Acceptability of Telerehabilitation: Experiences and Perceptions by Individuals with Stroke and Caregivers in an Early Supported Discharge Program
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Design
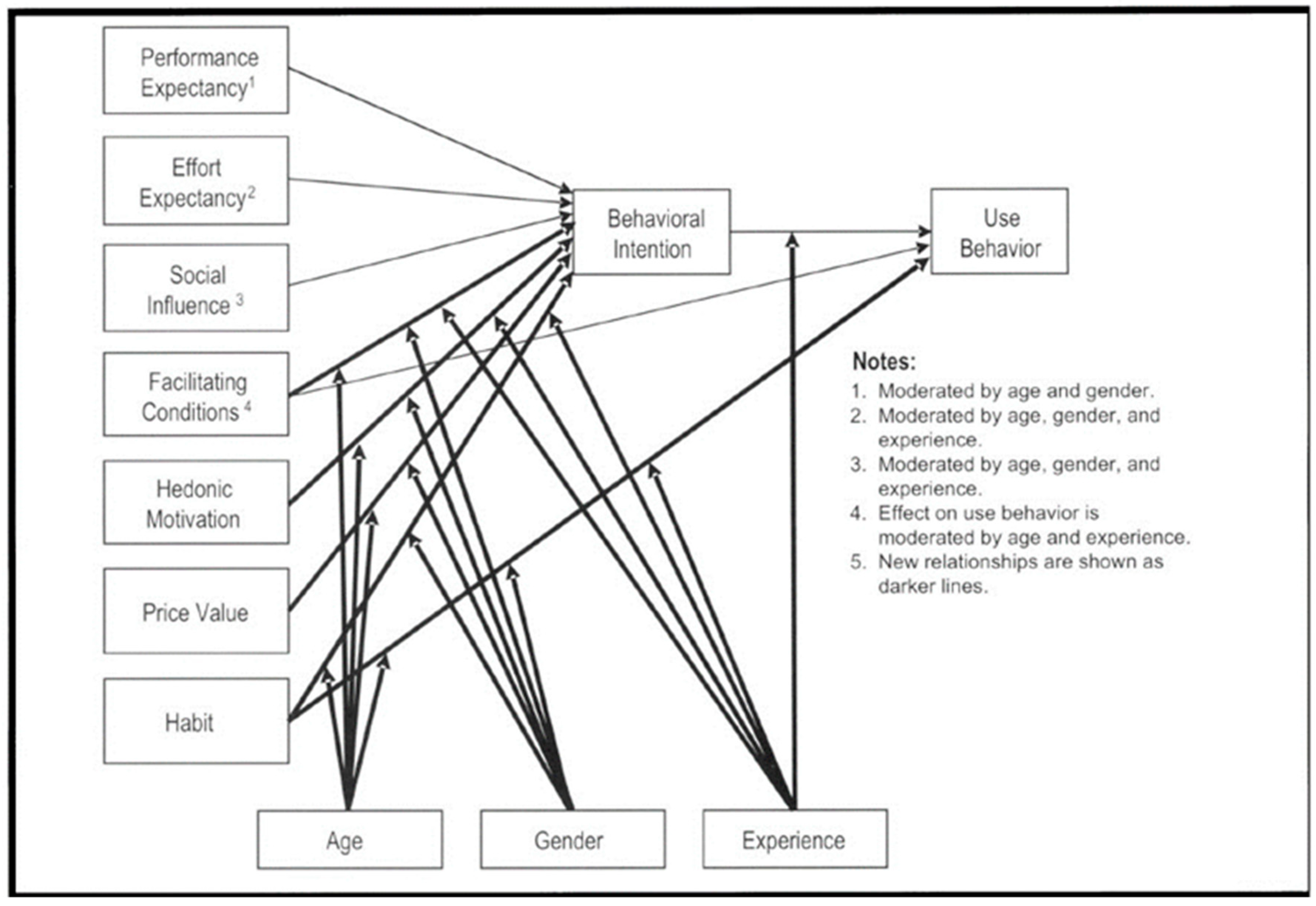
2.1.1. Theoretical Framework
2.1.2. Population and Recruitment
2.1.3. Intervention
The ESD Program
Telerehabilitation
2.1.4. Data Collection Procedure
Sociodemographic and Clinical Characteristics
Acceptability and Influencing Factors of Usability
2.1.5. Data Analysis
2.1.6. Ethical Considerations
3. Results
3.1. Description of Sample
3.2. Acceptability and Factors Influencing Usage of Telerehabilitation
3.2.1. Performance Expectancy
Participants’ Perception before Starting TR
Participants’ Perception after TR
3.2.2. Effort Expectancy
3.2.3. Social Influence
3.2.4. Facilitating Conditions
3.2.5. Hedonic Motivation
Society and the Health Care System
Remote Accessibility
3.2.6. Habit
3.2.7. Behavioral Intention
4. Discussion
5. Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Thrift, A.G.; Thayabaranathan, T.; Howard, G.; Howard, V.J.; Rothwell, P.M.; Feigin, V.L.; Norrving, B.; Donnan, G.A.; Cadilhac, D.A. Global stroke statistics. Int. J. Stroke 2017, 12, 13–32. [Google Scholar] [CrossRef]
- Crichton, S.L.; Bray, B.D.; McKevitt, C.; Rudd, A.G.; Wolfe, C.D.A. Patient outcomes up to 15 years aMer stroke: Survival, disability, quality of life, cognition and mental health. J. Neurol. Neurosurg. Psychiatry 2016, 7, 1091–1098. [Google Scholar] [CrossRef]
- Teasell, R.; Salbach, N.M.; Foley, N.; Mountain, A.; Cameron, J.I.; Jong, A.D.; Acerra, N.E.; Bastasi, D.; Carter, S.L.; Fung, J.; et al. Canadian Stroke Best Practice Recommendations: Rehabilitation, Recovery, and Community Participation following Stroke. Part One: Rehabilitation and Recovery Following Stroke; Update 2019. Int. J. Stroke 2020, 15, 763–788. [Google Scholar] [CrossRef] [PubMed]
- Jones, F.; Gombert, K.; Honey, S.; Cloud, G.; Harris, R.; Macdonald, A.; McKevitt, C.; Robert, G.; Clarke, D. Addressing inactivity after stroke: The Collaborative Rehabilitation in Acute Stroke (CREATE) study. Int. J. Stroke 2021, 16, 669–682. [Google Scholar] [CrossRef]
- Ministère de la Santé et des Services Sociaux (MSSS). Continuum of Services for Individuals at Risk of or Who Have Experienced a Stroke: Implementation Plan Phase 2016–2018. ©Government of Quebec. 2017. Available online: https://publications.msss.gouv.qc.ca/msss/fichiers/2017/17-944-01W.pdf (accessed on 27 October 2023).
- Chaiyawat, P.; Kulkantrakorn, K. Effectiveness of home rehabilitation program for ischemic stroke upon disability and quality of life: A randomized controlled trial. Clin. Neurol. Neurosurg. 2012, 114, 866–870. [Google Scholar] [CrossRef]
- Langhorne, P.; Baylan, S. Early supported discharge services for people with acute stroke. Cochrane Database Syst. Rev. 2017, 2017, CD000443. [Google Scholar] [CrossRef] [PubMed]
- Hitch, D.; Leech, K.; Neale, S.; Malcolm, A. Evaluating the implementation of an early supported discharge (ESD) program for stroke survivors: A mixed methods longitudinal case study. PLoS ONE 2020, 15, e0235055. [Google Scholar] [CrossRef] [PubMed]
- Kraut, J.; Singer, B.; Singer, K. Clinician and client views of utilising early supported discharge services. Int. J. Ther. Rehabil. 2016, 23, 464–471. [Google Scholar] [CrossRef]
- van der Veen, D.J.; Dopp, C.M.E.; Siemonsma, P.C.; Nijhuis-van der Sanden, M.W.G.; de Swart, B.J.M.; Steultjens, E.M. Factors influencing the implementation of Home-Based Stroke Rehabilitation: Professionals’ perspective. PLoS ONE 2019, 14, e0220226. [Google Scholar] [CrossRef]
- Salbach, N.M.; Mountain, A.; Lindsay, M.P.; Blacquiere, D.; McGuff, R.; Foley, N.; Corriveau, H.; Fung, J.; Gierman, N.; Inness, E.; et al. Canadian Stroke Best Practice Recommendations. Virtual Stroke Rehabilitation Interim Consensus Statement 2022. Am. J. Phys. Med. Rehabil. 2022, 101, 1076–1082. [Google Scholar] [CrossRef]
- Bettger, J.P.; Resnik, L.J. Telerehabilitation in the Age of COVID-19: An Opportunity for Learning Health System Research. Phys. Ther. 2020, 100, 1913–1916. [Google Scholar] [CrossRef]
- Laver, K.E.; Adey-Wakeling, Z.; Crotty, M.; Lannin, N.A.; George, S.; Sherrington, C. Telerehabilitation services for stroke. Cochrane Database Syst. Rev. 2020, 1, CD010255. [Google Scholar] [CrossRef]
- Tchero, H.; Teguo, M.T.; Lannuzel, A.; Rusch, E. Telerehabilitation for Stroke Survivors: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2018, 20, e10867. [Google Scholar] [CrossRef] [PubMed]
- Suso-Martí, L.; La Touche, R.; Herranz-Gómez, A.; Angulo-Díaz-Parreño, S.; Paris-Alemany, A.; Cuenca-Martínez, F. Effectiveness of Telerehabilitation in Physical Therapist Practice: An Umbrella and Mapping Review with Meta–Meta-Analysis. Phys. Ther. 2021, 101, pzab075. [Google Scholar] [CrossRef]
- Øra, H.P.; Kirmess, M.; Brady, M.C.; Sørli, H.; Becker, F. Technical Features, Feasibility, and Acceptability of Augmented Telerehabilitation in Post-stroke Aphasia—Experiences from a Randomized Controlled Trial. Front. Neurol. 2020, 11, 671. [Google Scholar] [CrossRef] [PubMed]
- Seron, P.; Oliveros, M.-J.; Gutierrez-Arias, R.; Fuentes-Aspe, R.; Torres-Castro, R.C.; Merino-Osorio, C.; Nahuelhual, P.; Inostroza, J.; Jalil, Y.; Solano, R.; et al. Effectiveness of Telerehabilitation in Physical Therapy: A Rapid Overview. Phys. Ther. 2021, 101, pzab053. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Universal Health Coverage (UHC). World Health Organization. 2019. Available online: https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-(uhc) (accessed on 15 May 2023).
- Chen, Y.; Chen, Y.; Zheng, K.; Dodakian, L.; See, J.; Zhou, R.; Chiu, N.; Augsburger, R.; McKenzie, A.; Cramer, S.C. A qualitative study on user acceptance of a home-based stroke telerehabilitation system. Top. Stroke Rehabil. 2020, 27, 81–92. [Google Scholar] [CrossRef] [PubMed]
- Theodoros, D.; Russell, T. Telerehabilitation: Current perspectives. Stud. Health Technol. Inform. 2008, 131, 191–209. [Google Scholar]
- Standing, C.; Standing, S.; McDermott, M.-L.; Gururajan, R.; Marvi, R.K. The Paradoxes of Telehealth: A Review of the Literature 2000–2015. Syst. Res. 2016, 35, 90–101. [Google Scholar] [CrossRef]
- Velez, M.; Lugo-Agudelo, L.H.; Patiño Lugo, D.F.; Glenton, C.; Posada, A.M.; Mesa Franco, L.F.; Negrini, S.; Kiekens, C.; Spir Brunal, M.A.; Bergquist, R.A.-S.; et al. Factors that influence the provision of home-based rehabilitation services for people needing rehabilitation: A qualitative evidence synthesis. Cochrane Database Syst. Rev. 2023, 2, CD014823. [Google Scholar]
- Auger, L.-P.; Moreau, E.; Côté, O.; Guerrera, R.; Rochette, A.; Kairy, D. Implementation of Telerehabilitation in an Early Supported Discharge Stroke Rehabilitation Program before and during COVID-19: An Exploration of Influencing Factors. Disabilities 2023, 3, 87–104. [Google Scholar] [CrossRef]
- World Health Organization. World Report on Disability Summary; World Health Organization: Geneva, Switzerland, 2011; pp. 1–23. [Google Scholar]
- Sandelowski, M. “What’s in a Name? Qualitative Description Revisited”. Res. Nurs. Health 2010, 33, 77–84. [Google Scholar] [CrossRef]
- Lambert, V.C.; Lambert, C.E. Qualitative descriptive research: An acceptable design. Pac. Rim Int. J. Nurs. Res. 2012, 16, 255–256. [Google Scholar] [CrossRef] [PubMed]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Damschroder, L.J.; Aron, D.C.; Keith, R.E.; Kirsh, S.R.; Alexander, J.A.; Lowery, J.C. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement. Sci. 2009, 4, 50. [Google Scholar] [CrossRef]
- Venkatesh, V.; Thong, J.Y.L.; Xu, X. Consumer Acceptance and Use of Information Technology: Extending the Unified Theory of Acceptance and Use of Technology. MIS Q. 2012, 361, 157. [Google Scholar] [CrossRef]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User Acceptance of Information Technology: Toward a Unified View. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef]
- Maruping, L.M.; Bala, H.; Venkatesh, V.; Brown, S.A. Going beyond intention: Integrating behavioral expectation into the unified theory of acceptance and use of technology. J. Assoc. Inf. Sci. Technol. 2017, 68, 623–637. [Google Scholar] [CrossRef]
- Chang, C.-M.; Liu, L.-W.; Huang, H.-C.; Hsieh, H.-H. Factors Influencing Online Hotel Booking: Extending UTAUT2 with Age, Gender, and Experience as Moderators. Information 2019, 10, 281. [Google Scholar] [CrossRef]
- Ain, N.; Kaur, K.; Waheed, M. The influence of learning value on learning management system use: An extension of UTAUT2. Inf. Dev. 2016, 32, 1306–1321. [Google Scholar] [CrossRef]
- Thérouanne, P.; Hayotte, M.; Halgand, F.; d’Arripe-Longueville, F. The Acceptability of Technology-Based Physical Activity Interventions in Postbariatric Surgery Women: Insights From Qualitative Analysis Using the Unified Theory of Acceptance and Use of Technology 2 Model. JMIR Hum. Factors 2023, 10, e42178. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Lin, Y.; Wei, Y.; Chen, X.; Wang, Y.; Zhang, L.; Zhou, M. Intervention of WeChat Group Guidance in Rapid Rehabilitation after Gynecological Laparoscopic Surgery. J. Healthc. Eng. 2021, 2021, 8914997. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Zhao, Z.; Guo, J.; Wang, Y.; Zhang, C.; Zheng, J.; Zou, Z.; Liu, W. Understanding Use Intention of mHealth Applications Based on the Unified Theory of Acceptance and Use of Technology 2 (UTAUT-2) Model in China. Int. J. Environ. Res. Public Health 2023, 20, 3139. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.-T.; Chao, C.-M.; Yu, C.-W.; Lin, F.-C.; Riboni, D. Extending the Utility of UTAUT2 for Hospital Patients’ Adoption of Medical Apps: Moderating Effects of e-Health Literacy. Mob. Inf. Syst. 2021, 2021, 8882317. [Google Scholar] [CrossRef]
- Palinkas, L.A.; Horwitz, S.M.; Green, C.A.; Wisdom, J.P.; Duan, N.; Hoagwood, K. Purposeful Sampling for Qualitative Data Collection and Analysis in Mixed Method Implementation Research. Adm. Policy Ment. Health 2015, 42, 533–544. [Google Scholar] [CrossRef]
- Coffey, A.J.; Atkinson, P.A. Making Sense of Qualitative Data: Complementary Research Strategies; SAGE Publications: Thousand Oaks, CA, USA, 1996. [Google Scholar]
- Kairy, D.; Tousignant, M.; Leclerc, N.; Cote, A.M.; Levasseur, M.; Researchers, T.T. The patient’s perspective of in-home telerehabilitation physiotherapy services following total knee arthroplasty. Int. J. Environ. Res. Public Health 2013, 10, 3998–4011. [Google Scholar] [CrossRef] [PubMed]
- Crepeau, E.B.; Garren, K.R. I looked to her as a guide: The therapeutic relationship in hand therapy. Disabil. Rehabil. 2011, 33, 872–881. [Google Scholar] [CrossRef] [PubMed]
- Caughlin, S.; Mehta, S.; Corriveau, H.; Eng, J.J.; Eskes, G.; Kairy, D.; Meltzer, J.; Sakakibara, B.M.; Teasell, R. Implementing Telerehabilitation After Stroke: Lessons Learned from Canadian Trials. Telemed. e-Health 2020, 26, 710–719. [Google Scholar] [CrossRef]
- Kairy, D.; Veras, M.; Archambault, P.; Hernandez, A.; Higgins, J.; Levin, M.F.; Poissant, L.; Raz, A.; Kaizer, F. Maximizing post-stroke upper limb rehabilitation using a novel telerehabilitation interactive virtual reality system in the patient’s home: Study protocol of a randomized clinical trial. Contemp. Clin. Trials 2016, 47, 49–53. [Google Scholar] [CrossRef]
- United Nations Educational, Scientific and Cultural Organization (UNESCO). UNESCO’s Internet Universality Indicators: A Framework for Assessing Internet Development. Available online: https://unesdoc.unesco.org/ark:/48223/pf0000367859 (accessed on 15 September 2023).
- Woolf, C.; Caute, A.; Haigh, Z.; Galliers, J.; Wilson, S.M.; Kessie, A.; Hirani, S.P.; Hegarty, B.; Marshall, J. A comparison of remote therapy, face to face therapy and an attention control intervention for people with aphasia: A quasi-randomised controlled feasibility study. Clin. Rehabil. 2016, 30, 359–373. [Google Scholar] [CrossRef]
- Sakakibara, B.M.; Lear, S.A.; Barr, S.I.; Benavente, O.; Goldsmith, C.H.; Silverberg, N.D.; Yao, J.; Eng, J.J. Development of a Chronic Disease Management Program for Stroke Survivors Using Intervention Mapping: The Stroke Coach. Arch. Phys. Med. Rehabil. 2017, 98, 1195–1202. [Google Scholar] [CrossRef]
- Sakakibara, B.M.; Lear, S.A.; Barr, S.I.; Benavente, O.; Goldsmith, C.H.; Silverberg, N.D.; Yao, J.; Eng, J.J. A telehealth intervention to promote healthy lifestyles after stroke: The stroke coach protocol. Int. J. Stroke 2018, 13, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Morse, H.; Biggart, L.; Pomeroy, V.; Rossit, S. Exploring perspectives from stroke survivors, carers and clinicians on virtual reality as a precursor to using telerehabilitation for spatial neglect post-stroke. Neuropsychol. Rehabil. 2022, 32, 707–731. [Google Scholar] [CrossRef] [PubMed]
- Kreider, C.M.; Hale-Gallardo, J.; Kramer, J.C.; Mburu, S.; Slamka, M.R.; Findley, K.E.; Myers, K.J.; Romero, S. Providers’ Shift to Telerehabilitation at the U.S. Veterans Health Administration during COVID-19: Practical Applications. Front. Public Health 2022, 10, 831762. [Google Scholar] [CrossRef] [PubMed]
- McCoyd, J.L.M.; Curran, L.; Candelario, E.; Findley, P. “There is Just a Different Energy”: Changes in the Therapeutic Relationship with the Telehealth Transition. Clin. Soc. Work J. 2022, 50, 325–336. [Google Scholar] [CrossRef]
- Anderson, M.; Dexter, B.; Hancock, A.; Hoffman, N.; Kerschke, S.; Hux, K.; Aggarwal, D. Implementing Team-Based Post-Stroke Telerehabilitation: A Case Example. Int. J. Telerehabil. 2022, 14, e6438. [Google Scholar] [CrossRef]
- Wavrock, D.; Schellenberg, G.; Schimmele, C. Canadians’ use of the Internet and digital technologies before and during the COVID-19 pandemic. Stat. Can. 2022, 2. [Google Scholar] [CrossRef]
- Kruse, C.S.; Karem, P.; Shifflett, K.; Vegi, L.; Ravi, K.; Brooks, M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J. Telemed. Telecare 2018, 24, 4–12. [Google Scholar] [CrossRef]
- Laperrière, A. Les critères de scientificité des méthodes qualitatives. In Enjeux Épistémologiques et Méthodologiques; Poupart, J.-P.D.J., Groulx, L.-H., Laperrière, A., Mayer, R., Pires, A.P., Eds.; La Recherche Qualitative: Boucherville, QC, Canada, 1997; pp. 365–390. [Google Scholar]
 ↔) show a dynamic, reciprocal relationship between two constructs, indicating influence in both directions. One-way arrows (→ ⇢) depict a unilateral relationship, emphasizing that one construct can impact the other without direct reciprocity.
↔) show a dynamic, reciprocal relationship between two constructs, indicating influence in both directions. One-way arrows (→ ⇢) depict a unilateral relationship, emphasizing that one construct can impact the other without direct reciprocity.
 ↔) show a dynamic, reciprocal relationship between two constructs, indicating influence in both directions. One-way arrows (→ ⇢) depict a unilateral relationship, emphasizing that one construct can impact the other without direct reciprocity.
↔) show a dynamic, reciprocal relationship between two constructs, indicating influence in both directions. One-way arrows (→ ⇢) depict a unilateral relationship, emphasizing that one construct can impact the other without direct reciprocity. 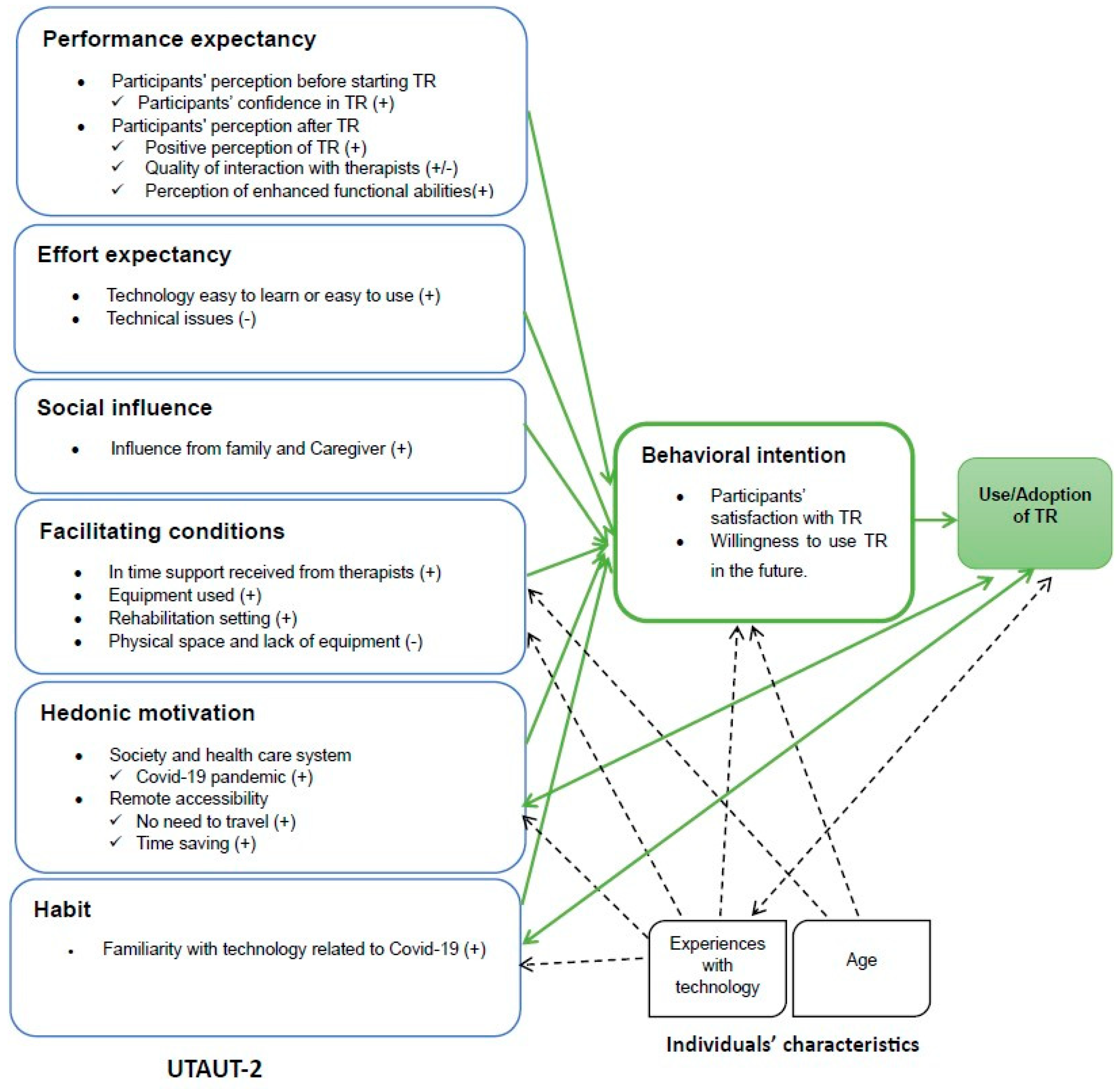
| Participants ID | Age (Years) | Genre | Level of Education | Type of Stroke | ESD Duration with TR Modality (Weeks) | Rehabilitation Disciplines Involved | Disciplines Using only TR/Number of TR Session/Week | Time Since Stroke at the Time of the Interview (Months) |
|---|---|---|---|---|---|---|---|---|
| Individuals With Stroke (IWS) | ||||||||
| IWS-1 | 76 | Male | University | Ischemic | 5 | PT, OT, SLP, SW; nurse, Psy | - OT/5/week - PT/5/week - SLP/5/week | 12 |
| IWS-2 | 77 | Female | University | Ischemic | 5 | OT, kinesiology | - OT/3/week - Kinesiology/3/week | 11 |
| IWS-3 | 65 | Male | Secondary | Ischemic | 5 | Psy, PT, SLP | - SLP/3/week | 12 |
| IWS-4 | 72 | Male | University | Ischemic | 6 | OT, SLP, SW, psy, PT | - OT/3/week - PT/3/week - SLP/3/week - SW/2/6weeks | 12 |
| IWS-5 | 50 | Female | College-level | Hemorrhagic | 5 | OT, PT, nurse, SW, art therapy | - OT/5/week - PT/5/week - Art therapy/5/week - Nurse/2/5weeks | 7 |
| IWS-6 | 66 | Male | University | Ischemic | 4 | OT, PT, SW | - OT/3/week - SW/3/week | 8 |
| Caregivers (C) | ||||||||
| C1 (IWS-5) | 42 | Male | Secondary | N/A | N/A | N/A | N/A | N/A |
| C2 (IWS-2) | 66 | Female | University | N/A | N/A | N/A | N/A | N/A |
| C3 (IWS-4) | 77 | Female | Vocational diploma | N/A | N/A | N/A | N/A | N/A |
| Factors Facilitating the Acceptance and Use of Telerehabilitation | Barriers to the Acceptance and Use of Telerehabilitation |
|---|---|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ouédraogo, F.; Auger, L.-P.; Moreau, E.; Côté, O.; Guerrera, R.; Rochette, A.; Kairy, D. Acceptability of Telerehabilitation: Experiences and Perceptions by Individuals with Stroke and Caregivers in an Early Supported Discharge Program. Healthcare 2024, 12, 365. https://doi.org/10.3390/healthcare12030365
Ouédraogo F, Auger L-P, Moreau E, Côté O, Guerrera R, Rochette A, Kairy D. Acceptability of Telerehabilitation: Experiences and Perceptions by Individuals with Stroke and Caregivers in an Early Supported Discharge Program. Healthcare. 2024; 12(3):365. https://doi.org/10.3390/healthcare12030365
Chicago/Turabian StyleOuédraogo, Fatimata, Louis-Pierre Auger, Emmanuelle Moreau, Odile Côté, Rosalba Guerrera, Annie Rochette, and Dahlia Kairy. 2024. "Acceptability of Telerehabilitation: Experiences and Perceptions by Individuals with Stroke and Caregivers in an Early Supported Discharge Program" Healthcare 12, no. 3: 365. https://doi.org/10.3390/healthcare12030365
APA StyleOuédraogo, F., Auger, L.-P., Moreau, E., Côté, O., Guerrera, R., Rochette, A., & Kairy, D. (2024). Acceptability of Telerehabilitation: Experiences and Perceptions by Individuals with Stroke and Caregivers in an Early Supported Discharge Program. Healthcare, 12(3), 365. https://doi.org/10.3390/healthcare12030365








