Investigating COVID-19 Pandemic Effects on Acute Pancreatitis Development—From the Perspective of Alcohol Sales (Consumption) in a Japanese Regional Hospital
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Japan’s State of Emergency Declarations and Infection Countermeasures
2.3. Patients
2.4. Japanese Criteria for Assessing AP Severity
2.5. Statistical Analysis
3. Results
3.1. Changes in Alcohol Consumption under the COVID-19 Pandemic
3.2. Number of AP Patients and Etiology
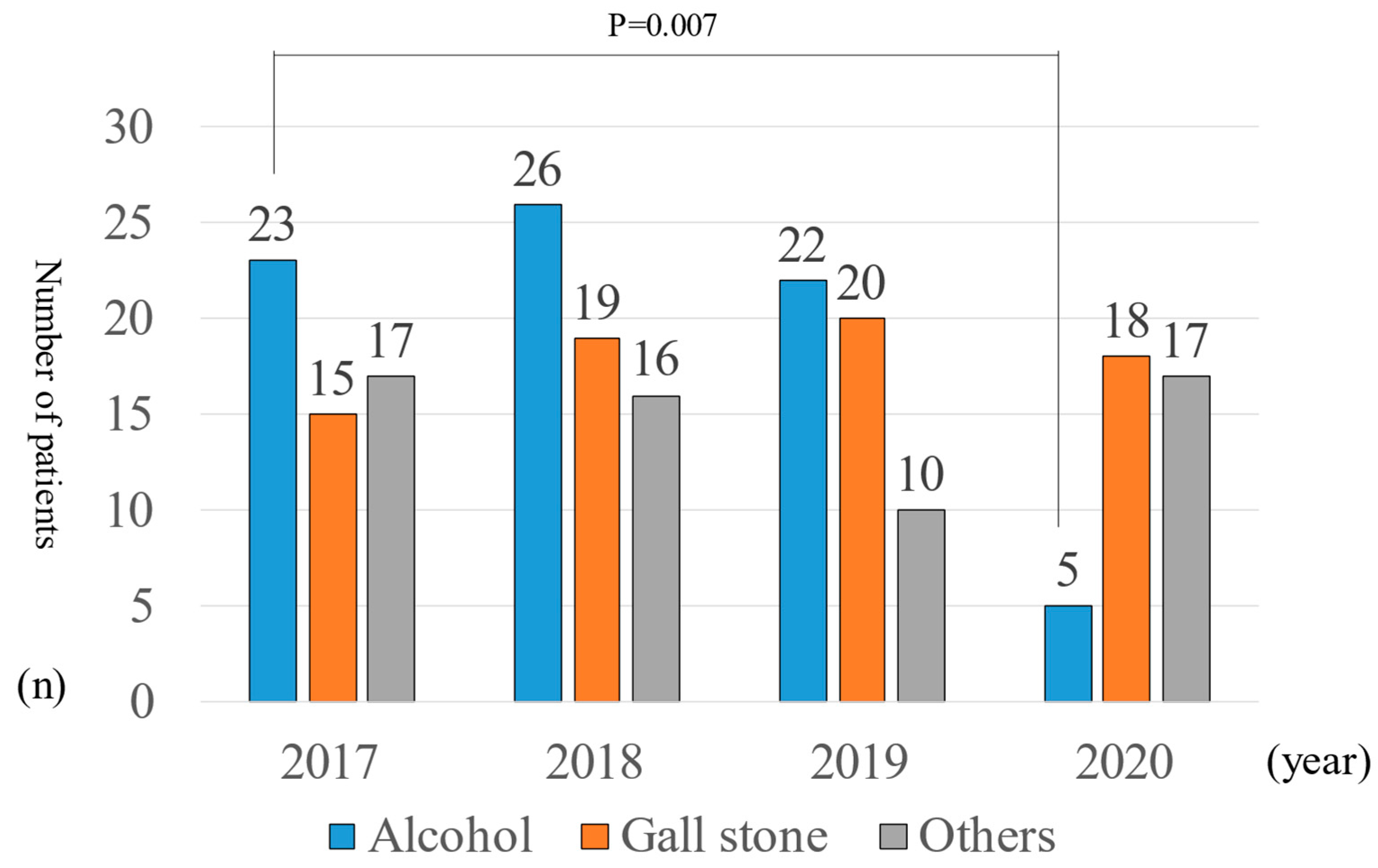
3.3. Number of Patients with Severe AP
3.4. Sex Differences of AP Patients
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- In Proceedings of the Declaration of a State of Emergency in Response to the Novel Coronavirus Disease. Available online: https://japan.kantei.go.jp/ongoingtopics/_00018.html (accessed on 8 August 2023).
- The Consumption of Alcoholic Beverages in Japan. Available online: https://www.nta.go.jp/taxes/sake/shiori-gaikyo/shiori/01.htm (accessed on 8 August 2023).
- Webster, P. Virtual health care in the era of COVID-19. Lancet 2020, 395, 1180–1181. [Google Scholar] [CrossRef] [PubMed]
- Wongtanasarasin, W.; Srisawang, T.; Yothiya, W.; Phinyo, P. Impact of national lockdown towards emergency department visits and admission rates during the COVID-19 pandemic in Thailand: A hospital-based study. Emerg. Med. Australas. 2021, 33, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, R.D.; O’Reilly, G.M.; Mitra, B.; Smit, V.; Miller, J.P.; Cameron, P.A. Impact of COVID-19 State of Emergency restrictions on presentations to two Victorian emergency departments. Emerg. Med. Australas. 2020, 32, 1027–1033. [Google Scholar] [CrossRef] [PubMed]
- Rennert-May, E.; Leal, J.; Thanh, N.X.; Lang, E.; Dowling, S.; Manns, B.; Wasylak, T.; Ronksley, P.E. The impact of COVID-19 on hospital admissions and emergency department visits: A population-based study. PLoS ONE 2021, 16, e0252441. [Google Scholar] [CrossRef]
- Ngu, N.L.Y.; Boyd, D.T.; Morgan, B.; Surampudi, A.; Brown, I.; Bykersma, C.; Kennett, G.; Yesmin, A.; Peng, Y.; Bell, S.; et al. Impact of increased alcohol consumption during the COVID-19-related lockdowns on admissions with liver disease, gastrointestinal bleeding and pancreatitis in Melbourne, Victoria. Intern. Med. J. 2023, 53, 830–834. [Google Scholar] [CrossRef] [PubMed]
- van Dijk, S.M.; Hallensleben, N.D.L.; van Santvoort, H.C.; Fockens, P.; van Goor, H.; Bruno, M.J.; Besselink, M.G. Dutch Pancreatitis Study Group. Acute pancreatitis: Recent advances through randomized trials. Gut 2017, 66, 2024–2032. [Google Scholar] [CrossRef]
- Morelli, N.; Rota, E.; Terracciano, C.; Immovilli, P.; Spallazzi, M.; Colombi, D.; Zaino, D.; Michieletti, E.; Guidetti, D. The Baffling Case of Ischemic Stroke Disappearance from the Casualty Department in the COVID-19 Era. Eur. Neurol. 2020, 83, 213–215. [Google Scholar] [CrossRef]
- De Filippo, O.; D’Ascenzo, F.; Angelini, F.; Bocchino, P.P.; Conrotto, F.; Saglietto, A.; Secco, G.G.; Campo, G.; Gallone, G.; Verardi, R.; et al. Reduced Rate of Hospital Admissions for ACS during COVID-19 Outbreak in Northern Italy. N. Engl. J. Med. 2020, 383, 88–89. [Google Scholar] [CrossRef]
- Yokoe, M.; Takada, T.; Mayumi, T.; Yoshida, M.; Isaji, S.; Wada, K.; Itoi, T.; Sata, N.; Gabata, T.; Igarashi, H.; et al. Japanese guidelines for the management of acute pancreatitis: Japanese Guidelines 2015. J. Hepatobiliary Pancreat. Sci. 2015, 22, 405–432. [Google Scholar] [CrossRef] [PubMed]
- Takada, T.; Isaji, S.; Mayumi, T.; Yoshida, M.; Takeyama, Y.; Itoi, T.; Sano, K.; Iizawa, Y.; Masamune, A.; Hirota, M.; et al. JPN clinical practice guidelines 2021 with easy-to-understand explanations for the management of acute pancreatitis. J. Hepatobiliary Pancreat. Sci. 2022, 29, 1057–1083. [Google Scholar] [CrossRef]
- Yamamiya, A.; Kitamura, K.; Yoshida, H.; Ishii, Y.; Mitsui, Y.; Irisawa, A. Prediction of the progression of walled-off necrosis in patients with acute pancreatitis on whole pancreatic perfusion CT. J. Hepatobiliary Pancreat. Sci. 2020, 27, 739–746. [Google Scholar] [CrossRef]
- Yamamiya, A.; Tominaga, K.; Hoshi, K.; Nagashima, K.; Minaguchi, T.; Haruyama, Y.; Irisawa, A. The Risk Factors for Progression to Chronic Pancreatitis in Patients with Past-History of Acute Pancreatitis: A Retrospective Analysis Based on Mechanistic Definition. J. Clin. Med. 2022, 11, 2209. [Google Scholar] [CrossRef]
- The Patient Survey in Japan. Available online: https://www.mhlw.go.jp/toukei/saikin/hw/kanja/10syoubyo/ (accessed on 8 August 2023).
- Tedros Adhanom Ghebreyesus. Foreword. Global Status Report on Alcohol and Health 201 & Switzerland: World Health Organization. Available online: https://www.who.int/publications/i/item/9789241565639 (accessed on 8 August 2023).
- Pollard, M.S.; Tucker, J.S.; Green, H.D., Jr. Changes in Adult Alcohol Use and Consequences During the COVID-19 Pandemic in the US. JAMA Netw. Open 2020, 3, e2022942. [Google Scholar] [CrossRef]
- Rehm, J.; Kilian, C.; Ferreira-Borges, C.; Jernigan, D.; Monteiro, M.; Parry, C.D.H.; Sanchez, Z.M.; Manthey, J. Alcohol use in times of the COVID 19: Implications for monitoring and policy. Drug Alcohol Rev. 2020, 39, 301–304. [Google Scholar] [CrossRef] [PubMed]
- Glowacz, F.; Schmits, E. Psychological distress during the COVID-19 lockdown: The young adults most at risk. Psychiatry Res. 2020, 293, 113486. [Google Scholar] [CrossRef]
- Lau, J.T.; Yang, X.; Pang, E.; Tsui, H.Y.; Wong, E.; Wing, Y.K. SARS-related perceptions in Hong Kong. Emerg. Infect. Dis. 2005, 11, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.; Liu, X.; Fang, Y.; Fan, B.; Fuller, C.J.; Guan, Z.; Yao, Z.; Kong, J.; Lu, J.; Litvak, I.J. Alcohol abuse/dependence symptoms among hospital employees exposed to a SARS outbreak. Alcohol Alcohol 2008, 43, 706–712. [Google Scholar] [CrossRef]
- Silczuk, A. Threatening increase in alcohol consumption in physicians quarantined due to coronavirus outbreak in Poland: The ALCOVID survey. J. Public Health 2020, 42, 461–465. [Google Scholar] [CrossRef]
- Schimmel, J.; Vargas-Torres, C.; Genes, N.; Probst, M.A.; Manini, A.F. Changes in alcohol-related hospital visits during COVID-19 in New York City. Addiction 2021, 116, 3525–3530. [Google Scholar] [CrossRef] [PubMed]
- Jackson, S.E.; Garnett, C.; Shahab, L.; Oldham, M.; Brown, J. Association of the COVID-19 lockdown with smoking, drinking and attempts to quit in England: An analysis of 2019–2020 data. Addiction 2021, 116, 1233–1244. [Google Scholar] [CrossRef]
- Murthy, P.; Narasimha, V.L. Effects of the COVID-19 pandemic and lockdown on alcohol use disorders and complications. Curr. Opin. Psychiatry 2021, 34, 376–385. [Google Scholar] [CrossRef]
- Itoshima, H.; Shin, J.H.; Takada, D.; Morishita, T.; Kunisawa, S.; Imanaka, Y. The impact of the COVID-19 epidemic on hospital admissions for alcohol-related liver disease and pancreatitis in Japan. Sci. Rep. 2021, 11, 14054. [Google Scholar] [CrossRef] [PubMed]
- Sugaya, N.; Yamamoto, T.; Suzuki, N.; Uchiumi, C. Alcohol Use and Its Related Psychosocial Effects during the Prolonged COVID-19 Pandemic in Japan: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 13318. [Google Scholar] [CrossRef]
- Trends in Medical Costs in Japan. Available online: https://www.mhlw.go.jp/topics/medias/year/20/index.html (accessed on 17 September 2023).
- Rodriguez-Leor, O.; Cid-Álvarez, B.; Ojeda, S.; Martín-Moreiras, J.; Rumoroso, J.R.; López-Palop, R.; Serrador, A.; Cequier, A.; Romaguera, R.; Cruz, I. Impact of the COVID-19 pandemic on interventional cardiology activity in Spain. Rec Interv Cardiol 2020, 2, 82–89. [Google Scholar] [CrossRef]
- Masamune, A.; Kikuta, K.; Hamada, S.; Tsuji, I.; Takeyama, Y.; Shimosegawa, T.; Okazaki, K.; Matsumoto, R.; Kume, K.; Miura, S.; et al. Japan Pancreas Society. Clinical practice of acute pancreatitis in Japan: An analysis of nationwide epidemiological survey in 2016. Pancreatology. 2020, 20, 629–636. [Google Scholar] [CrossRef] [PubMed]
- Population of Tochigi Prefecture. Available online: https://www.pref.tochigi.lg.jp/c05/kensei/aramashi/sugata/jinkou-menseki.html (accessed on 17 September 2023).
- Population of Tokyo. Available online: https://www.toukei.metro.tokyo.lg.jp/jsuikei/js-index.htm (accessed on 17 September 2023).
- Kawaida, K.; Yoshimoto, H.; Goto, R.; Saito, G.; Ogai, Y.; Morita, N.; Saito, T. The Use of All-You-Can-Drink System, Nomihodai, is Associated with the Increased Alcohol Consumption among College Students: A Cross-Sectional Tohoku. J. Exp. Med. 2018, 245, 263–267. [Google Scholar]
- Kono, H.; Wheeler, M.D.; Rusyn, I.; Lin, M.; Seabra, V.; Rivera, C.A.; Bradford, B.U.; Forman, D.T.; Thurman, R.G. Gender differences in early alcohol-induced liver injury: Role of CD14, NF-kappaB, and TNF-alpha. Am. J. Physiol. Gastrointest. Liver Physiol. 2000, 278, G652–G661. [Google Scholar] [CrossRef] [PubMed]
- Labor Force Survey in Medical Costs in Japan. Available online: https://www.stat.go.jp/data/roudou/rireki/gaiyou.html#ft_nendo (accessed on 29 September 2023).


| In 2017 | In 2018 | In 2019 | In 2020 | In 2021 | |
|---|---|---|---|---|---|
| Nationwide | 80.5 L | 79.3 L | 78.1 L | 75.0 L | 74.3 L |
| Tokyo | 111.6 L | 107.8 L | 105.0 L | 95.5 L | 96.6 L |
| Tochigi | 71.3 L | 69.2 L | 67.1 L | 65.3 L | 64.0 L |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sakuma, F.; Yamamiya, A.; Abe, Y.; Nagashima, K.; Minaguchi, T.; Kashima, K.; Kunogi, Y.; Fukushi, K.; Inaba, Y.; Sugaya, T.; et al. Investigating COVID-19 Pandemic Effects on Acute Pancreatitis Development—From the Perspective of Alcohol Sales (Consumption) in a Japanese Regional Hospital. Healthcare 2023, 11, 2769. https://doi.org/10.3390/healthcare11202769
Sakuma F, Yamamiya A, Abe Y, Nagashima K, Minaguchi T, Kashima K, Kunogi Y, Fukushi K, Inaba Y, Sugaya T, et al. Investigating COVID-19 Pandemic Effects on Acute Pancreatitis Development—From the Perspective of Alcohol Sales (Consumption) in a Japanese Regional Hospital. Healthcare. 2023; 11(20):2769. https://doi.org/10.3390/healthcare11202769
Chicago/Turabian StyleSakuma, Fumi, Akira Yamamiya, Yoko Abe, Kazunori Nagashima, Takahito Minaguchi, Ken Kashima, Yasuhito Kunogi, Koh Fukushi, Yasunori Inaba, Takeshi Sugaya, and et al. 2023. "Investigating COVID-19 Pandemic Effects on Acute Pancreatitis Development—From the Perspective of Alcohol Sales (Consumption) in a Japanese Regional Hospital" Healthcare 11, no. 20: 2769. https://doi.org/10.3390/healthcare11202769
APA StyleSakuma, F., Yamamiya, A., Abe, Y., Nagashima, K., Minaguchi, T., Kashima, K., Kunogi, Y., Fukushi, K., Inaba, Y., Sugaya, T., Tominaga, K., Goda, K., & Irisawa, A. (2023). Investigating COVID-19 Pandemic Effects on Acute Pancreatitis Development—From the Perspective of Alcohol Sales (Consumption) in a Japanese Regional Hospital. Healthcare, 11(20), 2769. https://doi.org/10.3390/healthcare11202769







