Nurses’ Attitudes and Perceptions Regarding Suicidal Patients: A Quasi-Experimental Study of Depression Management Training
Abstract
1. Introduction
The Current Study
2. Methods
2.1. Design
2.2. Procedure
2.3. Measures
2.3.1. The Vignettes
Nadav is 45 years old, married with three small children, and working full-time as a hospital security guard. About two months ago, he fell and injured his right knee during work hours. Since then, he has been limited in his walking ability and suffers from continuous pain. Following the fall, he took a long sick leave and stayed at home. In the last two weeks, he has returned to part-time work. Nadav is scheduled to undergo orthopedic surgery on his injured knee in about a month, and he is coming to your clinic for an ECG before the surgery. Nadav has a BMI of 30 and unbalanced diabetes. He is aware of his excess weight and diabetes, but he does not adhere to a healthy diet or exercise due to his working late shifts. His blood tests reveal that in the last three years, Nadav has suffered from low hemoglobin levels and a lack of vitamin B12.
2.3.2. Manipulation Check
2.3.3. Willingness to Refer to and Willingness to Inquire about Mental State and Suicide Risk
- The degree of willingness to refer (“To what extent would you be willing to refer the patient to a social worker/psychologist/physician regarding his mental state?”);
- The degree of willingness to ask the patient about his mental state (“To what extent would you be willing to ask the patient about his mental state?”);
- The degree of willingness to ask the patient about future suicide plans (“To what extent would you be willing to ask the patient about his future suicide plans?”).
2.3.4. Attitudes and Self-Competence Regarding Depression and Suicide Risk Assessment
Attitudes Regarding Depression Assessment
Attitudes Regarding Suicide Risk Assessment
Self-Competence Regarding Depression Assessment
Self-Competence Regarding Suicide Risk Assessment
2.3.5. Demographics, Clinical Training and Practice Characteristics
2.4. Data Analysis
3. Results
3.1. Description of the Sample
3.2. Manipulation Check
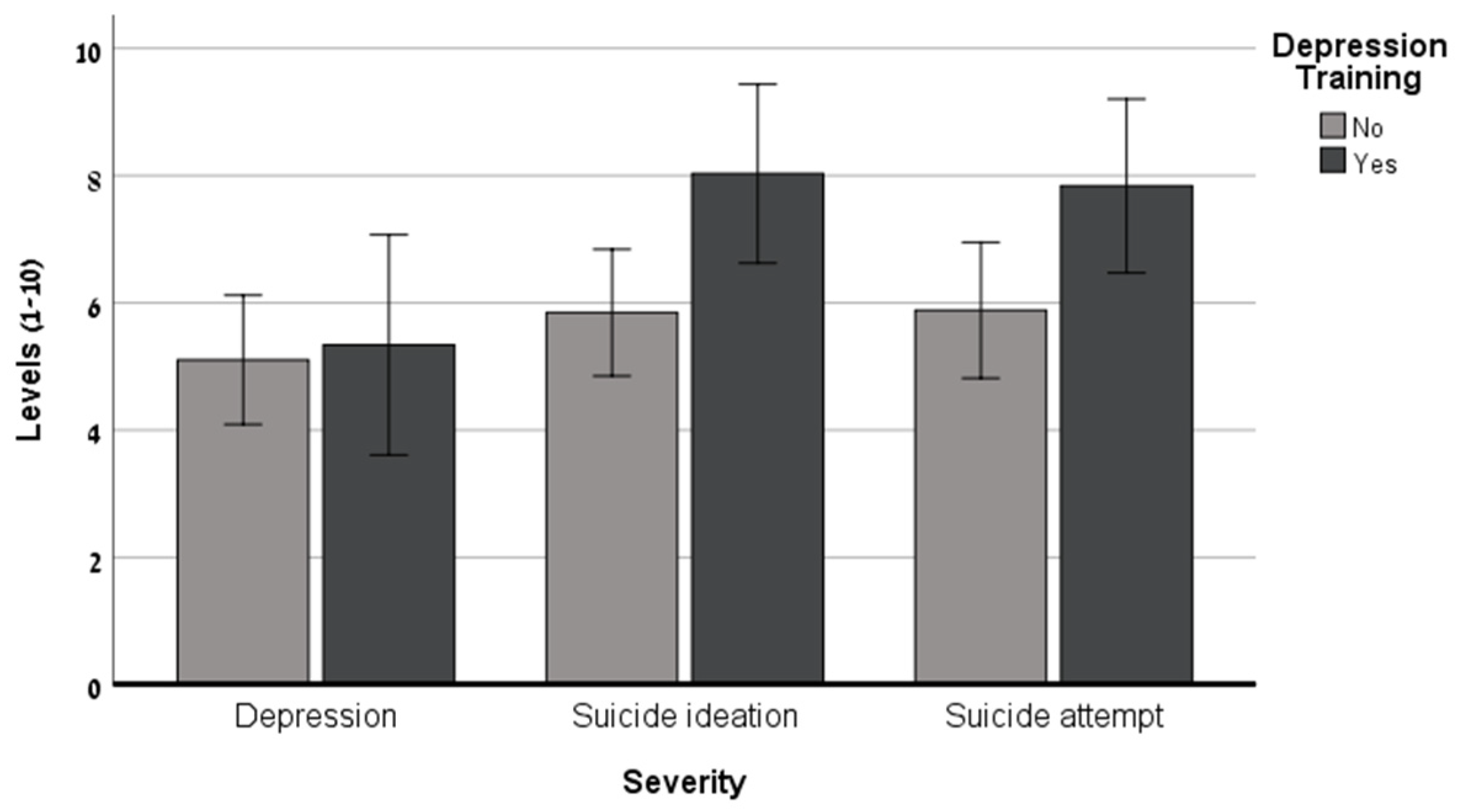
3.3. The Effect of Suicide Severity and Nurses’ Training in Depression Management
3.4. Nurses’ Attitudes toward Suicide Assessment as a Function of Their Training in Depression Management
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Sustainable Development Goals (SDGs). Available online: https://www.who.int/mental_health/suicide-prevention/SDGs/en/ (accessed on 8 August 2023).
- Mann, J.J.; Michel, C.A.; Auerbach, R.P. Improving suicide prevention through evidence-based strategies: A systematic review. Am. J. Psychiatry 2021, 178, 611–624. [Google Scholar] [CrossRef] [PubMed]
- Turecki, G.; Brent, D.A. Suicide and suicidal behavior. Lancet 2016, 387, 1227–1239. [Google Scholar] [CrossRef] [PubMed]
- Mann, J.J.; Apter, A.; Bertolote, J.; Beautrais, A.; Currier, D.; Haas, A.; Hegerl, U.; Lonnqvist, J.; Malone, K.; Marusic, A.; et al. Suicide prevention strategies: A systematic review. JAMA 2005, 294, 2064–2074. [Google Scholar] [CrossRef] [PubMed]
- Zalsman, G.; Hawton, K.; Wasserman, D.; van Heeringen, K.; Arensman, E.; Sarchiapone, M.; Carli, V.; Hoschl, C.; Barzilay, R.; Balazs, J.; et al. Suicide prevention strategies revisited: 10–year systematic review. Lancet Psychiatry 2016, 3, 646–659. [Google Scholar] [CrossRef]
- Hasin, D.S.; Sarvet, A.L.; Meyers, J.L.; Saha, T.D.; Ruan, W.J.; Stohl, M.; Grant, B.F. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry 2018, 75, 336–346. [Google Scholar] [CrossRef] [PubMed]
- Yonemoto, N.; Kawashima, Y.; Endo, K.; Yamada, M. Gatekeeper training for suicidal behaviors: A systematic review. J. Affect. Disord. 2019, 246, 506–514. [Google Scholar] [CrossRef] [PubMed]
- Graves, J.M.; Mackelprang, J.L.; Van Natta, S.E.; Holliday, C. Suicide prevention training: Policies for health care professionals across the United States as of October 2017. Am. J. Public Health 2018, 108, 760–768. [Google Scholar] [CrossRef] [PubMed]
- Hauge, L.J.; Stene-Larsen, K.; Grimholt, T.K.; Øien-Ødegaard, C.; Reneflot, A. Use of primary health care services prior to suicide in the Norwegian population 2006–2015. BMC Health Serv. Res. 2018, 18, 619. [Google Scholar] [CrossRef]
- Stene-Larsen, K.; Reneflot, A. Contact with primary and mental health care prior to suicide: A systematic review of the literature from 2000 to 2017. Scand. J. Public Health 2019, 47, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Sela, Y.; Grinberg, K.; Shapiro, Y.; Nissanholtz-Ganot, R. A cross-sectional study on preferred employment settings of final-year nursing students in Israel. Hum. Resour. Health 2020, 18, 1–9. [Google Scholar] [CrossRef]
- Bolster, C.; Holliday, C.; Oneal, G.; Shaw, M. Suicide assessment and nurses: What does the evidence show? Online J. Issues Nurs. 2015, 20, 81–87. [Google Scholar] [CrossRef]
- Lees, D.; Procter, N.; Fassett, D. Therapeutic engagement between consumers in suicidal crisis and mental health nurses. Int. J. Ment. Health Nurs. 2014, 23, 306–315. [Google Scholar] [CrossRef] [PubMed]
- Mughal, F.; Gorton, H.C.; Michail, M.; Robinson, J.; Saini, P. Suicide prevention in primary care. Crisis 2021, 42, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Boukouvalas, E.; El-Den, S.; Murphy, A.L.; Salvador-Carulla, L.; O’Reilly, C.L. Exploring health care professionals’ knowledge of, attitudes towards, and confidence in caring for people at risk of suicide: A systematic review. Arch. Suicide Res. 2019, 24, S1–S31. [Google Scholar] [CrossRef] [PubMed]
- Jansson, L.; Graneheim, U.H. Nurses’ experiences of assessing suicide risk in specialized mental health outpatient care in rural areas. Issues Ment. Health Nurs. 2018, 39, 554–560. [Google Scholar] [CrossRef] [PubMed]
- Rukundo, G.Z.; Wakida, E.K.; Maling, S.; Kaggwa, M.M.; Sserumaga, B.M.; Atim, L.M.; Atuhaire, C.D.; Obua, C. Knowledge, attitudes, and experiences in suicide assessment and management: A qualitative study among primary health care workers in southwestern Uganda. BMC Psychiatry 2022, 22, 605. [Google Scholar] [CrossRef] [PubMed]
- Valente, S. Nurses’ psychosocial barriers to suicide risk management. Nurs. Res. Pract. 2011, 2011, 650765. [Google Scholar] [CrossRef]
- Wärdig, R.E.; Hultsjö, S.; Lind, M.; Klavebäck, I. Nurses’ experiences of suicide prevention in primary health care (PHC)—A qualitative interview study. Issues Ment. Health Nurs. 2022, 43, 903–912. [Google Scholar] [CrossRef]
- Saunders, K.E.; Hawton, K.; Fortune, S.; Farrell, S. Attitudes and knowledge of clinical staff regarding people who self-harm: A systematic review. J. Affect. Disord. 2012, 139, 205–216. [Google Scholar] [CrossRef]
- Ferguson, M.; Reis, J.; Rabbetts, L.; McCracken, T.; Loughhead, M.; Rhodes, K.; Wepa, D.; Procter, N. The impact of suicide prevention education programs for nursing students: A systematic review. Int. J. Ment. Health Nurs. 2020, 29, 756–771. [Google Scholar] [CrossRef]
- Dabkowski, E.; Porter, J.E. An exploration into suicide prevention initiatives for mental health nurses: A systematic literature review. Int. J. Ment. Health Nurs. 2021, 30, 610–623. [Google Scholar] [CrossRef] [PubMed]
- Milner, A.J.; Carter, G.; Pirkis, J.; Robinson, J.; Spittal, M.J. Letters, green cards, telephone calls and postcards: Systematic and meta-analytic review of brief contact interventions for reducing self-harm, suicide attempts and suicide. Br. J. Psychiatry 2015, 206, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Morris, R.; Gask, L.; Webb, R.; Dixon, C.; Appleby, L. The effects on suicide rates of an educational intervention for front-line health professionals with suicidal patients (the STORM Project). Psychol. Med. 2005, 35, 957–960. [Google Scholar] [CrossRef] [PubMed]
- Pisani, A.R.; Cross, W.F.; Gould, M.S. The assessment and management of suicide risk: State of workshop education. Suicide Life Threat. Behav. 2011, 41, 255–276. [Google Scholar] [CrossRef] [PubMed]
- Brown, L.A.; Boudreaux, E.D.; Arias, S.A.; Miller, I.W.; May, A.M.; Camargo, C.A.; Bryan, C.J.; Armey, M.F. C-SSRS performance in emergency department patients at high risk for suicide. Suicide Life Threat. Behav. 2020, 50, 1097–1104. [Google Scholar] [CrossRef] [PubMed]
- Bresin, K.; Sand, E.; Gordon, K.H. Non-suicidal self-injury from the observer’s perspective: A vignette study. Arch. Suicide Res. 2013, 17, 185–195. [Google Scholar] [CrossRef] [PubMed]
- Levi-Belz, Y.; Barzilay, S.; Levy, D.; David, O. To treat or not to treat: The effect of hypothetical patients’ suicidal severity on therapists’ willingness to treat. Arch. Suicide Res. 2020, 24, 355–366. [Google Scholar] [CrossRef]
- Levi-Belz, Y.; Gamliel, E. The effect of perceived burdensomeness and thwarted belongingness on therapists’ assessment of patients’ suicide risk. Psychother. Res. 2016, 26, 436–445. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Carbin, M.G. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin. Psychol. Rev. 1998, 8, 77–100. [Google Scholar] [CrossRef]
- Posner, K.; Brown, G.K.; Stanley, B.; Brent, D.A.; Yershova, K.V.; Oquendo, M.A.; Currier, G.W.; Melvin, G.A.; Greenhill, L.; Shen, S.; et al. The Columbia–Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am. J. Psychiatry 2011, 168, 1266–1277. [Google Scholar] [CrossRef]
- Hunter, N. Clinical trainees’ personal history of suicidality and the effects on attitudes towards suicidal patients. New School Psychol. Bull. 2015, 13, 38–46. [Google Scholar]
- Norheim, A.B.; Grimholt, T.K.; Ekeberg, Ø. Attitudes towards suicidal behaviour in outpatient clinics among mental health professionals in Oslo. BMC Psychiatry 2013, 13, 90. [Google Scholar] [CrossRef] [PubMed]
- Samuelsson, M.; Åsberg, M. Training program in suicide prevention for psychiatric nursing personnel enhance attitudes to attempted suicide patients. Int. J. Nurs. Stud. 2002, 39, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Uncapher, H.; Areán, P.A. Physicians are less willing to treat suicidal ideation in older patients. J. Am. Geriatr. Soc. 2000, 48, 188–192. [Google Scholar] [CrossRef] [PubMed]
- Almaliah-Rauscher, S.; Ettinger, N.; Levi-Belz, Y.; Givon, Y. “Will you treat me? I’m suicidal!” The effect of patient gender, suicidal severity, and therapist characteristics on the therapist’s likelihood to treat a hypothetical suicidal patient. Clin. Psychol. Psychother. 2020, 27, 278–287. [Google Scholar] [CrossRef]
- Smith, M.; Stolder, M.E.; Jaggers, B.; Liu, M.F.; Haedtke, C. Depression training in nursing homes: Lessons learned from a pilot study. Issues Ment. Health Nurs. 2013, 34, 90–102. [Google Scholar] [CrossRef][Green Version]
- Brunero, S.; Smith, J.; Bates, E.; Fairbrother, G. Health professionals’ attitudes towards suicide prevention initiatives. J. Psychiatr. Ment. Health Nurs. 2008, 15, 588–594. [Google Scholar] [CrossRef]
- Elzinga, E.; de Kruif, A.J.; de Beurs, D.P.; Beekman, A.T.F.; Franx, G.; Gilissen, R. Engaging primary care professionals in suicide prevention: A qualitative study. PLoS ONE 2020, 15, e0242540. [Google Scholar] [CrossRef]
- Coppens, E.; Van Audenhove, C.; Iddi, S.; Arensman, E.; Gottlebe, K.; Koburger, N.; Hegerl, U. Effectiveness of community facilitator training in improving knowledge, attitudes, and confidence in relation to depression and suicidal behavior: Results of the OSPI-Europe intervention in four European countries. J. Affect. Disord. 2014, 165, 142–150. [Google Scholar] [CrossRef]
- Saini, V.K.; Gehlawat, P.; Gupta, T. Evaluation of knowledge and competency among nurses after a brief suicide prevention educational program: A pilot study. J. Fam. Med. Prim. Care 2020, 9, 6018–6022. [Google Scholar] [CrossRef]
- Harmer, B.; Lee, S.; Duong, T.V.H.; Saadabadi, A. Suicidal Ideation; StatPearls Publishing: Treasure Island, CA, USA, 2023. [Google Scholar]
- Wärdig, R.; Engström, A.S.; Carlsson, A.; Wärdig, F.; Hultsjö, S. Saving lives by asking questions: Nurses’ experiences of suicide risk assessment in telephone counselling in primary health care. Prim. Health Care Res. Dev. 2022, 23, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Solin, P.; Tamminen, N.; Partonen, T. Suicide prevention training: Self-perceived competence among primary healthcare professionals. Scand. J. Prim. Health Care 2021, 39, 332–338. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Nurses Association (APNA). Psychiatric-Mental Health Nurse Essential Competencies for Assessment and Management of Individuals at Risk for Suicide. Available online: https://sprc.org/online-library/psychiatric-mental-health-nurse-essential-competencies-for-assessment-and-management-of-individuals-at-risk-for-suicide/ (accessed on 8 August 2023).
- UCL. National Collaborating Centre for Mental Health, Self-Harm and Suicide Prevention Competence Framework: Community and Public Health. Available online: https://www.ucl.ac.uk/pals/research/clinical-educational-and-health-psychology/research-groups/core/competence-frameworks/self (accessed on 8 August 2023).
- Santos, D.C.R.; Lima, R.T.C.; Domingos, T.S.; Alencar, R.A. Professional attitudes towards suicidal behavior in primary health care: A quasi-experimental study. Texto Contexto Enferm. 2022, 31. [Google Scholar] [CrossRef]
- Rayner, G.; Blackburn, J.; Edward, K.L.; Stephenson, J.; Ousey, K. Emergency department nurse’s attitudes towards patients who self-harm: A meta-analysis. Int. J. Ment. Health Nurs. 2019, 28, 40–53. [Google Scholar] [CrossRef]
- Yamaguchi, S.; Mino, Y.; Uddin, S. Strategies and future attempts to reduce stigmatization and increase awareness of mental health problems among young people: A narrative review of educational interventions. Psychiatry Clin. Neurosci. 2011, 65, 405–415. [Google Scholar] [CrossRef]
- Bachmann, S. Epidemiology of suicide and the psychiatric perspective. Int. J. Environ. Res. Public. Health 2018, 15, 1425. [Google Scholar] [CrossRef]


| Variables | N | % | Mean | SD | Range |
|---|---|---|---|---|---|
| Sex | 139 | ||||
| Male | 16 | 11.5 | |||
| Female | 123 | 88.5 | |||
| Birth country | 139 | ||||
| Masked- | 104 | 74.8 | |||
| Masked- | 35 | 25.2 | |||
| Religion | 139 | ||||
| Masked | 121 | 87.1 | |||
| Masked | 18 | 12.9 | |||
| Work | 139 | ||||
| Community care | 130 | 93.5 | |||
| Other | 9 | 6.5 | |||
| Age | 138 | 41.58 | 10.46 | 24–62 | |
| Professional seniority | 134 | 15.33 | 11.23 | 1–42 |
| Suicide Severity Conditions | Statistical Analysis | ||||||
|---|---|---|---|---|---|---|---|
| Outcome Measure | Training in Depression Management | Depression (n = 43) M (SD) | SI (n = 50) M (SD) | SA (n = 50) M (SD) | Main Effect—Severity | Main Effect—Training | Main Effect—Interaction |
| Willingness to refer to mental health professional | No (n = 90) | 6.33 | 7.63 | 7.29 | F = 6.65 p < 0.002 Eta2 = 0.09 | F = 8.15 p < 0.005 Eta2 = 0.06 | F = 1.36 p = 0.258 Eta2 = 0.02 |
| (2.84) | (2.67) | (2.51) | |||||
| Yes (n = 54) | 6.64 | 9.00 | 9.44 | ||||
| (2.84) | (2.67) | (2.51) | |||||
| Willingness to ask the patient about mental state | No (n = 90) | 5.23 | 5.56 | 5.61 | F = 3.21 p < 0.05 Eta2 = 0.04 | F = 15.59 p < 0.001 Eta2 = 0.10 | F = 1.74 p = 0.178 Eta2 = 0.02 |
| (2.87) | (2.95) | (2.67) | |||||
| Yes (n = 54) | 5.82 | 8.00 | 8.44 | ||||
| (2.92) | (2.81) | (2.33) | |||||
| Willingness to ask the patient about suicide plan | No (n = 90) | 2.90 | 4.45 | 4.79 | F = 11.77 p < 0.001 Eta2 = 0.15 | F = 23.73 p < 0.001 Eta2 = 0.14 | F = 2.34 p = 0.100 Eta2 = 0.03 |
| (2.59) | (3.56) | (3.40) | |||||
| Yes (n = 54) | 3.82 | 8.33 | 8.00 | ||||
| (2.89) | (2.94) | (3.28) | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sela, Y.; Levi-Belz, Y. Nurses’ Attitudes and Perceptions Regarding Suicidal Patients: A Quasi-Experimental Study of Depression Management Training. Healthcare 2024, 12, 284. https://doi.org/10.3390/healthcare12030284
Sela Y, Levi-Belz Y. Nurses’ Attitudes and Perceptions Regarding Suicidal Patients: A Quasi-Experimental Study of Depression Management Training. Healthcare. 2024; 12(3):284. https://doi.org/10.3390/healthcare12030284
Chicago/Turabian StyleSela, Yael, and Yossi Levi-Belz. 2024. "Nurses’ Attitudes and Perceptions Regarding Suicidal Patients: A Quasi-Experimental Study of Depression Management Training" Healthcare 12, no. 3: 284. https://doi.org/10.3390/healthcare12030284
APA StyleSela, Y., & Levi-Belz, Y. (2024). Nurses’ Attitudes and Perceptions Regarding Suicidal Patients: A Quasi-Experimental Study of Depression Management Training. Healthcare, 12(3), 284. https://doi.org/10.3390/healthcare12030284







