The Impact of Limited English Proficiency on Healthcare Access and Outcomes in the U.S.: A Scoping Review
Abstract
1. Introduction
1.1. Background
1.2. Rationale for the Current Study
1.3. Objectives
2. Methods
2.1. Literature Sources and Search Strategy
2.2. Study Selection
- Included adults with limited English proficiency as a clearly defined subset of the study population. We defined adults as subjects over the age of 18.
- Included LEP subjects residing in the United States. We excluded studies not conducted in the United States, as policies and laws that govern language services as well as access to care may be different across English-speaking countries.
- Study outcomes were quantitative and related to healthcare service access (e.g., health screenings, ambulatory care, hospital care, or mental health) or to clearly defined health outcomes, including outcomes related to healthcare costs.
- Quantitative health care outcomes were specified for LEP populations based on spoken language. As noted in our objectives, electronic medical records typically contain only information regarding the primary language spoken. In order to isolate the effects of spoken language from those of literacy, we focused on studies that had outcomes based on spoken language only or clearly defined a subset of results based on spoken English ability.
- Because our objective was to focus on spoken language proficiency among immigrant populations that have a primary language other than English, we excluded any studies primarily focused on a deaf or hard-of-hearing population. Although this is an important topic, the research team felt that it would require a separate and focused review.
- We excluded studies with outcomes focused on access to particular drugs or types of drugs (such as opiate pain medications). Studies that assessed specific interventions were also excluded. Studies with only qualitative outcomes were excluded from the analysis.
- Studies published prior to 2000 were excluded by database filters due to changes in policy around medical records data collection and language accessibility. Our searches included dissertations and theses. However, we elected to exclude conference presentations, posters, and preprints. We excluded studies written in languages other than English and studies not primarily focused on adults, defined as subjects ages 18 and older.
- Studies were excluded if healthcare outcomes were not specified for the LEP population, if the LEP definition was not clearly based only on spoken language, or if outcomes were not available for spoken language only.
2.3. Data Extraction
3. Results
3.1. Ambulatory Care Studies
| Ambulatory Care Citation | Health Outcome | Study Design | Study Period | Sample Size (N=) | LEP Sample Size (n=) | Setting | LEP Definition | Languages | Study Outcomes (LEP Related) |
|---|---|---|---|---|---|---|---|---|---|
| [25] | mental health service use | cross-sectional | 2002–2003 | 1147 | 465 | United States | poor/fair English speaking ability | Spanish, Mandarin, Cantonese, Vietnamese, and Tagalong | Significantly fewer LEP individuals for both Latino and Asian populations (compared to EP individuals) accessed lifetime mental health services (42.8% vs. 54.2%, p = 0.01, 32.9% vs. 53.9%, p = 0.01). LEP individuals for both Latino (14.6 vs. 9.4 years, p = 0.01) and Asian populations (16.3 vs. 9.0 years, p = 0.001) live longer with their disorder untreated. The EP population had a significantly higher odds of lifetime treatment for their mental health, with EP Latinos and Asians (OR 1.7; OR 2.3) significantly more likely to receive treatment compared to LEP individuals. |
| [26] | usual source of care | cross-sectional | 2005 | 2740 | NA | California | reported speaking English less than ‘‘well.’’ | NA | 44.7% of LEP participants had a usual source of care other than the ER, significantly less than their EP counterparts (p < 0.01). |
| [31] | healthcare access | cross-sectional | 2011–2019 | 5032 | NA | Greater Los Angeles area | English speaking ability was described as not well or not at all | NA | No significant interaction between English proficiency and regular doctor access. |
| [33] | health care utilization (mental and physical health) | cross-sectional | 1996–1997 | 31,003 | 1652 | United States | language of survey | Spanish | For LEP Hispanic participants, 61% had a physician visit in the past year and 4.0% had a mental health visit in the past year. LEP Hispanic patients were significantly less likely than non-Hispanic White patients to have had a physician visit (RR, 0.77; CI, 0.72–0.83) and a mental health visit (RR, 0.50; CI, 0.32–0.76). |
| [48] | dental care | cross-sectional | 2009 | 439 | 247 | Massachusetts | Those who score no/low on the BEST Plus test | NA | Dental visit rates in the last year for LEP refugees were 48.6%, significantly lower than EP (p = 0.04). In the last year, 27.4% of LEP refugees had a preventative dental visit, significantly lower than EP (p < 0.01). |
| [34] | advanced care planning | cross-sectional | 2013–2017 | 620,948 | 15,656 | Northern California integrated health system | Needing an interpreter | Spanish | Advanced directive (AD) completion probability was much lower among Hispanic Spanish speakers compared to their English-speaking and White counterparts. Negative predictors of AD completion included living in a primarily Spanish- speaking community (living in a census tract where >35% of residents were Spanish speakers, OR = 0.9; 95% CI= 0.8–0.9). |
| [35] | cardiovascular risk outcomes | retrospective cohort study | 2010–2012 | 71 | 9 | Wishard Health Services & Eskenazi Health Indianapolis, IN | only speak Spanish | Spanish | There was no significant difference found in outcomes between the English speaking and Spanish speaking groups. |
| [37] | health service utilization | cross-sectional | 2000 | 1703 | 565 | Washington | Used interpreter service at least once | Spanish and other | A higher proportion of LEP patients visited primary care (95% versus 82%) and specialty care (60% versus 50%), but a lower proportion visited the emergency room (31% versus 47%). Annualized numbers of visits to primary care sites were 6.2 per year for LEP subjects compared to 3.8 for English speakers. Specialty visits were 2.9 per year for LEP subjects compared to 2.2 for English speakers. |
| [38] | usual source of care and healthcare utilization | cross-sectional | 2018 | 21,177 | 1730 | California | Participants who reported speaking English not well or not at all | Spanish, Cantonese, Mandarin, Korean, Tagalog, and Vietnamese | LEP individuals were significantly less likely than their EP counterparts to have a usual source of care other than the ER, have a usual place to go when sick or needing medical advice, have preventative care in the last year, delay not getting medical care in the past 12 months, and forgo necessary care (p < 0.01). |
| [39] | health care spending and utilization | cross-sectional | 1998–2018 | 120,546 | 17,776 | United States | if their interview was conducted in Spanish | Spanish | LEP Hispanics spent $1463 less on medical expenses on average compared to their EP Hispanic counterparts (p < 0.001). LEP Hispanic individuals spent $2802 less on medical expenses on average compared to EP non-Hispanic individuals (p < 0.001). LEP Hispanics spent $456 less on outpatient care on average compared to their EP Hispanic counterparts (p < 0.001). LEP Hispanic individuals spent $708 less on outpatient care on average compared to EP non-Hispanic individuals (p < 0.001). LEP individuals were significantly less likely to utilize outpatient visits compared to their non-Hispanic and Hispanic EP counterparts (p < 0.001). |
| [41] | healthcare utilization | cross-sectional | 2006–2007 | 2884 | NA | United States | English proficiency below moderate (read at least a little or somewhat) | NA | 37.25% of those who were classified as LEP had used healthcare in the last 2 years compared to their proficient (81.20%) and moderately proficient (64.53%) counterparts (p < 0.001). |
| [42] | usual source of care | cross-sectional | 2014 | 342 | 286 | California | Participants who reported speaking English less than ‘very well’ | Korean and other | Participants with LEP were 8.13 times more likely to not have no usual source of care (CI 2.40–27.56, p < 0.01). |
| [40] | delivery of healthcare & receipt of clinical and preventative health services | retrospective cohort study | 1995–1997 | 4380 | 327 | four HMOs in New England | Use of interpreter services | Spanish & Portuguese | There was a significant increase in nearly all clinical service usage (office visits, phone calls, urgent care visits, prescriptions written, and prescriptions filled) in the interpreter services group after the updated interpreter services were implemented. For example, there was a greater increase in the number of prescriptions filled by those in the interpreter services group (2.33 prescriptions per person) compared to those in the comparison group (0.86). For preventative services receipt (mammograms, breast exams, pap smears, fecal occult blood (FOB) testing, rectal exams, and flu vaccinations), the increase in receipt of these services in the control group ranged from 0.01–0.10. In contrast, the increase for the interpreter services group ranged from 0.01–0.26. There were significant increases in the number of rectal exams for men over 40 years old. However, this difference was not significant after adjusting for demographic differences between the groups. |
| [43] | usual source of care | cross-sectional | 2015 | 2594 | 1618 | Austin, Texas | Reported that they spoke English less than very well | NA | After controlling for covariates, the risk of having no usual place for care was 2.09 (42.2% vs. 31.4%) times higher among the LEP population (p< 0.001). The risk of having no regular check-up was 1.69 (35.6% vs. 27%) times as great (p < 0.001). Perceived unmet needs for medical care were 1.89 (14.6% vs. 6.4%) times as great (p < 0.001). Reported communication problems in healthcare settings were 4.95 (42.1% vs. 6.9%) times as great ( p < 0.001). |
| [36] | missed primary care appointments | cross-sectional | 2015–2018 | 159,054 | 42,030 | Hospitals in Boston | Preferred language of care was other than English | Spanish, Portuguese, and Haitian Creole | At baseline, the proportion of missed appointments was 19.4% among Spanish, Portuguese, and Haitian Creole speakers compared to 20.4% of English speakers. The prevalence of missed appointments increased by 0.74 percentage points (CI: 0.34, 1.15) among Spanish, Portuguese, and Haitian Creole speakers compared to English speakers over the same time period. This amounted to 799 additional missed appointments in the post-period than expected. |
| [44] | health care utilization | cross-sectional | 2005–2007 | 217 | NA | Arizona | low English speaking, writing, and reading skills | NA | Increased EP scores revealed a 6% increase in physician visits (p < 0.05). |
| [22] | mental health service use | cross-sectional | 2002–2003 | 372 | 234 | United States | Fair/poor English speaking ability | Spanish, Vietnamese, Mandarin, Cantonese, and | For adult Latino immigrants with psychiatric disorders, having LEP significantly decreased the odds of using mental health services (OR = 0.30; CI = 0.14, 0.64) compared to all immigrants with psychiatric disorders. In the Asian immigrant population with psychiatric disorders, LEP did not significantly affect mental health service use. |
| [21] | healthcare utilization | cross-sectional | 2007 | 1745 | 988 | California | English speaking ability was not well or not at all | Spanish, Korean, Mandarin, Vietnamese, and Cantonese | Among Asians, LEP individuals were less likely (p < 0.001) than EP and English only individuals to see a medical doctor in the past 12 months. Among Asian LEP population who had seen a doctor, the total number of doctor visits was significantly higher (5.73) than for EP (3.92) and English only (2.85). Group differences were not significant in the Latino population. |
| [23] | healthcare access | cohort cross- sectional | 2006–2016 | 190,698 | 16,484 | United States | (a) reported that a language other than English was spoken in their home or (b) reported that they did not speak English well or that they were not comfortable speaking English. | NA | The proportion of individuals with LEP who had a usual source of care before the ACA was 45.3% and after the ACA was 53.1% which was a significant improvement (p < 0.001). Compared to their LEP counterparts, EP individuals had a 4.9% higher chance of having a usual source of care (p < 0.001). The proportion of individuals with LEP who had to forgo any necessary care was reduced from 10.3% before the ACA to 7.1% after the ACA, a −3.5% difference. Compared to their LEP counterparts, EP individuals were 3.2% less likely to forgo any necessary care (p < 0.001). The proportion of individuals with LEP who had to forgo any necessary medical care was reduced from 4.8% to 2.8%, a −2.2% difference (p < 0.001). Compared to their LEP counterparts, EP individuals were 1.4% less likely to forgo necessary medical care. The proportion of individuals with LEP who had to forgo any necessary dental care was 7.5% before the ACA to 5.2% after the ACA, a −2.4% difference (p < 0.001). |
| [24] | dental care | cross-sectional | 2013–2014 | 2114 | United States | self-reported as “limited” | NA | When accounting for acculturation factors, LEP was a significant factor for having a dental visit in the previous 12 months (p < 0.05). However, after considering dental insurance and income, the LEP variable became insignificant (p= 0.18). | |
| [45] | medication management with home healthcare | retrospective matched case- control | 2010–2014 | 73,815 for oral; 7807 for injectable | 17,662 fororal; 2248 for injectable | nonprofit home health agency | NA | NA | LEP was associated with less improvement in oral MM (.049, CI [.032-.065]) and injectable medications (.078, CI [.023-.133]) when compared to English-speaking patients. |
| [46] | eye care | cross-sectional | 2000–2003 | 5455 | 2775 | La Puenta, California | Preferring Spanish/Speaking only Spanish at home | Spanish | For participants who only spoke Spanish at home, the odds ratio for one or more eye care visits in the last 12 months was 0.79 (p < 0.05) compared to those who spoke English or both languages at home. There was no significant difference for having a dilated eye exam and having one or more dilated eye exams in the past 12 months. |
| [47] | usual source of care | cross-sectional | 2003 and 2005 | 3011 | 1207 | California | English speaking described as not well or not at all | N/A | 10% of those with LEP had no usual source of care (p < 0.001, OR = 2.3). |
| [32] | following recommendations for healthcare visit | retrospective cohort study (chart review) | 2012–2013 | 1174 | 587 | Minnesota primary care practice | using an interpreter for the phone line | Somali, Asian languages -including Vietnamese, Cambodian and | LEP callers were less likely to follow the nurse’s recommendation than non-LEP callers (AOR, 0.65; p < 0.001). Stratified by recommended action LEP patients were less likely to follow through with recommendations to call an ambulance or visit the ED (AOR, 0.28; CI, 0.13, 0.60) and recommended home care (AOR, 0.34; CI, 0.22, 0.55), but more likely for follow through with a routine visit within a week (AOR, 2.45; 95% CI, 1.24, 4.82). |
| [2] | usual source of care, delays in getting care | cross-sectional | 2001 | 18,000 | 1242 | California | Individual reported speaking English not well or not at all | Spanish, Cantonese, Mandarin, Korean, Vietnamese, and Khmer, | In bivariate analysis LEP older adults had significantly higher proportions that lacked a usual source of care than older adults who speak English only. In multivariate analysis, LEP older adults had increased risk of not having a usual source of care (RR = 1.86, p = 0.033) compared with English only speakers, but no significant differences in delays in care. |
| [30] | preventative care utilization | cross-sectional | 2000–2004 | NA | NA | United States | If respondent answered survey in another language besides English | NA | LEP immigrant population with private insurance was significantly less likely to get their flu shot, have their cholesterol checked, go to the dentist, and get a breast exam in the past year compared to the native population. There was no significant difference found for primary care visits, mammograms, or prostate exams between LEP immigrant population and native population with private insurance. There were no significant differences found in preventive care between immigrants with LEP and native populations with pubic insurance or who were uninsured. |
| [29] | primary care utilization | cross-sectional | NA | 275 | 102 | Tennessee | Speaks English a little or not at all | NA | There was no significant difference in LEP and EP individuals in visiting their primary care provider regularly (p =0.057). |
| [27] | delayed medical care, forgone needed care, and visits to healthcare professional | cross-sectional | 2006 | 29,868 | 2606 | United States | Speaks English less than very well | Spanish and other languages | Compared to English-proficient individuals, more individuals with LEP had forgone care (p < 0.05) and fewer reported healthcare visits (p < 0.001). Through unadjusted analyses, the study found that LEP individuals had 18% higher odds of forgoing medical care and 58% lower odds of having a healthcare visit compared to English-proficient individuals. In adjusted analyses, LEP individuals had 34% lower odds of having a healthcare visit. |
| [28] | healthcare utilization | cross-sectional | 2000 | 49,327 | NA | California, Colorado, Hawaii, Kansas, Michigan, New York, Ohio, | Survey language and language spoken at home were Spanish | Spanish and other | For participants who were Hispanic-Spanish and Asian-Other, there were significantly lower reports of timeliness of care, provider communication, and staff helpfulness (HS: −11.470, −3.575, −5.502, AO: −12.649, −7.158, −10.270; p < 0.001). There was also a significant difference in getting the care needed among Asian-Other participants(−8.459; p < 0.001). |
3.2. Hospital Care Studies
| Hospital Care Citations | Health Outcome | Study Design | Study Period | Total Sample Size (N=) | LEP Sample Size (n=) | Setting | LEP Definition | Languages | Study Outcomes (LEP Related) |
|---|---|---|---|---|---|---|---|---|---|
| [68] | end-of-life and palliative care | retrospective cohort | 2010–2018 | 18,490 | 1363 | Washington | “In what language do you want to talk to your healthcare team about your care?” | Mandarin Cantonese Vietnamese Russian Spanish | In adjusted analyses, LEP patients had higher odds of ED visits in the last 30 days (OR 1.47; CI 1.26, 1.72) & 180 days of life (OR 1.36; CI 1.17, 1.57). LEP patients had higher odds of 30-day readmission within the last 90-days (12% vs. 7.6%; OR 1.64, CI 1.30, 2.07) & 180-days of life (14.1% vs. 9.6%; OR 1.44; CI 1.16, 1.71) & higher odds of having an in-hospital death (OR 1.24; CI 1.07, 1.44). LEP patients had lower odds of advance care planning documents prior to death (OR 0.68; CI 0.59–0.80) when compared to EP patients. |
| [75] | door-to-room time and patient satisfaction | prospective cohort | 2011–2013 | 163 | 55 | Level 1 trauma center with an ED | Patients rated their language skills | Spanish | The median door-to-room and likelihood of admission was not significantly different between English-speakers and Spanish-speakers. English-speakers generally felt that the nurses completely understood their medical complaints, scoring a median of 5 on a 5 point Likert scale. Spanish speakers felt nurses mostly understood their medical complaint, scoring a median of 4 on a 5 points, and this comparison was statistically different between the groups. Spanish- speaking patients were significantly less satisfied with their triage experience than English-speaking patients. Of patients who described themselves English speakers, nurses misclassified one patient as having LEP. Of the patients who described themselves as Spanish speakers, nurses misclassified 15 as English speakers. |
| [78] | Potentially preventable intubations | retrospective cohort | 1994–2003 | 274 | 21 | Level 1 trauma center in eastern North Carolina | Patient’s primary language | Spanish | 21 Spanish-speaking patients were intubated for less than 48 hours, compared to the 38% English-speaking patients. Spanish-speaking patients had less serious injuries as per the Injury Severity Score (ISS) compared to the English speaking group (10.5 vs. 13.0). The Spanish speaking group had greater Glasgow Coma Score (GCS) than English- speaking patients. |
| [62] | code status, advance directives, limiting life support decisions | retrospective cohort | 2011–2014 | 27,523 | 779 | Seven ICUs of varying specialties in a single center | Primary language or interpreter use as noted on medical chart | Arabic, Spanish, Somali, Cambodian, Vietnamese, Lao, Hmong, Russian, | After adjusting for illness severity, sex, education, & insurance status, patients with LEP were less likely to change their code status from full code to do not resuscitate (DNR) during ICU admission (OR, 0.62; p < 0.001) People with LEP who died in the ICU were less likely to receive a comfort measures order set (OR, 0.38; p = 0.03). |
| [76] | healthcare service delivery for initial ED visit and following 90 days | retrospective cohort | 1999 | 500 | 437 | urban academic teaching hospital | Self-reported primary language and if the patient is comfortable communicating in English | Spanish, Haitian Creole, and Portuguese Creole | English-speaking patients spent more hours (mean = 11.83 h, 95% CI 9.59–14.08) than LEP patients who did not receive interpreter services (8.62 hours, 95% CI 7.68–9.61) and LEP patients who did receive interpreter services (9.51 hours, 95% CI 7.10–11.92). English-speaking patients also had the highest post index visit ED cost (USD 988) when compared to the those who received interpreting services (USD 878) and those who did not (USD 710). English-speaking patients had more test and procedures done (mean = 13.40) than those who received interpreting services (12.69) and LEP patients who did not receive interpreting services (10.58). More English-speaking patients returned to the ED within 30 days of discharge (mean = 8724) than LEP patients who received interpretation services (7584) and those who did not receive interpreter services (5305). |
| [50] | morbidity and mortality after traumatic injury | retrospective cohort study | 2012–2018 | 13,104 | 2144 | Zuckerberg San Francisco General Hospital (ZSFG), an | English was not among patient self-reported languages spoken | Chinese, Spanish, and Other | LEP patients had an increased rate of TBI when compared to EP patients (41% versus 38%). In multivariate analyses, LEP patients were significantly associated with increased hospital LOS, decreased ICU LOS, decreased transfer to acute care hospital, and increased discharge home with home health services or skilled nursing facility (SNF)/rehabilitation. |
| [69] | healthcare utilization, end-of-life and palliative care for COVID-19 patients | retrospective cohort | 2020 | 337 | 89 | Two academic & four community hospitals in Boston | Self-reported primary language other than English listed in the EHR | Creole, Russian, Portuguese, Italian, Cantonese, Vietnamese, Portuguese Creole, Khmer, French, | More LEP patients died in the ICU than EP patients (61.8% vs. 35.1%). More LEP patients received CPR when compared to EP patients (10.1% vs. 3.6%). Patients with LEP were admitted or transferred to the ICU more often than EP patients (82.0% vs. 52.8%). LEP was not associated with delayed palliative care consultations. LEP patients more often received mechanical ventilation or ECMO than EP patients (82.2% vs. 61.8%), but time spent on mechanical ventilation or ECMO did not differ. LEP was associated with a longer hospital LOS (mean difference 4.12 days; 95% CI 1.72–6.53). However, LEP was not associated with ICU LOS. |
| [66] | peri-operative LOS | cross-sectional | 2018 | 574 | NA | Academic medical center in Boston | using interpreting services | Spanish, Portuguese, Chinese, Arabic, and Other | In unadjusted analyses, the median LOS decreased with increased number of interpreting events per day. Patients in Quartile 4, who had 3+ interpreting events per day, had a median LOS of 1 day. Patients in Quartile 1, who had less than one interpreting event per day, had a median LOS of 11 days. There was an association between greater frequency of interpreting events and shorter surgical patient’s peri-operative LOS. |
| [7] | instances of unintended harm to the patients not relating to their disease or condition | prospective cohort | 2005 | 1083 | 251 | Six Joint Commission accredited hospitals in the USA | Non-English speaking | NA | 49.1% of reported adverse events (defined as any unintended harm to the patient not due to their underlying disease or condition) in LEP patients caused physical harm. A greater proportion of LEP patient adverse events resulted in a higher level of harm. LEP patients experienced more adverse events due to communication failure when compared to EP patients (52.4% vs. 35.9%). LEP patients experienced more adverse effects due to practitioner factors than EP patients (21.9% vs. 17.2%). |
| [51] | interpersonal processes of care (IPC) and cesarean delivery | cross-sectional study | 2004–2006 | 1308 | NA | Kaiser Permanente Medical Center and San | Poor or no English proficient based on interview | Spanish | At KP-MC, women who reported good or fluent English proficiency were more likely to deliver via cesarean than women with poor or no English proficiency (OR = 0.04, 95% CI 0.005–0.33). However, at SFGH, women with poor or no English proficiency were more likely to delivery via cesarean (OR = 1.61, 95% CI 0.86–3.05). |
| [52] | Inpatient mortality rates & obstetric trauma | cross-sectional | 2009 | 3,211,457 | 545,762 | Community, non- rehabilitative hospitals in California | Patient’s self-reported principal language | Spanish & Asian- Pacific Islander languages (Chinese, Japanese, | The risk-adjusted inpatient mortality for congestive heart failure, strokes, and pneumonia among Spanish and API language speakers were similar to or somewhat lower than that of EP patients. Age-adjusted rates of obstetric trauma were lower among Spanish speakers and higher among API language-speakers when compared to EP patients. |
| [74] | quality of acute pain treatment for obstetric and gynecological care patients | cross-sectional | 2003 & 2006 | 185 | NA | two teaching hospitals | patients who reported a need for interpreter service | Spanish | The group who responded as “Not Always” receiving interpreter services reported significantly lower scores for pain control (OR = 0.4, 95% CI 0.2–0.8), timely response (OR = 0.4, 95% CI 0.2–0.8), and perceived helpfulness from staff to respond to pain (OR = 0.3, 95% CI 0.2–0.7) than those who reported “Always” using interpreter services. Language barriers were reported by 13% of patients in the “Not Always” group as an obstacle to obtaining pain medication compared to the 8% in the “Always” group. |
| [71] | understanding discharge instructions | Cross-sectional | 2005–2008 | 308 | 203 | Urban public hospital’s general medical-surgical floor | Asking patients “How well do you speak English? and “In what language do you prefer to receive medical care?” | Spanish & Chinese | LEP participants had fewer discharge medications than EP participants (3.6 vs. 4.6). LEP patients were less likely than EP patients to have post-discharge ED visits or re-hospitalization (9% vs. 27%). Models were adjusted for clinical site, data collection time-period, and discharge time. LEP status was associated with lower odds of understanding medication category (OR = 0.63) and the outcome of medication category and purpose (OR = 0.89). LEP patients who reported language concordant discharge instructions had lower odds of understanding than EP patients (OR = 0.39). |
| [53] | hospital costs, LOS, 30-day readmission, and 30-day mortality risk. | observational cohort | 2001–2003 | 5877 | 1146 | General Medicine Service at the University of California, San | language codes collected from patient registration databases | Chinese (Cantonese or Mandarin), Spanish, Russian | Spanish and Russian-speaking patients had lower 30-day readmission rates (2.5% and 6.4%, respectively) than the EP group and the Chinese-speaking group. Chinese-speaking patients had the highest 30-day mortality (OR = 1.0, 95% CI 0.8–1.4). LEP patients had a higher odds of readmission at 30-days post-discharge than the EP group (OR = 1.3; 95% CI 1.0–1.7). |
| [64] | 30-day readmission, LOS, & hospital expenditures | natural experiment | 2007–2010 | 8077 | 1963 | Academic medical center | Patient’s primary language entered at registration | Chinese, Russian, Spanish, other Asian language, and Other | LEP patients all received the intervention (Bedside Interpreter Intervention). The odds of 30-day readmission for the LEP group compared to the EP group was lower during the intervention period (0.64; 95% CI 0.43–0.95) than it was during the pre- & post-intervention periods (1.07; 95% CI 0.85–1.35 & 1.09, 95% CI 0.80–1.48 respectively). |
| [54] | advance care planning discussions prevalence | cross-sectional | 2005–2008 | 369 | 232 | medical and surgical wards of two large urban hospitals in the | If patients answered “not at all”, “not well” to the question “How well do you speak English?” | Spanish & Chinese | Participants’ English proficiency was not associated with report of advance care planning discussions. |
| [73] | hospital discharge | prospective cohort | 2012–2013 | 94 | 79 | cardiovascular, general surgery and orthopedic surgery floors in | Speaking English not at all or not well | Spanish, Cantonese, & Mandarin | Pre-post discharge preparedness and patient-reported knowledge of follow-up appointments, discharge medication administration and side effects did not differ significantly after the implementation of the bedside phone interpreters. However, in bivariate models, knowledge of medication purpose increased significantly from before compared to after the implementation (88% vs. 97%). |
| [77] | informed consent | prospective cohort | 2012 & 2013 | 152 | NA | Academic medical center | Hospital identification algorithm | Spanish, Cantonese, Mandarin | Researchers evaluated the impact of a bedside interpreter phone system intervention on informed consent. More patients in the post-intervention group significantly met the criteria for adequately informed consent when compared to the pre-implementation group (54% vs. 29%, respectively). Post-intervention LEP patients had statistically higher odds of informed consent in adjusted models when compared to LEP patients in the pre-implementation group (aOR = 2.56, 95% CI 1.15–5.72). The post-implementation group had statistically significant higher odds of understanding the reason for their surgery or procedure (aOR = 3.60, 95% CI 1.52–8.56). The post-intervention group also had statistically higher odds of having all their questions answered (aOR = 14.1, 95% CI 1.43–139.0). When compared to English-speaking patients, post-intervention LEP patients had 62% lower odds of adequately informed consent compared to English-speaking patients (aOR = 0.38; 95% CI 0.16–0.91). |
| [65] | hospital LOS and 30- day readmission rates | retrospective cohort | 2004–2007 | 3071 | NA | tertiary care, university hospital | Patients’ preferred language | Spanish, Portuguese, Vietnamese, Albanian, Russian, and Other | Patients who did not have an interpreter present on both admission and discharge days were in the hospital about 1.5 days longer than patients who had interpreters on both days. Patients who received interpreters on both admission and discharge days had a mean LOS of 2.57, compared to patients who received interpretation neither on admission nor discharge days had a mean adjusted LOS of 5.06 days. 103/423 (24.3%) patient admissions who did not have an interpreter present either at admission and discharge were readmitted within 30 days, compared to 163/963 (16.9%) of patients with an interpreter at admission only, 85/482 (17.6%) of those with an interpreter at discharge only, and 178/1192 (14.9%) with an interpreter at both admission and discharge day. |
| [72] | Post-discharge reported issues | retrospective cohort | 2018–2019 | 12,294 | 1566 | academic medical center | EHR listed a preferred language for healthcare other than English if the patient self-identified as needing an interpreter | Spanish, Cantonese, Russian, Mandarin, Vietnamese, other | More LEP patients needed assistance getting prescriptions filled (adjusted, 8.3% vs. 5.5%) and had concerns about their medications (adjusted 12.9% vs. 10.6%). While LEP patients had more post-discharge issues, there was no significant difference in issue severity. |
| [63] | Total joint arthroplasty (TJA) | retrospective cohort | 2015–2019 | 4721 | 378 | urban medical center | language preference other than English & request for interpreter services | Spanish, Chinese, other non- English language | In univariate analyses, patients with LEP who underwent TJA had longer LOS (median [IQR], 3 [2,3,4] days vs. 2 [1,2,3] days), higher costs of hospitalization (median [IQR] $15,000 [$13,000-$22,000] vs. $14,000 [$12,000-$19,000]), and were more likely to be discharged to a skilled care facility (161 patients [42.6%] vs. 889 patients [20.5%]) compared with patients with EP. There was no difference in 30-day readmission rates by language status. |
| [59] | unplanned ED revisit within 72 hours of discharge | retrospective cohort study | 2012 | 32,857 | 2943 | Mount Sinai Hospital, a tertiary medical center in NYC | used EHR patient language preference | NA | The unadjusted odds ratio between LEP status and hospital admission was 1.20 (95% CI 1.11–1.30), but the association disappeared when controlling for confounding variables. LEP patients had an OR of 1.19 (95% CI 1.02, 1.48) in unadjusted association with unplanned ED revisits within 72 hours. This association became stronger in adjusted variables with an OR of 1.24 (95% CI 1.02, 1.53). |
| [49] | emergency department visits and hospital admissions | retrospective cohort | 2012 | 3784 | 1892 | large primary health care network in Minnesota | Language spoken by patients and interpreter status in HER | Somali, Spanish, Vietnamese, Khmer, Arabic, and Other | There were significantly more total ED visits (841 vs. 620) and hospitalizations (408 vs. 343) for IS (interpreter service) patients compared with non-IS patients. The proportion of patients with at least 1 ED visit (23.7% vs. 15.4%) and at least 1 hospitalization (15.1% vs. 10.6%) was significantly higher among IS patients. Nearly twice as many IS patients had 3+ ED visits and hospitalizations than non-IS patients. |
| [60] | admission for emergency surgery from the ED. | retrospective cohort | 2019 | 85,899 | 9874 | quaternary care, urban, academic medical center | patients used hospital interpreter services | NA | LEP individuals had significantly higher odds of admission for surgery compared to EP individuals (OR 1.33, CI 1.17, 1.50), but this difference disappeared after adjusting the models. LEP Hispanics were more likely to be admitted for surgery than non-LEP Hispanics (OR 1.63, CI 1.08, 2.47). |
| [55] | informed consent documentation | retrospective cohort (matched chart review) | 2004–2006 | 148 | 74 | Public teaching hospital in San Francisco | primary language from HER | Spanish, Cantonese, and Mandarin | EP patients were more likely to have full documentation of informed consent (53%) than LEP patients, who also had evidence of interpretation (28%). Only 41% of LEP patients had a consent form in their language or had one signed by an interpreter. In the multivariate, adjusted analysis, there were no differences in documentation between the EP and LEP groups, nor between the Spanish and Chinese-speaking patients. |
| [56] | risk of emergency department visit admission | retrospective cohort | 2017 | 9,641,689 | 1,421,385 | California hospitals | Selected a non-English language as the principal language to communicate with the healthcare provider | Spanish, Mandarin, Cantonese, Tagalog, Vietnamese, and Other | LEP patients were less likely to be admitted for diabetes with short-term complications than EP patients (54.0% vs. 70.9%). More LEP patients were admitted to the hospitals than EP patients (median different of 1.3%, IQR = −1.1–5.1%).LEP patients were more likely to be admitted for COPD or asthma in older adults across all models (36.8%, 95% CI 35.0–38.6%] vs. 33.3% in EP patients (95% CI 31.7–34.9%). Admission rates for those who spoke Mandarin/Cantonese, Vietnamese, and or other had a significant difference in admission rate compared to English. |
| [57] | differences in discharge opioid prescribing for trauma patients | cross-sectional study | 2018 | 1419 | 237 | Zuckerberg San Francisco General Hospital and Trauma | English was not among patient self-reported languages spoken. | NA | 41% of LEP patients were discharged on opioid medications. In multivariable models, EP patients had 1.63 adjusted increased odds of receiving any opioid prescription at discharge. EP patients received 147 oral morphine equivalents (OMEs) on average, compared with 94 OMEs for LEP patients. |
| [58] | birth outcomes (Cesarean sections, VBACs) | cross-sectional | 2012 | 11,419 | 1149 | HI hospitals that collected language preference | Preferred language noted at intake | Micronesian, Japanese, Tagalong, Spanish, Ilocan, Visayan, Mandarin, Cantonese, Chuukese, Marshallese, Tongan, Somoan, Hawaiian | There was a significant difference between primary Caesarean deliveries between EP and LEP (RR = 1.18), with a higher relative risk for patients with diabetes (RR = 1.30). There is also a significant difference in vaginal birth after Cesarean (VBAC) between EP and LEP (RR = 1.02). |
| [67] | LOS | prospective cohort | 2011 | 245 | 124 | Level 1 trauma academic emergency department | Preferred primary language recorded during registration | Spanish, Navajo, Vietnamese, Chinese, Arabic | There were no differences in mean LOS from arrival time to the time seen by a provider when comparing EP patients to LEP patients. There were also no mean LOS differences from arrival time to discharge or admission decision when comparing LEP to EP patients. |
| [70] | diagnostic test orders with chest & abdominal pain | prospective cohort | 1997–1998 | 324 | 172 | Public hospital emergency department | English speaking proficiency | Spanish, Cantonese, Hindi, Mien, Arabic, Russian, Mandarin, Korean, and other | No diagnostic test was found to be statistically significantly different between EP & LEP patients with chest pain. The frequency of ordering of CBC counts, serum electrolyte determinations, urinalyses, ECGs, and abdominal CT scans was found to be statistically different between English-speaking and non–English-speaking patients with abdominal pain. |
| [61] | emergency medical services scene and transport times | retrospective case- control study | 2012 | 201 | 100 | Albuquerque Ambulance Service and emergency | Inability to sign the EMS run report secondary to language barrier | NA | LEP patients had greater odds of calling 911 for trauma (OR, 2.5; CI, 1.4–1.5). LEP patients had longer transport times (mean difference of 2.2 minutes, CI, 0.04–4.0). LEP patients were more likely to have an electrocardiogram (ECG) done in EMS (OR, 3.7; CI 1.7–8.1) and ED care (OR = 2.0: CI, 1.1–1.3). LEP patients were more likely to leave without being seen or leave against medical advice (OR = 0.2; CI 0.1–0.7). |
3.3. Screening Studies
| Screening Studies Citations | Health Outcome | Study Design | Study Period | Total Sample Size (N=) | LEP Sample Size (n=) | Setting | LEP definition | Languages | Study Outcomes (LEP Related) |
|---|---|---|---|---|---|---|---|---|---|
| [80] | cervical, breast, and two types of colorectal cancer test use | cross-sectional | 2001 | 9079 | Men = 1786; Women = 2425 | California | Respondent took the interview in Spanish | Spanish | There was no significant difference between LEP and EP among Mexican-American women who had a mammogram and pap test. There was no significant difference between LEP and EP among Mexican-American men and women who had a colorectal cancer screening test. |
| [81] | knowledge and utilization of breast and cervical cancer early detection practices | cross-sectional | NA | 135; cervical cancer survey sample = 35 | 63; cervical cancer survey sample = 21 | community sites in New York City | Participants assessed their English speaking ability as not at all, poor, or average | Chinese | EP women were more likely to have heard of the clinical breast exam (38%), compared with the women who judged their language abilities as either totally lacking (15%) or else poor (13%) and were more likely to have had a clinical breast exam in the previous year compared to LEP participants. EP participants were more likely to believe that they needed a pap smear compared to LEP participants (p < 0.01), and were more likely to have had a pap smear (50% EP v 28.6% poor English and 28.6% not at all) within a year of the survey. |
| [82] | serologic HBV testing | cross-sectional | 2002 | 509 | 262 | Seattle, Washington | English proficiency determined by “speaks fluently or well”, “speaks quite well”, and “does not speak well or at all” | Vietnamese | LEP was independently associated with higher odds of past HBV testing (OR = 2.5; CI = 1.3–4.7) compared to high English proficiency. |
| [83] | receipt of mammogram, clinical breast exam, and pap smear | cross-sectional | 2002–2003 | 1708 | 1284 | California | Preferred language to speak to doctor or medical provider | Cambodian, Laotian, Thai, and Tongan | LEP immigrants had significantly lower odds of receiving a mammogram (OR = 0.46), clinical breast exam (OR = 0.59), and pap smear (OR = 0.40) compared to EP immigrants. |
| [84] | colorectal cancer screening uptake | cross-sectional | 2008 | 99,883 | 2362 | United States | Survey was completed in Spanish | Spanish | 48.2% of LEP Latino men had the lowest adjusted screening rates compared to all the other Latino subgroups, which include Latina women with LEP (56.2%). Compared to non-Latino White men, LEP Latino men were the least likely to report colorectal cancer (CRC) test use (AOR 0.47; CI 0.35–0.63). |
| [85] | cancer screening | cross-sectional | 2000- 2004 | 2399 | 1020 | Texas | Language of interview | Spanish | Women that did the interview in Spanish and are border residents are less likely to utilize screening services. Those interviewed in Spanish are associated with a lower likelihood of having a pap smear (OR = 0.732, CI = 0.537, 0.998), clinical breast exam (OR = 0.489, CI = 0.383, 0.624), mammogram within the past two years (OR = 0.660 CI = 0.442, 0.986) after controlling for age and educational differences. |
| [79] | colorectal cancer screening completion rates | retrospective cohort study | 2015–2018 | 412 | 103 | Primary care clinic in the Midwest | identified in the EHR need for an interpreter | Somali, Cambodian, Vietnamese, Arabic, and other. | The percentage of mt-sDNA tests without useful results was 53.4% (55/103) among patients with LEP compared to 29.1% (90/309) among EP patients (p < 0.0001). This study demonstrates a significant disparity in colorectal cancer screening completion using the mt-sDNA test among populations with LEP. |
| [86] | cancer screening health behaviors | cross-sectional | NA | 99 | NA | Community center for refugees and immigrants | Asked to rate their English speaking ability. | Russian | English language was the only acculturation measure that was significantly related to behaviors and outcomes. Women who spoke and understood English better were more likely to conduct a breast self-exam (p < 0.05). |
| [87] | receipt of Papanicolaou tests, clinical breast examinations, and mammography | cross-sectional | 1996- 1997 | 1247 | No English = 278; Another language more fluently than English = 66 | Oakland, CA; Los Angeles, CA; and Newark, NJ | Asked what language they usually read and spoke | Spanish, Cantonese, or Japanese | Not speaking or reading English (Pap: OR = 0.43, CI = 0.34, 0.54; CBE: OR = 0.44, CI = 0.35, 0.57) or speaking another language more fluently than English (Pap: OR = 0.50, CI = 0.35, 0.72; CBE: OR = 0.55, CI = 0.38, 0.80) significantly reduced the likelihood of receipt of Pap testing or CBE (p < 0.01). Those who reported not speaking or reading English were less likely to receive a mammogram (OR = 0.63, CI = 0.50, 0.80). |
| [40] | receipt of preventative health screenings | retrospective cohort study | 1995–1997 | 4380 | 327 | Four HMOs in New England | Use of interpreter services | Spanish & Portuguese | For receipt of screening services the study found significantly lower rates of FOB testing and rectal exams, but no significant difference in mammograms, breast exams, and pap smears, in the LEP compared to the EP population. After implementation of interpretation services the significant differences in screenings between LEP and EP populations disappeared. |
| [88] | regular cervical cancer screening | randomized controlled trial | 2003- 2004 | 473 | NA | Washington, DC metropolitan area | asking participants their ability to read, write, listen to, and speak English, ranging from “not at all” to “very good.” | Mandarin, Cantonese, Taiwanese, and Fuzhou | Women with higher English proficiency were more likely to have received regular Pap tests than women with LEP (OR, 1.39; CI, 1.13–1.72). |
| [89] | colorectal cancer test rates | cross-sectional | 2005 | 18,304 | 590 | California | Speaks “no English”, or “does not speak it well” at home | Spanish | Those with LEP were 1.68 times more likely to have never had any CRC test (p < 0.01) (blood test or endoscopy). Among Mexican Americans, non-LEP respondents were significantly more likely to have had fecal occult blood test (FOBT) only (10% vs. 16%; p = 0.01), both tests (11% vs. 29%; p < 0.01), and to have ever had any test (45% vs. 67%; p < 0.01), compared to LEP respondents. |
| [90] | breast and cervical cancer screening behaviors | cross-sectional | 1998- 1999 | 438 | NA | Maryland | English language proficiency was assessed by asking respondents to rate their English | Korean | Korean women who speak some English (OR = 1.98; CI, 1.07, 3.67) and those who speak English very well (OR = 2.41; CI, 1.03, 5.62) reported greater odds of having a mammogram compared to those that speak little English. |
| [91] | regular cervical cancer screening | cross-sectional | 2000 | 459 | NA | Maryland | Spoken English proficiency ranked as none/little; average, good/fluently | Korean | In the bivariate analysis, spoken English proficiency was identified to be significantly related to having regular pap smears (p < 0.05). |
| [92] | cancer screening | cross-sectional | 2000–2001 | 55,428 | NA | California | Does not speak English at home | Spanish, Mandarin, Cantonese, Vietnamese, Korean, or Khmer | Individuals who do not speak English at home were less likely to get screened for colorectal cancer (OR 0.75; CI, 0.58–0.98). |
| [93] | cholesterol screening | cross-sectional | 2011 | 389,039 | 24,509 | United States | Questionnaire completed in Spanish | Spanish | There was a significant difference between LEP (68.8%) and EP (88.7%) population in cholesterol screening within the past 5 years (p < 0.000). LEP Spanish speaking individuals were more likely to never have been screened for cholesterol (OR = 1.43; CI, 1.22–1.69) compared to EP individuals even after controlling for socio-demographic factors. |
| [94] | cervical cancer screening behaviors | cross-sectional | 2015 | 97 | 43 | a Midwestern city | Spoke English not at all or not too well | NA | 23.1% of LEP individuals who spoke English not at all had ever received a pap smear. 56.7% of LEP individuals who spoke English not too well had ever received a pap smear. |
| [95] | colorectal cancer screening rates | retrospective cohort study | 2002–2006 | 23,297 | 1703 | NA | Not comfortable conversing in English | Spanish | Non-English speakers had a lower use of colorectal cancer screening (30.7% vs. 50.8%; OR, 0.63; CI, 0.51–0.76). The adjusted odds of being current with CRC screening was lower for those in the Other Language-Concordant cohort compared to those in the English-Concordant cohort (OR, 0.57; CI, 0.46–0.71). The Other Language-Discordant cohort did not statistically differ from the English-Concordant cohort (OR, 0.84; CI, 0.58–1.21). |
| [96] | HIV testing | cross-sectional | 2012–2015 | 304 | 194 | North Carolina | Speaking comfortably in only Spanish | Spanish | LEP men who have sex with other men were 0.31 times less likely to receive HIV testing compared to EP (CI, 0.16–0.57). |
| [97] | meeting colorectal cancer screening guidelines | cross-sectional | 2007 | 15,888 | 539 | California | LEP is defined as self- reporting speaking English “not well” and “not at all.” | Mandarin, Cantonese, Korean, and Vietnamese | Individuals with LEP only (OR = 0.60) and LEP plus limited health literacy (OR = 0.52) were significantly less likely to meet colorectal cancer screening guidelines. Among the 539 individuals in the sample with LEP, 54.5% had a language- concordant provider. |
| [98] | meeting guidelines for cervical, colorectal and breast cancer screening | cross-sectional | 2007 | cervical= 632; colorectal = 488; breast = 326. | cervical = 201; colorectal = 181; breast = 153 | California | self-reporting speaking English “not well” and “not at all” | Cantonese and Mandarin | LEP was not independently significantly associated with meeting any of the screening guidelines for breast, cervical, or colorectal cancer comparing LEP to EP among the Chinese population. |
| [99] | endorsement of breast cancer screening | cross-sectional | NA | 200 | 91 | Washington, DC | Primary language labeled as “other” | Amharic and other | Endorsement of breast cancer screening was more likely among women whose primary language was English compared to those who spoke a non-English language (OR = 3.83; CI: 1.24 to 11.87). |
| [100] | colorectal, breast, and cervical cancer screening | cross-sectional | 2012- 2013 | NA | NA | Northern California outpatient healthcare system | Primary language is not English | NA | LEP individuals are 0.81 times less likely to receive a mammography screening (CI: 0.71, 0.92). LEP individuals are 0.79 times less likely to receive a colorectal cancer screening (CI: 0.72, 0.87). |
| [101] | accessing coloscopy, mammography, and papanicolaou smear screening. | cross-sectional | 2013- 2015 | 1298 | NA | New York City | NA | NA | English language proficiency was a significant barrier for some screening methods such as colorectal cancer screening with colonoscopy, and cervical cancer with pap smear, but not for mammography. Non-English speakers are significantly less likely to have a pap smear (OR = 0.24, CI= 0.14–0.41) compared to English speaking participants. |
| [102] | papanicolaou smear screening access | cross-sectional | 2007–2008 | 318 | 271 | Boston, MA | Need a translator during a healthcare encounter. | Spanish | There was no significant difference in likelihood of having less than 5 or 5 or more lifetime pap smears between women who report that they need a translator during a healthcare encounter. |
3.4. Specific Condition Studies
| Specific Condition Citations | Health Outcome | Study Design | Study Period | Total Sample Size (N =) | LEP Sample Size (n = ) | Setting | LEP Definition | Languages | Study Outcomes (LEP Related) |
|---|---|---|---|---|---|---|---|---|---|
| [103] | clinical diagnosis of diabetic peripheral neuropathy recorded in the EHR | cross-sectional | 2003–2008 | 12,681 | 1626 | Kaiser Permanente of Northern California | asked if respondents had difficulty understanding English | NA | LEP was independently associated with absence of clinical documentation of diabetic peripheral neuropathy in the EHR, despite reporting symptoms when surveyed. [RR 0.80 (0.68, 0.94)] |
| [104] | acute stroke care benchmarks and mortality rate | retrospective cohort | 2013–2016 | 928 | 282 | UC Irving Stroke Center (inpatient) | preferred language as indicated on admission | Spanish, Other | There was no statistically significant difference in acute stroke care benchmarks between LEP patients and patients whose preferred language was English |
| [105] | access to specialist care for colorectal cancer | cross-sectional | 1999–2000 | 1079 | 75 | Participants from 9 northern California counties | self-report of language spoken at home | Spanish | White LEP people reported significantly more problems with access to care than other groups, including Hispanic and Asian LEP people (p< 0.001). |
| [106] | cataract surgery | cross-sectional | 1997–1999 | 4774 | NA | outpatient clinics in Arizona, specifically Pima and Santa Cruz | Preferred language on interview was “mostly Spanish” rather than “Spanish and English” | Spanish and English | Comparing those who obtained cataract surgery with those having visually significant cataract (i.e., those needing surgery), speaking English (OR, 1.80; p = 0.04) was significantly associated with having obtained cataract surgery, even after adjusting for demographic variables and other potential risk factors. |
| [107] | participation in diabetes self-care measures | cross-sectional | 2009–2010 | 250 | 250 | outpatient clinics in rural California | not stated—study included only Spanish- speaking participants | Spanish | Spanish-speaking type 2 diabetes patients who had a Spanish-speaking provider reported engaging in diabetic foot care more frequently than those who did not have a Spanish-speaking provider (1.4 days vs. 0.7 days per week, p= 0.01). |
| [108] | Clinical variables related to diagnosis and treatment of squamous cell carcinoma | retrospective cohort | 2014–2019 | 477 | 51 | single cancer treatment center in Boston | preferred language at time of patient registration | Spanish, Mandarin, Vietnamese, Farsi, Greek and Haitian Creole | The LEP patients were diagnosed with cancer at a later overall stage (p = 0.03) and less frequently treated with surgery alone compared to English speaking patients (p < 0.001). After adjusting for stage and site, LEP patients were significantly more likely to receive primary surgical management compared to primary non-surgical management [OR =2.29 95% CI (0.93, 5.58), p = 0.008]. |
| [109] | high BP measurement in the absence of a self-reported diagnosis of hypertension, and/or a hypertension med prescription | cross-sectional | 1993–1994 | 2597 | NA | Community setting, 5 southwestern states | Used three separate but overlapping LEP definitions, and reported on each separately: | Spanish | Those who used Spanish more than English for mass media were twice as likely to have undiagnosed hypertension than those who used primarily English. |
| [110] | Cancer-related surgery outcomes, including LOS, 30-day ED revisit, all-cause | retrospective cohort | 2012–2017 | 2467 | 824 | Inpatient; single urban hospital | LEP status was determined by examining language concordance between | NA | After adjusting the results for insurance status, comorbidities, and other factors, there was no difference in surgery outcomes found between the LEP and EP groups |
| [111] | adherence to prescribed hypoglycemic medication | retrospective cohort | 2006–2012 | 30,838 | 3205 | Kaiser Permanente Northern California | preferred language was Spanish in electronic health record | Spanish | LEP Latinos were more likely to be non-adherent to oral medications and insulin than English-speaking Latinos [RRs 1.11–1.17, p < 0.05] or Whites [RRs 1.36–1.49, p < 0.05]. |
| [113] | HgbA1c | cross-sectional | 2005–2006 | 6738 | 510 | Kaiser Permanente Northern California | self-report; DISTANCE survey asked if respondents had difficulty understanding | Spanish | Among LEP Latinos, having a language discordant physician was associated with significantly poorer glycemic control (OR 1.98; CI 1.03–3.80). |
| [112] | LDL and systolic BP | retrospective cohort | 2005–2006 | 7359 | 542 | Kaiser Permanente Northern California | self-report; DISTANCE survey asked if respondents had difficulty understanding | Spanish | There were no statistically significant differences between LEP and non-LEP patients in terms of BP control. Among Latinos, LEP patients were less likely to have poor lipid control than English-speaking patients (odds ratio, 0.71; 95% CI, 0.54–0.93), with no difference by LEP patient–physician language concordance. LDL control was poor across the entire study group. |
| [114] | Undiagnosed dementia | cross-sectional | 2011 | 7385 | 362 | Used data from a nationally representative study | Responding “not well” or “not at all” when asked how well patients understand or speak | NA | Older adults with LEP were found to have 3.10 higher odds of possible dementia (95% CI 2.06–4.66). LEP was associated with significantly greater odds of undiagnosed dementia (OR = 2.95, 95% CI 1.70–5.12). LEP accounted for 87.6% of the foreign-born status effect on possible dementia, ad it explained 56.1% of the foreign-born status effect on undiagnosed dementia. |
| [115] | adherent to antipsychotic medications, hospitalization and health care costs | retrospective cohort | 1999–2004 | 31,560 | 2823 | San Diego County | self-reported preferred language | Spanish and Asian languages | A greater proportion of LEP Latinos were adherent compared to English proficient Latinos (41% vs. 36%, respectively, p = 0.002). A lower proportion of LEP Asians were adherent compared to their English proficient counterparts (40% vs. 45%, respectively, p = 0.034). LEP Latinos were less likely than English proficient Latinos to experience psychiatric admissions (17% vs. 21%, p < 0.001); non-psychiatric admissions (20% vs. 22%, respectively, p = 0.014); and overall inpatient admissions (33% vs. 38%, respectively, p < 0.001). LEP Latinos and Asians had the lowest overall costs- healthcare services and pharmaceuticals per year (15,883 USD and 15,138 USD, respectively) compared to other groups (adjusted for adherence). |
| [116] | first point of contact with public mental health services, service utilization for 18 | retrospective cohort | 2000–2005 | 9243 | 1108 | public mental health services in San Diego county; included | Preferred language as listed in EMR | Spanish, Vietnamese, Tagalog | LEP patients are significantly less likely to first contact mental health services through an emergency department, and more likely to use an outpatient clinic. They are also significantly less likely to use emergency services within the first 6 months of treatment, and more likely to seek outpatient services (p < 0.001 for each comparison). |
| [117] | HgbA1c, BP, LDL | cross-sectional | 2003–2018 | 5017 | 889 | national survey administered in a community setting | Anyone who completed the survey in a language other than English or used an interpreter | Spanish, Other | Compared to English-speaking participants, the LEP group that spoke a language other than Spanish (199 participants) were more likely to have elevated HbA1c (OR = 1.6, 95% CI = 1.1, 2.4) or a combination of elevated HbA1c, elevated LDL, and elevated BP (OR = 3.1; 95% CI = 1.2, 8.2). |
| [118] | 30-day post-op complications and readmissions after non- emergent infrainguinal bypass surgery | retrospective cohort | 2007–2014 | 261 | 51 | Inpatient, single urban hospital | Preferred language in medical record | Spanish, Portuguese Creole, Haitian Creole, Albanian, Other | No statistically significant difference in outcomes was found between the LEP group and the EP group. |
| [119] | self-monitoring of blood glucose | cross-sectional | 1994–1997 | 44,181 | 168 | Kaiser Permanente Northern California | requested a materials in a non-English language, used a Spanish-speaking interviewer for survey, interviewer assessment | NA | The LEP population was more likely to have a less-than-daily practice of self-monitoring blood glucose (SMBG) among type 2 diabetic patients treated pharmacologically (OR 1.3, CI [1.2–1.5]), although there was no significant difference shown among Type I diabetics in SMBG practice. In a sub-group analysis there was a significant difference between Type I diabetic Hispanic LEP and EP populations in checking SMBG greater than 1 time daily, but not in greater than 3 times daily. |
| [120] | Hypertension as defined by systolic BP over 140 or diastolic BP over 90 | retrospective cross-sectional | 2003–2012 | 23,382 | 3269 | used data from a national survey administered in a community | Anyone who completed the survey in a language other than English or used an interpreter | Spanish, Other | LEP was associated with an odds ratio of 1.47 (95% confidence interval: [1.07–2.03]) for having elevated BP |
| [121] | CES-D scores (depression screening tool) | prospective cohort, longitudinal | 1993–2007 | 2945 | 1793 | community setting in 5 southwestern states | self-report of speaking English “not at all” or “not too well” on study survey | Spanish | The CES-D scores of LEP patients increased at a more rapid rate over time during the study period. |
| [122] | HgbA1c | retrospective cohort | 1997–1998 | 183 | 79 | outpatient public clinics in Denver, CO | Record of spoken language in the administrative database, then confirmed by | Spanish | LEP patients had no significant difference in glycemic control. However, the study only looked at Hispanic patients, and noted glycemic control was equally poor for the entire sample, regardless of language ability. |
| [123] | Depressive disorder diagnosis and/or prescription of anti- depressant | RCT, nested cohort | 2003–2005 | 782 | NA | Primary care clinic at NYC hospital | Participants were asked if they preferred an interpreter. If yes, they were considered LEP, | Spanish, Chinese | Among BDI-FS positive patients, Chinese-speakers were less likely to be diagnosed with depression compared with English speakers (31% vs. 10%, p < 0.05). |
| [124] | HgbA1c, self-reported hypoglycemic events | cross-sectional | 2011–2012 | 1053 | 793 | outpatient community health centers in Northern | Language preference for the survey. Preference for a language other than English meant LEP | Spanish, Chinese | The study found no significant difference in measured health outcomes between LEP and non-LEP groups |
| [125] | Rates of specific breast cancer surgery, receipt of recommended breast cancer treatment | retrospective cohort | 2008–2018 | 417 | 59 | Outpatient comprehensive cancer center in an urban area | Requiring an interpreter | Spanish, other | No difference was found between the LEP group and EP group in terms of breast cancer outcomes. The LEP group had a lower all-cause mortality rate in the unadjusted analysis |
| [140] | LOS, discharge disposition, and 30-day readmission rate | retrospective cohort | 2015–2019 | 2232 | 146 | UCSF neurosurgical center | self-report of English not primary language and preference for interpreter services at | Spanish, Chinese | An association was found between LEP and longer LOS (incidence rate ratio 1.11, 95% CI 1.00–1.24), and discharge to skilled care (OR 1.76, 95% CI 1.13–2.72), which remained after adjusting for confounders. There was no difference in 30-day readmission rates by language status. |
| [126] | Glasgow Outcome Scale-Extended scores at 6 months post- injury, access to rehab | retrospective cross-sectional | 1998–2005 | 476 | 42 | urban Level 1 trauma center | Because of the nature of the injuries being treated, definition was twofold: If patient was | Spanish | LEP was associated with an odds ratio of 15.093 (95% CI [1.632–139.617]) of having a GOSE score indicative of severe disability 6 months post-injury. This was true even though no statistically significant difference was found for LEP patients in terms of either severity of initial injury, or access to rehab services. |
| [127] | Positive PHQ-2 screening test, indicating depression risk | cross-sectional | 2013–2016 | 1532 | 519 | Community setting | Self-report of speaking English “not well” or “not at all” | NA | The study did not find a consistent, statistically significant link between LEP and depression risk. However, among South Asians, increased depression risk was associated with greater English proficiency (OR = 3.9, 95% CI: 1.6–9.2) |
| [128] | diabetes management | retrospective cohort | 2012–2013 | 13,456 | 1486 | Minnesota Mayo Clinic and Hennepin County Medical | need interpreter services | NA | LEP patients were less likely to meet guideline outcome recommendations for hemoglobin A1C (66.9 vs. 73.9%; p < 0.000) and LDL-C (59.3 vs. 71.4%; p < 0.0001), but more likely to meet guideline outcome recommendations for blood pressure (83.3 vs. 75.9%; p < 0.000). In adjusted regression analyses LEP patients were more likely to meet guideline outcome recommendations for blood pressure <140/90 (OR, 2.02 CI [1.7, 2.4]) compared to non-LEP |
| [129] | HgbA1c, systolic BP, and LDL cholesterol | cohort | 2007–2013 | 1605 | 1605 | outpatient clinics in the Kaiser Permanente Northern | self-report of Spanish as primary language in EMR | Spanish | LEP patients who switched to a language concordant provider had significantly better A1c and LDL control vs. those who switched between two language discordant providers. After adjustment, the prevalence of glycemic control increased by 10% (95% CI, 2% to 17%; P = 0.01), and LDL control increased by 9% (95% CI, 1% to 17%; p = 0.03). |
| [130] | Incidence of post- tonsillectomy hemorrhage, and operative or non- | retrospective cohort | 2015–2020 | 2466 | 1026 | Inpatient head and neck surgery center in Boston | primary language preference in medical record | NA | There were no statistically significant differences in disposition or outcomes for LEP patients. |
| [131] | Treatment outcomes in head and neck cancer (HNC) patients receiving curative | retrospective cohort | 2004–2010 | 131 | 20 | Private, non- profit, urban academic medical center | Primary language spoken | Spanish, Portuguese, Russian, Vietnamese, Arabic, Mandarin, Haitian | English proficiency was significantly associated with an improved three-year locoregional control (LRC) among EP patients (82.2%) when compared to LEP patients (58.3%). LEP patients who received chemoradiation had inferior 3 year LRC when compared to the LEP patients who only received radiation (29.2% vs. 87.5%). LEP was determined to be a significant predictor locoregional failure (LRF), though the significance went away after adjusting for race/ethnicity. |
| [132] | 30-day readmission rate | prospective cohort | 2012 | 145 | 45 | Columbia Presbyterian hospital in New York City | Preferred language on admission | Spanish | The hazard ratio for 30-day readmission for patients who did not speak English as a primary language was 2.2 (p = 0.052). |
| [133] | time in therapeutic range with warfarin | retrospective cohort | 2009–2010 | 3770 | 241 | Massachusetts General Hospital | self- reported speaking English less than “very well” | NA | LEP patients compared with non-LEP patients spent less time in therapeutic range (71.6% versus 74.0%, p = 0.01) and more time in danger range (12.9% versus 11.3%, p = 0.02). In adjusted analysis, LEP patients had lower time in therapeutic range compared with non-LEP patients (OR 1.5, CI [1.1, 2.2]), but were not at greater risk of spending more time the danger range. |
| [134] | Hep B serologic status | retrospective cohort | 1997–2017 | 22,565 | 16,449 | outpatient health center in New York City | Self-report of language preference in chart, LEP if other than English | Mandarin, Cantonese, Other | Overall, LEP status was associated with higher likelihood of HBV current or ever infection. In the multivariate analysis, specifically having Mandarin as a preferred language was associated with higher likelihood of Hep B current infection [OR 1.67 (CI 1.33–2.10)], or ever-infection [OR 1.93 (CI 1.69–2.21)]. |
| [135] | Hep B serologic status | retrospective cohort | 2000–2010 | 1234 | 1234 | Outpatient clinic in Seattle, WA | Primary spoken language in medical record | Somali, Amharic, Khmer, Vietnamese, Tigrinya, Oromo, Chinese, Other | Only 8.9% of the sample was vaccinated. 56% were core positive, meaning they had been exposed to Hep B in their lifetime. There was a higher prevalence of exposure among speakers of Khmer and Oromo. |
| [136] | Treatment adherence for CVD risk factor controlling medications | retrospective cohort | 2005 | 131,277 | 6712 | Kaiser Permanente Northern California | self-report language preference | Spanish | Spanish-speaking patients were less likely than English speaking patients to be in good adherence (51% versus 57%, p < 0.001). When considered separately adherence for glucose lowering medications, lipid lowering medications, and BP lowering medications also showed a significant difference between Spanish and English speaking patients. |
| [137] | HgbA1c, LDL, BP | retrospective cohort | 2013–2014 | 5460 | 1555 | Hennepin County Medical Center (Minneapolis) | Preferred language in medical record | Spanish, Somali, Amharic, other | More LEP patients met BP targets (83 vs. 68%, p = 0.000) and obtained LDL targets (89 vs. 85%, p = 0.000), but this group also had worse LDL control (57 vs. 62%, p = 0.001). |
| [12] | Asthma symptom control (by ACQ score), and service utilization | prospective cohort | 2004–2007 | 318 | 57 | primary care clinics, 1 in East Harlem, NY, and 1 in New Brunswick, NJ | report 1) that English was not their native language, and 2) that they could not speak as well as a native speaker | Spanish | Hispanic LEP patients had significantly higher ACQ scores (higher scores mean worse symptom control), at both the 1 month and 3-month follow-ups, with the most striking difference at the 3-month follow-up. This finding remained significant even after participants over 65 were excluded from the sample, and remained significant in the multivariate analysis. LEP patients also had significantly more exacerbations requiring inpatient follow-up, again even when controlling for age (p < 0.05 for all comparisons). |
| [13] | Asthma symptom control (by ACQ score), and service utilization | prospective cohort | 2009–2011 | 268 | 38 | Outpatient clinics in NYC and Chicago | Self-report of speaking English “very poorly,” “poorly” or “fairly” on initial study interview | Spanish | Hispanic LEP patients had worse asthma control (p = 0.0007) and increased likelihood of inpatient visits (p = 0.002). The finding persisted when results were adjusted for demographics, asthma history, comorbidities, depression, and health literacy. |
| [138] | Short-term clinical outcomes after surgery: LOS, mortality, any complication, and disposition to rehab | cross-sectional | 2009–2017 | 7324 | 554 | New Jersey inpatient neurosurgery wards | primary language recorded on admission was not English | Spanish, other | The non-Spanish-speaking LEP group had increased post-operative LOS (adjusted incidence rate ratio, 1.10; p = 0.008) and higher odds of a complication (adjusted OR, 1.36; p = 0.015). |
3.5. General Health Outcomes
| General Health Outcomes Citations | Health Outcome | Study Design | Study Period | Total Sample Size (N =) | LEP Sample Size (n = ) | Setting | LEP Definition | Languages | Study Outcomes (LEP Related) |
|---|---|---|---|---|---|---|---|---|---|
| [143] | mental health (general distress, somatic distress, and performance distress) | cross-sectional | NA | 83 | NA | Community centers and Buddhist temple in Midwest | English language proficiency measures on a Likert scale of 1 (very poor to 5 (excellent) | Vietnamese | Women who reported poorer English language proficiency had greater general distress and somatic distress compared to women with higher English proficiency. |
| [42] | Self-rated overall health status | cross-sectional | 2014 | 342 | 286 | California | Participants who reported less than ‘very well’ to the question—“Would you | Korean or other | LEP participants were 4.67 times more likely to rate their overall health as fair/poor compared to their EP counterparts (CI 1.25–16.40, p< 0.05). Data on physical activity and smoking status were not significant. |
| [148] | self-rated general health, mental distress, and cognitive health | cross-sectional | 2017–2018 | 2032 | 1512 | Los Angeles, CA; New York City, NY; Austin, TX, Honolulu, HI; | how well participants spoke English, not at all/a little) | Korean | LEP was a significant predictor in the model for self-rated health (OR = 1.99, CI = 1.37, 2.87) and mental distress (OR = 1.43, CI = 1.04, 1.96), but not for cognitive health |
| [145] | activity limitation, self-rating of general health, and symptoms of depression | cross-sectional | 2008–2013 | 1301 | 922 | FL, NY, and TX | reported that they spoke English less than very well | Korean | LEP significantly increased the odds of an activity limitation (OR = 2.72 ), fair or poor heath (OR = 2.59), and probable depression (OR = 1.73) compared to non-LEP. |
| [146] | self-reported mental health | cross-sectional | 2002–2003 | 865 | 481 | National | Language of interview | Spanish | LEP had statistically significant worse (RR = 2.12) mental health with no psychosis |
| [21] | physical and mental health status | cross-sectional | 2007 | 1745 | 988 | California | Reported English speaking ability was not well or not at all | Spanish, Korean, Mandarin, Vietnamese, and Cantonese | Of the four chronic health conditions studied, diabetes mellitus was the only condition that was significantly different across language groups for Latinos (LEP 27.2%, EP 18.6%, English Only [EO] 13.2%). Rates of chronic health conditions did not differ according to language status for Asian immigrants. Disability rates were significantly higher in Latinos and Asians with LEP than in their counterparts with EP and EO. Individuals with LEP had poorer self-rated physical and mental health compared to both EP and EO immigrants. |
| [150] | Self-rated overall health status | cross-sectional | 2010 | 381 | 137 do not speak English; 239 prefer to have an interpreter | community coalition in Lowell, MA | Do not Speak English; Prefer to have an interpreter in healthcare settings; prefer to | Khmer | In bivariate analysis, Speak English (OR= 3.3) and prefer to receive health information in English (OR = 1.96) are more likely to have excellent, very good, or good self-reported health. Prefer to have an interpreter in healthcare settings are less likely (OR = 0.38) to have excellent, very good, or good health. In the multivariate analysis, LEP was not a significant predictor of self-reported heath after taking age, sex, and disability into account. |
| [149] | Self-rated overall health status | cross-sectional | NA | 378 | 79 | Diabetes Prevention Program in Arkansas and Oklahoma | individual reported speaking English not well or not at all | Marshallese | Regression analysis showed that participants who reported speaking English not at all/not well were significantly less likely to report better general health (excellent health or good health vs. fair/poor health) compared with those who reported speaking English very well (OR = 0.22, CI:.09, 0.54). |
| [142] | self-rated overall health status, mental health, and physical functioning | cross-sectional | 2000 | 205 | NA | New York City | Speaking English proficiency rated as Not at all, Not too well, Some what, or Very well | Chinese, Korean | Language proficiency predicated variance in physical functioning, general health, and mental health. |
| [147] | Physical and Mental Component Summary Medical Outcomes Study Short-Form | cross-sectional | 2009–2011 | 439 | 293 | Massachusetts | the Basic English Skills Test Plus (BEST Plus) low proficiency (0–329), moderate proficiency (330–598) | Somali | Having low English proficiency (β = 1.75, p = 0.02) were associated with higher mental health scores in the unadjusted model but had no significant relationship in the adjusted model. Low English proficiency were significantly associated with lower physical health scores in the unadjusted β = −3.33, p < 0.00) but not the adjusted models. No impact of moderate proficiency was found. |
| [144] | self-rated overall health status, mental health, and physical functioning | cross-sectional | 2005 | 1196 | NA | California | English proficiency from “only English” (1) to “not at all” (5). | NA | Lower levels of English proficiency were associated with higher odds of reporting worse General Health [OR = 1.85 (1.56, 2.19)], more Limited Physical Days [OR = 1.23 (1.02, 1.49)], and more Limited Combined (mental and Physical Health) Days [OR = 1.23 (1.03, 1.47)]. |
| [151] | Self-rated overall health status | cross-sectional | 2003–2004 | 763 | 148 | National | self- rated respondents spoke English- ‘‘not well/ not at all’’ | NA | Logistic regression showed that those who spoke English very well had lower odds of rating their current health as good/fair/poor than those who did not speak English well/not at all. |
| [2] | Self-rated overall health status and mental health | cross-sectional | 2001 | 18,000 | 1242 | California | reported speaking English not well or not at all | Spanish, Cantonese, Mandarin, Korean, Vietnamese, and Khmer, | In bivariate analysis LEP older adults had significantly higher proportions that reported poorer general and emotional health status than older adults who speak English only. In multivariate analysis, LEP older adults had increased risk of being in fair or poor health (RR = 1.68, p < 0.001) and of feeling sad all or most of the time (RR = 2.49, p < 0.001) compared with English only speakers. |
| [152] | Self-rated overall health status | cross-sectional | 2007 | 51,048 | 3715 | California | Self-reporting speaking English “not well” and “not at all.” | Spanish, Mandarin, Cantonese, Korean, and Vietnamese | LEP pop were significantly more likely to report poor health status compared to those with English proficiency (42.9% vs. 14.9%). Compared to those with English proficiency and adequate health literacy, the odds ratios of poor health were 2.10 (CI: 1.70–2.58) for LEP. LEP was also significantly associated with poorer health status vs. the reference among Latinos (OR: 2.01; CI: 1.51–2.69), Vietnamese (OR: 5.46; CI: 2.47–12.05), Whites (OR: 2.05; CI: 1.03–4.08), and Other race/ethnicity (OR: 2.05; CI: 1.34–3.12). |
| [3] | oral health | cross-sectional | 2008 | 1870 | 231 | New York City | Self- reported ability to speak English was poor | Chinese, Spanish | Among Chinese group, those who reported that their ability was fair or better were 2.24 (1.02, 4.96) more likely, (compared to Chinese spoken English poor) to have gone to a dentist in the past year. Difference among Hispanic LEP group was non-significant. |
| [141] | lifetime and 12-month rates of any depressive, anxiety, and substance abuse disorders | cross-sectional | 2002–2003 | 2095 | 797 | National study | Individual reported that spoken English was “fair/poor.” | English, Spanish, Mandarin, Cantonese, Tagalog, and Vietnamese | In the regression analysis non-LEP men were significantly less likely than LEP men to have any lifetime (OR = 0.44) or 12 month (OR = 0.29) depressive disorder, lifetime (OR = 0.51) or 12 month (OR = 0.45) anxiety disorder, or lifetime (OR = 0.52) or 12 month psychiatric disorder (OR = 0.45). There was no significant difference in mental health diagnoses between women with LEP and those who were English proficient. |
| [153] | Self-rated overall health status | cross-sectional | 2010–2013 | 705 | self-rated English proficiency—473; ever need medical interpreter—244 | San Francisco, CA | self-rated spoken English proficiency (“not at all,” “poorly,”) or ever having need for medical interpretation at their doctor’s office | Cantonese, Mandarin | Speaking English “poorly” or ‘not at all,’ was significantly associated with poor self-rated health in regression models. The need for a medical interpreter was not associated with self-rated health. |
4. Discussion
- Ambulatory care studies generally showed that the LEP population was less likely to have a usual source of care and had fewer ambulatory care visits.
- In the hospitalization studies, 30-day readmission was clearly higher for LEP populations, which dovetails with the studies that found that LEP patients were less likely to receive discharge instructions that they could understand and, therefore, less likely to follow through with discharge instructions.
- Both the specific condition and general health outcome studies show a pattern of worse outcomes for physical and mental health for LEP populations compared to EP populations.
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Civil Rights Division of the U.S. Department of Justice. Commonly Asked Questions and Answers Regarding Limited English Proficient (LEP) Individuals. Available online: https://www.lep.gov/sites/lep/files/media/document/2020-03/042511_QA_LEP_General_0.pdf (accessed on 1 December 2013).
- Ponce, N.A.; Hays, R.D.; Cunningham, W.E. Linguistic Disparities in Health Care Access and Health Status among Older Adults. JGIM J. Gen. Intern. Med. 2006, 21, 786–791. [Google Scholar] [CrossRef]
- Shelley, D.; Russell, S.; Parikh, N.S.; Fahs, M. Ethnic Disparities in Self-Reported Oral Health Status and Access to Care among Older Adults in NYC. J. Urban Health Bull. N. Y. Acad. Med. 2011, 88, 651–662. [Google Scholar] [CrossRef]
- Twersky, S.E. Do State Laws Reduce Uptake of Medicaid/CHIP by US Citizen Children in Immigrant Families: Evaluating Evidence for a Chilling Effect. Int. J. Equity Health 2022, 21, 50. [Google Scholar] [PubMed]
- Budiman, A. Key Findings about U.S. Immigrants; Pew Research Center: Washington, DC, USA, 2020. [Google Scholar]
- U.S. Census Bureau’s American Community Survey (ACS). Household Language by Household Limited English Speaking Status 2022; U.S. Census Bureau’s American Community Survey (ACS): Suitland, ML, USA, 2022. [Google Scholar]
- Divi, C.; Koss, R.G.; Schmaltz, S.P.; Loeb, J.M. Language Proficiency and Adverse Events in US Hospitals: A Pilot Study. Int. J. Qual. Health Care 2007, 19, 60–67. [Google Scholar]
- Chen, A.H.; Youdelman, M.K.; Brooks, J. The Legal Framework for Language Access in Healthcare Settings: Title VI and Beyond. J. Gen. Intern. Med. 2007, 22, 362–367. [Google Scholar] [CrossRef] [PubMed]
- Civil Rights Division|Executive Order 13166. Available online: https://www.justice.gov/crt/executive-order-13166 (accessed on 20 December 2023).
- Haldar, S.; Pillai, D.; Published, S.A. Overview of Health Coverage and Care for Individuals with Limited English Proficiency (LEP). KFF. 2023. Available online: https://www.kff.org/racial-equity-and-health-policy/issue-brief/overview-of-health-coverage-and-care-for-individuals-with-limited-english-proficiency/ (accessed on 28 December 2023).
- Youdelman, M. Summary of State Law Requirements Addressing Language Needs in Health Care. Available online: https://healthlaw.org/resource/summary-of-state-law-requirements-addressing-language-needs-in-health-care-2/ (accessed on 20 December 2023).
- Wisnivesky, J.P.; Kattan, M.; Evans, D.; Leventhal, H.; Musumeci-Szabó, T.J.; McGinn, T.; Halm, E.A. Assessing the Relationship between Language Proficiency and Asthma Morbidity among Inner-City Asthmatics. Med. Care 2009, 47, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Wisnivesky, J.P.; Krauskopf, K.; Wolf, M.S.; Wilson, E.A.; Sofianou, A.; Martynenko, M.; Halm, E.A.; Leventhal, H.; Federman, A.D. The Association between Language Proficiency and Outcomes of Elderly Patients with Asthma. Ann. Allergy Asthma Immunol. 2012, 109, 179–184. [Google Scholar] [CrossRef]
- Montgomery, M.P.; Allen, E.D.; Thomas, O.; Robinson, B.F.; Clark, D.; Connelly, A.; Mott, J.A.; Conrey, E. Association between Pediatric Asthma Care Quality and Morbidity and English Language Proficiency in Ohio. J. Asthma 2019, 56, 603–610. [Google Scholar] [CrossRef]
- DuBard, C.A.; Gizlice, Z. Language Spoken and Differences in Health Status, Access to Care, and Receipt of Preventive Services among US Hispanics. Am. J. Public Health 2008, 98, 2021–2028. [Google Scholar] [CrossRef]
- John-Baptiste, A.; Naglie, G.; Tomlinson, G.; Alibhai, S.M.; Etchells, E.; Cheung, A.; Krahn, M. The Effect of English Language Proficiency on Length of Stay and In-Hospital Mortality. J. Gen. Intern. Med. 2004, 19, 221–228. [Google Scholar] [CrossRef]
- Choi, S.; Lee, J.A.; Rush, E. Ethnic and Language Disparities in Diabetes Care among California Residents. Ethn. Dis. 2011, 21, 183–189. [Google Scholar] [PubMed]
- Wang, Y.; Wilson, F.A.; Stimpson, J.P.; Wang, H.; Palm, D.W.; Chen, B.; Chen, L.W. Fewer Immigrants Have Preventable ED Visits in the United States. Am. J. Emerg. Med. 2018, 36, 352–358. [Google Scholar] [CrossRef] [PubMed]
- Anderson, T.S.; Karliner, L.S.; Lin, G.A. Association of Primary Language and Hospitalization for Ambulatory Care Sensitive Conditions. Med. Care 2020, 58, 45. [Google Scholar] [CrossRef] [PubMed]
- Falagas, M.E.; Pitsouni, E.I.; Malietzis, G.A.; Pappas, G. Comparison of PubMed, Scopus, Web of Science, and Google Scholar: Strengths and Weaknesses. FASEB J. 2008, 22, 338–342. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.; Worley, C.B.; Allen, R.S.; Vinson, L.; Crowther, M.R.; Parmelee, P.; Chiriboga, D.A. Vulnerability of Older Latino and Asian Immigrants with Limited English Proficiency. J. Am. Geriatr. Soc. 2011, 59, 1246–1252. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.; Aguado Loi, C.X.; Chiriboga, D.A.; Jang, Y.; Parmelee, P.; Allen, R.S. Limited English Proficiency as a Barrier to Mental Health Service Use: A Study of Latino and Asian Immigrants with Psychiatric Disorders. J. Psychiatr. Res. 2011, 45, 104–110. [Google Scholar] [CrossRef]
- Lu, T.; Myerson, R. Disparities in Health Insurance Coverage and Access to Care by English Language Proficiency in the USA, 2006–2016. JGIM J. Gen. Intern. Med. 2020, 35, 1490–1497. [Google Scholar] [CrossRef]
- Luo, H.; Wu, B. Acculturation and Dental Service Use Among Asian Immigrants in the U.S. Am. J. Prev. Med. 2016, 51, 939–946. [Google Scholar] [CrossRef]
- Bauer, A.M.; Chen, C.-N.; Alegría, M. English Language Proficiency and Mental Health Service Use among Latino and Asian Americans with Mental Disorders. Med. Care 2010, 48, 1097–1104. [Google Scholar] [CrossRef]
- Cordasco, K.M.; Ponce, N.A.; Gatchell, M.S.; Traudt, B.; Escarce, J.J. English Language Proficiency and Geographical Proximity to a Safety Net Clinic as a Predictor of Health Care Access. J. Immigr. Minor. Health 2011, 13, 260–267. [Google Scholar] [CrossRef]
- Shi, L.; Lebrun, L.A.; Tsai, J. The Influence of English Proficiency on Access to Care. Ethn. Health 2009, 14, 625–642. [Google Scholar] [CrossRef]
- Weech-Maldonado, R.; Morales, L.S.; Elliott, M.; Spritzer, K.; Marshall, G.; Hays, R.D.; Weech-Maldonado, R.; Morales, L.S.; Elliott, M.; Spritzer, K.; et al. Race/Ethnicity, Language, and Patients’ Assessments of Care in Medicaid Managed Care. Health Serv. Res. 2003, 38, 789–808. [Google Scholar] [CrossRef]
- Saenphansiri, X.; Wyant, D.K.; Wofford, L.G. Barriers to Health Care among Laotian Americans in Middle Tennessee. J. Health Care Poor Underserved 2017, 28, 1537–1558. [Google Scholar] [CrossRef]
- Pylypchuk, Y.; Hudson, J. Immigrants and the Use of Preventive Care in the United States. Health Econ. 2009, 18, 783–806. [Google Scholar] [CrossRef]
- Dhanjani, S.A.; Yang, H.-H.; Goyal, S.; Zhang, K.; Gee, G.; Cowgill, B. Trends in Health Care Access Disparities Among Asian and Pacific Islander Health Fair Participants in Los Angeles, 2011–2019. Public Health Rep. 2023, 138, 97–106. [Google Scholar] [CrossRef] [PubMed]
- Njeru, J.W.; Damodaran, S.; North, F.; Jacobson, D.J.; Wilson, P.M.; St Sauver, J.L.; Radecki Breitkopf, C.; Wieland, M.L. Telephone Triage Utilization among Patients with Limited English Proficiency. BMC Health Serv. Res. 2017, 17, 706. [Google Scholar] [CrossRef] [PubMed]
- Fiscella, K.; Franks, P.; Doescher, M.P.; Saver, B.G. Disparities in Health Care by Race, Ethnicity, and Language among the Insured: Findings from a National Sample. Med. Care 2002, 40, 52–59. [Google Scholar] [CrossRef]
- Gonzalez, R.; Lyon, L.; Rabbani, J.; Conell, C.; Postlethwaite, D.; Spaulding, M.; Mason, M. The Association of Spanish Language Preference with Advance Directive Completion. J. Am. Geriatr. Soc. 2021, 69, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Gonzalvo, J.D.; Sharaya, N.H. Language Concordance as a Determinant of Patient Outcomes in a Pharmacist-Managed Cardiovascular Risk Reduction Clinic. J. Pharm. Pract. 2016, 29, 103–105. [Google Scholar] [CrossRef] [PubMed]
- Jirmanus, L.Z.; Ranker, L.; Touw, S.; Mahmood, R.; Kimball, S.L.; Hanchate, A.; Lasser, K.E. Impact of United States 2017 Immigration Policy Changes on Missed Appointments at Two Massachusetts Safety-Net Hospitals. J. Immigr. Minor. Health 2022, 24, 807–818. [Google Scholar] [CrossRef] [PubMed]
- Graham, E.A.; Jacobs, T.A.; Kwan-Gett, T.S.; Cover, J. Health Services Utilization by Low-Income Limited English Proficient Adults. J. Immigr. Minor. Health 2008, 10, 207–217. [Google Scholar] [CrossRef] [PubMed]
- Gulati, R.K.; Hur, K. Association Between Limited English Proficiency and Healthcare Access and Utilization in California. J. Immigr. Minor. Health 2022, 24, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Himmelstein, J.; Himmelstein, D.U.; Woolhandler, S.; Bor, D.H.; Gaffney, A.; Zallman, L.; Dickman, S.; McCormick, D. Health Care Spending And Use Among Hispanic Adults With And Without Limited English Proficiency, 1999–2018: Study Examines Health Care Spending and Use among Hispanic Individuals with and without Limited English Proficiency. Health Aff. 2021, 40, 1126–1134. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, E.A.; Lauderdale, D.S.; Meltzer, D.; Shorey, J.M.; Levinson, W.; Thisted, R.A. Impact of Interpreter Services on Delivery of Health Care to Limited-English-Proficient Patients. J. Gen. Intern. Med. 2001, 16, 468–474. [Google Scholar] [CrossRef]
- Hoerster, K.D.; Mayer, J.A.; Gabbard, S.; Kronick, R.G.; Roesch, S.C.; Malcarne, V.L.; Zuniga, M.L. Impact of Individual-, Environmental-, and Policy-Level Factors on Health Care Utilization Among US Farmworkers. Am. J. Public Health 2011, 101, 685–692. [Google Scholar] [CrossRef]
- Ivey, S.L.; Kim, H.; Yoo, E.; Hwang, N.; Cha, D.D.; Lee, J.; Tseng, W. Health and Healthcare Needs of Koreans in San Francisco Bay Area: The Korean Needs Assessment (KoNA) Project. J. Immigr. Minor. Health 2019, 21, 1043–1051. [Google Scholar] [CrossRef]
- Jang, Y.; Kim, M.T. Limited English Proficiency and Health Service Use in Asian Americans. J. Immigr. Minor. Health 2019, 21, 264–270. [Google Scholar] [CrossRef]
- Kang, S.; Kim, I.; Kim, W. Differential Patterns of Healthcare Service Use Among Chinese and Korean Immigrant Elders. J. Immigr. Minor. Health 2016, 18, 1455–1461. [Google Scholar] [CrossRef]
- Miner, S.M.; Squires, A.P.; Ma, C.; McDonald, M.V.; Jones, S.A. Detecting Disparities in Medication Management Among Limited English Proficient and English Proficient Home Health Patients. Home Health Care Manag. Pract. 2020, 32, 28–33. [Google Scholar] [CrossRef]
- Morales, L.S.; Varma, R.; Paz, S.H.; Lai, M.Y.; Mazhar, K.; Andersen, R.M.; Azen, S.P. Self-Reported Use of Eye Care among Latinos: The Los Angeles Latino Eye Study. Ophthalmology 2010, 117, 207–215.e1. [Google Scholar] [CrossRef]
- Nguyen, D. The Effects of Sociocultural Factors on Older Asian Americans’ Access to Care. J. Gerontol. Soc. Work 2012, 55, 55–71. [Google Scholar] [CrossRef]
- Geltman, P.L.; Hunter Adams, J.; Penrose, K.L.; Cochran, J.; Rybin, D.; Doros, G.; Henshaw, M.; Paasche-orlow, M. Health Literacy, Acculturation, and the Use of Preventive Oral Health Care by Somali Refugees Living in Massachusetts. J. Immigr. Minor. Health 2014, 16, 622–630. [Google Scholar] [CrossRef]
- Njeru, J.W.; St. Sauver, J.L.; Jacobson, D.J.; Ebbert, J.O.; Takahashi, P.Y.; Fan, C.; Wieland, M.L. Emergency Department and Inpatient Health Care Utilization among Patients Who Require Interpreter Services. BMC Health Serv. Res. 2015, 15, 214. [Google Scholar] [CrossRef]
- Castro, M.R.H.; Schwartz, H.; Hernandez, S.; Calthorpe, L.; Fernández, A.; Stein, D.; Mackersie, R.C.; Menza, R.; Bongiovanni, T. The Association of Limited English Proficiency With Morbidity and Mortality After Trauma. J. Surg. Res. 2022, 280, 326–332. [Google Scholar] [CrossRef]
- Hessol, N.A.; Odouli, R.; Escobar, G.J.; Stewart, A.L.; Fuentes-Afflick, E. Interpersonal Processes of Care and Cesarean Delivery in Two Health Care Settings. Am. J. Public Health 2012, 102, 1722–1728. [Google Scholar] [CrossRef] [PubMed]
- Hines, A.L.; Andrews, R.M.; Moy, E.; Barrett, M.L.; Coffey, R.M. Disparities in Rates of Inpatient Mortality and Adverse Events: Race/Ethnicity and Language as Independent Contributors. Int. J. Environ. Res. Public Health 2014, 11, 13017–13034. [Google Scholar] [CrossRef]
- Karliner, L.S.; Kim, S.E.; Meltzer, D.O.; Auerbach, A.D. Influence of Language Barriers on Outcomes of Hospital Care for General Medicine Inpatients. J. Hosp. Med. 2010, 5, 276–282. [Google Scholar] [CrossRef]
- Kulkarni, S.P.; Karliner, L.S.; Auerbach, A.D.; Pérez-stable, E.J. Physician Use of Advance Care Planning Discussions in a Diverse Hospitalized Population. J. Immigr. Minor. Health 2011, 13, 620–624. [Google Scholar] [CrossRef] [PubMed]
- Schenker, Y.; Wang, F.; Selig, S.J.; Ng, R.; Fernandez, A. The Impact of Language Barriers on Documentation of Informed Consent at a Hospital with On-Site Interpreter Services. J. Gen. Intern. Med. 2007, 22 (Suppl. S2), 294–299. [Google Scholar] [CrossRef] [PubMed]
- Schulson, L.; Lin, M.-Y.; Paasche-Orlow, M.K.; Hanchate, A.D. Limited English Proficient Patient Visits and Emergency Department Admission Rates for Ambulatory Care Sensitive Conditions in California: A Retrospective Cohort Study. JGIM J. Gen. Intern. Med. 2021, 36, 2683–2691. [Google Scholar] [CrossRef]
- Schwartz, H.E.M.; Matthay, Z.A.; Menza, R.; Fernández, A.; Mackersie, R.; Stein, D.M.; Bongiovanni, T. Inequity in Discharge Pain Management for Trauma Patients with Limited English Proficiency. J. Trauma Acute Care Surg. 2021, 91, 898–902. [Google Scholar] [CrossRef]
- Sentell, T.; Chang, A.; Ahn, H.J.; Miyamura, J. Maternal Language and Adverse Birth Outcomes in a Statewide Analysis. Women Health 2016, 56, 257–280. [Google Scholar] [CrossRef]
- Ngai, K.M.; Grudzen, C.R.; Lee, R.; Tong, V.Y.; Richardson, L.D.; Fernandez, A. The Association Between Limited English Proficiency and Unplanned Emergency Department Revisit Within 72 Hours. Ann. Emerg. Med. 2016, 68, 213–221. [Google Scholar] [CrossRef]
- Rigney, G.H.; Ghoshal, S.; Mercaldo, S.; Cheng, D.; Parks, J.J.; Velmahos, G.C.; Lev, M.H.; Raja, A.S.; Flores, E.J.; Succi, M.D. Assessing the Relationship Between Race, Language, and Surgical Admissions in the Emergency Department. West. J. Emerg. Med. 2023, 24, 141–148. [Google Scholar] [CrossRef]
- Weiss, N.R.; Weiss, S.J.; Tate, R.; Oglesbee, S.; Ernst, A.A. Language Disparities in Patients Transported by Emergency Medical Services. Am. J. Emerg. Med. 2015, 33, 1737–1741. [Google Scholar] [CrossRef] [PubMed]
- Barwise, A.; Jaramillo, C.; Novotny, P.; Wieland, M.L.; Thongprayoon, C.; Gajic, O.; Wilson, M.E. Differences in Code Status and End-of-Life Decision Making in Patients With Limited English Proficiency in the Intensive Care Unit. Mayo Clin. Proc. 2018, 93, 1271–1281. [Google Scholar] [CrossRef] [PubMed]
- Manuel, S.P.; Nguyen, K.; Karliner, L.S.; Ward, D.T.; Fernandez, A. Association of English Language Proficiency With Hospitalization Cost, Length of Stay, Disposition Location, and Readmission Following Total Joint Arthroplasty. JAMA Netw. Open 2022, 5, e221842. [Google Scholar] [CrossRef] [PubMed]
- Karliner, L.S.; Pérez-Stable, E.J.; Gregorich, S.E. Convenient Access to Professional Interpreters in the Hospital Decreases Readmission Rates and Estimated Hospital Expenditures for Patients With Limited English Proficiency. Med. Care 2017, 55, 199–206. [Google Scholar] [CrossRef]
- Lindholm, M.; Hargraves, J.L.; Ferguson, W.J.; Reed, G. Professional Language Interpretation and Inpatient Length of Stay and Readmission Rates. J. Gen. Intern. Med. 2012, 27, 1294–1299. [Google Scholar] [CrossRef]
- de Crescenzo, C.; Chen, Y.-W.; Adler, J.; Zorigtbaatar, A.; Kirwan, C.; Maurer, L.R.; Chang, D.C.; Yeh, H. Increasing Frequency of Interpreting Services Is Associated With Shorter Peri-Operative Length of Stay. J. Surg. Res. 2022, 270, 178–186. [Google Scholar] [CrossRef]
- Wallbrecht, J.; Hodes-Villamar, L.; Weiss, S.J.; Ernst, A.A. No Difference in Emergency Department Length of Stay for Patients with Limited Proficiency in English. South. Med. J. 2014, 107, 1–5. [Google Scholar] [CrossRef]
- Abedini, N.C.; Downey, L.; Engelberg, R.A.; Curtis, J.R.; Sharma, R.K. End-of-Life Healthcare Utilization and Palliative Care Use among Older Adults with Limited English Proficiency. J. Am. Geriatr. Soc. 2022, 70, 2847–2857. [Google Scholar] [CrossRef]
- Chua, I.S.; Shi, S.M.; Jia, Z.; Leiter, R.; Rodriguez, J.A.; Sivashanker, K.; Yeh, I.M.; Bernacki, R.; Levine, D.M. Differences in End-of-Life Care between COVID-19 Inpatient Decedents with English Proficiency and Limited English Proficiency. J. Palliat. Med. 2022, 25, 1629–1638. [Google Scholar] [CrossRef]
- Waxman, M.A.; Levitt, M.A. Are Diagnostic Testing and Admission Rates Higher in Non-English-Speaking versus English-Speaking Patients in the Emergency Department? Ann. Emerg. Med. 2000, 36, 456–461. [Google Scholar] [CrossRef]
- Karliner, L.S.; Auerbach, A.; Nápoles, A.; Schillinger, D.; Nickleach, D.; Pérez-Stable, E.J. Language Barriers and Understanding of Hospital Discharge Instructions. Med. Care 2012, 50, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Malevanchik, L.; Wheeler, M.; Gagliardi, K.; Karliner, L.; Shah, S.J. Disparities After Discharge: The Association of Limited English Proficiency and Postdischarge Patient-Reported Issues. Jt. Comm. J. Qual. Patient Saf. 2021, 47, 775–782. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Nápoles, A.; Mutha, S.; Pérez-Stable, E.J.; Gregorich, S.E.; Livaudais-Toman, J.; Karliner, L.S. Hospital Discharge Preparedness for Patients with Limited English Proficiency: A Mixed Methods Study of Bedside Interpreter-Phones. Patient Educ. Couns. 2018, 101, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Jimenez, N.; Moreno, G.; Leng, M.; Buchwald, D.; Morales, L.S. Patient-Reported Quality of Pain Treatment and Use of Interpreters in Spanish-Speaking Patients Hospitalized for Obstetric and Gynecological Care. J. Gen. Intern. Med. 2012, 27, 1602–1608. [Google Scholar] [CrossRef]
- Balakrishnan, V.; Roper, J.; Cossey, K.; Roman, C.; Jeanmonod, R. Misidentification of English Language Proficiency in Triage: Impact on Satisfaction and Door-to-Room Time. J. Immigr. Minor. Health 2016, 18, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, J.; Bernstein, E.; Dave, A.; Hardt, E.; James, T.; Linden, J.; Mitchell, P.; Oishi, T.; Safi, C. Trained Medical Interpreters in the Emergency Department: Effects on Services, Subsequent Charges, and Follow-Up. J. Immigr. Health 2002, 4, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Pérez-Stable, E.J.; Gregorich, S.E.; Crawford, M.H.; Green, A.; Livaudais-Toman, J.; Karliner, L.S. Increased Access to Professional Interpreters in the Hospital Improves Informed Consent for Patients with Limited English Proficiency. J. Gen. Intern. Med. 2017, 32, 863–870. [Google Scholar] [CrossRef] [PubMed]
- Bard, M.R.; Goettler, C.E.; Schenarts, P.J.; Collins, B.A.; Toschlog, E.A.; Sagraves, S.G.; Rotondo, M.F. Language barrier leads to the unnecessary intubation of trauma patients. Am. Surg. 2004, 70, 783–786. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.C.; Njeru, J.W.; Wieland, M.L.; Rutten, L.J.; Jacobson, D.J.; Jenkins, G.D.; Fan, C. Disparities Among Limited English Proficient Patients in Colon Cancer Screening with Multi-Target DNA Stool Test. J. Immigr. Minor. Health 2022, 24, 556–559. [Google Scholar] [CrossRef] [PubMed]
- Breen, N.; Rao, S.; Meissner, H. Immigration, Health Care Access, and Recent Cancer Tests Among Mexican-Americans in California. J. Immigr. Minor. Health 2010, 12, 433–444. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.-T.; Wang, J. Chinese Female Immigrants English-Speaking Ability and Breast and Cervical Cancer Early Detection Practices in the New York Metropolitan Area. Asian Pac. J. Cancer Prev. APJCP 2013, 14, 733–738. [Google Scholar] [CrossRef]
- Choe, J.H.; Taylor, V.M.; Yasui, Y.; Burke, N.; Nguyen, T.; Acorda, E.; Carey Jackson, J. Health Care Access and Sociodemographic Factors Associated with Hepatitis B Testing in Vietnamese American Men. J. Immigr. Minor. Health 2006, 8, 193–201. [Google Scholar] [CrossRef]
- Dang, J.; Lee, J.; Tran, J.H.; Kagawa-Singer, M.; Foo, M.A.; Nguyen, T.-U.N.; Valdez-Dadia, A.; Thomson, J.; Tanjasiri, S.P. The Role of Medical Interpretation on Breast and Cervical Cancer Screening among Asian American and Pacific Islander Women. J. Cancer Educ. Off. J. Am. Assoc. Cancer Educ. 2010, 25, 253–262. [Google Scholar] [CrossRef][Green Version]
- Diaz, J.A.; Roberts, M.B.; Clarke, J.G.; Simmons, E.M.; Goldman, R.E.; Rakowski, W. Colorectal Cancer Screening: Language Is a Greater Barrier for Latino Men than Latino Women. J. Immigr. Minor. Health 2013, 15, 472–475. [Google Scholar] [CrossRef][Green Version]
- Fernández, L.E.; Morales, A. Language and Use of Cancer Screening Services among Border and Non-Border Hispanic Texas Women. Ethn. Health 2007, 12, 245–263. [Google Scholar] [CrossRef]
- Ivanov, L.L.; Hu, J.; Leak, A. Immigrant Women’s Cancer Screening Behaviors. J. Community Health Nurs. 2010, 27, 32–45. [Google Scholar] [CrossRef]
- Jacobs, E.A.; Karavolos, K.; Rathouz, P.J.; Ferris, T.G.; Powell, L.H. Limited English Proficiency and Breast and Cervical Cancer Screening in a Multiethnic Population. Am. J. Public Health 2005, 95, 1410–1416. [Google Scholar] [CrossRef]
- Ji, C.S.; Chen, M.-Y.; Sun, J.; Liang, W. Cultural Views, English Proficiency and Regular Cervical Cancer Screening among Older Chinese American Women. Womens Health Issues Off. Publ. Jacobs Inst. Womens Health 2010, 20, 272–278. [Google Scholar] [CrossRef] [PubMed]
- Johnson-Kozlow, M.; Roussos, S.; Rovniak, L.; Hovell, M. Colorectal Cancer Test Use among Californians of Mexican Origin: Influence of Language Barriers. Ethn. Dis. 2009, 19, 315–322. [Google Scholar]
- Juon, H.S.; Choi, Y.; Kim, M.T. Cancer Screening Behaviors among Korean-American Women. Cancer Detect. Prev. 2000, 24, 589–601. [Google Scholar] [PubMed]
- Juon, H.-S.; Seung-Lee, C.; Klassen, A.C. Predictors of Regular Pap Smears among Korean-American Women. Prev. Med. 2003, 37, 585–592. [Google Scholar] [CrossRef] [PubMed]
- Kandula, N.R.; Wen, M.; Jacobs, E.A.; Lauderdale, D.S. Low Rates of Colorectal, Cervical, and Breast Cancer Screening in Asian Americans Compared with Non-Hispanic Whites: Cultural Influences or Access to Care? Cancer 2006, 107, 184–192. [Google Scholar] [CrossRef]
- Kenik, J.; Jean-Jacques, M.; Feinglass, J. Explaining Racial and Ethnic Disparities in Cholesterol Screening. Prev. Med. 2014, 65, 65–69. [Google Scholar] [CrossRef]
- Kue, J.; Hanegan, H.; Tan, A. Perceptions of Cervical Cancer Screening, Screening Behavior, and Post-Migration Living Difficulties Among Bhutanese-Nepali Refugee Women in the United States. J. Community Health 2017, 42, 1079–1089. [Google Scholar] [CrossRef]
- Linsky, A.; McIntosh, N.; Cabral, H.; Kazis, L.E. Patient-Provider Language Concordance and Colorectal Cancer Screening. J. Gen. Intern. Med. 2011, 26, 142–147. [Google Scholar] [CrossRef]
- Painter, T.M.; Song, E.Y.; Mullins, M.M.; Mann-Jackson, L.; Alonzo, J.; Reboussin, B.A.; Rhodes, S.D. Social Support and Other Factors Associated with HIV Testing by Hispanic/Latino Gay, Bisexual, and Other Men Who Have Sex with Men in the U.S. South. AIDS Behav. 2019, 23, 251–265. [Google Scholar] [CrossRef]
- Sentell, T.; Braun, K.L.; Davis, J.; Davis, T. Colorectal Cancer Screening: Low Health Literacy and Limited English Proficiency among Asians and Whites in California. J. Health Commun. 2013, 18 (Suppl. S1), 242–255. [Google Scholar] [CrossRef]
- Sentell, T.L.; Tsoh, J.Y.; Davis, T.; Davis, J.; Braun, K.L. Low Health Literacy and Cancer Screening among Chinese Americans in California: A Cross-Sectional Analysis. BMJ Open 2015, 5, e006104. [Google Scholar] [CrossRef] [PubMed]
- Sheppard, V.B.; Hurtado-de-Mendoza, A.; Song, M.; Hirpa, F.; Nwabukwu, I. The Role of Knowledge, Language, and Insurance in Endorsement of Cancer Screening in Women of African Origin. Prev. Med. Rep. 2015, 2, 517–523. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Thompson, C.A.; Gomez, S.L.; Chan, A.; Chan, J.K.; McClellan, S.R.; Chung, S.; Olson, C.; Nimbal, V.; Palaniappan, L.P. Patient and Provider Characteristics Associated with Colorectal, Breast, and Cervical Cancer Screening among Asian Americans. Cancer Epidemiol. Biomark. Prev. Publ. Am. Assoc. Cancer Res. Cosponsored Am. Soc. Prev. Oncol. 2014, 23, 2208–2217. [Google Scholar] [CrossRef] [PubMed]
- Van Manh, A.L.; Blondeau-Lecomte, E.; Makoni, N.; Jandorf, L.; Perumalswami, P. Identifying Factors Associated with Cancer Screening in Immigrant Populations Living in New York City. J. Community Health 2020, 45, 1027–1029. [Google Scholar] [CrossRef]
- Watts, L.; Joseph, N.; Velazquez, A.; Gonzalez, M.; Munro, E.; Muzikansky, A.; Rauh-Hain, J.A.; Del Carmen, M.G. Understanding Barriers to Cervical Cancer Screening among Hispanic Women. Am. J. Obstet. Gynecol. 2009, 201, 199.e1–199.e8. [Google Scholar] [CrossRef] [PubMed]
- Adams, A.S.; Parker, M.M.; Moffet, H.H.; Jaffe, M.; Schillinger, D.; Callaghan, B.; Piette, J.; Adler, N.E.; Bauer, A.; Karter, A.J. Communication Barriers and the Clinical Recognition of Diabetic Peripheral Neuropathy in a Diverse Cohort of Adults: The DISTANCE Study. J. Health Commun. 2016, 21, 544–553. [Google Scholar] [CrossRef]
- Anderson, N.; Janarious, A.; Liu, S.; Flanagan, L.A.; Stradling, D.; Yu, W. Language Disparity Is Not a Significant Barrier for Time-Sensitive Care of Acute Ischemic Stroke. BMC Neurol. 2020, 20, 363. [Google Scholar] [CrossRef]
- Ayanian, J.Z.; Zaslavsky, A.M.; Guadagnoli, E.; Fuchs, C.S.; Yost, K.J.; Creech, C.M.; Cress, R.D.; O’Connor, L.C.; West, D.W.; Wright, W.E. Patients’ Perceptions of Quality of Care for Colorectal Cancer by Race, Ethnicity, and Language. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2005, 23, 6576–6586. [Google Scholar] [CrossRef]
- Broman, A.T.; Hafiz, G.; Muñoz, B.; Rodriguez, J.; Snyder, R.; Klein, R.; West, S.K. Cataract and Barriers to Cataract Surgery in a US Hispanic Population: Proyecto VER. Arch. Ophthalmol. 2005, 123, 1231–1236. [Google Scholar] [CrossRef]
- Detz, A.; Mangione, C.M.; Nunez de Jaimes, F.; Noguera, C.; Morales, L.S.; Tseng, C.-H.; Moreno, G. Language Concordance, Interpersonal Care, and Diabetes Self-Care in Rural Latino Patients. J. Gen. Intern. Med. 2014, 29, 1650–1656. [Google Scholar] [CrossRef]
- Duraiswamy, S.; Rubin, S.J.; Kim, Y.; Mur, T.; Edwards, H.A. Limited English Proficiency and Head and Neck Cancer Outcomes. Am. J. Otolaryngol. 2022, 43, 103470. [Google Scholar] [CrossRef]
- Eamranond, P.P.; Patel, K.V.; Legedza, A.T.R.; Marcantonio, E.R.; Leveille, S.G. The Association of Language with Prevalence of Undiagnosed Hypertension among Older Mexican Americans. Ethn. Dis. 2007, 17, 699–706. [Google Scholar]
- Feeney, T.; Park, C.; Godley, F.; Cassidy, M.; Sachs, T.; McAneny, D.; Tseng, J.F.; Drake, F.T. Provider-Patient Language Discordance and Cancer Operations: Outcomes from a Single Center Linked to a State Vital Statistics Registry. World J. Surg. 2020, 44, 3324–3332. [Google Scholar] [CrossRef] [PubMed]
- Fernández, A.; Quan, J.; Moffet, H.; Parker, M.M.; Schillinger, D.; Karter, A.J. Non-Adherence to Newly Prescribed Diabetes Medications Among Insured Latino and White Patients With Diabetes. JAMA Intern. Med. 2017, 177, 371–379. [Google Scholar] [CrossRef]
- Fernandez, A.; Warton, E.M.; Schillinger, D.; Moffet, H.H.; Kruger, J.; Adler, N.; Karter, A.J. Language Barriers and LDL-C/SBP Control among Latinos with Diabetes. Am. J. Manag. Care 2018, 24, 405–410. [Google Scholar]
- Fernandez, A.; Schillinger, D.; Warton, E.M.; Adler, N.; Moffet, H.H.; Schenker, Y.; Salgado, M.V.; Ahmed, A.; Karter, A.J. Language Barriers, Physician-Patient Language Concordance, and Glycemic Control among Insured Latinos with Diabetes: The Diabetes Study of Northern California (DISTANCE). J. Gen. Intern. Med. 2011, 26, 170–176. [Google Scholar] [CrossRef]
- Franco, Y.; Choi, E.Y. The Relationship Between Immigrant Status and Undiagnosed Dementia: The Role of Limited English Proficiency. J. Immigr. Minor. Health 2020, 22, 914–922. [Google Scholar] [CrossRef]
- Gilmer, T.P.; Ojeda, V.D.; Barrio, C.; Fuentes, D.; Garcia, P.; Lanouette, N.M.; Lee, K.C. Adherence to Antipsychotics among Latinos and Asians with Schizophrenia and Limited English Proficiency. Psychiatr. Serv. 2009, 60, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Gilmer, T.P.; Ojeda, V.D.; Folsom, D.P.; Fuentes, D.; Garcia, P.; Jeste, D.V. Initiation and Use of Public Mental Health Services by Persons with Severe Mental Illness and Limited English Proficiency. Psychiatr. Serv. 2007, 58, 1555–1562. [Google Scholar] [CrossRef] [PubMed]
- Holman, H.; Müller, F.; Bhangu, N.; Kottutt, J.; Alshaarawy, O. Impact of Limited English Proficiency on the Control of Diabetes and Associated Cardiovascular Risk Factors. The National Health and Nutrition Examination Survey, 2003–2018. Prev. Med. 2023, 167, 107394. [Google Scholar] [CrossRef]
- Inagaki, E.; Farber, A.; Kalish, J.; Siracuse, J.J.; Zhu, C.; Rybin, D.V.; Doros, G.; Eslami, M.H. Role of Language Discordance in Complication and Readmission Rate after Infrainguinal Bypass. J. Vasc. Surg. 2017, 66, 1473–1478. [Google Scholar] [CrossRef] [PubMed]
- Karter, A.J.; Ferrara, A.; Darbinian, J.A.; Ackerson, L.M.; Selby, J.V. Self-Monitoring of Blood Glucose: Language and Financial Barriers in a Managed Care Population with Diabetes. Diabetes Care 2000, 23, 477–483. [Google Scholar] [CrossRef]
- Kim, E.J.; Kim, T.; Paasche-Orlow, M.K.; Rose, A.J.; Hanchate, A.D. Disparities in Hypertension Associated with Limited English Proficiency. J. Gen. Intern. Med. 2017, 32, 632–639. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.; Kim, M.; Park, S.; Jimenez, D.E.; Chiriboga, D.A. Limited English Proficiency and Trajectories of Depressive Symptoms Among Mexican American Older Adults. Gerontologist 2019, 59, 856. [Google Scholar] [CrossRef]
- Lasater, L.M.; Davidson, A.J.; Steiner, J.F.; Mehler, P.S. Glycemic Control in English- vs. Spanish-Speaking Hispanic Patients with Type 2 Diabetes Mellitus. Arch. Intern. Med. 2001, 161, 77–82. [Google Scholar] [CrossRef]
- Leng, J.C.F.; Changrani, J.; Tseng, C.-H.; Gany, F. Detection of Depression with Different Interpreting Methods among Chinese and Latino Primary Care Patients: A Randomized Controlled Trial. J. Immigr. Minor. Health 2010, 12, 234–241. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Leung, L.B.; Vargas-Bustamante, A.; Martinez, A.E.; Chen, X.; Rodriguez, H.P.; Vargas-Bustamante, A. Disparities in Diabetes Care Quality by English Language Preference in Community Health Centers. Health Serv. Res. 2018, 53, 509–531. [Google Scholar] [CrossRef]
- Madans, A.R.; Zera, R.T.; Nygaard, R.M. The Effect of Language Barriers on Variation and Receipt of Early State Breast Cancer Treatment: A Single Center Study at a Midwestern, Metropolitan, Safety Net Hospital. J. Health Disparities Res. Pract. 2019, 12, 59–70. [Google Scholar]
- Marquez de la Plata, C.; Hewlitt, M.; de Oliveira, A.; Hudak, A.; Harper, C.; Shafi, S.; Diaz-Arrastia, R. Ethnic Differences in Rehabilitation Placement and Outcome after TBI. J. Head Trauma Rehabil. 2007, 22, 113–121. [Google Scholar] [CrossRef]
- Misra, S.; Wyatt, L.C.; Wong, J.A.; Huang, C.Y.; Ali, S.H.; Trinh-Shevrin, C.; Islam, N.S.; Yi, S.S.; Kwon, S.C. Determinants of Depression Risk among Three Asian American Subgroups in New York City. Ethn. Dis. 2020, 30, 553–562. [Google Scholar] [CrossRef]
- Njeru, J.W.; Boehm, D.H.; Jacobson, D.J.; Guzman-Corrales, L.M.; Fan, C.; Shimotsu, S.; Wieland, M.L. Diabetes Outcome and Process Measures Among Patients Who Require Language Interpreter Services in Minnesota Primary Care Practices. J. Community Health 2017, 42, 819–825. [Google Scholar] [CrossRef]
- Parker, M.M.; Fernández, A.; Moffet, H.H.; Grant, R.W.; Torreblanca, A.; Karter, A.J. Association of Patient-Physician Language Concordance and Glycemic Control for Limited-English Proficiency Latinos With Type 2 Diabetes. JAMA Intern. Med. 2017, 177, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Plocienniczak, M.; Rubin, B.R.; Kolli, A.; Levi, J.; Tracy, L. Outcome Disparities and Resource Utilization Among Limited English Proficient Patients After Tonsillectomy. Ann. Otol. Rhinol. Laryngol. 2022, 131, 1241–1246. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, M.M.; Romesser, P.B.; Jalisi, S.; Zaner, K.S.; Cooley, T.P.; Grillone, G.; Kachnic, L.A.; Truong, M.T. The Influence of Limited English Proficiency on Outcome in Patients Treated with Radiotherapy for Head and Neck Cancer. Patient Educ. Couns. 2014, 97, 276–282. [Google Scholar] [CrossRef] [PubMed]
- Regalbuto, R.; Maurer, M.S.; Chapel, D.; Mendez, J.; Shaffer, J.A. Joint Commission Requirements for Discharge Instructions in Patients with Heart Failure: Is Understanding Important for Preventing Readmissions? J. Card. Fail. 2014, 20, 641–649. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, F.; Hong, C.; Chang, Y.; Oertel, L.B.; Singer, D.E.; Green, A.R.; López, L. Limited English Proficient Patients and Time Spent in Therapeutic Range in a Warfarin Anticoagulation Clinic. J. Am. Heart Assoc. 2013, 2, e000170. [Google Scholar] [CrossRef] [PubMed]
- Tang, A.S.; Lyu, J.; Wang, S.; He, Q.; Pong, P.; Harris, A.M. Disparities in Hepatitis B Virus Infection and Immunity Among New York City Asian American Patients, 1997 to 2017. Am. J. Public Health 2018, 108, S327–S335. [Google Scholar] [CrossRef] [PubMed]
- Terasaki, G.; Desai, A.; McKinney, C.M.; Haider, M.Z. Seroprevalence of Hepatitis B Infection Among Immigrants in a Primary Care Clinic: A Case for Granular Ethnicity and Language Data Collection. J. Immigr. Minor. Health 2017, 19, 987–990. [Google Scholar] [CrossRef]
- Traylor, A.H.; Schmittdiel, J.A.; Uratsu, C.S.; Mangione, C.M.; Subramanian, U. Adherence to Cardiovascular Disease Medications: Does Patient-Provider Race/Ethnicity and Language Concordance Matter? J. Gen. Intern. Med. 2010, 25, 1172–1177. [Google Scholar] [CrossRef]
- Wilhelm, A.K.; Jacobson, D.J.; Guzman-Corrales, L.; Fan, C.; Baker, K.; Njeru, J.W.; Wieland, M.L.; Boehm, D.H. Regional Variation in Diabetic Outcomes by Country-of-Origin and Language in an Urban Safety Net Hospital. J. Community Health 2016, 41, 798–804. [Google Scholar] [CrossRef]
- Witt, E.E.; Eruchalu, C.N.; Dey, T.; Bates, D.W.; Goodwin, C.R.; Ortega, G. Non-English Primary Language Is Associated with Short-Term Outcomes After Supratentorial Tumor Resection. World Neurosurg. 2021, 155, e484–e502. [Google Scholar] [CrossRef]
- Gany, F.; Leng, J.C.F.; Winston, G.; Tseng, C.-H.; Qin, A.; Changrani, J. Diabetes Care and Language Discordance among Chinese and Latino Primary Care Patients. Ethn. Dis. 2011, 21, 473–479. [Google Scholar]
- Manuel, S.P.; Chia, Z.K.; Raygor, K.P.; Fernández, A. Association of Language Barriers With Process Outcomes After Craniotomy for Brain Tumor. Neurosurgery 2022, 91, 590–595. [Google Scholar] [CrossRef]
- Takeuchi, D.T.; Zane, N.; Hong, S.; Chae, D.H.; Gong, F.; Gee, G.C.; Walton, E.; Sue, S.; Alegría, M. Immigration-Related Factors and Mental Disorders among Asian Americans. Am. J. Public Health 2007, 97, 84–90. [Google Scholar] [CrossRef]
- Mui, A.C.; Kang, S.-Y.; Kang, D.; Domanski, M.D. English Language Proficiency and Health-Related Quality of Life among Chinese and Korean Immigrant Elders. Health Soc. Work 2007, 32, 119–127. [Google Scholar] [CrossRef]
- Brown, C.; Schale, C.L.; Nilsson, J.E. Vietnamese Immigrant and Refugee Women’s Mental Health: An Examination of Age of Arrival, Length of Stay, Income, and English Language Proficiency. J. Multicult. Couns. Dev. 2010, 38, 66–76. [Google Scholar] [CrossRef]
- Nguyen, D.; Reardon, L.J. The Role of Race and English Proficiency on the Health of Older Immigrants. Soc. Work Health Care 2013, 52, 599–617. [Google Scholar] [CrossRef] [PubMed]
- Jang, Y.; Yoon, H.; Park, N.S.; Chiriboga, D.A. Health Vulnerability of Immigrants with Limited English Proficiency: A Study of Older Korean Americans. J. Am. Geriatr. Soc. 2016, 64, 1498–1502. [Google Scholar] [CrossRef] [PubMed]
- Kato, K. Cultural Understandings of Mental Health: The Role of Language and Ethnic Identity. J. Ethn. Cult. Stud. 2018, 5, 58–73. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.E.; Smock, L.; Hunter-Adams, J.; Xuan, Z.; Cochran, J.; Paasche-Orlow, M.K.; Geltman, P.L. Relationships Between English Language Proficiency, Health Literacy, and Health Outcomes in Somali Refugees. J. Immigr. Minor. Health 2019, 21, 451–460. [Google Scholar] [CrossRef]
- Jang, Y.; Yoon, H.; Park, J.; Park, N.S.; Chiriboga, D.A.; Kim, M.T. Health Risks Posed by Social and Linguistic Isolation in Older Korean Americans. J. Am. Geriatr. Soc. 2021, 69, 3258–3266. [Google Scholar] [CrossRef]
- McElfish, P.A.; Scott, A.J.; Rowland, B.; Felix, H.C.; Narcisse, M.-R.; Kaminicki, K.F.; Long, C.R.; Selig, J.P. Investigating the Association between English Proficiency and General Health among Marshallese Adults in the United States. J. Health Care Poor Underserved 2021, 32, 724–736. [Google Scholar] [CrossRef] [PubMed]
- Koch-Weser, S.; Liang, S.L.; Grigg-Saito, D.C. Self-Reported Health among Cambodians in Lowell, Massachusetts. J. Health Care Poor Underserved 2006, 17, 133–145. [Google Scholar] [CrossRef] [PubMed]
- Okafor, M.C.; Carter-pokras, O.D.; Picot, S.J.; Zhan, M. The Relationship of Language Acculturation (English Proficiency) to Current Self-Rated Health Among African Immigrant Adults. J. Immigr. Minor. Health 2013, 15, 499–509. [Google Scholar] [CrossRef] [PubMed]
- Sentell, T.; Braun, K.L. Low health literacy, limited English proficiency, and health status in Asians, Latinos, and other racial/ethnic groups in California. J. Health Commun. 2012, 17 (Suppl S3), 82–99. [Google Scholar] [CrossRef]
- Tsoh, J.Y.; Sentell, T.; Gildengorin, G.; Le, G.M.; Chan, E.; Fung, L.-C.; Pasick, R.J.; Stewart, S.; Wong, C.; Woo, K.; et al. Healthcare Communication Barriers and Self-Rated Health in Older Chinese American Immigrants. J. Community Health 2016, 41, 741–752. [Google Scholar] [CrossRef]
- Rajaram, A.; Thomas, D.; Sallam, F.; Verma, A.A.; Rawal, S. Accuracy of the Preferred Language Field in the Electronic Health Records of Two Canadian Hospitals. Appl. Clin. Inform. 2020, 11, 644–649. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMAScR): Checklist and Explanation. Ann Intern Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
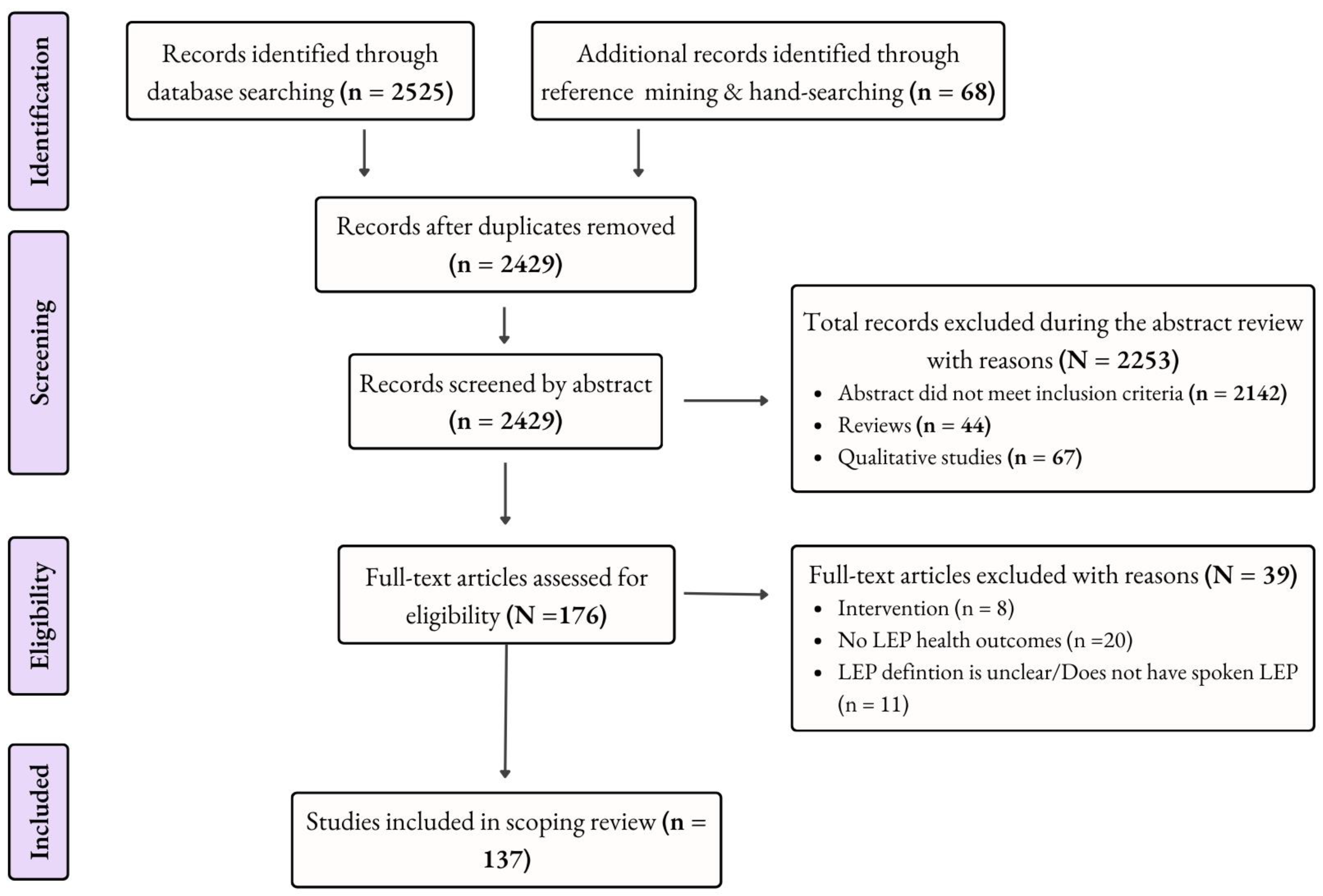
| Database | Search String and/or Strategy | Filters | Number of Results |
|---|---|---|---|
| PubMed | ((((limited English proficiency[MeSH Terms]) OR (language barrier[MeSH Terms])) AND ((((hospitalization[MeSH Terms]) OR (delivery of healthcare[MeSH Terms])) OR (quality of healthcare[MeSH Terms])) OR (emergency departments[MeSH Terms]))) AND (united states)) NOT (digital divide[MeSH Terms]) | English Exclude preprints Adult: 19+ years From 2000 to 2023 | 935 |
| Academic Search Premier | SU (“limited English proficiency” OR “language barriers”) AND SU (“health services accessibility” OR “health outcome assessment” OR “hospitals” OR “emergency departments”) NOT SU (“digital literacy” OR “digital divide”) | SmartText Searching English Source Type(s): Academic Journals and Trade Publications From 2000 to 2023 | 292 |
| CINAHL | ((((limited English proficiency) OR (language barrier)) AND ((((hospitalization) OR (delivery of healthcare)) OR (quality of healthcare)) OR (emergency departments))) AND (united states)) NOT (digital divide) | Basic Search English Source Type(s): Academic Journals and Dissertations From 2000 to 2023 | 326 |
| Sociological Abstracts | (“limited English proficiency” OR “language barriers” OR “language proficiency”) AND (health care) | Advanced Search English Source Types: Scholarly Journals, Dissertations and Theses, and Other Sources. United States From 2000 to 2023 | 956 |
| EconLit | TX language proficiency AND SU (“health care” OR “health behavior”) | English Source Type(s): Academic Journals and Dissertations From 2000 to 2023 | 16 |
| TOTAL | - | - | 2525 |
| Publicly Available State or National Dataset Used | Research Focus Area | Number of Papers Using |
|---|---|---|
| American Hospital Association (AHA) Annual Survey | Hospital Care | 1 |
| Asian American Quality of Life Survey | Ambulatory Care | 1 |
| Behavioral Risk Factor Surveillance System | Screening | 3 |
| California Cancer Registry | Specific Conditions | 1 |
| California Health Interview Survey | Ambulatory Care; General Health Outcomes; Screening | 10 |
| Community Tracking Study Household Survey | Ambulatory Care | 1 |
| DISTANCE Study Data (Diabetes Study of Northern California) | Specific Conditions | 3 |
| Hawaii’s Health Information Corporation’s Inpatient Database | Hospital Care | 1 |
| Hispanic Established Population for Epidemiological Studies of the Elderly (Hispanic EPESE) | Specific Conditions | 2 |
| Los Angeles Latino Eye Study (LALES) | Ambulatory Care | 1 |
| Medical Expenditure Panel Survey | Ambulatory Care | 2 |
| Minnesota Community Measures registry | Specific Conditions | 1 |
| National Agricultural Workers Survey (NAWS) | Ambulatory Care | 1 |
| National Consumer Assessment of Healthcare Providers and Systems (CAHPS) Benchmarking Database (NCBD) | Ambulatory Care | 1 |
| National Health and Aging Trends Study | Specific Conditions | 1 |
| National Health and Nutrition Examination Survey (NHANES) | Specific Conditions | 2 |
| National Health Interview Survey (NHIS) | Ambulatory Care | 2 |
| National Latino and Asian American Household Survey | Ambulatory Care; General Health Outcomes | 3 |
| National Trauma Registry of the American College of Surgeons (NTRACS) | Hospital Care | 1 |
| New Immigrant Survey | General Health Outcomes | 1 |
| State Inpatient Database (SID)—New Jersey * | Specific Conditions | 1 |
| State Inpatient Database (SID)—California * | Hospital Care | 1 |
| Study of Women’s Health Across the Nation (SWAN) | Screening | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Twersky, S.E.; Jefferson, R.; Garcia-Ortiz, L.; Williams, E.; Pina, C. The Impact of Limited English Proficiency on Healthcare Access and Outcomes in the U.S.: A Scoping Review. Healthcare 2024, 12, 364. https://doi.org/10.3390/healthcare12030364
Twersky SE, Jefferson R, Garcia-Ortiz L, Williams E, Pina C. The Impact of Limited English Proficiency on Healthcare Access and Outcomes in the U.S.: A Scoping Review. Healthcare. 2024; 12(3):364. https://doi.org/10.3390/healthcare12030364
Chicago/Turabian StyleTwersky, Sylvia E., Rebeca Jefferson, Lisbet Garcia-Ortiz, Erin Williams, and Carol Pina. 2024. "The Impact of Limited English Proficiency on Healthcare Access and Outcomes in the U.S.: A Scoping Review" Healthcare 12, no. 3: 364. https://doi.org/10.3390/healthcare12030364
APA StyleTwersky, S. E., Jefferson, R., Garcia-Ortiz, L., Williams, E., & Pina, C. (2024). The Impact of Limited English Proficiency on Healthcare Access and Outcomes in the U.S.: A Scoping Review. Healthcare, 12(3), 364. https://doi.org/10.3390/healthcare12030364







