65% | 86.18% | 12.89% | 78.05% | |||||||
| HemoglobinA1c Testing | Ophthalmological Examination | Serum Lipid Status Checking | Serum Creatinine Determination | Influenza Vaccination | Prevalence of DM Aged 40–54 | Prevalence of DM Aged 55–69 | |
|---|---|---|---|---|---|---|---|
| Baranya/Budapest | 0.046 [0.020; 0.073] | −0.068 [−0.117; −0.018] | 0.046 [0.020; 0.073] | 0.027 [0.011; 0.044] | 0.091 [0.003; 0.178] | −0.040 [−0.111; 0.032] | −0.014 [−0.059; 0.031] |
| Bács-Kiskun/Budapest | 0.051 [0.025; 0.077] | −0.184 [−0.233; −0.135] | 0.051 [0.025; 0.077] | 0.026 [0.010; 0.042] | 0.002 [−0.085; 0.088] | −0.070 [−0.140; 0] | −0.079 [−0.123; −0.035] |
| Békés/Budapest | 0.004 [−0.025; 0.034] | −0.204 [−0.259; −0.148] | 0.005 [−0.025; 0.034] | −0.010 [−0.028; 0.008] | −0.097 [−0.195; 0.001] | −0.080 [−0.160; 0] | −0.067 [−0.117; −0.017] |
| Borsod-Abaúj-Zemplén/Budapest | 0.026 [0; 0.052] | −0.119 [−0.168; −0.071] | 0.026 [0; 0.052] | −0.015 [−0.031; 0.002] | −0.058 [−0.145; 0.029] | −0.131 [−0.201; −0.060] | −0.149 [−0.193; −0.104] |
| Csongrád/Budapest | 0.044 [0.015; 0.072] | −0.067 [−0.121; −0.013] | 0.044 [0.015; 0.073] | 0.012 [−0.006; 0.03] | −0.058 [−0.154; 0.038] | −0.154 [−0.231; −0.076] | −0.152 [−0.201; −0.103] |
| Fejér/Budapest | 0.016 [−0.012; 0.043] | −0.139 [−0.191; −0.087] | 0.016 [−0.012; 0.044] | −0.001 [−0.018; 0.017] | −0.052 [−0.144; 0.040] | −0.043 [−0.117; 0.032] | −0.040 [−0.087; 0.007] |
| Győr-Moson-Sopron/Budapest | 0.024 [−0.003; 0.05] | −0.319 [−0.370; −0.269] | 0.024 [−0.003; 0.051] | −0.011 [−0.028; 0.005] | −0.188 [−0.278; −0.099] | −0.023 [−0.096; 0.05] | 0.015 [−0.031; 0.061] |
| Hajdú-Bihar/Budapest | 0.07 [0.042; 0.098] | −0.025 [−0.078; 0.028] | 0.070 [0.042; 0.098] | 0.018 [0; 0.035] | −0.123 [−0.217; −0.029] | −0.084 [−0.160; −0.007] | −0.095 [−0.143; −0.047] |
| Heves/Budapest | −0.010 [−0.038; 0.018] | −0.362 [−0.414; −0.309] | −0.010 [−0.038; 0.018] | −0.023 [−0.041; −0.006] | −0.026 [−0.119; 0.067] | −0.094 [−0.169; −0.018] | −0.097 [−0.144; −0.049] |
| Komárom-Esztergom/Budapest | −0.052 [−0.081; −0.023] | −0.273 [−0.327; −0.219] | −0.052 [−0.080; −0.023] | −0.035 [−0.053; −0.017] | −0.051 [−0.147; 0.045] | −0.144 [−0.222; −0.066] | −0.043 [−0.092; 0.006] |
| Nógrád/Budapest | −0.069 [−0.103; −0.036] | −0.265 [−0.328; −0.203] | −0.069 [−0.103; −0.036] | −0.031 [−0.051; −0.010] | −0.003 [−0.114; 0.108] | −0.205 [−0.296; −0.115] | −0.183 [−0.240; −0.126] |
| Pest/Budapest | −0.003 [−0.026; 0.021] | −0.156 [−0.201; −0.112] | −0.002 [−0.026; 0.021] | −0.009 [−0.024; 0.006] | −0.065 [−0.144; 0.014] | −0.045 [−0.11; 0.019] | 0.003 [−0.037; 0.043] |
| Somogy/Budapest | −0.003 [−0.031; 0.025] | −0.203 [−0.255; −0.150] | −0.003 [−0.031; 0.026] | −0.012 [−0.03; 0.005] | 0.188 [0.095; 0.282] | 0.018 [−0.059; 0.094] | 0.014 [−0.034; 0.062] |
| Szabolcs-Szatmár-Bereg/Budapest | 0.064 [0.037; 0.091] | −0.155 [−0.206; −0.105] | 0.064 [0.037; 0.091] | 0.031 [0.014; 0.047] | −0.093 [−0.182; −0.003] | −0.090 [−0.163; −0.017] | −0.083 [−0.129; −0.037] |
| Jász-Nagykun-Szolnok/Budapest | 0.030 [0.002; 0.058] | −0.254 [−0.306; −0.203] | 0.031 [0.003; 0.058] | −0.008 [−0.025; 0.010] | −0.113 [−0.205; −0.021] | −0.046 [−0.121; 0.029] | −0.073 [−0.120; −0.026] |
| Tolna/Budapest | −0.055 [−0.085; −0.025] | −0.164 [−0.220; −0.107] | −0.054 [−0.084; −0.024] | 0.025 [0.006; 0.044] | 0.148 [0.048; 0.248] | 0.037 [−0.045; 0.118] | 0.043 [−0.008; 0.094] |
| Vas/Budapest | 0.068 [0.039; 0.097] | −0.122 [−0.176; −0.067] | 0.068 [0.039; 0.098] | 0.036 [0.018; 0.054] | −0.136 [−0.233; −0.039] | −0.032 [−0.111; 0.047] | 0.008 [−0.041; 0.057] |
| Veszprém/Budapest | 0 [−0.028; 0.027] | −0.168 [−0.220; −0.116] | 0 [−0.028; 0.028] | −0.001 [−0.018; 0.017] | 0.004 [−0.089; 0.096] | −0.107 [−0.183; −0.032] | −0.062 [−0.110; −0.015] |
| Zala/Budapest | 0.015 [−0.013; 0.043] | −0.167 [−0.219; −0.114] | 0.015 [−0.012; 0.043] | 0.009 [−0.009; 0.026] | 0.110 [0.017; 0.202] | −0.144 [−0.219; −0.069] | −0.094 [−0.142; −0.047] |
| GMP type (adult/mixed) | 0.020 [0.006; 0.034] | 0.010 [−0.016; 0.036] | 0.020 [0.006; 0.034] | 0.015 [0.006; 0.024] | −0.052 [−0.099; −0.006] | −0.019 [−0.057; 0.018] | 0.011 [−0.013; 0.035] |
| Settlement type (urban/rural) | 0.017 [0.003; 0.03] | 0.027 [0.001; 0.052] | 0.017 [0.003; 0.030] | 0.013 [0.005; 0.022] | −0.006 [−0.052; 0.040] | −0.045 [−0.082; −0.007] | −0.034 [−0.058; −0.011] |
| GP (vacancy/age < 65) | 0 [−0.021; 0.021] | 0.018 [−0.020; 0.057] | 0 [−0.021; 0.021] | 0.006 [−0.007; 0.019] | −0.119 [−0.188; −0.051] | 0.023 [−0.033; 0.079] | −0.001 [−0.036; 0.034] |
| GP (age ≥ 65X/age < 65) | −0.027 [−0.036; −0.018] | −0.016 [−0.033; 0] | −0.027 [−0.036; −0.018] | −0.017 [−0.023; −0.012] | −0.033 [−0.062; −0.003] | −0.032 [−0.056; −0.008] | −0.028 [−0.043; −0.013] |
| List size (≤800/1201–1600) | −0.007 [−0.029; 0.016] | −0.055 [−0.097; −0.014] | −0.006 [−0.029; 0.016] | −0.003 [−0.017; 0.010] | 0.023 [−0.051; 0.096] | −0.036 [−0.096; 0.024] | −0.022 [−0.06; 0.015] |
| List size (801–1200/1201–1600) | −0.007 [−0.019; 0.004] | −0.001 [−0.022; 0.021] | −0.007 [−0.019; 0.004] | −0.004 [−0.011; 0.003] | 0.004 [−0.035; 0.043] | −0.022 [−0.054; 0.009] | −0.010 [−0.030; 0.010] |
| List size (1601–2000/1201–1600) | −0.005 [−0.014; 0.004] | −0.018 [−0.035; −0.001] | −0.005 [−0.014; 0.004] | 0 [−0.006; 0.005] | −0.015 [−0.045; 0.015] | 0.011 [−0.013; 0.036] | 0.008 [−0.008; 0.023] |
| List size (>2000/1201–1600) | −0.023 [−0.033; −0.012] | −0.021 [−0.041; −0.001] | −0.023 [−0.033; −0.012] | −0.011 [−0.018; −0.004] | −0.043 [−0.078; −0.007] | 0.003 [−0.026; 0.032] | 0.004 [−0.015; 0.022] |
| Level of education (low/medium) | −0.030 [−0.043; −0.018] | −0.056 [−0.080; −0.032] | −0.031 [−0.043; −0.018] | −0.018 [−0.026; −0.010] | −0.004 [−0.046; 0.038] | 0.037 [0.003; 0.072] | 0.009 [−0.013; 0.030] |
| Level of education (high/medium) | 0.013 [0.001; 0.026] | 0.020 [−0.004; 0.044] | 0.013 [0.001; 0.026] | 0.006 [−0.002; 0.014] | 0.035 [−0.008; 0.078] | −0.136 [−0.171; −0.101] | −0.067 [−0.088; −0.045] |
| Employment ratio (low/medium) | −0.005 [−0.018; 0.008] | −0.010 [−0.034; 0.014] | −0.005 [−0.018; 0.008] | −0.002 [−0.011; 0.006] | 0.050 [0.007; 0.094] | 0.039 [0.004; 0.075] | 0.029 [0.007; 0.051] |
| Employment ratio (high/medium) | 0.001 [−0.013; 0.014] | 0.016 [−0.009; 0.042] | 0.001 [−0.013; 0.014] | −0.004 [−0.012; 0.004] | 0.008 [−0.037; 0.053] | −0.052 [−0.088; −0.015] | −0.053 [−0.076; −0.03] |
| Housing density (low/medium) | 0.012 [−0.001; 0.024] | −0.048 [−0.072; −0.025] | 0.012 [−0.001; 0.024] | 0.003 [−0.004; 0.011] | 0 [−0.042; 0.041] | −0.044 [−0.078; −0.010] | −0.024 [−0.045; −0.003] |
| Housing density (high/medium) | −0.002 [−0.013; 0.009] | −0.021 [−0.041; −0.001] | −0.002 [−0.013; 0.009] | −0.002 [−0.009; 0.004] | 0 [−0.036; 0.036] | 0.037 [0.008; 0.066] | 0.023 [0.004; 0.041] |
| Proportion Roma (low/medium) | −0.003 [−0.016; 0.009] | 0.008 [−0.015; 0.031] | −0.003 [−0.016; 0.009] | 0.003 [−0.005; 0.01] | 0.047 [0.006; 0.087] | −0.031 [−0.065; 0.002] | 0.007 [−0.014; 0.028] |
| Proportion Roma (high/medium) | −0.004 [−0.017; 0.009] | −0.013 [−0.037; 0.012] | −0.004 [−0.017; 0.009] | 0.002 [−0.006; 0.011] | −0.028 [−0.071; 0.016] | 0.013 [−0.023; 0.048] | 0.019 [−0.004; 0.041] |
| HemoglobinA1c Testing | Ophthalmological Examination | Serum Lipid Status Checking | Serum Creatinine Determination | Influenza Vaccination | Prevalence of DM Aged 40–54 | Prevalence of DM Aged 55–69 | |
|---|---|---|---|---|---|---|---|
| Explanatory power of the model (r2) | 0.114 | 0.210 | 0.113 | 0.105 | 0.039 | 0.130 | 0.119 |
| Baranya/Budapest | 0.071 [0.030; 0.111] | −0.052 [−0.090; −0.014] | 0.071 [0.031; 0.111] | 0.068 [0.027; 0.108] | 0.044 [0.002; 0.085] | −0.022 [−0.062; 0.018] | −0.012 [−0.053; 0.028] |
| Bács-Kiskun/Budapest | 0.086 [0.042; 0.130] | −0.157 [−0.199; −0.116] | 0.086 [0.042; 0.130] | 0.071 [0.027; 0.116] | 0.001 [−0.045; 0.047] | −0.043 [−0.087; 0.000] | −0.078 [−0.122; −0.035] |
| Békés/Budapest | 0.006 [−0.037; 0.049] | −0.150 [−0.190; −0.109] | 0.007 [−0.036; 0.050] | −0.024 [−0.067; 0.019] | −0.044 [−0.089; 0.000] | −0.043 [−0.085; 0.000] | −0.057 [−0.100; −0.014] |
| Borsod-Abaúj-Zemplén/Budapest | 0.052 [−0.001; 0.104] | −0.121 [−0.171; −0.072] | 0.053 [0.000; 0.105] | −0.047 [−0.100; 0.005] | −0.036 [−0.091; 0.018] | −0.096 [−0.148; 0.044] | −0.176 [−0.228; −0.123] |
| Csongrád/Budapest | 0.066 [0.023; 0.110] | −0.051 [−0.093; −0.010] | 0.067 [0.023; 0.111] | 0.029 [−0.015; 0.073] | −0.028 [−0.073; 0.018] | −0.085 [−0.129; −0.042] | −0.136 [−0.180; −0.092] |
| Fejér/Budapest | 0.023 [−0.018; 0.064] | −0.104 [−0.143; −0.065] | 0.024 [−0.017; 0.065] | −0.001 [−0.043; 0.040] | −0.024 [−0.067; 0.018] | −0.023 [−0.064; 0.017] | −0.035 [−0.075; 0.006] |
| Győr-Moson-Sopron/Budapest | 0.036 [−0.005; 0.076] | −0.244 [−0.282; −0.205] | 0.036 [−0.005; 0.077] | −0.028 [−0.069; 0.013] | −0.089 [−0.132; −0.047] | −0.013 [−0.053; 0.028] | 0.013 [−0.028; 0.054] |
| Hajdú-Bihar/Budapest | 0.115 [0.069; 0.162] | −0.021 [−0.065; 0.023] | 0.116 [0.069; 0.162] | 0.047 [0.000; 0.094] | −0.063 [−0.112; −0.015] | −0.051 [−0.097; −0.004] | −0.092 [−0.138; −0.046] |
| Heves/Budapest | −0.014 [−0.052; 0.024] | −0.247 [−0.283; −0.211] | −0.013 [−0.051; 0.025] | −0.051 [−0.089; −0.013] | −0.011 [−0.050; 0.029] | −0.046 [−0.084; −0.009] | −0.077 [−0.115; −0.039] |
| Komárom-Esztergom/Budapest | −0.066 [−0.103; −0.029] | −0.175 [−0.210; −0.141] | −0.066 [0.102; −0.029] | −0.072 [−0.109; −0.035] | −0.020 [−0.059; 0.018] | −0.0067 [−0.103; −0.031] | −0.032 [−0.068; 0.005] |
| Nógrád/Budapest | −0.078 [−0.115; −0.040] | −0.150 [−0.186; −0.115] | −0.078 [−0.115; −0.040] | −0.056 [−0.093; −0.018] | −0.001 [−0.040; 0.038] | −0.084 [−0.121; −0.047] | −0.121 [−0.158; −0.083] |
| Pest/Budapest | −0.006 [−0.059; 0.047] | −0.176 [−0.226; −0.126] | −0.005 [−0.058; 0.048] | −0.032 [−0.085; 0.021] | −0.045 [−0.100; 0.010] | −0.037 [−0.090; 0.015] | 0.004 [−0.049; 0.057] |
| Somogy/Budapest | −0.004 [−0.044; 0.035] | −0.143 [−0.180; −0.106] | −0.004 [−0.043, 0.036] | −0.028 [−0.067; 0.012] | 0.083 [0.041, 0.124] | 0.009 [−0.030; 0.048] | 0.012 [−0.028; 0.051] |
| Szabolcs-Szatmár-Bereg/Budapest | 0.110 [0.063; 0.156] | −0.135 [−0.178; −0.091] | 0.110 [0.064; 0.157] | 0.085 [0.038; 0.132] | −0.050 [−0.098; −0.001] | −0.056 [−0.102; −0.010] | −0.084 [−0.130; −0.038] |
| Jász-Nagykun-Szolnok/Budapest | 0.044 [0.004; 0.085] | −0.189 [−0.228; −0.151] | 0.045 [0.004; 0.086] | −0.018 [−0.059; 0.023] | −0.052 [−0.095; −0.010] | −0.025 [−0.065; 0.016] | −0.063 [−0.104; −0.022] |
| Tolna/Budapest | −0.064 [−0.099; −0.029] | −0.097 [−0.130; −0.064] | −0.064 [−0.099; −0.028] | 0.048 [0.012; 0.083] | 0.054 [0.018; 0.091] | 0.016 [−0.019; 0.051] | 0.030 [−0.005; 0.065] |
| Vas/Budapest | 0.084 [0.048; 0.120] | −0.076 [−0.110; −0.042] | 0.085 [0.049; 0.121] | 0.072 [0.036; 0.108] | −0.053 [−0.090; −0.015] | −0.014 [−0.050; 0.021] | 0.006 [−0.030; 0.042] |
| Veszprém/Budapest | −0.001 [−0.039; 0.038] | −0.116 [−0.152; −0.080] | 0.000 [−0.038; 0.038] | −0.001 [−0.040; 0.037] | 0.002 [−0.038; 0. 041] | −0.054 [−0.091; −0.016] | −0.050 [−0.088; −0.012] |
| Zala/Budapest | 0.019 [−0.016; 0.055] | −0.107 [−0.140; 0.073] | 0.020 [−0.016; 0.055] | 0.018 [−0.018; 0.053] | 0.044 [0.007; 0.081] | −0.067 [−0.102; −0.032] | −0.070 [−0.106; −0.035] |
| GMP type (adult/mixed) | 0.069 [0.021; 0.117] | 0.017 [−0.029; 0.062] | 0.069 [0.021; 0.117] | 0.084 [0.035; 0.132] | −0.057 [−0.107; −0.007] | −0.025 [−0.072; 0.023] | 0.022 [−0.026; 0.070] |
| Settlement type (urban/rural) | 0.059 [0.010; 0.108] | 0.048 [0.001; 0.094] | 0.059 [0.010; 0.108] | 0.075 [0.026; 0.125] | −0.007 [−0.058; 0.045] | −0.058 [−0.107; −0.009] | −0.072 [−0.121; −0.023] |
| GP (vacancy/age < 65) | 0.000 [−0.029; 0.029] | 0.013 [−0.014; 0.041] | 0.000 [−0.029, 0.029] | 0.014 [−0.015; 0.044] | −0.053 [−0.083; −0.022] | 0.012 [−0.017; 0.041] | 0.000 [−0.030; 0.029] |
| GP (age ≥ 65X/age < 65) | −0.082 [−0.110; −0.055] | −0.025 [−0.051; 0.001] | −0.082 [−0.110; −0.055] | −0.086 [−0.113; −0.058] | −0.032 [−0.060; −0.003] | −0.036 [−0.063; −0.009] | −0.050 [−0.078; −0.023] |
| List size (≤800/1201–1600) | −0.009 [−0.038; 0.021] | −0.037 [−0.064; −0.009] | −0.008 [−0.038; 0.021] | −0.007 [−0.037; 0.022] | 0.009 [−0.021; 0.040] | −0.017 [−0.046; 0.012] | −0.017 [−0.047; 0.012] |
| List size (801–1200/1201–1600) | −0.019 [−0.049; 0.011] | −0.001 [−0.029; 0.028] | −0.019 [−0.049; 0.011] | −0.017 [−0.047; 0.014] | 0.003 [−0.028; 0.035] | −0.021 [−0.051; 0.009] | −0.015 [−0.045; 0.015] |
| List size (1601–2000/1201–1600) | −0.017 [−0.048; 0.015] | −0.031 [−0.061; −0.001] | −0.017 [−0.048; 0.015] | −0.001 [−0.033; 0.030] | −0.016 [−0.049; 0.017] | 0.014 [−0.017; 0.046] | 0.016 [−0.016; 0.047] |
| List size (>2000/1201–1600) | −0.068 [−0.100; −0.036] | −0.031 [−0.061; −0.001] | −0.068 [−0.100; −0.036] | −0.053 [−0.085; −0.021] | −0.040 [−0.074; −0.007] | 0.003 [−0.029; 0.035] | 0.006 [−0.026; 0.038] |
| Level of education (low/medium) | −0.108 [−0.153; −0.063] | −0.100 [−0.142; −0.057] | −0.108 [0.153; −0.063] | −0.103 [−0.148; −0.058] | −0.005 [−0.0051; 0.042] | 0.048 [0.004; 0.093] | 0.019 [−0.026; 0.063] |
| Level of education (high/medium) | 0.048 [0.002; 0.094] | 0.036 [−0.007; 0.079] | 0.048 [0.002; 0094] | 0.036 [−0.010; 0.082] | 0.039 [−0.009; 0.087] | −0.176 [−0.222; −0.131] | −0.139 [−0.185; −0.093] |
| Employment ratio (low/medium) | −0.018 [−0.064; 0.028] | −0.018 [−0.061; 0.026] | −0.018 [−0.064; 0.028] | −0.014 [−0.061; 0.032] | 0.056 [0.008; 0.104] | 0.051 [0.005; 0.097] | 0.061 [0.015; 0.107] |
| Employment ratio (high/medium) | 0.002 [−0.046; 0.050] | 0.030 [−0.016; 0.075] | 0.002 [−0.046; 0.050] | −0.024 [−0.072; 0.025] | 0.009 [−0.041; 0.059] | −0.067 [−0.115; −0.020] | −0.111 [−0.159; −0.063] |
| Housing density (low/medium) | 0.041 [−0.003; 0.084] | −0.084 [−0.126; −0.043] | 0.040 [−0.003; 0.084] | 0.018 [−0.025; 0.062] | −0.001 [−0.046; 0.045] | −0.056 [−0.099; −0.013] | −0.049 [−0.092; −0.005] |
| Housing density (high/medium) | −0.008 [−0.046; 0.031] | −0.038 [−0.074; −0.002] | −0.007 [−0.046; 0.031] | −0.013 [−0.051; 0.026] | 0.000 [−0.040; 0.040] | 0.049 [0.011; 0.086] | 0.047 [0.009; 0.085] |
| Proportion Roma (low/medium) | −0.012 [−0.055; 0.031] | 0.015 [−0.026; 0.055] | −0.012 [−0.055; 0.031] | 0.016 [−0.027; 0.059] | 0.051 [0.006; 0.096] | −0.040 [−0.083; 0.002] | 0.014 [−0.029; 0.057] |
| Proportion Roma (high/medium) | −0.014 [−0.0060; 0.033] | −0.022 [−0.066; 0.022] | −0.014 [−0.060; 0.033] | 0.014 [−0.033; 0.061] | −0.031 [−0.079; 0.018] | 0.016 [−0.030; 0.063] | 0.039 [−0.007; 0.086] |
References
- Sun, H.; Saeedi, P.; Karuranga, S.; Pinkepank, M.; Ogurtsova, K.; Duncan, B.B.; Stein, C.; Basit, A.; Chan, J.C.N.; Mbanya, J.C.; et al. IDF Diabetes Atlas: Global, Regional and Country-Level Diabetes Prevalence Estimates for 2021 and Projections for 2045. Diabetes Res. Clin. Pract. 2022, 183, 109119. [Google Scholar] [CrossRef]
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and Regional Diabetes Prevalence Estimates for 2019 and Projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th Edition. Diabetes Res. Clin. Pract. 2019, 157, 107843. [Google Scholar] [CrossRef]
- Barnett, K.; Mercer, S.W.; Norbury, M.; Watt, G.; Wyke, S.; Guthrie, B. Epidemiology of Multimorbidity and Implications for Health Care, Research, and Medical Education: A Cross-Sectional Study. Lancet 2012, 380, 37–43. [Google Scholar] [CrossRef]
- Macinko, J.; Starfield, B.; Shi, L. The Contribution of Primary Care Systems to Health Outcomes within Organization for Economic Cooperation and Development (OECD) Countries, 1970–1998. Health Serv. Res. 2003, 38, 831–866. [Google Scholar] [CrossRef] [PubMed]
- Lachin, J.M.; Genuth, S.; Cleary, P.; Davis, M.D.; Nathan, D.M. Retinopathy and Nephropathy in Patients with Type 1 Diabetes Four Years after a Trial of Intensive Therapy. N. Engl. J. Med. 2000, 342, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Hemmingsen, B.; Lund, S.S.; Gluud, C.; Vaag, A.; Almdal, T.; Hemmingsen, C.; Wetterslev, J. Intensive Glycaemic Control for Patients with Type 2 Diabetes: Systematic Review with Meta-Analysis and Trial Sequential Analysis of Randomised Clinical Trials. BMJ 2011, 343, d6898. [Google Scholar] [CrossRef] [PubMed]
- UK Prospective Diabetes Study Group. Tight Blood Pressure Control and Risk of Macrovascular and Microvascular Complications in Type 2 Diabetes: UKPDS 38. BMJ 1998, 317, 703–713. [Google Scholar] [CrossRef]
- Roland, M.; Guthrie, B. Quality and Outcomes Framework: What Have We Learnt? BMJ 2016, 354, i4060. [Google Scholar] [CrossRef] [PubMed]
- Khan, N.; Rudoler, D.; McDiarmid, M.; Peckham, S. A Pay for Performance Scheme in Primary Care: Meta-Synthesis of Qualitative Studies on the Provider Experiences of the Quality and Outcomes Framework in the UK. BMC Fam. Pract. 2020, 21, 142. [Google Scholar] [CrossRef] [PubMed]
- NICE UK, Standards and Indicators. Indicators|Standards and Indicators. NICE. Available online: https://www.nice.org.uk/standards-and-indicators/indicators (accessed on 15 December 2021).
- Australian Institute of Health and Welfare. Indicators for the Australian National Diabetes Strategy 2016–2020: Data Update; Australian Institute of Health and Welfare: Canberra, Australia, 2021.
- Kovács, N.; Pálinkás, A.; Sipos, V.; Nagy, A.; Harsha, N.; Kőrösi, L.; Papp, M.; Ádány, R.; Varga, O.; Sándor, J. Factors Associated with Practice-Level Performance Indicators in Primary Health Care in Hungary: A Nationwide Cross-Sectional Study. Int. J. Environ. Res. Public Health 2019, 16, 3153. [Google Scholar] [CrossRef] [PubMed]
- Gabrys, L.; Heidemann, C.; Schmidt, C.; Baumert, J.; Teti, A.; Du, Y.; Paprott, R.; Ziese, T.; Banzer, W.; Böhme, M.; et al. Robert Koch-Institut. Selecting and Defining Indicators for Diabetes Surveillance in Germany. J. Health Monit. 2018, 3, 3–21. [Google Scholar] [CrossRef]
- Forbes, L.J.; Marchand, C.; Doran, T.; Peckham, S. The Role of the Quality and Outcomes Framework in the Care of Long-Term Conditions: A Systematic Review. Br. J. Gen. Pract. 2017, 67, e775–e784. [Google Scholar] [CrossRef]
- Khunti, K.; Gadsby, R.; Millett, C.; Majeed, A.; Davies, M. Quality of Diabetes Care in the UK: Comparison of Published Quality-of-Care Reports with Results of the Quality and Outcomes Framework for Diabetes. Diabet. Med. J. Br. Diabet. Assoc. 2007, 24, 1436–1441. [Google Scholar] [CrossRef]
- Rhys, G.; Beerstecher, H.J.; Morgan, C.L. Primary Care Capitation Payments in the UK. An Observational Study. BMC Health Serv. Res. 2010, 10, 156. [Google Scholar] [CrossRef]
- Cunningham, S.G.; Carinci, F.; Brillante, M.; Leese, G.P.; McAlpine, R.R.; Azzopardi, J.; Beck, P.; Bratina, N.; Bocquet, V.; Doggen, K.; et al. Core Standards of the EUBIROD Project. Defining a European Diabetes Data Dictionary for Clinical Audit and Healthcare Delivery. Methods Inf. Med. 2016, 55, 166–176. [Google Scholar] [CrossRef] [PubMed]
- Marshall, M.N.; Shekelle, P.G.; McGlynn, E.A.; Campbell, S.; Brook, R.H.; Roland, M.O. Can Health Care Quality Indicators Be Transferred between Countries? BMJ Qual. Saf. 2003, 12, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Nagy, A.; Kovács, N.; Pálinkás, A.; Sipos, V.; Vincze, F.; Szőllősi, G.; Ádány, R.; Czifra, Á.; Sándor, J. Improvement in Quality of Care for Patients with Type 2 Diabetes in Hungary between 2008 and 2016: Results from Two Population-Based Representative Surveys. Diabetes Ther. 2019, 10, 757–763. [Google Scholar] [CrossRef] [PubMed]
- Kringos, D.; Boerma, W.; Bourgueil, Y.; Cartier, T.; Dedeu, T.; Hasvold, T.; Hutchinson, A.; Lember, M.; Oleszczyk, M.; Rotar Pavlic, D.; et al. The Strength of Primary Care in Europe: An International Comparative Study. Br. J. Gen. Pract. J. R. Coll. Gen. Pract. 2013, 63, e742–e750. [Google Scholar] [CrossRef] [PubMed]
- Ádány, R.; Kósa, K.; Sándor, J.; Papp, M.; Fürjes, G. General practitioners’ cluster: A model to reorient primary health care to public health services. Eur. J. Public Health 2013, 23, 529–530. [Google Scholar] [CrossRef] [PubMed]
- Jakab, Z. Public health, primary care and the ‘cluster’ model. Eur. J. Public Health 2013, 23, 528. [Google Scholar] [CrossRef]
- Ben-Shlomo, Y.; White, I.; McKeigue, P.M. Prediction of general practice workload from census based social deprivation scores. J. Epidemiol. Community Health 1992, 46, 532–536. [Google Scholar] [CrossRef]
- Sándor, J.; Kósa, K.; Papp, M.; Fürjes, G.; Kőrösi, L.; Jakovljevic, M.; Ádány, R. Capitation-Based Financing Hampers the Provision of Preventive Services in Primary Health Care. Front. Public Health 2016, 4, 200. [Google Scholar] [CrossRef]
- Greenland, S.; Robins, J.M. Empirical-Bayes Adjustments for Multiple Comparisons Are Sometimes Useful. Epidemiology 1991, 2, 244–251. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Templeton, G.F. A Two-Step Approach for Transforming Continuous Variables to Normal: Implications and Recommendations for IS Research. Commun. Assoc. Inf. Syst. 2011, 28, 4. [Google Scholar] [CrossRef]
- Bickel, P.J.; Doksum, K.A. An Analysis of Transformations Revisited. J. Am. Stat. Assoc. 1981, 76, 296–311. [Google Scholar] [CrossRef]
- Flowers, J.; Hall, P.; Pencheon, D. Public Health Indicators. Public Health 2005, 119, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.A.B.; Hashim, M.J.; King, J.K.; Govender, R.D.; Mustafa, H.; Al Kaabi, J. Epidemiology of Type 2 Diabetes—Global Burden of Disease and Forecasted Trends. J. Epidemiol. Glob. Health 2020, 10, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Grintsova, O.; Maier, W.; Mielck, A. Inequalities in Health Care among Patients with Type 2 Diabetes by Individual Socio-Economic Status (SES) and Regional Deprivation: A Systematic Literature Review. Int. J. Equity Health 2014, 13, 43. [Google Scholar] [CrossRef]
- Suwannaphant, K.; Laohasiriwong, W.; Puttanapong, N.; Saengsuwan, J.; Phajan, T. Association between Socioeconomic Status and Diabetes Mellitus: The National Socioeconomics Survey, 2010 and 2012. J. Clin. Diagn. Res. JCDR 2017, 11, LC18–LC22. [Google Scholar] [CrossRef]
- Flatz, A.; Casillas, A.; Stringhini, S.; Zuercher, E.; Burnand, B.; Peytremann-Bridevaux, I. Association between Education and Quality of Diabetes Care in Switzerland. Int. J. Gen. Med. 2015, 8, 87–92. [Google Scholar] [CrossRef] [PubMed]
- Choudhry, N.K.; Fletcher, R.H.; Soumerai, S.B. Systematic Review: The Relationship between Clinical Experience and Quality of Health Care. Ann. Intern. Med. 2005, 142, 260–273. [Google Scholar] [CrossRef]
- Tsugawa, Y.; Newhouse, J.P.; Zaslavsky, A.M.; Blumenthal, D.M.; Jena, A.B. Physician Age and Outcomes in Elderly Patients in Hospital in the US: Observational Study. BMJ 2017, 357, j1797. [Google Scholar] [CrossRef]
- Andrus, M.R.; Kelley, K.W.; Murphey, L.M.; Herndon, K.C. A Comparison of Diabetes Care in Rural and Urban Medical Clinics in Alabama. J. Community Health 2004, 29, 29–44. [Google Scholar] [CrossRef]
- Lutfiyya, M.N.; Patel, Y.R.; Steele, J.B.; Tetteh, B.S.; Chang, L.; Aguero, C.; Prakash, O.; Lipsky, M.S. Are There Disparities in Diabetes Care? A Comparison of Care Received by US Rural and Non-Rural Adults with Diabetes. Prim. Health Care Res. Dev. 2009, 10, 320–331. [Google Scholar] [CrossRef]
- Goyder, E.C.; Botha, J.L.; McNally, P.G. Inequalities in Access to Diabetes Care: Evidence from a Historical Cohort Study. BMJ Qual. Saf. 2000, 9, 85–89. [Google Scholar] [CrossRef][Green Version]
- Nosrati, E.; Jenum, A.; Tran, A.; Marmot, M.; King, L. Ethnicity and Place: The Geography of Diabetes Inequalities under a Strong Welfare State. Eur. J. Public Health 2017, 28, 30–34. [Google Scholar] [CrossRef]
- Ramalho, A.; Castro, P.; Lobo, M.; Souza, J.; Santos, P.; Freitas, A. Integrated Quality Assessment for Diabetes Care in Portuguese Primary Health Care Using Prevention Quality Indicators. Prim. Care Diabetes 2021, 15, 507–512. [Google Scholar] [CrossRef]
- Connolly, V.; Unwin, N.; Sherriff, P.; Bilous, R.; Kelly, W. Diabetes Prevalence and Socioeconomic Status: A Population Based Study Showing Increased Prevalence of Type 2 Diabetes Mellitus in Deprived Areas. J. Epidemiol. Community Health 2000, 54, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Maier, W.; Holle, R.; Hunger, M.; Peters, A.; Meisinger, C.; Greiser, K.H.; Kluttig, A.; Völzke, H.; Schipf, S.; Moebus, S.; et al. DIAB-CORE Consortium. The Impact of Regional Deprivation and Individual Socio-Economic Status on the Prevalence of Type 2 Diabetes in Germany. A Pooled Analysis of Five Population-Based Studies. Diabet. Med. J. Br. Diabet. Assoc. 2013, 30, e78–e86. [Google Scholar] [CrossRef] [PubMed]
- Berkowitz, S.A.; Meigs, J.B.; DeWalt, D.; Seligman, H.K.; Barnard, L.S.; Bright, O.-J.M.; Schow, M.; Atlas, S.J.; Wexler, D.J. Material Need Insecurities, Control of Diabetes Mellitus, and Use of Health Care Resources: Results of the Measuring Economic Insecurity in Diabetes Study. JAMA Intern. Med. 2015, 175, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Törő, V.; Sarvary, A.; Takács, P.; Barkaszi, A.; György, L.; Kósa, Z. Assessment of Quality Care of Chronic Illness Patients Living in Roma Colonies and in the General Population: A Comparative Study. Cent. Eur. J. Occup. Environ. Med. 2017, 23, 58–69. [Google Scholar]
- Kolvek, G.; Rosicova, K.; Rosenberger, J.; Podracka, L.; Stewart, R.; Nagyova, I.; Reijneveld, S.A.; Dijk, J.P. End-Stage Renal Disease among Roma and Non-Roma: Roma Are at Risk. Int. J. Public Health 2012, 57, 751–754. [Google Scholar] [CrossRef] [PubMed]
- Nøkleby, K.; Berg, T.J.; Mdala, I.; Tran, A.T.; Bakke, Å.; Gjelsvik, B.; Claudi, T.; Cooper, J.G.; Løvaas, K.F.; Thue, G.; et al. Variation between General Practitioners in Type 2 Diabetes Processes of Care. Prim. Care Diabetes 2021, 15, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Turchin, A.; Shubina, M.; Pendergrass, M.L. Relationship of Physician Volume with Process Measures and Outcomes in Diabetes. Diabetes Care 2007, 30, 1442–1447. [Google Scholar] [CrossRef] [PubMed]
- Zeh, P.; Sandhu, H.; Cannaby, A.-M.; Sturt, J. Cultural Barriers Impeding Ethnic Minority Groups from Accessing Effective Diabetes Care Services: A Systematic Review of Observational Studies. Divers. Equal. Health Care 2014, 11, 9–33. [Google Scholar] [CrossRef]
- Jin, Y.; Zhu, W.; Yuan, B.; Meng, Q. Impact of Health Workforce Availability on Health Care Seeking Behavior of Patients with Diabetes Mellitus in China. Int. J. Equity Health 2017, 16, 80. [Google Scholar] [CrossRef]
- Patel, M.R. Social Determinants of Poor Management of Type 2 Diabetes among the Insured. Curr. Diab. Rep. 2020, 20, 67. [Google Scholar] [CrossRef]
- Schillinger, D.; Grumbach, K.; Piette, J.; Wang, F.; Osmond, D.; Daher, C.; Palacios, J.; Sullivan, G.D.; Bindman, A.B. Association of Health Literacy with Diabetes Outcomes. JAMA 2002, 288, 475–482. [Google Scholar] [CrossRef]
- Rosiek, A.; Kornatowski, T.; Frackowiak-Maciejewska, N.; Rosiek-Kryszewska, A.; Wyżgowski, P.; Leksowski, K. Health Behaviors of Patients Diagnosed with Type 2 Diabetes Mellitus and Their Influence on the Patients’ Satisfaction with Life. Ther. Clin. Risk Manag. 2016, 12, 1783–1792. [Google Scholar] [CrossRef]
| Indicator Name | Target Group | Indicator Definition | |
|---|---|---|---|
| Process indicators | HemoglobinA1c testing | Primary health care patients with DM | Proportion of diabetics who were involved in hemoglobin A1c testing (at least once in previous 12 months) |
| Ophthalmological examination | Primary health care patients with DM | Proportion of diabetics who participated in an ophthalmological examination (at least once in previous 12 months) | |
| Serum creatinine check | Primary health care patients with DM | Proportion of diabetic patients who participated in a serum creatinine determination (at least once in previous 12 months) | |
| Influenza vaccination | Primary health care patients with DM under 65 years old | Proportion of diabetic patients under 65 years of age who were vaccinated against influenza | |
| Lipid status checking | Primary health care patients with DM | Proportion of diabetics who participated in a serum lipid status test (at least once in previous 12 months) | |
| Prevalence indicators | DM patients aged 40–54 years | 40–54-years-old primary health care patients with DM | Proportion of diabetic patients, aged 40–54 years, who redeemed a diabetic medicine at least 4 times in the previous 12 months |
| DM patients aged 55–69 years | 55–69-years-old primary health care patient with DM | Proportion of diabetic patients, aged 55–69 years, who redeemed a diabetic medicine at least 4 times in the previous 12 months |
| Structural Characteristics of the GMP | Categories | GMP | DM Patients | ||
|---|---|---|---|---|---|
| N | Percentage | N | Percentage | ||
| Settlement type | Rural | 3172 | 66.30% | 365,381 | 70.80% |
| Urban | 1612 | 33.70% | 150,671 | 29.20% | |
| GMP list size | <800 | 153 | 3.00% | 7207 | 1.40% |
| 801–1200 | 655 | 14.00% | 45,335 | 8.78% | |
| 1201–1600 | 1522 | 32.00% | 142,544 | 27.62% | |
| 1601–2000 | 1504 | 31.00% | 178,537 | 34.60% | |
| >2000 | 950 | 20.00% | 142,429 | 27.60% | |
| GP vacancy | Filled | 4608 | 96.30% | 503,713 | 97.60% |
| Vacant | 176 | 3.70% | 12,339 | 2.40% | |
| GMP type | Adult | 3317 | 69.00% | 385,372 | 74.68% |
| Mixed | 1467 | 31.00% | 130,680 | 25.32% | |
| Age of GP (years) | <65 | 1019 | 22.11% | 103,895 | 20.12% |
| ≥65 | 3589 | 77.89% | 399,818 | 77.48% | |
| County | Baranya | 207 | 4.33% | 21,458 | 4.15% |
| Bács-Kiskun | 256 | 5.35% | 27,720 | 5.37% | |
| Békés | 187 | 3.91% | 19,939 | 3.86% | |
| Borsod-Abaúj-Zemplén | 370 | 7.73% | 35,345 | 6.85% | |
| Csongrád | 204 | 4.26% | 18,907 | 3.66% | |
| Fejér | 194 | 4.06% | 22,576 | 4.37% | |
| Győr-Moson-Sopron | 202 | 4.22% | 23,251 | 4.51% | |
| Hajdú-Bihar | 242 | 5.06% | 25,993 | 5.04% | |
| Heves | 160 | 3.34% | 16,616 | 3.22% | |
| Komárom-Esztergom | 141 | 2.95% | 16,105 | 3.12% | |
| Nógrád | 109 | 2.28% | 10,537 | 2.04% | |
| Pest | 466 | 9.74% | 61,273 | 11.87% | |
| Somogy | 172 | 3.60% | 18,934 | 3.67% | |
| Szabolcs-Szatmár-Bereg | 265 | 5.54% | 28,431 | 5.50% | |
| Jász-Nagykun-Szolnok | 192 | 4.01% | 21,118 | 4.10% | |
| Tolna | 119 | 2.49% | 14,144 | 2.74% | |
| Vas | 133 | 2.78% | 14,551 | 2.82% | |
| Veszprém | 164 | 3.43% | 18,889 | 3.66% | |
| Zala | 141 | 2.95% | 14,868 | 2.90% | |
| Budapest | 860 | 17.98% | 85,397 | 16.55% | |
| Total | 4784 | 100% | 516,052 | 100% | |
| Process Indicators | DM Prevalence | ||||||
|---|---|---|---|---|---|---|---|
| HemoglobinA1c Testing | Ophthalmological Examination | Serum Creatinine Testing | Serum Lipid Status Testing | Influenza Vaccination | Among 40–54-Years-Old | Among 55–69-Years-Old | |
| GMP characteristics | |||||||
| GMP type (adult/mixed) | 0.069 [0.021; 0.117] | 0.017 [−0.029; 0.062] | 0.084 [0.035; 0.132] | 0.069 [0.021; 0.117] | −0.057 [−0.107; −0.007] | −0.025 [−0.072; 0.023] | 0.022 [−0.026; 0.070] |
| Settlement type (urban/rural) | 0.059 [0.010; 0.108] | 0.048 [0.001; 0.094] | 0.075 [0.026; 0.125] | 0.059 [0.010; 0.108] | −0.007 [−0.058; 0.045] | −0.058 [−0.107; −0.009] | −0.072 [−0.121; −0.023] |
| GP (vacancy/ age < 65) | 0.000 [−0.029; 0.029] | 0.013 [−0.014; 0.041] | 0.014 [−0.015; 0.044] | 0.000 [−0.029, 0.029] | −0.053 [−0.083; −0.022] | 0.012 [−0.017; 0.041] | 0.000 [−0.030; 0.029] |
| GP (age ≥ 65X/age < 65) | −0.082 [−0.110; −0.055] | −0.025 [−0.051; 0.001] | −0.086 [−0.113; −0.058] | −0.082 [−0.110; −0.055] | −0.032 [−0.060; −0.003] | −0.036 [−0.063; −0.009] | −0.050 [−0.078; −0.023] |
| List size (≤800/1201–1600) | −0.009 [−0.038; 0.021] | −0.037 [−0.064; −0.009] | −0.007 [−0.037; 0.022] | −0.008 [−0.038; 0.021] | 0.009 [−0.021; 0.040] | −0.017 [−0.046; 0.012] | −0.017 [−0.047; 0.012] |
| List size (801–1200/1201–1600) | −0.019 [−0.049; 0.011] | −0.001 [−0.029; 0.028] | −0.017 [−0.047; 0.014] | −0.019 [−0.049; 0.011] | 0.003 [−0.028; 0.035] | −0.021 [−0.051; 0.009] | −0.015 [−0.045; 0.015] |
| List size (1601–2000/1201–1600) | −0.017 [−0.048; 0.015] | −0.031 [−0.061; −0.001] | −0.001 [−0.033; 0.030] | −0.017 [−0.048; 0.015] | −0.016 [−0.049; 0.017] | 0.014 [−0.017; 0.046] | 0.016 [−0.016; 0.047] |
| List size (>2000/1201–1600) | −0.068 [−0.100; −0.036] | −0.031 [−0.061; −0.001] | −0.053 [−0.085; −0.021] | −0.068 [−0.100; −0.036] | −0.040 [−0.074; −0.007] | 0.003 [−0.029; 0.035] | 0.006 [−0.026; 0.038] |
| Patient characteristics | |||||||
| Level of education (low/medium) | −0.108 [−0.153; −0.063] | −0.100 [−0.142; −0.057] | −0.103 [−0.148; −0.058] | −0.108 [−0.153; −0.063] | −0.005 [−0.051; 0.042] | 0.048 [0.004; 0.093] | 0.019 [−0.026; 0.063] |
| Level of education (high/medium) | 0.048 [0.002; 0.094] | 0.036 [−0.007; 0.079] | 0.036 [−0.010; 0.082] | 0.048 [0.002; 0.094] | 0.039 [−0.009; 0.087] | −0.176 [−0.222; −0.131] | −0.139 [−0.185; −0.093] |
| Employment ratio (low/medium) | −0.018 [−0.064; 0.028] | −0.018 [−0.061; 0.026] | −0.014 [−0.061; 0.032] | −0.018 [−0.064; 0.028] | 0.056 [0.008; 0.104] | 0.051 [0.005; 0.097] | 0.061 [0.015; 0.107] |
| Employment ratio (high/medium) | 0.002 [−0.046; 0.050] | 0.030 [−0.016; 0.075] | −0.024 [−0.072; 0.025] | 0.002 [−0.046; 0.050] | 0.009 [−0.041; 0.059] | −0.067 [−0.115; −0.020] | −0.111 [−0.159; −0.063] |
| Housing density (low/medium) | 0.041 [−0.003; 0.084] | −0.084 [−0.126; −0.043] | 0.018 [−0.025; 0.062] | 0.040 [−0.003; 0.084] | −0.001 [−0.046; 0.045] | −0.056 [−0.099; −0.013] | −0.049 [−0.092; −0.005] |
| Housing density (high/medium) | −0.008 [−0.046; 0.031] | −0.038 [−0.074; −0.002] | −0.013 [−0.051; 0.026] | −0.007 [−0.046; 0.031] | 0.000 [−0.040; 0.040] | 0.049 [0.011; 0.086] | 0.047 [0.009; 0.085] |
| Proportion Roma (low/medium) | −0.012 [−0.055; 0.031] | 0.015 [−0.026; 0.055] | 0.016 [−0.027; 0.059] | −0.012 [−0.055; 0.031] | 0.051 [0.006; 0.096] | −0.040 [−0.083; 0.002] | 0.014 [−0.029; 0.057] |
| Proportion Roma (high/medium) | −0.014 [−0.060; 0.033] | −0.022 [−0.066; 0.022] | 0.014 [−0.033; 0.061] | −0.014 [−0.060; 0.033] | −0.031 [−0.079; 0.018] | 0.016 [−0.030; 0.063] | 0.039 [−0.007; 0.086] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jargalsaikhan, U.; Kasabji, F.; Vincze, F.; Pálinkás, A.; Kőrösi, L.; Sándor, J. Relationships between the Structural Characteristics of General Medical Practices and the Socioeconomic Status of Patients with Diabetes-Related Performance Indicators in Primary Care. Healthcare 2024, 12, 704. https://doi.org/10.3390/healthcare12070704
Jargalsaikhan U, Kasabji F, Vincze F, Pálinkás A, Kőrösi L, Sándor J. Relationships between the Structural Characteristics of General Medical Practices and the Socioeconomic Status of Patients with Diabetes-Related Performance Indicators in Primary Care. Healthcare. 2024; 12(7):704. https://doi.org/10.3390/healthcare12070704
Chicago/Turabian StyleJargalsaikhan, Undraa, Feras Kasabji, Ferenc Vincze, Anita Pálinkás, László Kőrösi, and János Sándor. 2024. "Relationships between the Structural Characteristics of General Medical Practices and the Socioeconomic Status of Patients with Diabetes-Related Performance Indicators in Primary Care" Healthcare 12, no. 7: 704. https://doi.org/10.3390/healthcare12070704
APA StyleJargalsaikhan, U., Kasabji, F., Vincze, F., Pálinkás, A., Kőrösi, L., & Sándor, J. (2024). Relationships between the Structural Characteristics of General Medical Practices and the Socioeconomic Status of Patients with Diabetes-Related Performance Indicators in Primary Care. Healthcare, 12(7), 704. https://doi.org/10.3390/healthcare12070704






