Abstract
This research analyzes the dental hygiene habits of schoolchildren from parents’ perspectives, using the STEPS approach recommended by the World Health Organization. The key points of oral health care in children include the role of the family in encouraging and maintaining proper oral hygiene practices. This study aimed to assess the oral hygiene practices of schoolchildren with on-site dentists in Romania. Additionally, it sought to establish correlations between these behaviors and the educational levels of the adults with whom they live with. The participants were selected from the zero grade to the eighth grade, totaling 3843students. Statistical analysis involved the application of Fisher’s Exact Test and Z-tests with Bonferroni correction. Multinominal and binominal logistic regression models were employed to predict the impact of parents’ education on children’s oral health status and behavior. The oral health status of children evaluated by parents as poor was more frequent in children whose parents had a primary or gymnasium education (p < 0.001). Female adults with a university education evaluated the gum health of their children as very good to a much greater extent (41.7%, p < 0.001). Regarding the use of auxiliary means, the majority of parents with a university education mentioned that their children use dental floss (26.4% females/27.4% males) (p < 0.001), compared to those with primary education, where the percentage was only (1.2% males/3.5% females) (p < 0.001). The results of this study highlight that the education level of the adults with whom the children live with influences the perception of the teeth and gums health status, the frequency of oral hygiene, the use of fluoride toothpaste, and auxiliary brushing aids.
1. Introduction
The state of oral health is influenced by oral conditions that cause discomfort or tooth loss, having a negative impact on the appearance, quality of life, or nutritional intake influencing the growth and development of children. Caries and gum disease are the most widespread health problems, affecting more than 80% of children in some countries [1]. Oral conditions limit participation in school, professional, or domestic activities, leading to absences from school or work, which causes a significant loss of school or work hours globally. Moreover, the psychosocial impact of these problems negatively affects the quality of life [2].
It is useful to manage the factors that have an impact on children’s oral health in order to develop and implement supporting public health actions focused on children and parenting behaviors in an effort to provide them optimal oral care and a better quality of life [3]. Schools offer a favorable framework for promoting oral health because, in the world, more than a billion children are enrolled in educational institutions. School health education programs can also contribute to the improvement and well-being of families, school staff, and community members [1].
It is universally accepted that socioeconomic level influences health status [4]. This also applies to oral health [5]. Economic standing is associated with a higher risk of carious lesions [6]. Educating parents and children about tooth decay prevention has long been considered a fundamental element of any dental treatment plan [7]. That is why parents’ knowledge of oral health and appropriate oral health care practices for children are very important [8]. The increased incidence of dental caries is not solely determined by biological factors interacting with the causative microorganisms. Carious lesions are also associated with socioeconomic conditions, education, and eating habits [9].
It has been shown that the incidence of carious lesions is higher in disadvantaged cities in certain countries [10,11]. Key aspects of oral health care in pediatric patients include factors that highlight a family’s ability to promote and maintain appropriate oral hygiene behaviors. Parents with poor oral hygiene habits are risk factors for dental caries in their children [12].
In addition to this determinants, oral health is related to lifestyle, which is an important factor in most chronic diseases. A protective element of oral health is proper oral hygiene and age-appropriate exposure to fluoride [2]. The effects of fluoride on the prevalence of dental caries incidence is confirmed, and the correlation with socio-economic status is validated [13]. The most significant way to benefit from the positive effects of fluoride is the use of fluoride-containing toothpaste [14]. Numerous studies support the promotion of tooth brushing with fluoridated toothpaste in the context of oral health programs conducted in schools [15,16,17].
Drinking water, beverages that are made with fluoridated water, and certain foods are major sources of fluoride in general. The American Dental Association suggests an ideal concentration of 0.7 ppm fluoride, equivalent to 0.7 mg fluoride per liter of water, in drinking water [18]. Since, in general, drinking water sources in Romania are low in fluoride, the probability of suffering an overdose through the use of topical treatments is minimal [19]. Therefore, it is imperative to assess exposure to risk factors using appropriate surveys to identify the vulnerable population, as well as the behaviors with the highest risk potential that require addressing. This must be performed before planning and implementing oral health promotion programs for children [20]. There is a lack of centralized national studies providing information on the oral health status of schoolchildren in Romania [21]. Information regarding oral health education represents the means by which a shift in dental treatments can be achieved, moving from invasive therapy to prevention [21].
In Romania, the dental care system is both public and private. According to data provided by National Institute of Public Health, in the year 2021, approximately 20,000 dentists were registered in Romania, with around 20% of them working in the public system. Regarding educational institutions, only 3% of the educational units have a school office and a dentist [22]. This percentage is too small to ensure preventive, diagnostic, and treatment dental procedures for the school population.
The present study aimed to carry out a detailed analysis of the oral hygiene behavior of students in relation to the level of education of the adult with whom the child lives and the family’s living environment.
2. Materials and Methods
2.1. Study Design and Sample Selection of Participants
The educational system in Romania is organized into 9 educational levels, called the International Standard Classification of Education (ISCED 0 to 8): early education (ISCED 0), primary education (ISCED 1), lower secondary education (ISCED 2), upper secondary education (ISCED 3), non-university tertiary education (ISCED 4), higher education (ISCED 5–8) [23].
In this study, carried out in the period 2022–2023, students enrolled in public educational institutions, from the educational level ISCED level 1 (grade 0 to grade 4) and ISCED level 2 (grade 5 to grade 8), were selected. Students were selected from 35 counties (NUTS 3) and the 6 sectors of Bucharest (capital of the country), from schools where there is a dental practice authorized and school dentist, according to the methodology developed by the National Institute of Public Health in Romania (Figure 1) [24].
Figure 1.
Nomenclature of Territorial Units for Statistics (NUTS)—the levels for Romania.
A minimum of 2 schools were selected from each county and from each sector of Bucharest and a minimum of 5 children from each age category. In accordance with Romanian regulations, children are enrolled in the school unit in the family’s area of residence, but there are also situations in which parents can choose another educational unit outside the school district [25]. According to the situation analysis carried out by the National Institute of Public Health, in Romania there are 467 school dental offices in the urban environment [22], and Bucharest is the most populated city in Romania with 137 school dental offices [26]. The participants were selected from grade 0tograde 8, with a total of 3843 students, respectively, parents/legal representatives who completed the informed consent form for participation of the student in the study, as well as the evaluation questionnaire related to the oral health status of the child. For children 7 years to 14 years, the age distribution was relatively homogeneous, the most frequent age categories being 9 years (11.9%) and 10 years (11.9%). The mean age was 10.56 ± 2.61 years, the median being 11 years (interpercentile range: 8–13 years); 53.4% are females.
2.2. Ethical Consideration
Before implementation, the study was submitted to the Research Ethics Committee of the “Carol Davila” University of Medicine and Pharmacy Bucharest. It was approved in accordance with the Methodology for Monitoring Oral Health in Schools, having the registration number 36927/29.11.2022. Written consent was obtained from the legal representative of the children participating in the study.
2.3. The Translation and the Adaptation of the Questionnaire
The data were obtained by applying a questionnaire dedicated to children, developed by the World Health Organization (WHO) and presented within the methodology published in 2013 [27]. According to the methodology of the present study, the self-administered questionnaire was filled out by the parents of the students who previously completed the informed consent form regarding the child’s participation in the study. Prior to application, the STEPS questionnaire was validated and adapted to the target group, the parents of students in grades 0–8, according to the WHO methodology from 2020 [28]. In this sense, the English version of the questionnaire was translated into Romanian in the first stage by two bilingual Romanian translators, then the two translations were compared in a face-to-face meeting, where the authors of the study consulted with two specialists in education and sociology and made sure that the way each question was formulated did not change the meaning of the answer options. The retroversion was carried out by an independent translator, from Romanian to English, then the version administered to the respondents was completed. This version was tested among 20 adults who were asked to rate the clarity and difficulty of the questions and answers. This did not lead to the need for any changes. The questionnaire consisted of items related to: general information (age and gender of the child, class, as well as socio-demographic data, background and level of education of the parents); parents’ perception of their children’s oral health (teeth and gums) and information related to their children’s personal oral hygiene; frequency of tooth brushing; means used for oral hygiene; including auxiliary aids; use of toothpaste; parents’ knowledge of using fluoride toothpaste.
3. Results
The distribution of the participants analyzed in the study related to the children’s place of origin is presented in Figure 2. Most children come from Bucharest (16.81%), and a percentage of 89.5% reside in the urban environment.
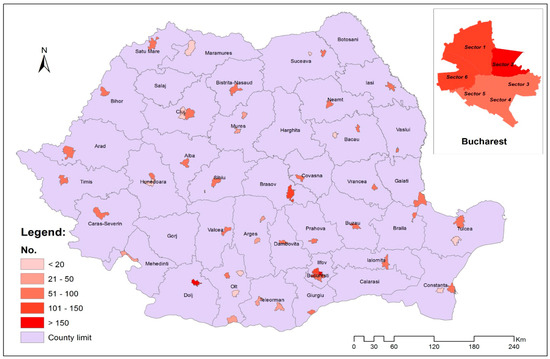
Figure 2.
The territorial distribution of the studied sample by counties (NUTS 3).
Among the parents of the children participating in the study, and out of the majority of female adults with whom they lived, 62.4%, had a university education, 29.6% ahigh school education, 4.8% a secondary school education, 0.4% of the children did not live with a female adult, and 206 did not answer this question. According to the results, the majority of male adults had a high school education (35.6%) or a university education (51.3%), 5.5% of children did not live with a male adult, and 216 preferred not to answer.
The statistical analysis was performed using IBM SPSS Statistics 25 and illustrated using Microsoft Office Excel/Word 2021. Qualitative variables were expressed in absolute terms or as percentages, and they were tested between groups using Fisher’s Exact Test. Z-tests with Bonferroni correction were conducted to further detail the results obtained in contingency table.
Very good health status was significantly more common in children whose male adults had a university education (33.2%) compared to those with a high school/gymnasium or primary education. Health status perceived as very good was significantly more frequent in children whose adults, both female and male, had a university education rather than high school or gymnasium. Excellent health status was significantly more common in children whose female adults had a university education compared to those with a high school education.
The poor oral health status of children’s teeth assessed by parents was significantly more frequent in children whose parents have primary or gymnasium education (p < 0.001) (Table 1).

Table 1.
The perception of children’s dental health related to the socioeconomic status of the parents.
The perception of gum health as poor was significantly more frequent in children whose male adults had a gymnasium education (9.2%), than a high school or university education (1.9%/0.6%).
Female adults with a university education rated the health status of their children’s gums as very good in a much higher proportion (41.7%, p < 0.001), compared to those with a high school or gymnasium education (Table 2).

Table 2.
Perception of oral health status of children’s gums according to parents’ socioeconomic status.
Regarding differences in gingival health, it has been noted that very good status was significantly more common in children whose male adults had a university education (42.1%), compared to those with high school, gymnasium, or primary education. Excellent gum status was significantly more common in children whose male adults had a university education.
Regarding the frequency of dental hygiene among children, most parents who mentioned that their children brush at least twice a day were those with university education. Absent dental hygiene was significantly more frequent in children whose adults had a primary education (Table 3).

Table 3.
Distribution of participants related to the parental socioeconomic status and frequency of dental hygiene among children.
Among the disparities noted regarding the frequency of dental hygiene, it has been noticed that dental hygiene practiced two or more times a day was significantly more common in children whose male adults had a university education (58.9%), compared to those with gymnasium (29.7%) or primary education (17.4%). It has been noted that dental hygiene practiced several times a week was significantly more common in children whose female adults had a primary education (15.1%) compared to those with an academic education. Similarly, the case of tooth brushing once a day was higher among children with high school educated female adults (44.3%).
The behavior of the parents regarding the use of toothpaste and fluoride toothpaste is described in Table 4; it was observed that the higher the level of education of the adult with whom the child lives, greater attention is paid to the use of toothpaste and the use of fluoride toothpaste (p < 0.001) respectively.

Table 4.
Distribution of participants regarding the use of toothpaste/fluoride toothpaste.
The results show that the use of fluoride toothpaste was significantly more common in children whose male adults had a university/high school/gymnasium education (79.9%/75.2%/68.9%), compared to those with a primary education (41.8%). In the case of female adults who responded to this question, the absence of fluoride toothpaste usage was significantly more common in children whose female adults had a primary education (57.7%), compared to those with a gymnasium/high school/university education (31.5%/27.2%/19.9%).
Regarding the use of auxiliary means by children, the majority of parents with a university education mentioned that their children use dental floss (26.4% female/27.4% male), compared to those with a primary education, where the percentage was only 3.5% female/1.2% male (p < 0.001) (Table 5).

Table 5.
Distribution of participants related to parents’ socioeconomic status and use of brushing aids.
In relation to predicting the perceived oral health status of teeth and gums, as well as the frequency of tooth brushing and dental hygiene auxiliary aids, the multinomial regression models were employed. For predicting the use of toothpaste, the fluoride toothpaste, toothbrush, dental floss, and plastic toothpicks, bivariate regression models were utilized (Table 6).

Table 6.
Multinomial and binomial logistic regression models used in predicting effects of parents’ studies across children’s oral health.
In the case of dental health, both univariate and multivariate models (where both parents’ education levels were simultaneously considered in the prediction model) showed that the education levels of both parents had a significant effect on perceived health and oral hygiene habits of their children. Thus, observing the increasing trends of odds ratio (OR) values, compared to non-university education, a university education increase the odds of having a better perceived health status. The increase in odds is more pronounced for very good or excellent oral health states compared to others (comparing OR values among themselves). In the case of gum health, in the multivariable model, only the mothers’ education had a significant effect, exhibiting the same trend as observed for teeth health. Regarding the frequency of dental hygiene, a similar pattern is observed; both mothers’ and fathers’ education levels have a significant effect on dental hygiene frequency, similar to teeth/gums health. The increase in the odds of having better dental hygiene due to the presence of university education is greater for the appropriate frequency of dental hygiene compared to absent/very rare hygiene (a few times a month) (Table 6).
For the use of toothpaste, fluoride toothpaste, and plastic toothpicks, according to multivariable models, only mothers’ education levels had a significant and important effect on their usage. For example, the presence of university education in mothers significantly increased (p = 0.001) the odds of using fluoride toothpaste for children by 1.484 times (95% confidence interval: 1.174–1.875).
4. Discussion
The development of behavioral habits begins in childhood, involving parents, having an essential role in the formation of behavior related to oral health care of children.
Based on the results highlighted above, the level of education of the adults with whom the children live influences six categories of factors. These elements are: the perception of children’s dental health status, the perception of children’s gingival health status, the performance of oral hygiene and its frequency, as well as the use of fluoride toothpaste and brushing aids. This aspect can mean understanding the contextual elements associated with the way of life and level of education of adults.
In accordance with the objective of the study, the influence of socioeconomic factors and the perception of oral health status were highlighted in children from grades 0–8 in Romania. The differences between the groups were not significant, so the rural residence of the children was not significantly associated with the health status or the frequency of oral hygiene. This particularity is probably determined by the predominance of the urban living environment in which the child lives and by the fact that the study took place only in the urban environment, where there were dental offices in schools.
During the school years, the identification of risk factors leading to the appearance of carious lesions can refine the classification of caries risk in students and improve the management of existing resources in order reduce oral health inequalities [29,30,31].
Scientific articles have demonstrated that parents’ level of education and their social class have a significant impact on the profile of children’s oral health status [32]. The results of their analysis show that the parent’s level of education and increased family income decreases the prevalence of dental caries. Thus, the parents’ level of education and their profession influence the children’s oral health status [33]. Similar to the research carried out in Romania, it is highlighted that the lack of education of the parents has influences on the oral hygiene behaviors of the children [34]. Socioeconomic factors have also been correlated with the use of brushing aids [35]. Similar to another study conducted in Romania, the results highlight a potential influence of the parents’ education level, both for the mother and the father, regarding the dental brushing habits of children [21].
According to a study carried out in the Netherlands, the socioeconomic level of the mother is closely related to the occurrence of dental caries. The prevalence of carious lesions being much higher in the population categories with low socioeconomic level [5]. A range of studies highlights the positive impact of school-based oral health programs, especially those based on gamification [36]. Inequalities related to the different education levels of parents can be reduced with the help of programs initiated in school. School-based oral health programs represent effective tools for eliminating disparities in oral health [37]. Targeting teachers could improve the effectiveness of dental health education campaigns for children [38]. It is emphasized that maintaining a satisfactory level of oral hygiene at home depends on parental involvement, toothbrushing instructions, and educational programs [39].
In Denmark, Christensen et al. highlighted that a low maternal education level, low family wage income, and large families are associated with an increased prevalence of carious lesions [40]. The connection between the socioeconomic level of the family and dental hygiene ishighlighted in this study, and the presence of caries is highlighted in other studies [41]. These studies should stimulate the development of effective prevention strategies, with special attention to social classes with low incomes.
Attitudes and practices related to oral hygiene, diet, and individual factors related to cariogenesis can be effectively managed by ensuring access to the resources students need, even if they are limited [34]. Understanding the evolution of the distribution of risk factors and the prevalence of carious lesions with the help of repeated surveys is crucial for making the adjustment of strategies developed at the community level for the promotion of oral health [20].
The differences between the knowledge related to the health of the stomatognathic system and the attitudes of parents regarding oral hygiene underline the importance of oral health education [42]. Since oral hygiene is an important factor for oral health, adequate guidelines on dental hygiene methods and the relationship between dental hygiene and dental caries should be provided to the population [3]. Therefore, we should investigate these behaviors in more detail in order to provide a solid basis for prevention programs [43].
Strengths: The present research represents one of the most important studies carried out in our country, being the only national study that uses the methodology developed by the National Institute of Public Health and that evaluates the influence of family socioeconomic factors and the perception of adults on the behaviors related to children’s oral hygiene. It is the first study carried out in Romania that correlates the socioeconomic status of the parents and the use of fluoride toothpaste. In contrast to the previous studies carried out in Romania, which were carried out on a smaller sample, in this national study the cohort is composed of a large number that determines a more detailed analysis and a broader understanding of the determinants involved in the analysis of oral health status. This research reinforces the need for the development of prevention strategies for oral health, among children in Romania.
Limitations of the study: The correspondence between the parents’ perception with the oral condition of the children has not been assessed. The study was carried out in the urban environment, which led to an image that did not include the situation in the rural environment, where there are no school dental offices.
Possible further directions of research are the evaluation of the students’ behaviors related to diet and pattern of dental visits, as well as the correlation with clinical evaluation of the oral status carried out by the school dentists. The relationship between the effect of rurality, the educational level of the parents, and the oral health behavior of children can also be evaluated.
5. Conclusion
This research demonstrates that there is a possible correlation between the education level of the adult with whom the child lives and the perceived health and oral hygiene habits of their children. Furthermore, both mothers’ and fathers’ education have an impact on the frequency of oral hygiene among children. Building on the results that emphasize the use of fluoride toothpaste, the mother’s education level had a significant influence on their usage. Therefore, the main objective of school campaigns should be to inform and raise awareness among the target population regarding the importance of performing dental toothbrushing and using auxiliary means for tooth cleaning. It would be highly beneficial for students to practice tooth-brushing techniques and to learn about auxiliary brushing tools in the school dental offices. This is because, once children have acquired these skills, they can then educate their parents about these habits at home. The findings suggest that is crucial to have educational programs in Romania for taking care of schoolchildren’s oral health that involve parents, along with educators, including teachers and professors, under the guidance of dentists.
Author Contributions
Conceptualization, A.-C.P., R.S., M.T. and S.-M.P.; methodology, S.-M.P., M.T., C.F. and R.S.; software, A.-C.P. and A.R.T.; validation, M.M.I., C.F. and S.-M.P.; formal analysis, A.-C.P., M.T. and C.F.; investigation, A.-C.P., M.T., R.S. and S.-M.P.; resources, A.C., M.M.I., A.R.T. and C.F.; data curation, A.-C.P., M.T. and S.-M.P.; writing—original draft preparation, A.-C.P., M.T., A.C., A.R.T., M.M.I. and C.F.; writing—review and editing, R.S. and S.-M.P.; visualization, A.R.T. and M.T.; supervision, S.-M.P.; project administration, A.-C.P., R.S., M.T. and S.-M.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Research Ethics Committee of “Carol Davila” University of Medicine and Pharmacy Bucharest, protocol no. 36927/29.11.2022.
Informed Consent Statement
Informed consent was obtained from all parents involved in the study.
Data Availability Statement
The data presented in this study are available from the corresponding authors upon reasonable request.
Acknowledgments
The authors would like to thank the local authorities for their continuous support and essential collaboration during the conduct of the research. The study was conducted under the auspices of the University of Medicine and Pharmacy “Carol Davila”, through the Interdisciplinary Research and Development Center in Dentistry. “Publication of this paper was supported by the University of Medicine and Pharmacy Carol Davila, through the institutional program Publish not Perish”.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kwan, S.Y.; Petersen, P.E.; Pine, C.M.; Borutta, A. Health-promoting schools: An opportunity for oral health promotion. Bull. World Health Organ. 2005, 83, 677–685. [Google Scholar] [PubMed]
- Petersen, P.E. The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century--the approach of the WHO Global Oral Health Programme. Community Dent. Oral. Epidemiol. 2003, 31 (Suppl. 1), 3–23. [Google Scholar] [CrossRef] [PubMed]
- Castilho, A.R.; Mialhe, F.L.; Barbosa, T.d.S.; Puppin-Rontani, R.M. Influence of family environment on children’s oral health: A systematic review. J Pediatr. 2013, 89, 116–123. [Google Scholar] [CrossRef]
- Marmot, M.; Allen, J.; Bell, R.; Bloomer, E.; Goldblatt, P. Consortium for the European Review of Social Determinants of Health and the Health Divide. WHO European review of social determinants of health and the health divide. Lancet 2012, 380, 1011–1029. [Google Scholar] [CrossRef] [PubMed]
- van der Tas, J.T.; Kragt, L.; Elfrink, M.E.C.; Bertens, L.C.M.; Jaddoe, V.W.V.; Moll, H.A.; Ongkosuwito, E.M.; Wolvius, E.B. Social inequalities and dental caries in six-year-old children from the Netherlands. J. Dent. 2017, 62, 18–24. [Google Scholar] [CrossRef]
- Schwendicke, F.; Dörfer, C.E.; Schlattmann, P.; Foster Page, L.; Thomson, W.M.; Paris, S. Socioeconomic inequality and caries: A systematic review and meta-analysis. J. Dent. Res. 2015, 94, 10–18. [Google Scholar] [CrossRef]
- Harris, J. Dental neglect in children. Paediatr. Child Health 2012, 22, 476–482. [Google Scholar] [CrossRef]
- Chen, L.; Hong, J.; Xiong, D.; Zhang, L.; Li, Y.; Huang, S.; Hua, F. Are parents’ education levels associated with either their oral health knowledge or their children’s oral health behaviors? A survey of 8446 families in Wuhan. BMC Oral Health 2020, 20, 203. [Google Scholar] [CrossRef]
- Abbass, M.M.S.; Mahmoud, S.A.; El Moshy, S.; Rady, D.; AbuBakr, N.; Radwan, I.A.; Ahmed, A.; Abdou, A.; Al Jawaldeh, A. The prevalence of dental caries among Egyptian children and adolescences and its association with age, socioeconomic status, dietary habits and other risk factors. A cross-sectional study. F1000Research 2019, 8, 8. [Google Scholar] [CrossRef]
- Duijster, D.; van Loveren, C.; Dusseldorp, E.; Verrips, G.H. Modelling community, family, and individual determinants of childhood dental caries. Eur. J. Oral Sci. 2014, 122, 125–133. [Google Scholar] [CrossRef]
- Kämppi, A.; Tanner, T.; Päkkilä, J.; Patinen, P.; Järvelin, M.R.; Tjäderhane, L.; Anttonen, V. Geographical distribution of dental caries prevalence and associated factors in young adults in Finland. Caries. Res. 2013, 47, 346–354. [Google Scholar] [CrossRef]
- Mattila, M.L.; Rautava, P.; Ojanlatva, A.; Paunio, P.; Hyssälä, L.; Helenius, H.; Sillanpää, M. Will the role of family influence dental caries among seven-year-old children? Acta Odontol. Scand. 2005, 63, 73–84. [Google Scholar] [CrossRef]
- Mačiulskienė, V.; Razmienė, J.; Andruškevičienė, V.; Bendoraitienė, E. Estimation of Caries Treatment Needs in First Permanent Molars of Lithuanian 5-6-Year-Old Children, Based on Caries Lesion Activity Assessment. Medicina 2020, 56, 105. [Google Scholar] [CrossRef] [PubMed]
- Vilhena, F.V.; Sales-Peres, S.H.; Caldana Mde, L.; Buzalaf, M.A. Novo protocolo para as ações de saúde bucal coletiva: Padronização no armazenamento, distribuição e uso do material de higiene bucal [A new protocol for use and storage of tooth-brushing material for school children]. Cien. Saude Colet. 2008, 13 (Suppl. 2), 2097–2103. [Google Scholar] [CrossRef] [PubMed]
- Melo, P.; Fine, C.; Malone, S.; Frencken, J.E.; Horn, V. The effectiveness of the Brush Day and Night programme in improving children’s toothbrushing knowledge and behaviour. Int. Dent. J. 2018, 68 (Suppl. 1), 7–16. [Google Scholar] [CrossRef] [PubMed]
- Melo, P.; Fine, C.; Malone, S.; Taylor, S. Impact of the Brush Day & Night Programme on Oral Health Knowledge and Behaviour in Children. Int. Dent. J. 2021, 71 (Suppl. 1), S4–S14. [Google Scholar] [CrossRef] [PubMed]
- Štefanová, E.; Baška, T.; Holubčíková, J.; Timková, S.; Tatarková, M.; Sovičová, M.; Hudečková, H. Selected Behavioural Factors Affecting Oral Health in Schoolchildren: Results from the Health Behaviour in School-Aged Children (HBSC) Slovak Study. Int. J. Environ. Res. Public Health 2020, 17, 7516. [Google Scholar] [CrossRef]
- Kritikou, K.; Vinereanu, A.; Munteanu, A. Fluoride in Dentistry: Updated Short Guide on Dental Caries Prevention. Rom. J. Dent. Med. 2022, XXV, 97–109. [Google Scholar]
- Gavrila-Ardelean, L.; Gavrila-Ardelean, M.; Lackner, A.K.; Kozma, A. The role and resources of fluor in oral health. ORL.ro. 2021, 52, 42–46. [Google Scholar] [CrossRef]
- Sfeatcu, R.; Cărămidă, M.; Sava-Rosianu, R.; Matichescu, M.L.; Galuscan, A.; Dumitrache, M.A. Carious status and socio-behavioral risk factors among 12 year-old children in South-Central region in Romania. BMC Oral Health 2023, 23, 644. [Google Scholar] [CrossRef]
- Dumitrescu, R.; Sava-Rosianu, R.; Jumanca, D.; Balean, O.; Damian, L.-R.; Fratila, A.D.; Maricutoiu, L.; Hajdu, A.I.; Focht, R.; Dumitrache, M.A.; et al. The Impact of Parental Education on Schoolchildren’s Oral Health—A Multicenter Cross-Sectional Study in Romania. Int. J. Environ. Res. Public Health 2022, 19, 11102. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Public Health. Available online: https://insp.gov.ro/download/cnepss/stare-de-sanatate/boli_netransmisibile/sanatate_orala/Analiza-de-situatie-sanatatea-orala-2023.pdf (accessed on 18 October 2023).
- The European Commission. Available online: https://eurydice.eacea.ec.europa.eu/ro/national-education-systems/romania/organizarea-sistemului-de-educatie-si-structura-sa (accessed on 4 October 2023).
- National Institute of Public Health. Available online: https://insp.gov.ro/download/cnepss/metodologii_ghirduri_recomandrari_si_evidente_stintifice/metodologii/metodologii_evaluare_santate_copii/Metodologie-sanatate-orala-revizuita-19-aprilie-2022.pdf (accessed on 18 October 2023).
- Ministry of Education. Available online: https://juridicisj.eu/ORDIN%20nr%204183%202022%20Regulament%20cadru%20functionare%20unitati%20invatamant%20preuniversitar.pdf (accessed on 18 October 2023).
- ASSMB. Available online: https://assmb.ro/article/lista-cabinetelor-stomatologice-din-unit-ile-de-inv-mant-preuniversitar-i-universitar-de-stat-din-municipiul-bucure-ti (accessed on 18 October 2023).
- Petersen, P.E.; Baez, R.J. World Health Organization. In Oral Health Surveys: Basic Methods, 5th ed.; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- World Health Organization Process of Translation and Adaptation of Instruments. Available online: http://www.who.int/substance_abuse/research_tools/translation/en/ (accessed on 29 August 2023).
- Tan, S.H.X.; Teo, Y.Y.; Tan, M.H.X.; Gao, X. Childhood Factors and Dental Caries in the Permanent Dentition: Findings of an 8-Year Study Under a Nationwide School Dental Service. Int. Dent. J. 2021, 71, 508–515. [Google Scholar] [CrossRef]
- Källestål, C.; Wall, S. Socio-economic effect on caries. Incidence data among Swedish 12–14-year-olds. Community Dent. Oral Epidemiol. 2002, 30, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Saldūnaitė, K.; Bendoraitienė, E.A.; Slabšinskienė, E.; Vasiliauskienė, I.; Andruškevičienė, V.; Zūbienė, J. The role of parental education and socioeconomic status in dental caries prevention among Lithuanian children. Medicina 2014, 50, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Pizzo, G.; Piscopo, M.R.; Matranga, D.; Luparello, M.; Pizzo, I.; Giuliana, G. Prevalence and socio-behavioral determinants of dental caries in Sicilian schoolchildren. Med. Sci. Monit. 2010, 16, PH83-9. [Google Scholar] [PubMed]
- Kato, H.; Tanaka, K.; Shimizu, K.; Nagata, C.; Furukawa, S.; Arakawa, M.; Miyake, Y. Parental occupations, educational levels, and income and prevalence of dental caries in 3-year-old Japanese children. Environ. Health Prev. Med. 2017, 22, 80. [Google Scholar] [CrossRef] [PubMed]
- Dumitrescu, R.; Sava-Rosianu, R.; Jumanca, D.; Balean, O.; Damian, L.-R.; Guglielmo Giuseppe Campus; Maricutoiu, L.; Alexa, V.T.; Sfeatcu, R.; Daguci, C.; et al. Dental Caries, Oral Health Behavior, and Living Conditions in 6–8-Year-Old Romanian School Children. Children 2022, 9, 903. [Google Scholar] [CrossRef]
- Park, J.B.; Han, K.; Park, Y.G.; Ko, Y. Association between socioeconomic status and oral health behaviors: The 2008-2010 Korea national health and nutrition examination survey. Exp. Ther. Med. 2016, 12, 2657–2664. [Google Scholar] [CrossRef]
- GeethaPriya, P.R.; Asokan, S.; Kandaswamy, D.; Shyam, S. Impact of different modes of school dental health education on oral health-related knowledge, attitude and practice behaviour: An interventional study. Eur. Arch. Paediatr. Dent. 2020, 21, 347–354. [Google Scholar] [CrossRef]
- Gargano, L.; Mason, M.K.; Northridge, M.E. Advancing Oral Health Equity Through School-Based Oral Health Programs: An Ecological Model and Review. Front. Public Health 2019, 7, 359. [Google Scholar] [CrossRef]
- Thomas, S.; Tandon, S.; Nair, S. Effect of dental health education on the oral health status of a rural child population by involving target groups. J. Indian Soc. Pedod. Prev. Dent. 2000, 18, 115–125. [Google Scholar] [PubMed]
- McKittrick, T.R.; Jacobsen, K.H. Oral hygiene practices among middle-school students in 44 low- and middle-income countries. Int. Dent. J. 2014, 64, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Christensen, L.B.; Twetman, S.; Sundby, A. Oral health in children and adolescents with different socio-cultural and socio-economic backgrounds. Acta Odontol. Scand. 2010, 68, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Cianetti, S.; Lombardo, G.; Lupatelli, E.; Rossi, G.; Abraha, I.; Pagano, S.; Paglia, L. Dental caries, parents educational level, family income and dental service attendance among children in Italy. Eur. J. Paediatr. Dent. 2017, 18, 15–18. [Google Scholar] [CrossRef]
- Rajab, L.D.; Petersen, P.E.; Bakaeen, G.; Hamdan, M.A. Oral health behaviour of schoolchildren and parents in Jordan. Int. J. Paediatr. Dent. 2002, 12, 168–176. [Google Scholar] [CrossRef]
- Jepsen, S.; Blanco, J.; Buchalla, W.; Carvalho, J.C.; Dietrich, T.; Dörfer, C.; Eaton, K.A.; Figuero, E.; Frencken, J.E.; Graziani, F.; et al. Prevention and control of dental caries and periodontal diseases at individual and population level: Consensus report of group 3 of joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J. Clin. Periodontol. 2017, 44 (Suppl. 18), S85–S93. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).