Effectiveness of Nonpharmacological Behavioural Interventions in Managing Dental Fear and Anxiety among Children: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Identification of Studies (PICO) and Eligibility Criteria
2.2. Search Strategy
2.3. Study Selection
2.4. Data Extraction
2.5. Assessment of Risk of Bias of Included Studies
2.6. Data Synthesis
2.7. Subgroup Analysis
2.8. Assessment of Heterogeneity
2.9. Assessment of Publication Bias
2.10. Assessment of Certainty of Evidence
3. Results
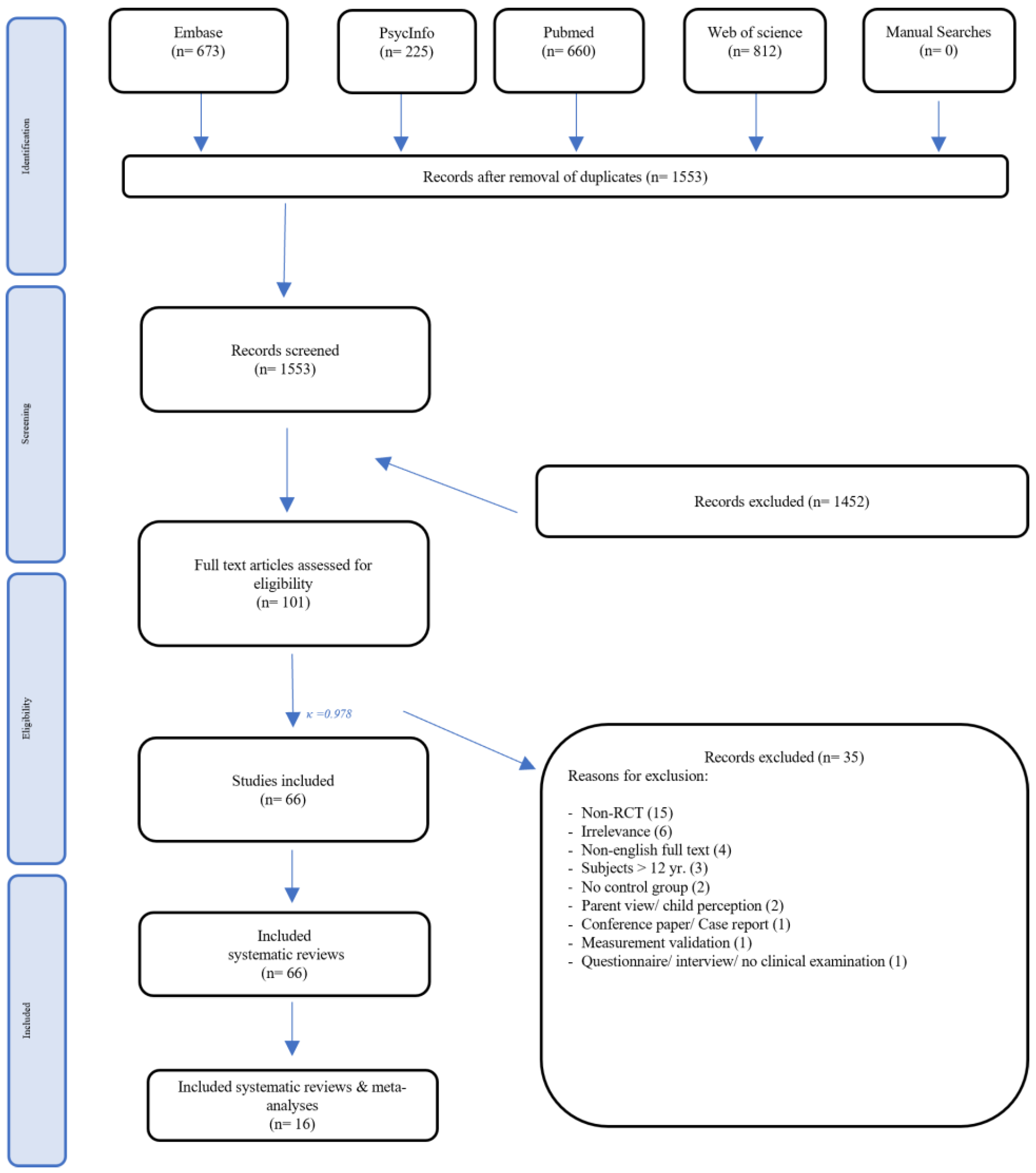
3.1. Study Selection
3.2. Study Characteristics
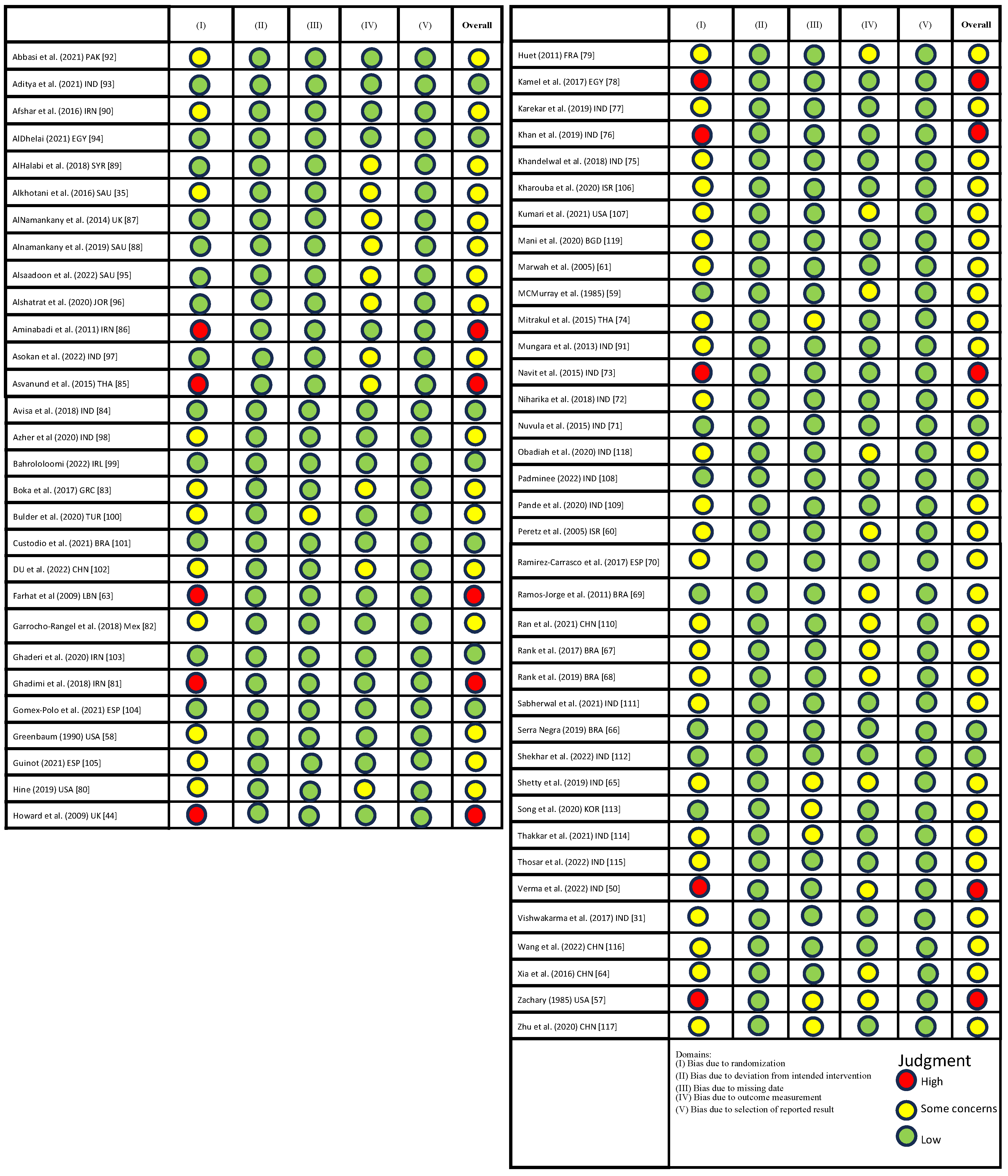
3.3. ROBS
3.4. Comparisons between NPBIs
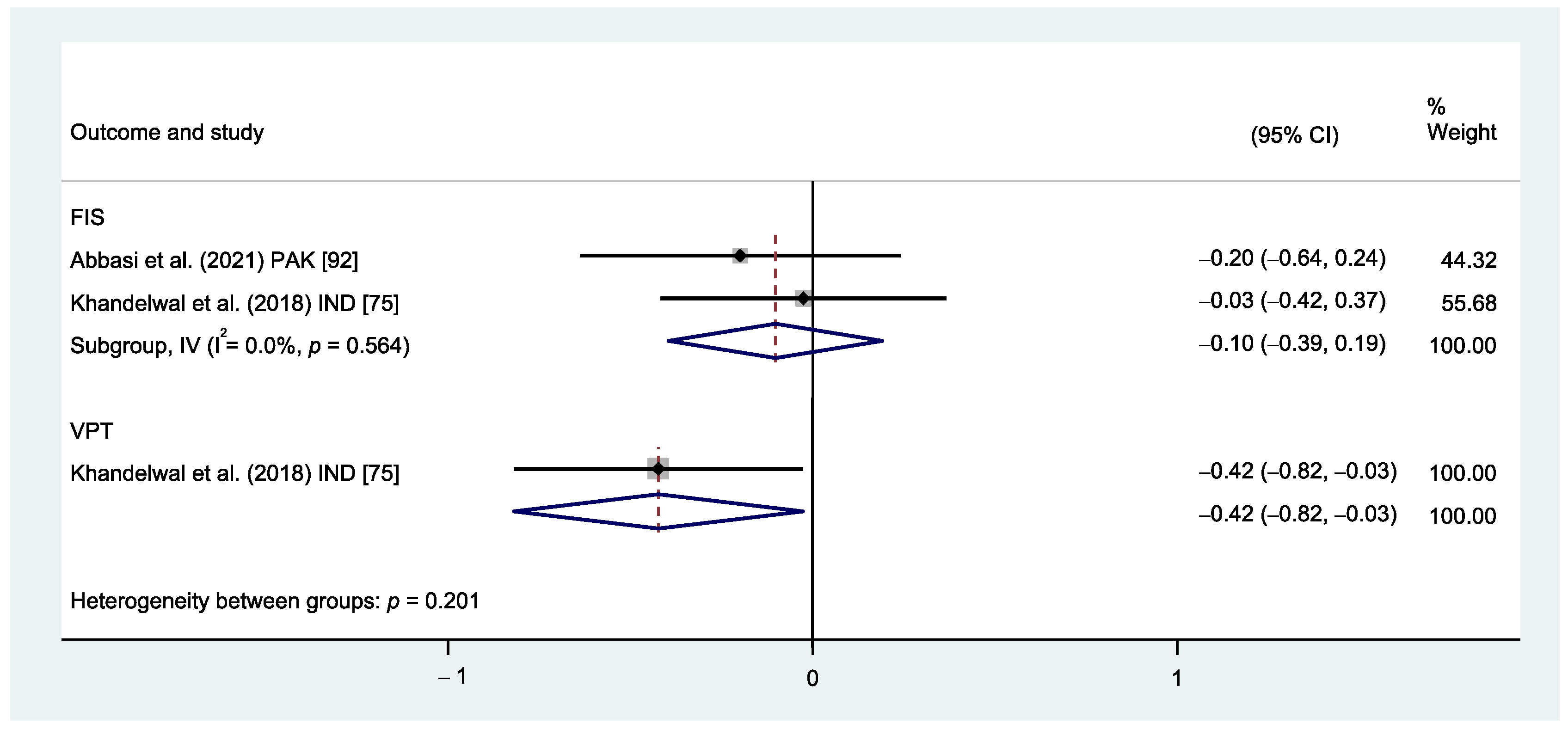
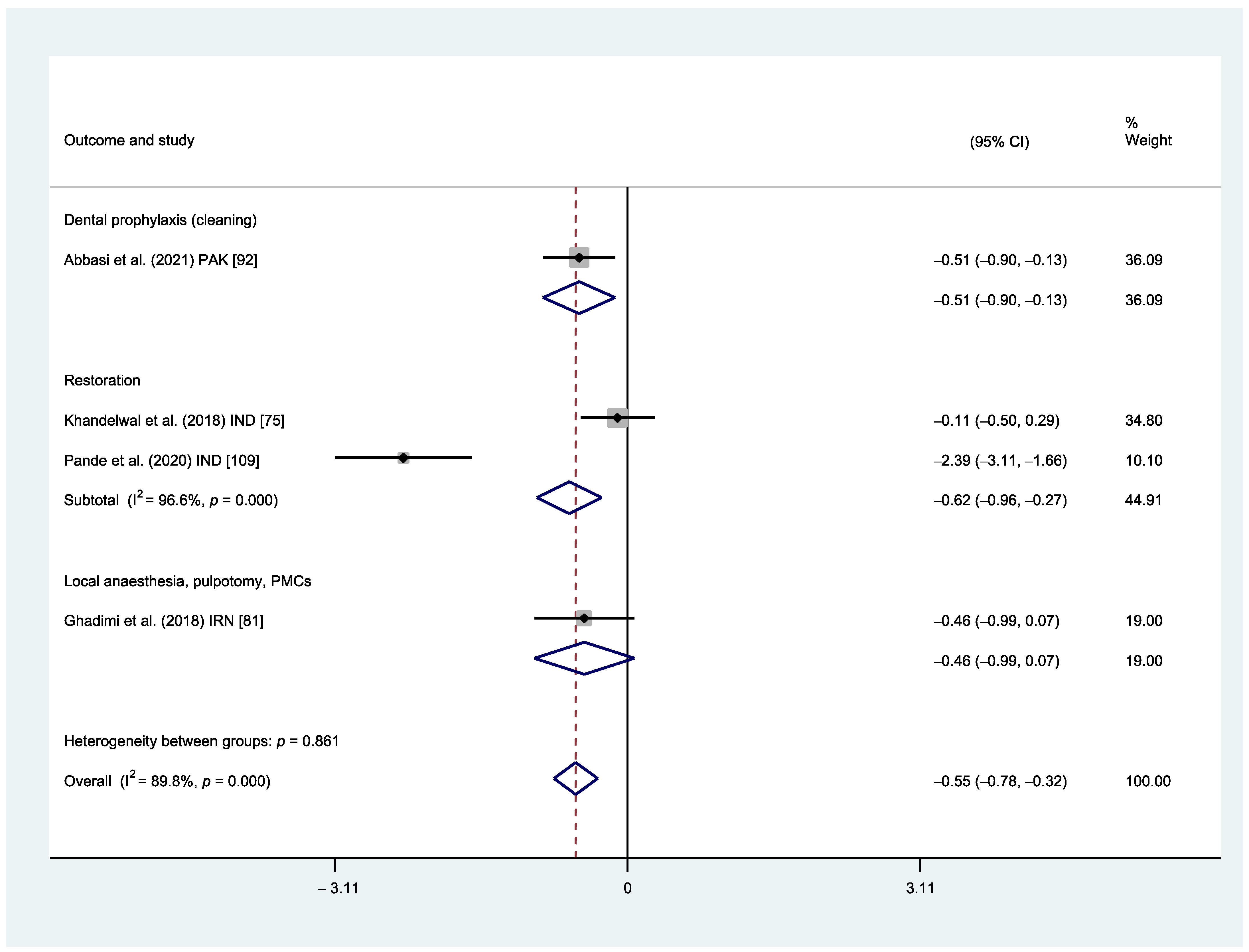
3.4.1. Distraction vs. Tell–Show–Do (TSD)
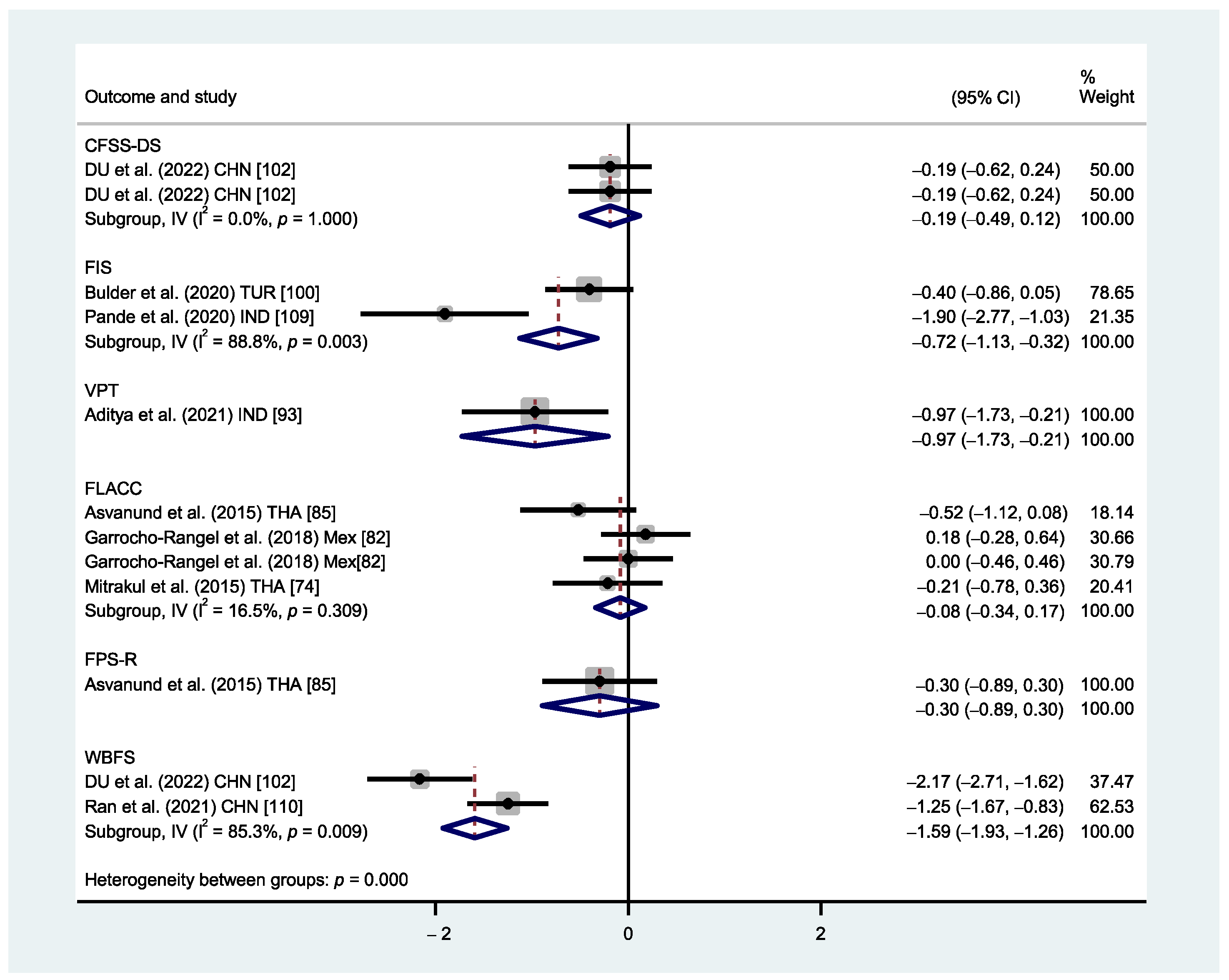
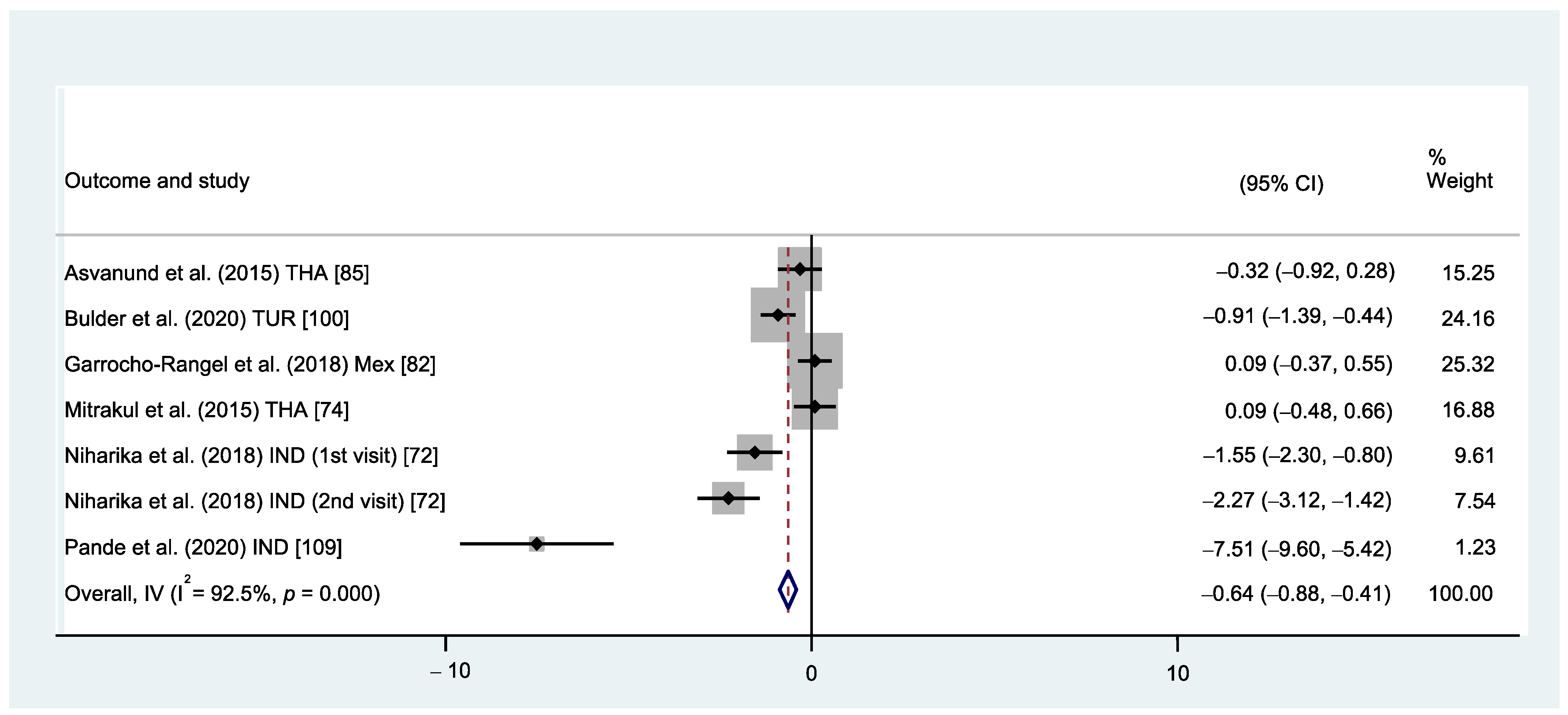
3.4.2. Virtual Reality (VR) vs. Traditional Behaviour Management
3.4.3. Tell–Show–Do vs. no Behavioural Intervention
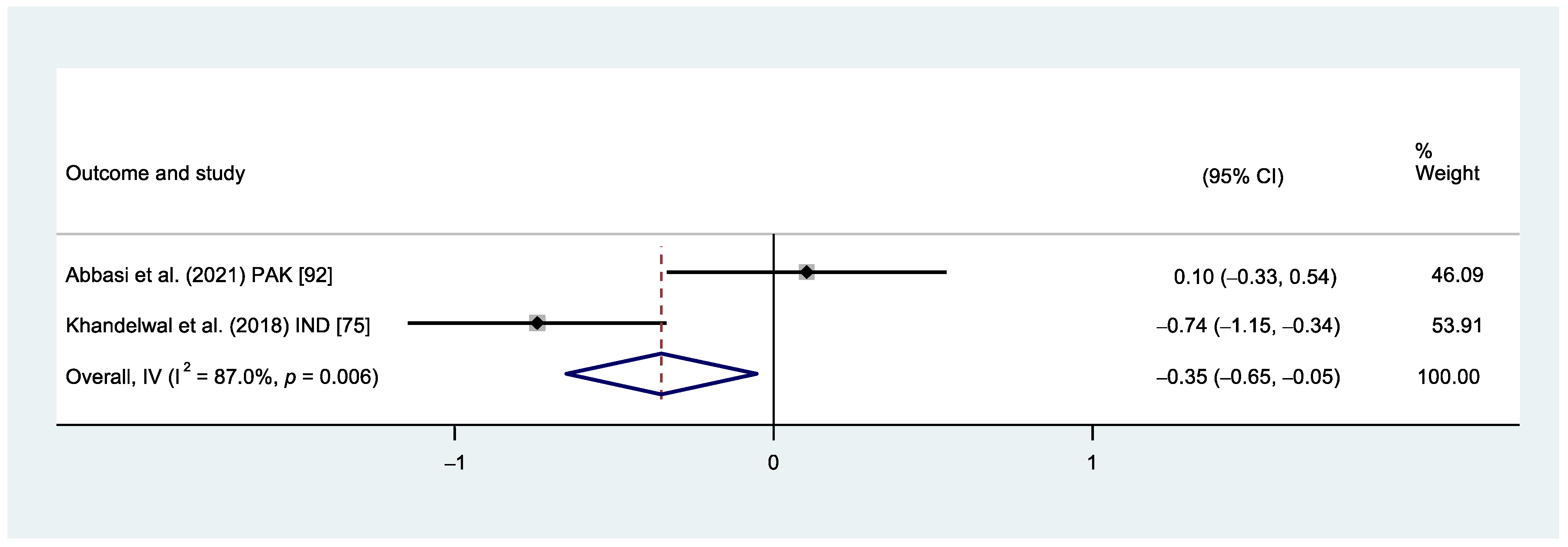
3.4.4. Video Modelling vs. Traditional Behavioural Management
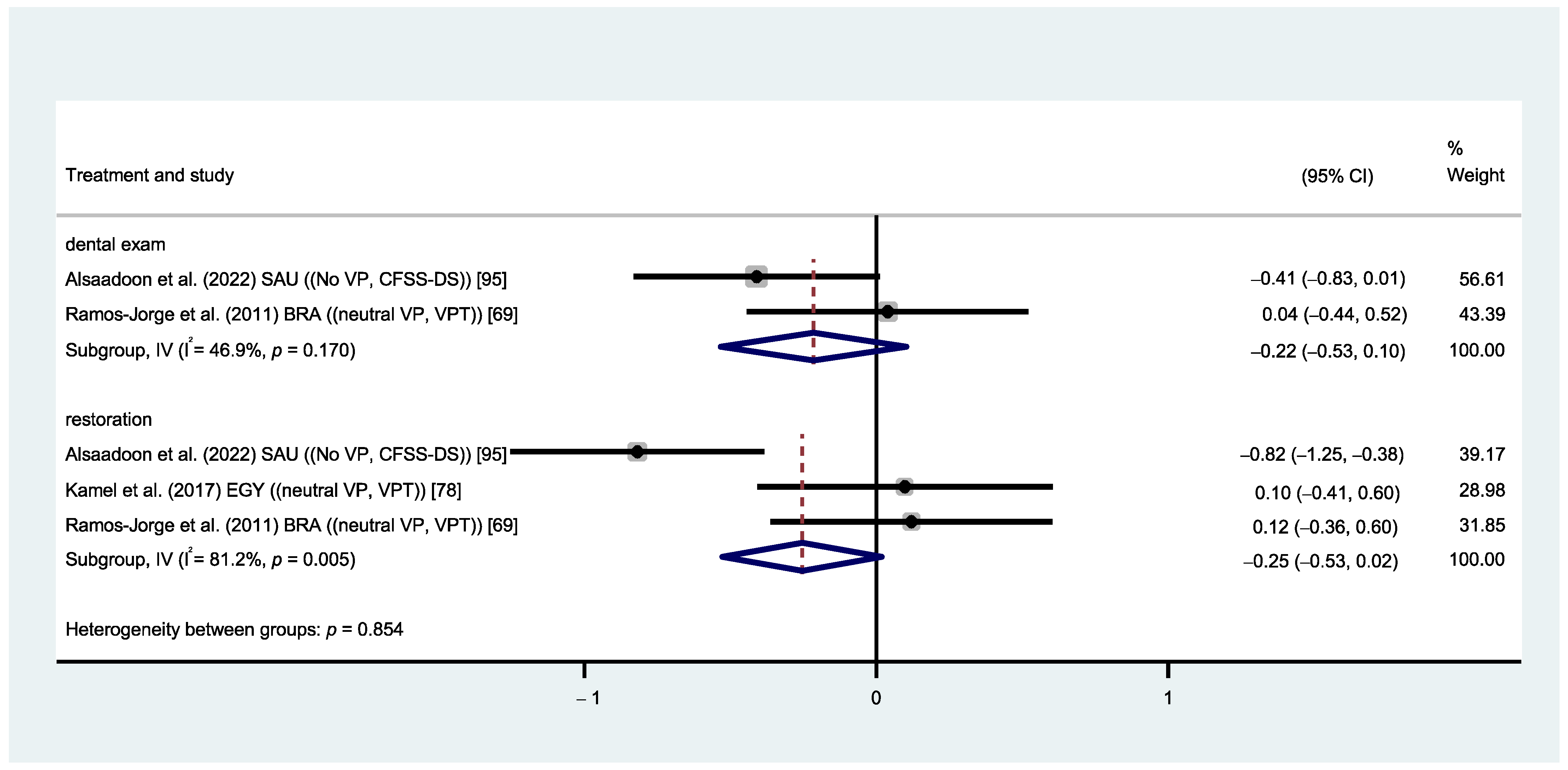
3.4.5. Visual Pedagogy vs. No Visual Pedagogy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| 1 | (paediatric or pediatric or child* or child management or paediatric dentistry or pediatric dentistry).mp. |
| 2 | (dental anxiety or dental fear or dental phobia or odontophobia).mp. |
| 3 | (Behavior* or conditioning or cognitive or cope or coping or Desensiti* or Exposure or flooding or hypno* or distract* or picture* or reapprais* or Mindfulness or Meditation or nonpharmacologic* or non-pharmacologic* or relax* or breath* or music* or audi* or visual* or odor* or smell* or reinforce* or tell show do or tell-show-do or model* or muscle* or biofeedback).mp. |
| 4 | Dental care or dental treatment or dentistry or oral health |
| 5 | review OR systematic review OR literature review OR meta-analysis OR case report OR case series |
| 6 | (animals or “not humans”).mp. [mp = title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword heading word, floating subheading word, candidate term word] |
| 7 | 5 or 6 |
| 8 | 1 and 2 and 3 and 4 NOT 7 |
- (pediatric or preschool or child*).mp. [mp = title, book title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
- dental caries/
- (Behavior* or conditioning or cognitive or cope or coping or Desensiti* or Exposure or flooding or hypno* or distract* or reapprais* or Mindfulness or Meditation or nonpharmacologic* or non-pharmacologic* or relax* or breath* or music* or audi* or visual* or odor* or smell* or reinforce* or tell show do or tell-show-do or model* or muscle* or biofeedback or virtual reality).mp. [mp = title, book title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
- (stress* or anxi* or fear* or phobi* or pain* or emotion*).mp. [mp = title, book title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
- (review or systematic review or literature review or meta-analysis or case report or case series).mp. [mp = title, book title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
- (“animals” or “not humans”).mp. [mp = title, book title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms]
- 1 and 2 and 3 and 4
- 5 and 6
- 7 not 8
- Title = (pediatric or preschool or child* or child* or infant*)
- AND Title = (dental caries OR carie* OR carious OR DMF)
- AND Title = (Behavior* OR conditioning OR cognitive OR cope OR coping OR Desensiti* OR Exposure OR flooding OR hypno* OR distract* OR reapprais* OR Mindfulness OR Meditation OR nonpharmacologic* OR non-pharmacologic* OR relax* OR breath* OR music* OR audi* OR visual* OR odor* OR smell* OR reinforce* OR “tell show do” OR “tell-show-do” OR model* OR muscle* OR “virtual reality” OR “biofeedback”)
- AND Title = (stress* OR anxi* OR fear* OR phobi* OR pain* OR emotion* OR fear* OR phobi* OR pain* OR emotion*)
- AND ALL = (“review” OR “systematic review” OR “meta-analysis” OR “case report” OR “case series”)
- AND ALL = (“animals” OR “not humans”)
Appendix B

References
- Kilinc, G.; Akay, A.; Eden, E.; Sevinc, N.; Ellidokuz, H. Evaluation of children’s dental anxiety levels at a kindergarten and at a dental clinic. Braz. Oral Res. 2016, 30, e72. [Google Scholar] [CrossRef] [PubMed]
- Klingberg, G. Dental anxiety and behaviour management problems in paediatric dentistry—A review of background factors and diagnostics. Eur. Arch. Paediatr. Dent. 2008, 9, 11–15. [Google Scholar] [CrossRef]
- Appukuttan, D.P. Strategies to manage patients with dental anxiety and dental phobia: Literature review. Clin. Cosmet. Investig. Dent. 2016, 8, 35. [Google Scholar] [CrossRef]
- Yon, M.J.Y.; Chen, K.J.; Gao, S.S.; Duangthip, D.; Lo, E.C.M.; Chu, C.H. Dental fear and anxiety of kindergarten children in Hong Kong: A cross-sectional study. Int. J. Environ. Res. Public Health 2020, 17, 2827. [Google Scholar] [CrossRef]
- Lee, C.Y.; Chang, Y.Y.; Huang, S.T. Prevalence of dental anxiety among 5- to 8-year-old Taiwanese children. J. Public Health Dent. 2007, 67, 36–41. [Google Scholar] [CrossRef]
- Salem, K.; Kousha, M.; Anissian, A.; Shahabi, A. Dental fear and concomitant factors in 3–6 year-old children. J. Dent. Res. Dent. Clin. Dent. Prospect. 2012, 6, 70. [Google Scholar]
- Lu, C.; Zhang, Y.Y.; Xiang, B.; Peng, S.-M.; Gu, M.; Wong, H.M. Management of fear and anxiety in dental treatments: A systematic review and meta-analysis of randomized controlled trials. Odontology 2022, 111, 20–32. [Google Scholar] [CrossRef]
- Yamada, M.; Tanabe, Y.; Sano, T.; Noda, T. Cooperation during dental treatment: The Children’s Fear Survey Schedule in Japanese children. Int. J. Paediatr. Dent. 2002, 12, 404–409. [Google Scholar] [CrossRef]
- Popescu, S.M.; Dascălu, I.T.; Scrieciu, M.; Mercuţ, V.; Moraru, I.; Ţuculină, M.J. Dental anxiety and its association with behavioral factors in children. Curr. Health Sci. J. 2014, 40, 261. [Google Scholar]
- Nicolas, E.; Collado, V.; Faulks, D.; Bullier, B.; Hennequin, M. A national cross-sectional survey of dental anxiety in the French adult population. BMC Oral Health 2007, 7, 12. [Google Scholar] [CrossRef]
- De Carvalho, R.W.F.; de Carvalho Bezerra Falcão, P.G.; de Luna Campos, G.J.; de Souza Andrade, E.S.; do Egito Vasconcelos, B.C.; da Silva Pereira, M.A. Prevalence and predictive factors of dental anxiety in Brazilian adolescents. J. Dent. Child. 2013, 80, 41–46. [Google Scholar]
- Bedi, R.; Sutcliffe, P.; Donnan, P.T.; McConnachie, J. The prevalence of dental anxiety in a group of 13- and 14-year-old Scottish children. Int. J. Paediatr. Dent. 1992, 2, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Armfield, J.M.; Spencer, A.J.; Stewart, J.F. Dental fear in Australia: Who’s afraid of the dentist? Aust. Dent. J. 2006, 51, 78–85. [Google Scholar] [CrossRef]
- Thomson, W.M.; Stewart, J.F.; Carter, K.D.; Spencer, A.J. Dental anxiety among Australians. Int. Dent. J. 1996, 46, 320–324. [Google Scholar]
- Schwarz, E.; Birn, H. Dental anxiety in Danish and Chinese adults—A cross-cultural perspective. Soc. Sci. Med. 1995, 41, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Zinke, A.; Hannig, C.; Berth, H. Comparing oral health in patients with different levels of dental anxiety. Head Face Med. 2018, 14, 25. [Google Scholar] [CrossRef]
- Haworth, S.; Dudding, T.; Waylen, A.; Thomas, S.J.; Timpson, N.J. Is dental general anaesthesia in childhood a risk factor for caries and anxiety? Br. Dent. J. 2017, 222, 299–304. [Google Scholar] [CrossRef]
- Klepac, R.K.; Dowling, J.; Hauge, G. Characteristics of clients seeking therapy for the reduction of dental avoidance: Reactions to pain. J. Behav. Ther. Exp. Psychiatry 1982, 13, 293–300. [Google Scholar] [CrossRef]
- Ramos-Jorge, J.; Marques, L.S.; Homem, M.A.; Paiva, S.M.; Ferreira, M.C.; Oliveira Ferreira, F.; Ramos-Jorge, M.L. Degree of dental anxiety in children with and without toothache: Prospective assessment. Int. J. Paediatr. Dent. 2013, 23, 125–130. [Google Scholar] [CrossRef]
- Abanto, J.; Carvalho, T.S.; Mendes, F.M.; Wanderley, M.T.; Bönecker, M.; Raggio, D.P. Impact of oral diseases and disorders on oral health-related quality of life of preschool children. Community Dent. Oral Epidemiol. 2011, 39, 105–114. [Google Scholar] [CrossRef]
- DiMaggio, C.; Sun, L.; Li, G. Early childhood exposure to anesthesia and risk of developmental and behavioral disorders in a sibling birth cohort. Anesth. Analg. 2011, 113, 1143. [Google Scholar] [CrossRef]
- Jankauskiene, B.; Virtanen, J.I.; Kubilius, R.; Narbutaite, J. Oral health-related quality of life after dental general anaesthesia treatment among children: A follow-up study. BMC Oral Health 2014, 14, 81. [Google Scholar] [CrossRef]
- Liu, Y.Q.; Zhang, Q.; Wang, Y.; Qu, X.; Zou, J. Evaluation of therapeutic effect and health economics of general anesthesia and routine outpatient dental treatment in children with severe early child caries. Hua Xi Kou Qiang Yi Xue Za Zhi Huaxi Kouqiang Yixue Zazhi West China J. Stomatol. 2021, 39, 703–708. [Google Scholar]
- Kanellis, M.J.; Damiano, P.C.; Momany, E.T. Medicaid costs associated with the hospitalization of young children for restorative dental treatment under general anesthesia. J. Public Health Dent. 2000, 60, 28–32. [Google Scholar] [CrossRef]
- Lee, H.H.; Milgrom, P.; Starks, H.; Burke, W. Trends in death associated with pediatric dental sedation and general anesthesia. Pediatr. Anesth. 2013, 23, 741–746. [Google Scholar] [CrossRef]
- Almeida, A.G.; Roseman, M.M.; Sheff, M.; Huntington, N.; Hughes, C.V. Future caries susceptibility in children with early childhood caries following treatment under general anesthesia. Pediatr. Dent. 2000, 22, 302–306. [Google Scholar]
- Kakaounaki, E.; Tahmassebi, J.F.; Fayle, S.A. Repeat general anaesthesia, a 6-year follow up. Int. J. Paediatr. Dent. 2011, 21, 126–131. [Google Scholar] [CrossRef]
- Berkowitz, R.; Moss, M.; Billings, R.; Weinstein, P. Clinical outcomes for nursing caries treated using general anesthesia. ASDC J. Dent. Child. 1997, 64, 210–211, 228. [Google Scholar]
- Foster, T.; Perinpanayagam, H.; Pfaffenbach, A.; Certo, M. Recurrence of early childhood caries after comprehensive treatment with general anesthesia and follow-up. J. Dent. Child. 2006, 73, 25–30. [Google Scholar]
- Campbell, C.; Soldani, F.; Busuttil-Naudi, A.; Chadwick, B. Update of Non-pharmacological behaviour management guideline. Br. Soc. Paediatr. Dent. 2011, 1–37. [Google Scholar]
- Vishwakarma, A.P.; Bondarde, P.A.; Patil, S.B.; Dodamani, A.S.; Vishwakarma, P.Y.; Mujawar, S.A. Effectiveness of two different behavioral modification techniques among 5–7-year-old children: A randomized controlled trial. J. Indian Soc. Pedod. Prev. Dent. 2017, 35, 143–149. [Google Scholar] [CrossRef]
- Patil, V.H.; Vaid, K.; Gokhale, N.S.; Shah, P.; Mundada, M.; Hugar, S.M. Evaluation of effectiveness of dental apps in management of child behaviour: A pilot study. Int. J. Pedod. Rehabil. 2017, 2, 14. [Google Scholar]
- Fakhruddin, K.S.; Gorduysus, M.O. Effectiveness of audiovisual distraction eyewear and computerized delivery of anesthesia during pulp therapy of primary molars in phobic child patients. Eur. J. Dent. 2015, 9, 470–475. [Google Scholar] [CrossRef]
- Oliveira, N.; Santos, J.; Linhares, M. Audiovisual distraction for pain relief in paediatric inpatients: A crossover study. Eur. J. Pain 2017, 21, 178–187. [Google Scholar] [CrossRef]
- Al-Khotani, A.; Bello, L.A.A.; Christidis, N. Effects of audiovisual distraction on children’s behaviour during dental treatment: A randomized controlled clinical trial. Acta Odontol. Scand. 2016, 74, 494–501. [Google Scholar] [CrossRef] [PubMed]
- Havelka, C.; McTigue, D.; Wilson, S.; Odom, J. The influence of social status and prior explanation on parental attitudes toward behavior management techniques. Pediatr. Dent. 1992, 14, 376. [Google Scholar]
- Wong, D.; Perez-Spiess, S.; Julliard, K. Attitudes of Chinese parents toward the oral health of their children with caries: A qualitative study. Pediatr. Dent. 2005, 27, 505–512. [Google Scholar]
- Machen, J.B. Parental acceptance of pediatric dentistry behavior management techniques. Pediatr. Dent. 1984, 6, 193. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef]
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; Welch, V.A.; Higgins, J.P.; Thomas, J. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 2019, ED000142. [Google Scholar] [CrossRef] [PubMed]
- Buchanan, H.; Niven, N. Validation of a Facial Image Scale to assess child dental anxiety. Int. J. Paediatr. Dent. 2002, 12, 47–52. [Google Scholar] [CrossRef]
- Venham, L.L.; Gaulin-Kremer, E. A self-report measure of situational anxiety for young children. Pediatr. Dent. 1979, 1, 91–96. [Google Scholar] [PubMed]
- Krikken, J.B.; van Wijk, A.J.; ten Cate, J.M.; Veerkamp, J.S. Measuring dental fear using the CFSS-DS. Do children and parents agree? Int. J. Paediatr. Dent. 2013, 23, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Howard, K.E.; Freeman, R. Reliability and validity of a faces version of the Modified Child Dental Anxiety Scale. Int. J. Paediatr. Dent. 2007, 17, 281–288. [Google Scholar] [CrossRef] [PubMed]
- Venham, L.L.; Gaulin-Kremer, E.; Munster, E.; Bengston-Audia, D.; Cohan, J. Interval rating scales for children’s dental anxiety and uncooperative behavior. Pediatr. Dent. 1980, 2, 195–202. [Google Scholar] [PubMed]
- Sadana, G.; Grover, R.; Mehra, M.; Gupta, S.; Kaur, J.; Sadana, S. A novel Chotta Bheem–Chutki scale for dental anxiety determination in children. J. Int. Soc. Prev. Community Dent. 2016, 6, 200. [Google Scholar] [PubMed]
- Miró, J.; Huguet, A. Evaluation of reliability, validity, and preference for a pediatric pain intensity scale: The Catalan version of the faces pain scale—Revised. Pain 2004, 111, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Corah, N.L.; Gale, E.N.; Illig, S.J. Assessment of a dental anxiety scale. J. Am. Dent. Assoc. 1978, 97, 816–819. [Google Scholar] [CrossRef]
- Garra, G.; Singer, A.J.; Taira, B.R.; Chohan, J.; Cardoz, H.; Chisena, E.; Thode, H.C., Jr. Validation of the Wong-Baker FACES pain rating scale in pediatric emergency department patients. Acad. Emerg. Med. 2010, 17, 50–54. [Google Scholar] [CrossRef] [PubMed]
- Verma, N.; Gupta, A.; Garg, S.; Dogra, S.; Joshi, S.; Vaid, P. Outcome of Conventional versus Digital Mode of Behaviour Modification with or without Maternal Presence in Paediatric Dental Patients—A Pilot Study. J. Clin. Diagn. Res. 2022, 16, ZC66–ZC70. [Google Scholar] [CrossRef]
- Gift, A.G. Visual analogue scales: Measurement of subjective phenomena. Nurs. Res. 1989, 38, 286–287. [Google Scholar] [CrossRef] [PubMed]
- Galamb, D.; Lenkey, Á.; Oláh, A.; Máth, J.; Márton, I.; Alberth, M. Objective and subjective measurements for assessing dental fear in adolescents: A pilot study. Changes 2017, 20, 10. [Google Scholar]
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M. Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; Wiley: Hoboken, NJ, USA, 2019; Volume 10, ISBN 9781119536604. [Google Scholar]
- Higgins, J.; Churchill, R.; Chandler, J.; Cumpston, M. Cochrane Handbook for Systematic Reviews of Interventions Version 5.2. 0 (updated June 2017). The Cochrane Collaboration, 2017. Available online: https://training.cochrane.org/handbook (accessed on 12 February 2024).
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Jaeschke, R.; Guyatt, G.H.; Dellinger, P.; Schünemann, H.; Levy, M.M.; Kunz, R.; Norris, S.; Bion, J. Use of GRADE grid to reach decisions on clinical practice guidelines when consensus is elusive. BMJ 2008, 337, a744. [Google Scholar] [CrossRef] [PubMed]
- Zachary, R.A.; Friedlander, S.; Huang, L.N.; Silverstein, S.; Leggott, P. Effects of stress-relevant and-irrelevant filmed modeling on children’s responses to dental treatment. J. Pediatr. Psychol. 1985, 10, 383–401. [Google Scholar] [CrossRef] [PubMed]
- Greenbaum, P.E.; Turner, C.; Cook, E.W.; Melamed, B.G. Dentists’ voice control: Effects on children’s disruptive and affective behavior. Health Psychol. 1990, 9, 546. [Google Scholar] [CrossRef] [PubMed]
- McMurray, N.E.; Lucas, J.O.; Arbres-Duprey, V.; Wright, F.A. The effects of mastery and coping models on dental stress in young children. Aust. J. Psychol. 1985, 37, 65–70. [Google Scholar] [CrossRef]
- Peretz, B.; Gluck, G. Magic trick: A behavioural strategy for the management of strong-willed children. Int. J. Paediatr. Dent. 2005, 15, 429–436. [Google Scholar] [CrossRef]
- Marwah, N.; Prabhakar, A.; Raju, O. Music distraction-its efficacy in management of anxious pediatric dental patients. J. Indian Soc. Pedod. Prev. Dent. 2005, 23, 168–170. [Google Scholar] [CrossRef]
- Howard, K.E.; Freeman, R. An evaluation of the PALS after treatment modelling intervention to reduce dental anxiety in child dental patients. Int. J. Paediatr. Dent. 2009, 19, 233–242. [Google Scholar] [CrossRef]
- Farhat-McHayleh, N.; Harfouche, A.; Souaid, P. Techniques for managing behaviour in pediatric dentistry: Comparative study of live modelling and tell-show-do based on children’s heart rates during treatment. J. Can. Dent. Assoc. 2009, 75, 283a–283f. [Google Scholar]
- Xia, Y.-H.; Song, Y.-R. Usage of a reward system for dealing with pediatric dental fear. Chin. Med. J. 2016, 129, 1935–1938. [Google Scholar] [CrossRef]
- Shetty, V.; Suresh, L.R.; Hegde, A.M. Effect of virtual reality distraction on pain and anxiety during dental treatment in 5 to 8 year old children. J. Clin. Pediatr. Dent. 2019, 43, 97–102. [Google Scholar] [CrossRef]
- Serra-Negra, J.; Abreu, M.; Flores-Mendoza, C.; Brant, M.; Auad, S. The reassuring role of music associated with the personality traits of children during dental care: A randomized clinical trial. Eur. Arch. Paediatr. Dent. 2019, 20, 441–449. [Google Scholar] [CrossRef]
- Rank, R.C.I.C.; Rank, M.S.; Vilela, J.E.R.; Ogawa, W.N.; Correa, M.S.N.P. Dental anxiety and behavior in young children undergoing different distraction techniques. Pesqui. Bras. Odontopediatria Clínica Integr. 2017, 17, 1–11. [Google Scholar]
- Rank, R.; Vilela, J.; Rank, M.; Ogawa, W.; Imparato, J.C.P. Effect of awards after dental care in children’s motivation. Eur. Arch. Paediatr. Dent. 2019, 20, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Jorge, M.; Ramos-Jorge, J.; Vieira de Andrade, R.; Marques, L. Impact of exposure to positive images on dental anxiety among children: A controlled trial. Eur. Arch. Paediatr. Dent. 2011, 12, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Carrasco, A.; Butrón-Téllez Girón, C.; Sanchez-Armass, O.; Pierdant-Pérez, M. Effectiveness of hypnosis in combination with conventional techniques of behavior management in anxiety/pain reduction during dental anesthetic infiltration. Pain Res. Manag. 2017, 2017, 1434015. [Google Scholar] [CrossRef]
- Nuvvula, S.; Alahari, S.; Kamatham, R.; Challa, R. Effect of audiovisual distraction with 3D video glasses on dental anxiety of children experiencing administration of local analgesia: A randomised clinical trial. Eur. Arch. Paediatr. Dent. 2015, 16, 43–50. [Google Scholar] [CrossRef]
- Niharika, P.; Reddy, N.V.; Srujana, P.; Srikanth, K.; Daneswari, V.; Geetha, K.S. Effects of distraction using virtual reality technology on pain perception and anxiety levels in children during pulp therapy of primary molars. J. Indian Soc. Pedod. Prev. Dent. 2018, 36, 364–369. [Google Scholar] [CrossRef]
- Navit, S.; Johri, N.; Khan, S.A.; Singh, R.K.; Chadha, D.; Navit, P.; Sharma, A.; Bahuguna, R. Effectiveness and comparison of various audio distraction aids in management of anxious dental paediatric patients. J. Clin. Diagn. Res. 2015, 9, ZC05. [Google Scholar] [CrossRef]
- Mitrakul, K.; Asvanund, Y.; Arunakul, M.; Paka-Akekaphat, S. Effect of audiovisual eyeglasses during dental treatment in 5–8 year-old children Introduction. Eur. J. Paediatr. Dent. 2015, 16, 26418930. [Google Scholar]
- Khandelwal, D.; Kalra, N.; Tyagi, R.; Khatri, A.; Gupta, K. Control of anxiety in pediatric patients using “Tell Show Do” method and audiovisual distraction. J. Contemp. Dent. Pract. 2018, 19, 1058–1064. [Google Scholar]
- Khan, S.; Rao, D.; Jasuja, P.; Malik, S.; Al Yami, S.; Al Makrami, M. Passive Distraction: A Technique to Maintain Children’s Behavior Undergoing Dental Treatment. Indo Am. J. Pharm. Sci. 2019, 6, 4043–4048. [Google Scholar]
- Karekar, P.; Bijle, M.N.; Walimbe, H. Effect of three behavior guidance techniques on anxiety indicators of children undergoing diagnosis and preventive dental care. J. Clin. Pediatr. Dent. 2019, 43, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Kamel, D.O.; Wahba, N.A.; Talaat, D.M. Comparison between positive dental images and neutral images in managing anticipatory anxiety of children. J. Clin. Pediatr. Dent. 2017, 41, 116–119. [Google Scholar] [CrossRef]
- Huet, A.; Lucas-Polomeni, M.-M.; Robert, J.-C.; Sixou, J.-L.; Wodey, E. Hypnosis and dental anesthesia in children: A prospective controlled study. Int. J. Clin. Exp. Hypn. 2011, 59, 424–440. [Google Scholar] [CrossRef] [PubMed]
- Hine, J.F.; Hajek, R.T.; Roberts, H.J.; Allen, K.D. Decreasing disruptive behaviour during routine dental visits: A video modelling intervention for young children. Int. Dent. J. 2019, 69, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Ghadimi, S.; Estaki, Z.; Rahbar, P.; Shamshiri, A. Effect of visual distraction on children’s anxiety during dental treatment: A crossover randomized clinical trial. Eur. Arch. Paediatr. Dent. 2018, 19, 239–244. [Google Scholar] [CrossRef]
- Garrocho-Rangel, A.; Ibarra-Gutiérrez, E.; Rosales-Bérber, M.; Esquivel-Hernández, R.; Esparza-Villalpando, V.; Pozos-Guillén, A. A video eyeglasses/earphones system as distracting method during dental treatment in children: A crossover randomised and controlled clinical trial. Eur. J. Paediatr. Dent. 2018, 19, 74–79. [Google Scholar]
- Boka, V.; Arapostathis, K.; Charitoudis, G.; Veerkamp, J.; van Loveren, C.; Kotsanos, N. A study of parental presence/absence technique for child dental behaviour management. Eur. Arch. Paediatr. Dent. 2017, 18, 405–409. [Google Scholar] [CrossRef]
- Avisa, P.; Kamatham, R.; Vanjari, K.; Nuvvula, S. Effectiveness of acupressure on dental anxiety in children. Pediatr. Dent. 2018, 40, 177–183. [Google Scholar]
- Asvanund, Y.; Mitrakul, K.; Juhong, R.-O.; Arunakul, M. Effect of audiovisual eyeglasses during local anesthesia injections in 5-to 8-year-old children. Quintessence Int. 2015, 46, 513. [Google Scholar]
- Aminabadi, N.A.; Vafaei, A.; Erfanparast, L.; Oskouei, S.G.; Jamali, Z. Impact of pictorial story on pain perception, situational anxiety and behavior in children: A cognitive-behavioral schema. J. Clin. Pediatr. Dent. 2011, 36, 127–132. [Google Scholar] [CrossRef]
- Al-Namankany, A.; Petrie, A.; Ashley, P. Video modelling and reducing anxiety related to dental injections—A randomised clinical trial. Br. Dent. J. 2014, 216, 675–679. [Google Scholar] [CrossRef] [PubMed]
- Alnamankany, A. Video modelling and dental anxiety in children. A randomised clinical trial. Eur. J. Paediatr. Dent. 2019, 20, 242–246. [Google Scholar]
- Al-Halabi, M.N.; Bshara, N.; AlNerabieah, Z. Effectiveness of audio visual distraction using virtual reality eyeglasses versus tablet device in child behavioral management during inferior alveolar nerve block. Anaesth. Pain Intensive Care 2018, 22, 55–61. [Google Scholar]
- Afshar, H.; Nakhjavani, Y.B.; Mahmoudi-Gharaei, J.; Paryab, M.; Zadhoosh, S. The effect of parental presence on the 5 year-old children’s anxiety and cooperative behavior in the first and second dental visit. Iran. J. Pediatr. 2011, 21, 193. [Google Scholar] [PubMed]
- Mungara, J.; Injeti, M.; Joseph, E.; Elangovan, A.; Sakthivel, R.; Selvaraju, G. Child’s dental fear: Cause related factors and the influence of audiovisual modeling. J. Indian Soc. Pedod. Prev. Dent. 2013, 31, 215–220. [Google Scholar] [PubMed]
- Abbasi, H.; Saqib, M.; Jouhar, R.; Lal, A.; Ahmed, N.; Ahmed, M.A.; Alam, M.K. The efficacy of little lovely dentist, dental song, and tell-show-do techniques in alleviating dental anxiety in paediatric patients: A clinical trial. BioMed Res. Int. 2021, 2021, 1119710. [Google Scholar] [CrossRef]
- Aditya, P.; Prasad, M.G.; Nagaradhakrishna, A.; Raju, N.S.; Babu, D.N. Comparison of effectiveness of three distraction techniques to allay dental anxiety during inferior alveolar nerve block in children: A randomized controlled clinical trial. Heliyon 2021, 7, e08092. [Google Scholar] [CrossRef] [PubMed]
- AlDhelai, T.A.; Khalil, A.M.; Elhamouly, Y.; Dowidar, K.M. Influence of active versus passive parental presence on the behavior of preschoolers with different intelligence levels in the dental operatory: A randomized controlled clinical trial. BMC Oral Health 2021, 21, 420. [Google Scholar] [CrossRef]
- Alsaadoon, A.M.; Sulimany, A.M.; Hamdan, H.M.; Murshid, E.Z. The use of a dental storybook as a dental anxiety reduction medium among pediatric patients: A randomized controlled clinical trial. Children 2022, 9, 328. [Google Scholar] [CrossRef] [PubMed]
- Alshatrat, S.M.; Sabarini, J.M.; Hammouri, H.M.; Al-Bakri, I.A.; Al-Omari, W.M. Effect of immersive virtual reality on pain in different dental procedures in children: A pilot study. Int. J. Paediatr. Dent. 2022, 32, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Asokan, S.; Priya, P.G.; Natchiyar, S.N.; Elamathe, M. Effectiveness of distraction techniques in the management of anxious children–A randomized controlled pilot trial. J. Indian Soc. Pedod. Prev. Dent. 2020, 38, 407–412. [Google Scholar] [PubMed]
- Azher, U.; Srinath, S.K.; Nayak, M. Effectiveness of bubble breath play therapy in the dental management of anxious children: A pilot study. J. Contemp. Dent. Pract. 2020, 21, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Bahrololoomi, Z.; Sadeghiyeh, T.; Rezaei, M.; Maghsoudi, N. The Effect of Breathing Exercise Using Bubble Blower on Anxiety and Pain during Inferior Alveolar Nerve Block in Children Aged 7 to 10 Years: A Crossover Randomized Clinical Trial. Pain Res. Manag. 2022, 2022, 7817267. [Google Scholar] [CrossRef] [PubMed]
- Buldur, B.; Candan, M. Does virtual reality affect children’s dental anxiety, pain, and behaviour? a randomised, placebo-controlled, cross-over trial. Pesqui. Bras. Odontopediatria Clínica Integr. 2020, 21, e0082. [Google Scholar] [CrossRef]
- CustÓdio, N.B.; Cademartori, M.G.; Azevedo, M.S.; Mendes, M.d.A.; Schardozim, L.R.; Costa, L.R.d.R.S.d.; Goettems, M.L. Efficacy of audiovisual distraction using eyeglasses during dental care: A randomized clinical trial. Braz. Oral Res. 2021, 35, e26. [Google Scholar] [CrossRef]
- Du, Q.; Ma, X.; Wang, S.; Zhou, S.; Luo, C.; Tian, K.; Fei, W.; Liu, X. A digital intervention using virtual reality helmets to reduce dental anxiety of children under local anesthesia and primary teeth extraction: A randomized clinical trial. Brain Behav. 2022, 12, e2600. [Google Scholar] [CrossRef]
- Ghaderi, F.; Solhjou, N. The effects of lavender aromatherapy on stress and pain perception in children during dental treatment: A randomized clinical trial. Complement. Ther. Clin. Pract. 2020, 40, 101182. [Google Scholar] [CrossRef]
- Gómez-Polo, C.; Vilches, A.-A.; Ribas, D.; Castaño-Séiquer, A.; Montero, J. Behaviour and anxiety management of paediatric dental patients through virtual reality: A randomised clinical trial. J. Clin. Med. 2021, 10, 3019. [Google Scholar] [CrossRef]
- Guinot, F.; Mercadé, M.; Oprysnyk, L.; Veloso, A.; Boj, J. Comparison of active versus passive audiovisual distraction tools on children’s behaviour, anxiety and pain inpaediatric dentistry: A randomised crossover clinical trial. Eur. J. Paediatr. Dent. 2021, 22, 230–236. [Google Scholar]
- Kharouba, J.; Peretz, B.; Blumer, S. The effect of television distraction versus Tell-Show-Do as behavioral management techniques in children undergoing dental treatments. Quintessence Int. 2020, 51, 486–494. [Google Scholar] [PubMed]
- Kumari, S.; Bahuguna, R.; Garg, N.; Yeluri, R. Immersive and non-immersive virtual reality distraction on pain perception to intraoral injections. J. Clin. Pediatr. Dent. 2021, 45, 389–394. [Google Scholar] [CrossRef]
- Padminee, K.; Hemalatha, R.; Shankar, P.; Senthil, D.; Jayakaran, T.G.; Kabita, S. Effectiveness of biofeedback relaxation and audio-visual distraction on dental anxiety among 7- to 12-year-old children while administering local anaesthesia: A randomized clinical trial. Int. J. Paediatr. Dent. 2022, 32, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Pande, P.; Rana, V.; Srivastava, N.; Kaushik, N. Effectiveness of different behavior guidance techniques in managing children with negative behavior in a dental setting: A randomized control study. J. Indian Soc. Pedod. Prev. Dent. 2020, 38, 259–265. [Google Scholar]
- Ran, L.; Zhao, N.; Fan, L.; Zhou, P.; Zhang, C.; Yu, C. Application of virtual reality on non-drug behavioral management of short-term dental procedure in children. Trials 2021, 22, 562. [Google Scholar] [CrossRef]
- Sabherwal, P.; Kalra, N.; Tyagi, R.; Khatri, A.; Srivastava, S. Hypnosis and progressive muscle relaxation for anxiolysis and pain control during extraction procedure in 8–12-year-old children: A randomized control trial. Eur. Arch. Paediatr. Dent. 2021, 22, 823–832. [Google Scholar] [CrossRef]
- Shekhar, S.; Suprabha, B.; Shenoy, R.; Rao, A.; Rao, A. Effect of active and passive distraction techniques while administering local anaesthesia on the dental anxiety, behaviour and pain levels of children: A randomised controlled trial. Eur. Arch. Paediatr. Dent. 2022, 23, 417–427. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Chung, H.; Sohn, S.; Kinn, Y. Effects of psychological behaviour management programme on dental fear and anxiety in children: A randomised controlled clinical trial. Eur. J. Paediatr. Dent. 2020, 21, 287–291. [Google Scholar]
- Thakkar, T.; Naik, S.; Dixit, U. Assessment of dental anxiety in children between 5 and 10 years of age in the presence of a therapy dog: A randomized controlled clinical study. Eur. Arch. Paediatr. Dent. 2021, 22, 459–467. [Google Scholar] [CrossRef]
- Thosar, N.R.; Bane, S.P.; Deulkar, P.V.; Deshpande, M.A.; Gupta, S.; Deshpande Sr, M.A. Effectiveness of two different behavior modification techniques for anxiety reduction in children. Cureus 2022, 14, e28141. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhang, J.; Sun, D. Randomized Crossover Study of Auricular Plaster Therapy to Relieve Dental Anxiety in Children. Front. Psychiatry 2022, 13, 862575. [Google Scholar] [CrossRef] [PubMed]
- Zhu, M.; Yu, H.; Xie, B.; Li, H.; He, Q.; Li, H.; Su, J.; Li, X. Experiential learning for children’s dental anxiety: A cluster randomized trial. BMC Oral Health 2020, 20, 216. [Google Scholar] [CrossRef]
- Obadiah, I.; Subramanian, E. Effect of a Relaxation Training Exercise on Behaviour, Anxiety and Pain During Administration of Intra-Oral Local Anaesthesia in Children of Age 6 to 12 years: Randomized Controlled Trial. J. Res. Med. Dent. Sci. 2020, 8, 364–370. [Google Scholar]
- Babu, G.; Mani, G. Effect of audio and audio-visual distraction aids in reducing anxiety during pedodontic care. Bioinformation 2020, 16, 1007–1012. [Google Scholar]
- Cox, I.; Krikken, J.; Veerkamp, J. Influence of parental presence on the child’s perception of, and behaviour, during dental treatment. Eur. Arch. Paediatr. Dent. 2011, 12, 200–204. [Google Scholar] [CrossRef] [PubMed]
- Aslan, A.; Tüzüner, T.; Baygın, Ö.; Yılmaz, N.; Sagdıc, S. Reliability and validity of the Turkish version of the Abeer Children Dental Anxiety Scale (ACDAS). Contemp. Pediatr. 2021, 2, 142–150. [Google Scholar] [CrossRef]
- Prabhakar, A.; Marwah, N.; Raju, O. A comparison between audio and audiovisual distraction techniques in managing anxious pediatric dental patients. J. Indian Soc. Pedod. Prev. Dent. 2007, 25, 177–182. [Google Scholar]
- Sinha, M.; Christopher, N.C.; Fenn, R.; Reeves, L. Evaluation of nonpharmacologic methods of pain and anxiety management for laceration repair in the pediatric emergency department. Pediatrics 2006, 117, 1162–1168. [Google Scholar] [CrossRef]
- Wang, Z.-X.; Sun, L.-H.; Chen, A.-P. The efficacy of non-pharmacological methods of pain management in school-age children receiving venepuncture in a paediatric department: A randomized controlled trial of audiovisual distraction and routine psychological intervention. Swiss Med. Wkly. 2008, 138, 579–584. [Google Scholar] [CrossRef]
- Wismeijer, A.A.; Vingerhoets, A.J. The use of virtual reality and audiovisual eyeglass systems as adjunct analgesic techniques: A review of the literature. Ann. Behav. Med. 2005, 30, 268–278. [Google Scholar] [CrossRef]
- Sharar, S.R.; Carrougher, G.J.; Nakamura, D.; Hoffman, H.G.; Blough, D.K.; Patterson, D.R. Factors influencing the efficacy of virtual reality distraction analgesia during postburn physical therapy: Preliminary results from 3 ongoing studies. Arch. Phys. Med. Rehabil. 2007, 88, S43–S49. [Google Scholar] [CrossRef] [PubMed]
- Bryson, S. Virtual reality in scientific visualization. Commun. ACM 1996, 39, 62–71. [Google Scholar] [CrossRef]
- Carl, E.; Stein, A.T.; Levihn-Coon, A.; Pogue, J.R.; Rothbaum, B.; Emmelkamp, P.; Asmundson, G.J.; Carlbring, P.; Powers, M.B. Virtual reality exposure therapy for anxiety and related disorders: A meta-analysis of randomized controlled trials. J. Anxiety Disord. 2019, 61, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Dahlander, A.; Soares, F.; Grindefjord, M.; Dahllöf, G. Factors associated with dental fear and anxiety in children aged 7 to 9 years. Dent. J. 2019, 7, 68. [Google Scholar] [CrossRef]
- American Academy of Pediatric Dentistry. The Reference Manual of Pediatric Dentistry; American Academy of Pediatric Dentistry: Chicago, IL, USA, 2020; pp. 243–247. [Google Scholar]
- Nunn, J.; Foster, M.; Master, S.; Greening, S. British Society of Paediatric Dentistry: A policy document on consent and the use of physical intervention in the dental care of children. Int. J. Paediatr. Dent. 2008, 18, 39–46. [Google Scholar] [CrossRef]
- Raadal, M.; Strand, G.V.; Amarante, E.C.; Kvale, G. Relationship between caries prevalence at 5 years of age and dental anxiety at 10. Eur. J. Paediatr. Dent. 2002, 3, 22–26. [Google Scholar]
- Von Baeyer, C.L.; Forsyth, S.J.; Stanford, E.A.; Watson, M.; Chambers, C.T. Response biases in preschool children’s ratings of pain in hypothetical situations. Eur. J. Pain 2009, 13, 209–213. [Google Scholar] [CrossRef] [PubMed]
- Ten Berge, M.; Veerkamp, J.S.; Hoogstraten, J.; Prins, P.J. Behavioural and emotional problems in children referred to a centre for special dental care. Community Dent. Oral Epidemiol. 1999, 27, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Eli, I.; Uziel, N.; Blumensohn, R.; Baht, R. Modulation of dental anxiety—The role of past experiences, psychopathologic traits and individual attachment patterns. Br. Dent. J. 2004, 196, 689–694. [Google Scholar] [CrossRef] [PubMed]
- Townend, E.; Dimigen, G.; Fung, D. A clinical study of child dental anxiety. Behav. Res. Ther. 2000, 38, 31–46. [Google Scholar] [CrossRef] [PubMed]
- Yon, M.J.Y.; Chen, K.J.; Gao, S.S.; Duangthip, D.; Lo, E.C.M.; Chu, C.H. An introduction to assessing dental fear and anxiety in children. Healthcare 2020, 8, 86. [Google Scholar] [CrossRef]
- Rosenberg, H.M.; Katcher, A.H. Heart rate and physical activity of children during dental treatment. J. Dent. Res. 1976, 55, 648–651. [Google Scholar] [CrossRef]
- Nussbaumer-Streit, B.; Klerings, I.; Dobrescu, A.; Persad, E.; Stevens, A.; Garritty, C.; Kamel, C.; Affengruber, L.; King, V.; Gartlehner, G. Excluding non-English publications from evidence-syntheses did not change conclusions: A meta-epidemiological study. J. Clin. Epidemiol. 2020, 118, 42–54. [Google Scholar] [CrossRef]
| No. | Study (Year and Country) | Study Design, Setting | N Patient; Age Range (Years Old) | Intervention Group | Control Groups | Method of Assessment | Evaluation Time | Outcome |
|---|---|---|---|---|---|---|---|---|
| 1 | Abbasi et al. (2021) PAK [92] | RCT 4 parallel groups, dental clinic | 160; 6–11 | (1) Mobile application “little lovely dentist” (2) You-tube “Dental video songs” (3) Tell–show–do | No intervention | (1) Heart rate (2) Facial image scale | Pre-op/post-op | Dental anxiety |
| 2 | Aditya et al. (2021) IND [93] | RCT, 4 parallel groups, dental clinic | 60; 6–9 | (1) Fidget spinner (2) Kaleidoscope (3) VR Distraction | NO distraction | (1) Venham’s picture test (2) Pulse oximeter (3) Pulse rate (4) SpO2 | 6M | Dental anxiety |
| 3 | Afshar et al. (2016) IRN [90] | RCT, 2 (control, study) groups, dental clinic | 67; 5 | (1) Parental presence (2) Parental absence | No control group | (1) HR (2) Venham scale (3) Frankl BRS | Not stated | Dental anxiety |
| 4 | AlDhelai (2021) EGY [94] | RCT, 2 parallel groups, dental clinic | 150; 3–6 | Parental active presence | Parental passive presence | (1) FIS (2) FBRS (3) IQ level | Not stated | Child’s behaviour based on their IQ level |
| 5 | Al-Halabi et al. (2018) SYR [89] | RCT 3 groups, dental clinic | 101; 6–10 | Audio-visual distraction (1) Eyeglass (2) VR box or tablet | Conventional NP-BMT | (1) WBFS (2) HR (3) FLACC-BRS | 6M | Dental anxiety |
| 6 | Al-khotani et al. (2016) SAU [35] | RCT 2 parallel groups, dental clinic | 56; 7–9 | AV distraction | NO intervention | (1) FIS (2) MVARS (3) vital signs (4) BP (3) PR | Pre-op/post-op | Dental anxiety |
| 7 | Al-namankany et al. (2014) UK [87] | RCT 2 parallel groups, dental clinic | 80; 6–12 | Modelling video | OH instruction video | (1) Abeer Children Dental Anxiety Scale (2) VAS | Before watching the video/after watching the video | Dental anxiety |
| 8 | Alnamankany et al. (2019) SAU [88] | RCT 2 parallel groups, hospital | 46; 6–10 | Modelling video | OH instruction video | Abeer Children Dental Anxiety Scale | Before watching the video/after watching the video | Dental anxiety |
| 9 | Alsaadoon et al. (2022) SAU [95] | RCT 2 parallel groups, dental clinic | 93; 6–8 | Received storybook | No intervention | (1) CFSS-DS (2) VCAS (3) FBRS | Pre-op/post-op | Dental anxiety |
| 10 | Alshatrat et al. (2020) JOR [96] | RCT, 2 groups, dental clinic | 54; 5–12 | VR distraction | No intervention | (1) VAS (2) Wong–Baker faces (3) FLACC scale | Not stated | - Dental pain - Dental anxiety |
| 11 | Aminabadi et al. (2011) IRN [86] | RCT 2 parallel groups, dental clinic | 80; 6–7 | Pictorial story (dentist) | Pictorial story (barbershop) | (1) Wong–Baker faces (2) MCDAS scale (3) Sound, eye and motor scale | Pre-op/post-op | - Dental pain - Dental anxiety |
| 12 | Asokan et al. (2022) IND [97] | RCT, 3 parallel groups, school | 60; 4–5 | 1st group: magic trick distraction 2nd group: mobile dental game distraction | 3rd group: TSD | Chotta Bheem–Chutki scale | Post-op | Dental anxiety |
| 13 | Asvanund et al. (2015) THA [85] | RCT, split mouth crossover, dental clinic | 49; 5–8 | 1st visit: not wearing AV eyeglass 2nd visit: wearing AV eyeglass | 1st visit: wearing AV eyeglass 2nd visit: not wearing AV eyeglass | (1) Faces Pain Scale-Revised (2) Heart rate (3) FLACC | 2 visits, 1–4 weeks apart | Dental pain |
| 14 | Avisa et al. (2018) IND [84] | RCT 3 parallel groups, dental clinic | 210; 8–12 | (1) Acupressure (2) Sham | (1)No intervention | (1) MCDAS scale (2) Frankl (3) Pulse rate | Pre-op/post-op | Dental anxiety |
| 15 | Azher et al. (2020) IND [98] | RCT 2 parallel groups, dental clinic | 48; 6–8 | Bubble breath play therapy | Tell–show–do | (1) Pulse rate (2) Venham’s anxiety and behaviour rating scale | Pre-op/post-op | Dental anxiety |
| 16 | Bahrololoomi (2022) IRL [99] | RCT 2 crossover groups, dental clinic | 35; 7–10 | 1st group: with breathing exercise 2nd group: No breathing exercise | 1st group: No breathing exercise 2nd group: with breathing exercise | (1) FIS (2) BP (3) FLACC (4) WBFPS | Not stated | Dental anxiety |
| 17 | Boka et al. (2017) GRC [83] | RCT 2 groups, dental clinic | 61; 3–8 | Parental presence/absence + conventional NP-BMT | No PPA + conventional NP-BMT | Frankl scale | Pre-op/post-op | Childs’ behaviour |
| 18 | Bulder et al. (2020) TUR [100] | RCT 2 crossover (placebo control) groups, dental clinic | 76; 7–11 | 1st group: - 1st visit ‘attention placebo control’ (control) - 2nd visit ‘VR’ (intervention) | 2nd group: - 1st visit ‘VR’ (intervention)’ - 2nd visit ‘attention placebo control’ (control) | (1) CFSS-DS (2) FIS (3) HR | Pre-op/post-op | - Dental anxiety - Dental pain - Child’s behaviour |
| 19 | Custodio et al. (2021) BRA south [101] | RCT 2, dental clinic | 44; 6–9 | AV eyeglasses distraction | Conventional NP-BMT | (1) VAS (2) FLACC (3) HR (4) FPS-R scale | Pre-op/post-op | - Child’s behaviour - Dental anxiety - Dental pain - Behaviour - Body movement - Pain perception |
| 20 | DU et al. (2022) CHN [102] | RCT 2 groups, dental clinic | 86; 4–9 | VR relaxation | Traditional NP-BMT | (1) Modified CFSS-DS (2) Wong–Baker faces (3) Houpt scale (4) Simulator sickness questionnaire | Not stated | - Dental anxiety - Pain perception |
| 21 | Farhat-McHayleh et al. (2009) LBN [63] | RCT 3 parallel groups, dental clinic | 155; 5–9 | Group 1&2 ‘Live modeling’ | 3rd Group: Tell–show–do | HR | Not stated | - Dental anxiety - Which of the child’s 2 parents represented the model most suitable for live modeling |
| 22 | Garrocho-Rangel et al. (2018) Mex [82] | RCT 1 crossover group, dental clinic | 40; 5–8 | Interventional dental visit ‘Video eyeglasses/earphones system distraction’ | Control dental visit ‘Tradition non-aversive behaviour management’ | (1) FLACC (2) HR (3) O2 saturation | Two dental sessions | - Dental anxiety - Pain perception |
| 23 | Ghaderi et al. (2020) IRN [103] | RCT 1 crossover group, dental clinic | 24; 7–9 | 1st group: - 1st visit ‘treated with no lavender (control)’ - 2nd visit ‘treated with lavender (intervention)’ | 2nd group: - 1st visit ‘treated with lavender (intervention)’ - 2nd visit ‘no lavender(control)’ | Anxiety: (1) Salivary cortisol (2) PR Pain perception: (1) Face rating scale | Two dental visits | - Dental anxiety - Pain perception |
| 24 | Ghadimi et al. (2018) IRN [81] | RCT 2 crossover groups, dental clinic | 28; 4–5 | 1st group: - 1st visit ‘cartoon distraction (intervention)’ - 2nd visit ‘tell–show–do (control)’ | 2nd group: - 1st visit ‘tell–show–do (control)’ - 2nd visit ‘cartoon distraction (intervention)’ | (1) Venham picture test (2) PR (3) FBRS | Two dental visits | - Dental anxiety - Patient’s behaviour |
| 25 | Gomex-Polo et al. (2021) ESP [104] | RCT 2 parallel groups, dental clinic | 80; 5–10 | VR distraction | No distraction | (1) Facial image scale test (2) Frankl test | Not stated | - Dental anxiety - Patient’s behaviour |
| 26 | Greenbaum (1990) USA [58] | RCT, 2 groups, dental clinic | 40; 3.5–4 | Loud voice during tx | Normal voice during tx | (1) Dental subscale (2) Self-assessment mannequin | Not stated | Dental fear |
| 27 | Guinot (2021) ESP [105] | RCT, crossover | 68; 6–8 | Video game ‘PlayStation’ | Cartoon film | (1) Modified Corah dental anxiety scale (2) Venham picture test (3) Wong–Baker faces scale (4) Frankl scale (5) Heart rate | 10 M | Dental anxiety |
| 28 | Hine et al. (2019) USA [80] | RCT, dental clinic | 40; 3–6 | 4 min Video modeling | 14 min clip of popular children’s cartoon | (1) 15 s partial-interval recording and included physical and vocal disruptions. (2) Likert-type scale | Pre-op/post-op | Disruptive behaviour |
| 29 | Howard et al. (2009) UK [44] | RCT 2 parallel groups, dental clinic | 73; 5–10 | PALS model at the end of each | Motivational rewards | (1) MCDAS (2) DMFT | Not stated | - Dental anxiety - Dental caries |
| 30 | Huet et al. (2011) FRA [79] | RCT 2 parallel groups, dental clinic | 30; 5–12 | Hypnosis | No Hypnosis | (1) Modified Yale scale (2) VAS (3) Modified objective pain score | Over 3M | - Dental anxiety - Pain experience |
| 31 | Kamel et al. (2017) EGY [78] | RCT 2 parallel groups, dental clinic | 60; 4–6 | Positive images of dental treatment | Neutral cartoon images | (1) Frankl rating scale (2) Venham picture test | Not stated | - Dental behaviour - Dental anxiety |
| 32 | Karekar et al. (2019) IND [77] | RCT 3 parallel groups, dental clinic | 63; 7–9 | (1) Live modelling (2) Film modelling | (3) Tell–show–do | (1) FIS (2) HR | Before, during, and after diagnosis/preventive treatment | Dental anxiety |
| 33 | Khan et al. (2019) IND [76] | RCT 2 parallel groups, dental clinic | 100; 4–10 | AV distraction through VR Glasses 3D Box | Normal dental setup (no intervention) | (1) FIS (2) MVARS (3) BP (4) HR | Pre-op/post-op | Dental anxiety |
| 34 | Khandelwal et al. (2018) IND [75] | RCT, 4 groups, dental clinic | 400; 5–8 | (1) AVD (2) TSD + AVD | (1) No intervention (2) Tell–show–do | (1) FIS (2) VPT (3) BP (4) HR (5) SpO2 | Before, during, and after Tx | Dental anxiety |
| 35 | Kharouba et al. (2020) ISR [106] | RCT, 2 parallel groups, dental clinic | 69; 5–12 | TV distraction | Tell–show–do | (1) FIS (2) Frankl scale (4) HR (5) SpO2 | Pre-op/post-op | - Dental anxiety - Child’s cooperation |
| 36 | Kumari et al. (2021) USA [107] | RCT 2 parallel groups, dental clinic | 100; 6–12 | Immersive VR | Non-immersive VR | (1) MCDAS (2) VAS (3) WBFRS | Pre-op/post-op | - Dental anxiety - Pain perception |
| 37 | Mani et al. (2020) BGD [119] | RCT 3 parallel groups, hospital | 30; 6–12 | (1) Audio distraction (2) Audio-visual distraction | (3) No intervention | (1) HR (2) Venham’s picture rate (3) Venham’s clinical rating scale | 1st and 2nd visits | Dental anxiety |
| 38 | Marwah et al. (2005) IND [61] | RCT 2 parallel groups, dental clinic | 40; 4–8 | Music distraction is divided into (subgroups) depends on the pt.’s selection: a. instrumental music group b. nursery rhymes music group | No intervention | (1) Venham’s picture rate (2) Venham’s anxiety rating scale (3) HR (4) SpO2 | Four dental visits | - Dental anxiety - Type of music that is helpful in the reduction of anxiety |
| 39 | McMurray et al. (1985) [59] | RCT parallel groups, dental clinic | 80; 9–12 | Film model demonstrating coping strategies McMurray et al. (1985) | Film model concerned with dental hygiene | (1): Picture analogue scale (PDAS) (2) Pulse rate (3) DAI | Children were observed 1–2 week during dental examination following phycological treatment (locus of control and coping strategies) | Dental anxiety |
| 40 | Mitrakul et al. (2015) THA [74] | RCT 2 groups, dental clinic | 42; 5–8 | 1st visit: ‘without wearing AV eyeglass’ 2nd visit: ‘wearing AV eyeglass’ | 1st visit: ‘wearing AV eyeglass’ 2nd visit: ‘without wearing AV eyeglass’ | (1) Faces Pain Scale-Revised (2) FLACC (3) HR | - Pre-operation - RD placement - 1st use of hand-piece - 5 min interval during the remaining Tx | - Dental pain - Dental anxiety |
| 41 | Mungara et al. (2012) IND [91] | RCT 2 groups, dental clinic | 90; 5–9 | Film modeling | Not exposed to any film | (1) CFSS-DS | Baseline fear rating before the 1st visit and after the second visit | Dental anxiety |
| 42 | Navit et al. (2015) IND [73] | RCT 5 parallel groups, dental clinic | 150; 6–12 | (1) Instrumental music group (2) Musical nursery rhymes group (3) Movie songs group (4) Audio stories group | No intervention | (1) VPT (2) VCRS (3) HR | 4 dental visits ‘6M’ | Dental anxiety |
| 43 | Niharika et al. (2018) IND [72] | RCT 2 single blinded-crossover groups, dental clinic | 40; 4–8 | Group A: Session I: tell–show–do Session II: with VR Session III: no VR | Group B: Session I: tell–show–do Session II: no VR Session III: with VR | (1) Wong–Baker faces (2) MCDAS (3) HR | Three dental sessions | - Dental anxiety - Dental pain |
| 44 | Nuvvula et al. (2015) IND [71] | RCT 3 parallel groups, dental clinic, and school | 90; 7–10 | (1) Audio (basic technique + music) (2) AV (basic technique + 3D AV) | Basic behaviour guidance technique without distraction | (1) MCDASf (2) Pulse rate (3) Wright’s modification of FBRS and Houpt scale | Pre-op/post-op ‘7M’ | Dental anxiety |
| 45 | Obadiah et al. (2020) IND [118] | RCT 2 groups, dental clinic | 60; 6–12 | Breathing exercise + bubble toy | No intervention | (1) Frankl behaviour rating scale (2) FIS (3) FLACC (4) Wong–Baker faces pain scale | 1st and 2nd visits ‘5M’ | - Dental anxiety - Pain perception |
| 46 | Padminee (2022) IND [108] | RCT 2 parallel groups, dental clinic | 70; 7–12 | Breathing relaxation through BrightHearts application during IANB delivery in the 1st 2 visit | VR through AV googles during IANB administration in the 1st 2 visits | (1) HR (2) Chotta Bheem–Chutki CBC scale(cartoon-based anxiety measuring scale) | 3 dental visits | Dental anxiety |
| 47 | Pande et al. (2020) IND [109] | RCT 4 parallel groups, dental clinic | 60; 5–8 | (1) Audio distraction (2) AVD using VR (3) Mobile phone Game Distraction | (1) Tell–show–do | (1) BP (2) HR (3) FIS | Pre-op/post-op | Dental anxiety |
| 48 | Peretz et al. (2005) ISR [60] | RCT 2 groups, dental clinic | 70; 3–6 | Magic tricks | Tell–show–do | (1) Time from the beginning of the session to sitting on the dental chair (2) Ability to perform a dental examination (3) Frankl’s behavioural category | Pre-op/post-op | Child’s behaviour |
| 49 | Ramirez-Carrasco et al. (2017) ESP [70] | RCT 2 parallel groups, dental clinic | 40; 5–9 | Headphones ‘classic directive hypnosis’ | Headphones to bleck out the dental drill’s noise | (1) FLACC (2) HR | During the dental visit | - Dental Anxiety - Dental pain |
| 50 | Ramos-Jorge et al. (2011) BRA [19] | RCT 2 parallel groups, dental clinic | 70; 4–11 | Positive image of dentistry and dental treatment | Dentally neutral image | VPT | Pre-op/post-op ‘5M’ | Dental Anxiety |
| 51 | Ran et al. (2021) CHN [110] | RCT 2 groups, dental clinic | 120; 4–8 | VR | Tell–show–do | (1) CFSS-DS (2) WBFS (3) FBRS | - Pre-op/during - Dental procedure | - Dental anxiety - Dental pain - Compliance score in perioperative children |
| 52 | Rank et al. (2017) BRA [67] | RCT 4 groups, dental clinic | 62; 4–6 | (1) Mirror and conversation (2) Toys (3) Children’s stories | (1) No distraction tool | (1) FIS (2) BRS | During dental procedure For ‘6 M’ | - Dental anxiety - Behaviours |
| 53 | Rank et al. (2019) BRA [68] | RCT 2 groups, dental clinic | 306; 4–6 | (1) a. Say–show–do b. Positive reinforcement technique with awards after dental care | (1) Say–show–do | VPT | Pre-op/post-op For ‘10 M’ | Children’s motivation in two dental visits and the difference occuring between genders |
| 54 | Sabherwal et al. (2021) IND [111] | RCT 3 groups, dental clinic | 60; 8–12 | (1) Hypnosis (2) Progressive muscle relaxation | (1) Communication and rapport building | (1) Visual Facial Anxiety Scale (2) HR (3) SpO2 (4) BP (5) Wong–Baker faces pain scale | Pre-op/post-op For ‘5 M’ | - Dental anxiety - Dental pain |
| 55 | Serra Negra (2019) BRA [66] | RCT 2 crossover groups, dental clinic | 34; 4–6 | 1st restoration session: music 2nd restoration session: No music | 1st restoration session: No music 2nd restoration session: music | (1) Pulse rate (2) EPQ-j ‘Brazilian version of the Eysenck Personality Questionnaire-Junior’ | The study consisted of three consecutive clinic consultations, each lasting about 25 min, separated by intervals of 7 days. | Effect of music on children’s pulse rate |
| 56 | Shekhar et al. (2022) IND [112] | RCT 3 parallel groups, dental clinic | 123; 8–12 | (1) Communication with verbal positive reinforcement + stress ball ‘active distraction’ (2) Communication with verbal positive reinforcement + AV distraction ‘passive distraction’ | (1) Communication with verbal positive reinforcement | (1) MCDAS (2) HR (3) Venham’s scale (4) Self-reporting and observational scale | Pre-op/post-op | - Dental anxiety - Dental pain |
| 57 | Shettty et al. (2019) IND [65] | RCT 2 parallel groups, dental clinic | 120; 5–8 | VR distraction | Conventional behaviour management technique | (1) MCDAS(f)r (2) Wong–Baker faces pain rating scale (3) Salivary cortisol levels | Pre-op/post-op | - Dental anxiety - Dental pain |
| 58 | Song et al. (2020) KOR [113] | RCT 2 groups, dental clinic | 48; 3–7 | 1st treatment: ‘watched cartoon animation’ and 2nd treatment: ‘used the programme’ | 1st treatment and 2nd treatment: ‘pts watched cartoon animation’ | (1) Heart rate (2) Wong–Baker faces Pain rating scale | Pre-op/post-op For ‘6 M’ | - Dental anxiety - Dental pain |
| 59 | Thakkar et al. (2021) IND [114] | RCT 2 groups, dental clinic | 102; 5–8 | Pet therapy group | Conventional behaviour management technique | (1) MCDASf (2) HR | Pre-op/post-op | Dental anxiety |
| 60 | Thosar et al. (2022) IND [115] | RCT 2 groups, dental clinic | 30; 4–11 | 1st visit: communication 2nd visit: magic thumb | 1st visit: communication 2nd visit: favourite cartoon on a mobile as AV | (1) VPT (2) Modified dental analogue scale (3) HR (4) SpO2 | - VPT and modified dental analogue scale were used post-op - HR and SpO2 were used pre-op, during, and post-op - For ‘3 M’ | Dental anxiety |
| 61 | Verma et al. (2022) IND [50] | Pilot study, RCT 4 groups, dental clinic | 80; 4–6 | (1) Tell–show–do with maternal presence (2) Mobile MG (3) MG with maternal presence | (1) Tell–show–do | (1) Frankl behaviour rating scale (2) RMS-PS (3) FLACC | Pre-op/post-op For ‘6 M’ | Dental anxiety |
| 62 | Vishwakarma et al. (2017) IND [31] | RCT 2 groups, dental clinic | 98; 5–7 | Phase I (1st visit): live modelling Phase II (2nd visit): after 7 days, subjects were subjected to rotary treatment | Phase I (1st visit): Tell–play–do Phase II (2nd visit): after 7 days, subjects were subjected to rotary treatment | (1) HR (2) FIS (3) Venham 6-point index | Pre-op/post-op | Dental anxiety |
| 63 | Wang et al. (2022) CHN [116] | RCT 2 crossover groups, dental clinic | 80; 9–12 | 1st treatment: auricular plaster therapy (anti-anxiety) + tell–show–do 2nd treatment: auricular plaster therapy (control) + tell–show–do | 1st treatment: auricular plaster therapy (control) + tell–show–do 2nd treatment: auricular plaster therapy (anti-anxiety) + tell–show–do | (1) Salivary Cortisol (2) Heart rate (3) FCS (4) MCDAS (5) Venham’s clinical anxiety obedience level rating scale | Pre-op/post-op For ‘7 M’ | Dental anxiety |
| 64 | Xia et al. (2016) CHN [64] | RCT 2 parallel groups, dental clinic | 100; 3–12 | Reward ‘pencil eraser, a cartoon sticker, or a small notebook’. | No intervention | CFSS-DS | Pre-op/post-op | Dental anxiety |
| 65 | Zachary (1985) USA [57] | RCT 3 stratified groups, dental clinic | 53; 3–11 | Stress relevant film | Stress irrelevant film | (1) VPT (2) Fear thermometer (3) Palmer sweat index (4) Behaviour profile rating scale (5) Global anxiety rating scale (6) Global behaviour rating scale | Pre-op/post-op | -The effectiveness of modeling film on representative, non-clinical sample of children - the effects of stress-relevant vs. irrelevant film intervention |
| 66 | Zhu et al. (2020) CHN [117] | RCT Class-based cluster 2 groups, school | 988; 7–8 | Experiential learning | Tell–show–do | (1) Modified CFSS-DS (2) BP (3) HR | Pre-op/post-op | Dental anxiety |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almarzouq, S.S.F.S.; Chua, H.; Yiu, C.K.Y.; Lam, P.P.Y. Effectiveness of Nonpharmacological Behavioural Interventions in Managing Dental Fear and Anxiety among Children: A Systematic Review and Meta-Analysis. Healthcare 2024, 12, 537. https://doi.org/10.3390/healthcare12050537
Almarzouq SSFS, Chua H, Yiu CKY, Lam PPY. Effectiveness of Nonpharmacological Behavioural Interventions in Managing Dental Fear and Anxiety among Children: A Systematic Review and Meta-Analysis. Healthcare. 2024; 12(5):537. https://doi.org/10.3390/healthcare12050537
Chicago/Turabian StyleAlmarzouq, Sarrah S. F. S., Helene Chua, Cynthia K. Y. Yiu, and Phoebe P. Y. Lam. 2024. "Effectiveness of Nonpharmacological Behavioural Interventions in Managing Dental Fear and Anxiety among Children: A Systematic Review and Meta-Analysis" Healthcare 12, no. 5: 537. https://doi.org/10.3390/healthcare12050537
APA StyleAlmarzouq, S. S. F. S., Chua, H., Yiu, C. K. Y., & Lam, P. P. Y. (2024). Effectiveness of Nonpharmacological Behavioural Interventions in Managing Dental Fear and Anxiety among Children: A Systematic Review and Meta-Analysis. Healthcare, 12(5), 537. https://doi.org/10.3390/healthcare12050537







