Depression and Suicidal Ideation in Patients with Mental Illness in South Korea: The Mediating Effect of Alcohol Drinking
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Study Population
2.3. Measures
2.3.1. Variables
2.3.2. Depression
2.3.3. Alcohol Drinking
2.3.4. Suicidal Ideation
2.4. Data Collection
2.5. Data Analysis
3. Results
3.1. General Characteristics of the Participants and the Difference of Suicidal Ideation Depending on their General Characteristics
3.2. Degrees of Depression, Alcohol Use, and Suicidal Ideation
3.3. Correlations between the Study Participants’ Depression, Alcohol Use, and Suicidal Ideation
3.4. Effects of the Study Participants’ Depression and Alcohol Drinking on Suicidal Ideation
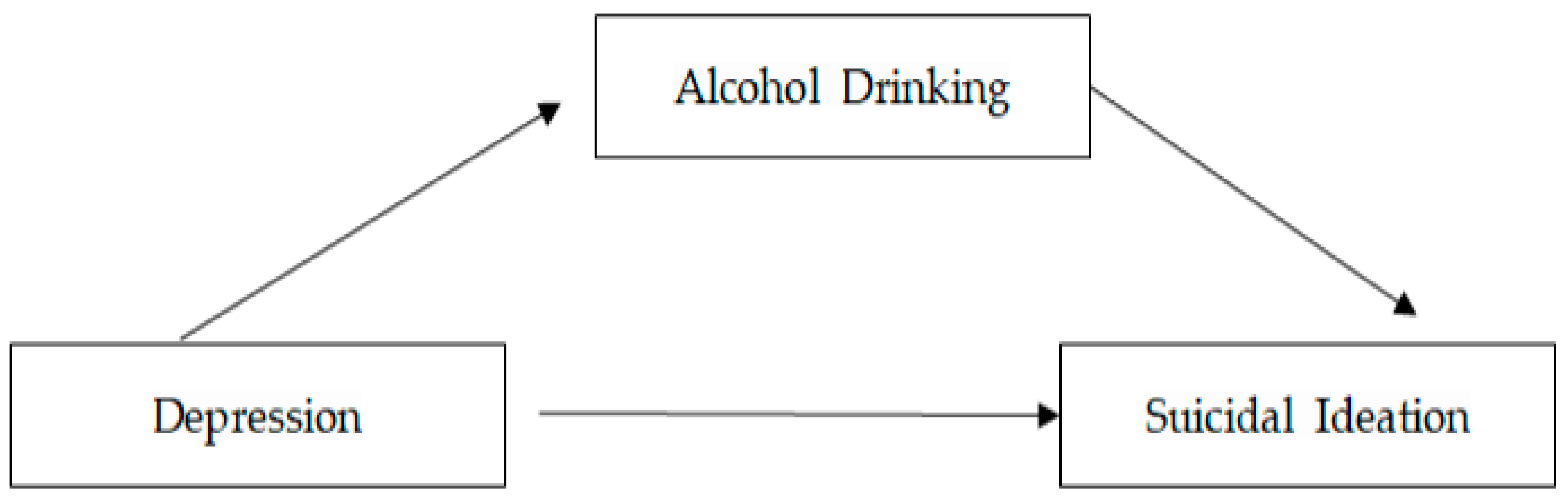
3.5. The Mediating Effect of Alcohol Drinking on the Relationship between the Study Participants’ Depression and Suicidal Ideation
4. Discussion
5. Conclusions and Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- National Statistical Office. 2022. Available online: https://www.index.go.kr/unity/potal/indicator/IndexInfo.do?popup=Y&clasCd=2&idxCd=5091 (accessed on 21 September 2023).
- Brådvik, L. Suicide risk and mental disorders. Int. J. Environ. Res. Public Health 2018, 15, 2028. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.; Jang, S.Y.; Chun, S.Y.; Lee, T.H.; Han, K.T.; Park, E.C. Mortality in schizophrenia and other psychoses: Data from the South Korea national health insurance cohort, 2002. J. Korean Med. Sci. 2017, 32, 835–842. [Google Scholar] [CrossRef] [PubMed]
- Arsenault-Lapierre, G.; Kim, C.; Turecki, G. Psychiatric diagnoses in 3275 suicides: A meta-analysis. BMC Psychiatry 2004, 4, 37. [Google Scholar] [CrossRef] [PubMed]
- Hirokawa, S.; Kawakami, N.; Matsumoto, T.; Inagaki, A.; Eguchi, N.; Tsuchiya, M. Mental disorders and suicide in Japan: A nation-wide psychological autopsy case-control study. J. Affect. Disord 2012, 140, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Boenisch, S.; Bramesfeld, A.; Mergl, R.; Havers, I.; Althaus, D.; Lehfeld, H.; Niklewski, G.; Hegerl, U. The role of alcohol use disorder and alcohol consumption in suicide attempts-A secondary analysis of 1921 suicide attempts. Eur. Psychiatry 2010, 25, 414–420. [Google Scholar] [CrossRef]
- Min, S.K. Modern Psychiatry; Ilchokak: Seoul, Republic of Korea, 2010. [Google Scholar]
- Rossau, C.D.; Mortensen, P.B. Risk factors for suicide in patients with schizophrenia: Nested case-control study. Br. J. Psychiatry 1997, 171, 355–359. [Google Scholar] [CrossRef]
- Kim, M.Y.; Ha, S.J.; Jun, S.S. Factors related to suicidal ideation in patients with chronic schizophrenia, depressive disorder, or bipolar disorder. J. Korean Acad. Psychiatr. Ment. Health Nurs. 2015, 24, 217–225. [Google Scholar] [CrossRef][Green Version]
- Lee, K.S.; Ko, Y.M.; Kim, K.S. Factors associated with suicidal ideation of psychiatric patients using mental health promotion and medical institutions in Ulsan Metropolitan City. J. Korean Neuropsychiatr. Assoc. 2021, 60, 298–306. [Google Scholar] [CrossRef]
- Cannon, B.; Mulroy, R.; Otto, M.W. Dysfuntional attitudes and poor problem solving skill predict hopelessness in Major depression. J. Affect. Disorder 1999, 55, 45–49. [Google Scholar] [CrossRef]
- Mehlenbeck, R.; Spirito, A.; Barnett, N.; Overholser, J. Behavioral factors: Substance use. In Evaluating and Treating Adolescent Suicide Attempters: From Research to Practice; Spiritom, A., Overholser, J.C., Eds.; Academic Press: San Diego, CA, USA, 2003. [Google Scholar]
- Brent, D.A.; Perper, J.A.; Moritz, G.; Allan, C.; Friend, A.; Roth, B.S.; Schweers, J.; Balach, L.; Baugher, M. Psychiatric risk factors for adolescent suicide: A case control study. J. Am. Acad. Child Adolesc. Psychiatry 1993, 32, 521–529. [Google Scholar] [CrossRef]
- Clark, D.C.; Fawcett, J. An empirically based model of suicide risk assessment for patients with affective disorder. In Suicide and Clinical Practice; Jacobs, D., Ed.; American Psychiatric Press: Washington, DC, USA, 1992. [Google Scholar]
- Goldman, M.S.; Del Boca, F.K.; Darkes, J. Alcohol expectancy theory: The application of cognitive neuroscience. In Psychological Theories of Drinking and Alcoholism, 2nd ed.; Leonard, K.E., Ed.; Guilford Press: New York, NY, USA, 1999. [Google Scholar]
- Cooper, M.; Wood, P.K.; Orcutt, H.K.; Albino, A. Personality and the predisposition to engage in risky or problem behaviors during adolescence. J. Personal. Soc. Psychol. 2003, 84, 390–410. [Google Scholar] [CrossRef] [PubMed]
- Derogatis, L.R.; Fitzpatrick, M. The SCL-90-R, the Brief Symptom Inventory (BSI), and the BSI-18. In The Use of Psychological; Maruish, M.E., Ed.; American Psychological Associations: Washington, DC, USA, 2004. [Google Scholar]
- Radloff, L.S. The CES-D scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Cho, M.J.; Kim, K.H. Diagnostic validity of the CES-D (Korean version) in the assessment of DSM-III-R major depression. J. Korean Neuropsychiatry 1993, 32, 381–399. [Google Scholar]
- Babor, T.F.; de la Fuente, J.R.; Saunders, J.; Grant, M. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Health Care; World Health Organization: Geneva, Switzerland, 1989. [Google Scholar]
- Lee, B.O.; Lee, C.H.; Lee, P.G.; Choi, M.J.; Namkoong, K. Development of Korean version of alcohol use disorders identification test [AUDITK]: Its reliability and validity. J. Korean Acad. Addict. Psychiatry 2000, 4, 83–92. [Google Scholar]
- Harlow, L.L.; Newcomb, M.D.; Bentler, P.M. Depression, self-derogation, substance use, and suicide ideation: Lack of purpose in life as a mediational factor. J. Clin. Psychol. 1986, 42, 2–5. [Google Scholar] [CrossRef]
- Kim, H.S. A study on epistemology of Korean elder’s suicidal thought. J. Korea Gerontol. Soc. 2002, 22, 159–172. [Google Scholar]
- Seo, S.Y.; Kim, H.S.; Kim, Y.T. Factors influencing suicidal ideation in people with mental disorder. J. Korean Acad Commun. Health Nurs. 2013, 24, 245–254. [Google Scholar] [CrossRef]
- Lee, M.Y.; Kim, Y.S. Factors influencing suicidal ideation in people with mental disorder. Korean J. Health Serv. Manag. 2014, 8, 209–220. [Google Scholar]
- Baron, R.M.; Kenny, D.A. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Personal. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Tidemalm, D.; Långström, N.; Lichtenstein, P.; Runeson, B. Risk of suicide after suicide attempt according to coexisting psychiatric disorder: Swedish cohort study with long term follow-up. Br. Med. J. 2008, 337, 1–6. [Google Scholar] [CrossRef]
- Heo, E.H.; Jeong, S.H.; Kang, H.Y. Comparative study on personality assessment inventory and MMPI-2 profiles of groups with high and low depression and suicide ideation in psychiatry patients and discriminant variables of depression and suicide ideation. J. Korean Neuropsychiatr. Assoc. 2018, 57, 86–95.00E5. [Google Scholar] [CrossRef]
- Bossarte, R.M.; Swahn, M.H. The associations between early alcohol use and suicide attempts among adolescents with a history of major depression. Addict. Behav. 2011, 36, 532–535. [Google Scholar] [CrossRef]
- Swahn, M.H.; Bossarte, R.M. Gender, early alcohol use, and suicide ideation and attempts: Findings from the 2005 Youth Risk Behavior Survey. J. Adolesc. Health 2007, 41, 175–181. [Google Scholar] [CrossRef]
- Hufford, M.R. Alcohol and suicidal behavior. Clin. Psychol. Rev. 2001, 21, 797–811. [Google Scholar] [CrossRef]
- Goldston, D.B. Conceptual issues in understanding the relationship between suicidal behavior and substance use during adolescence. J. Drug Alcohol Depend. 2004, 76, 79–91. [Google Scholar] [CrossRef]
- Yoon, M.S.; Cho, H.J. A Longitudinal effects analysis of adolescent drinking on the suicidal ideation. J. Youth Welf. 2011, 13, 43. [Google Scholar]
- Mamun, M.A. Suicide and suicidal behaviors in the context of COVID-19 pandemic in Bangladesh: A systematic review. Psychol. Res. Behav. Manag. 2021, 14, 695–704. [Google Scholar] [CrossRef] [PubMed]
- Mamun, M.A.; Sakib, N.; Gozal, D.; Bhuiyan, A.I.; Hossain, S.; Bodrud-Doza, M.; Al Mamun, F.; Hosen, I.; Safiq, M.B.; Abdullah, A.H.; et al. The COVID-19 pandemic and serious psychological consequences in Bangladesh: A population based nationwide study. J. Affect. Disord. 2021, 279, 462–472. [Google Scholar] [CrossRef] [PubMed]
- Gang, M.H. Influencing factors on alcohol use of persons with severe mental illness in the community. J. Digit. Policy Manag. 2013, 11, 585–593. [Google Scholar] [CrossRef]
- Gregg, L.; Barrowclough, C.; Haddock, G. Reasons for increased substance use in psychosis. Clin. Psychol. Rev. 2007, 27, 494–510. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s)and not of MDPI and/or the editor(s). MDPI and/or the editor(s)disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
| Characteristics | Category | n | % | Mean ± SD | Suicidal Ideation | |
|---|---|---|---|---|---|---|
| Mean ± SD | t/F (p) Scheffé Test | |||||
| Gender | Male | 81 | 49.7 | 8.08 ± 3.92 | −2.84 (0.005) | |
| Female | 82 | 50.3 | 10.09 ± 5.11 | |||
| Age (years) | 20 s | 35 | 21.5 | 44.10 ± 13.29 | 10.86 ± 5.21 | 1.71 (0.149) |
| 30 s | 25 | 15.3 | 8.13 ± 4.10 | |||
| 40 s | 42 | 24.8 | 9.61 ± 5.18 | |||
| 50 s | 35 | 21.5 | 8.64 ± 4.27 | |||
| ≥60 s | 26 | 16.9 | 8.25 ± 3.84 | |||
| Religion | Have | 82 | 50.3 | 8.84 ± 5.07 | 0.95 (0.341) | |
| None | 81 | 49.7 | 9.57 ± 5.261 | |||
| Hospitalization status | Inpatient | 68 | 41.6 | 8.60 ± 4.57 | 0.16 (0.850] | |
| Outpatient | 95 | 58.4 | 9.44 ± 4.75 | |||
| Diagnosis | Schizophrenia a | 82 | 50.3 | 7.34 ± 3.59 a | 22.55 (<0.001) c > a,b | |
| Bipolar disorder b | 32 | 19.6 | 8.84 ± 4.59 a | |||
| Depression c | 49 | 30.1 | 12.39 ± 4.75 c | |||
| First onset | <20 | 49 | 30.3 | 30.35 ± 13.71 | 7.91 ± 3.86 | 2.18 (0.091) |
| 20 s | 33 | 20.0 | 10.06 ± 5.54 | |||
| 30 s | 36 | 22.1 | 9.89 ± 4.25 | |||
| ≥40 | 45 | 27.6 | 9.67 ± 4.91 | |||
| Number of admissions | 0 | 51 | 31.4 | 2.91 ± 1.54 | 7.91 ± 3.86 | 1.85 (0.123) |
| 1 | 31 | 18.9 | 10.06 ± 5.54 | |||
| 2 | 36 | 22.1 | 9.89 ± 4.25 | |||
| ≥3 | 45 | 27.6 | 9.67 ± 4.91 | |||
| Sleep time | ≤4 a | 34 | 21.1 | 7.74 ± 2.33 | 12.29 ± 5.67 | 7.06 (<0.001) a,b > c,d |
| 5–6 b | 26 | 16.2 | 10.37 ± 5.32 | |||
| 7–8 c | 52 | 31.9 | 7.90 ± 3.52 | |||
| ≥9 d | 51 | 30.8 | 8.51 ± 4.33 | |||
| Sleep satisfaction | Satisfaction a | 53 | 32.4 | 7.40 ± 3.62 a | 16.44 (<0.001) c > a,b | |
| Neutral b | 56 | 34.1 | 8.78 ± 4.36 b | |||
| Dissatisfied c | 54 | 33.5 | 12.37 ± 5.06 c | |||
| Previous suicide attempts | Have | 82 | 50.3 | 11.30 ± 4.96 | 6.64 (<0.001) | |
| None | 81 | 49.7 | 6.98 ± 3.22 | |||
| Variable | Mean ± SD | Actual Range | Reference Range |
|---|---|---|---|
| Depression | 26.97 ± 13.62 | 0–58 | 0–60 |
| Slowdown in physical behavior | 11.20 ± 6.15 | 0–24 | 0–24 |
| Depressive emotion | 9.55 ± 5.61 | 0–21 | 0–21 |
| Positive emotion | 4.10 ± 2.05 | 0–9 | 0–9 |
| Interpersonal relationship | 2.12 ± 1.79 | 0–6 | 0–6 |
| Alcoholdrinking | 4.32 ± 8.48 | 0–40 | 0–40 |
| Suicide ideation | 9.15 ± 4.69 | 5–20 | 5–20 |
| Variable | Depression | Alcohol Drinking | Suicide Ideation |
|---|---|---|---|
| r(p) | r(p) | r(p) | |
| Depression | 1 | ||
| Alcohol drinking | 0.26 (<0.001) | 1 | |
| Suicide ideation | 0.63 (<0.001) | 0.36 (<0.001) | 1 |
| Variable | Model 1 | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B | β | p | B | β | p | B | β | p | |
| Gender | 1.57 | 0.16 | 0.007 | 1.07 | 0.11 | 0.044 | 1.38 | 0.14 | 0.009 |
| Age | −0.69 | −0.18 | 0.003 | −0.639 | −0.17 | 0.002 | −0.63 | −19 | 0.002 |
| Religion | 0.03 | 0.14 | 0.623 | 0.03 | 0.03 | 0.580 | 0.02 | 0.02 | 0.659 |
| Hospitalization status | 0.02 | 0.11 | 0.666 | −0.01 | −0.01 | 0.846 | −0.01 | −0.01 | 0.937 |
| Diagnosis | 1.3 | 0.25 | <0.001 | 0.968 | 0.18 | 0.004 | 0.73 | 0.13 | 0.031 |
| First onset | 0.03 | 0.03 | 0.620 | 0.04 | 0.04 | 0.432 | 0.04 | 0.05 | 0.393 |
| Number of admissions | −0.02 | −0.03 | 0.603 | −0.02 | −0.02 | 0.611 | −0.03 | −0.03 | 0.558 |
| Sleep time | −0.64 | −0.14 | 0.030 | −0.10 | −0.10 | 0.090 | −0.08 | −0.09 | 0.127 |
| Sleep satisfaction | 0.85 | 0.14 | 0.043 | 0.07 | 0.08 | 0.163 | 0.07 | 0.07 | 0.250 |
| Previous suicide attempt | −3.4 | −0.36 | <0.001 | −2.62 | −0.28 | <0.001 | −2.43 | −0.26 | <0.001 |
| Depression | 0.15 | 0.43 | <0.001 | 0.14 | 0.42 | <0.001 | |||
| Alcohol use | 0.09 | 0.17 | 0.005 | ||||||
| R2 | 0.447 | 0.537 | 0.560 | ||||||
| Adj. R2 | 0.426 | 0.523 | 0.543 | ||||||
| F change | 21.03 | 36.46 | 33.08 | ||||||
| Durbin–Watson | 1.81 | ||||||||
| Step | Independent Variables | Dependent Variables | B | S.E | β | T(p) | R2 | Adjusted R2 | F (p) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Depression | Alcohol drinking | 0.16 | 0.04 | 0.26 | 3.46(<0.001) | 0.069 | 0.063 | 11.98 (<0.001) |
| 2 | Depression | Suicidal ideation | 0.21 | 0.02 | 0.63 | 10.38(<0.001) | 0.401 | 0.398 | 107.92 (<0.001) |
| 3 | Depression, alcohol drinking | Suicidal ideation | 0.19 | 0.02 | 0.57 | 9.45(<0.001) | 0.442 | 0.435 | 63.38 (<0.001) |
| 0.12 | 0.034 | 0.21 | 3.42(<0.001) | ||||||
| Sobel test Z(p) = 3.63 (p < 0.001) | |||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, K.; Lee, O. Depression and Suicidal Ideation in Patients with Mental Illness in South Korea: The Mediating Effect of Alcohol Drinking. Healthcare 2023, 11, 2711. https://doi.org/10.3390/healthcare11202711
Lee K, Lee O. Depression and Suicidal Ideation in Patients with Mental Illness in South Korea: The Mediating Effect of Alcohol Drinking. Healthcare. 2023; 11(20):2711. https://doi.org/10.3390/healthcare11202711
Chicago/Turabian StyleLee, Kyoungsook, and Oisun Lee. 2023. "Depression and Suicidal Ideation in Patients with Mental Illness in South Korea: The Mediating Effect of Alcohol Drinking" Healthcare 11, no. 20: 2711. https://doi.org/10.3390/healthcare11202711
APA StyleLee, K., & Lee, O. (2023). Depression and Suicidal Ideation in Patients with Mental Illness in South Korea: The Mediating Effect of Alcohol Drinking. Healthcare, 11(20), 2711. https://doi.org/10.3390/healthcare11202711






